Abstract
Comparison of the results of bioabsorbable interference screws and posts for hamstring graft distal fixation in ACL reconstructions are presented. The results of 20 patients with bioabsorbable screws were compared to 22 patients with posts. The assessement was based on Lysholm-Gillquist and Marshall scores and the KT-1000 device. In the study group the points gained were 38.9 in the Lysholm-Gillquist and 12.89 in the Marshall scale. The average KT-1000 difference was 2.46 mm. In the control group the points gained were 32.93 in the Lysholm-Gillquist and 11.47 in the Marshall scale. The average KT-1000 difference was 2.5 mm. There were 14 patients in the study group with interference screw problems; in 2 the implants were removed. (1) There are no differences in outcome using bioabsorbable interference screws and posts for distal fixation of hamstring ACL grafts. (2) The lack of bioabsorbtion with poly L-lactide interference screws is frequent and causes problems.
Résumé
Le but de cette étude est de comparer les résultats d’une vis d’interférence résorbable ou non résorbable dans la fixation des muscles ischio-jambiers pour la reconstruction du LCA. Les résultats de 20 patients avec vis d’interférence résorbable ont été comparés à 22 patients avec vis non résorbable. Les résultats ont été évalués selon le score de Lysholm et Gillquist, le score de Marshall et l’appareil KT-1000. Dans le groupe d’étude, l’amélioration du score a été de 38.9 pour Lysholm-Gillquist et de 12.89 avec la méthode de Marshall, avec une différence de 2.46 mm avec l’appareillage KT-1000. Dans le groupe contrôle, l’amélioration a été de 32.93 avec la méthode Lysholm-Gillquist et de 11.47 avec la méthode de Marshall, la différence avec KT-1000 de 2.5 mm. Il y avait 14 patients dans le groupe d’étude avec vis d’interférence et deux implants ont dû être enlevé. Il n’y a pas de différence significative que l’on utilise ou non des vis d’interférence biorésorbable. Avec ces vis d’interférence poly L-Lactide biorésorbable leur résorption est fréquente et peut être source de problèmes.
Introduction
ACL reconstruction procedures have become more and more popular mostly due to very good results achieved by individuals in returning to the preinjury activity level. Several operative techniques have been described. All authors stress the need for prompt rehabilitation focused on muscle strengthening and almost immediate full range of motion exercises. Rigid fixation of the graft is a “sine qua non” condition [17]. The patellar ligament (LP), called the gold standard, is frequently replaced by hamstring tendons as a source of the graft. Numerous works prove them to be efficient and reliable. They are thought to cause fewer problems in anterior knee symptoms and are at least equal in every other way to the patellar tendon [1, 8, 10]. Many fixation devices have been invented aiming to reach rigid stability just after the graft implantation. Despite numerous laboratory and clinical studies, no system has been shown to be outstandingly better than others currently in use [2]. The critical issue is to assure stability of the graft for the period required to incorporate the graft into the bone tunnel [18, 25]. After this period the fixation device is no longer needed and can be removed. However, the next operative procedure is inevitable. Left in place, the fixation device leaves the patient with constant concern about “carrying” the metal parts.
The potential solution seemed to be bioabsorbable materials. Kulkarni was the first to describe the medical use of poly-L-lactic acid (PLLA) for the suture and rods for the repair of mandibular fractures in dogs [11]. The very first report of PLLA in ACL surgery was by Barber [4]. Further works proved that bioresorbable materials assure enough strength and can withstand pull-out forces comparable or superior to titanium interference screws [6]. The aperture fixation they offer is potentially more physiological, easing the graft ingrowth. Due to the ability to be absorbed, no removal is required [4]. However, although the manufacturers claim optimal performance and full bioabsorption, the fixation device might cause several problems. Broken screws, joint cavity material migration, excessive inflammatory response, cyst formation, osteolytic changes and, most commonly, delayed absorption are mentioned in this issue [5, 19, 20, 23].
The purpose of the study was to compare the clinical results using poly L-lactide bioabsorbable interference screws (Arthrex, Naples, FL) to using screw-posts (ChM, Lewickie, Poland) for distal fixation of ACL grafts delivered from quadrupled semitendinosus (ST) and gracilis (GR) tendons in ACL reconstruction.
Materials and methods
A consecutive cohort of 42 patients, male and female, who sought treatment for a chronic tear of the anterior cruciate ligament at our institutions was asked to participate in the study. They were assigned into one of the two groups and observed prospectively.
The study group consisted of 20 patients, and the control group consisted of 22 patients. Bioabsorbable screws in the study group and post-screws in the control group were used for distal fixation. Patients were treated between September 2003 and December 2003 by the same operating team.
In the study group there were 6 females and 14 males. The patient ages varied from 17 to 46 years (mean 24.5 years). In the control group there were 7 females and 15 males and patient ages varied from 18 to 48 years (mean 23.7 years). In both groups the minimum follow-ups were longer than 30 months. There were no statistically important differences between the groups regarding gender, age and concomitant meniscal and chondral lesions.
Clinical results were assessed with physical examination, Lysholm and Gillquist and Marshall scores [12, 14]. Restored stability was evaluated using clinical stability tests and KT-1000 assessment. KT-1000 assessment was done only at the final examination.
Statistical analysis was performed using SPSS Statistica 6.0 PL software. Non-parametric Mann-Whitney “U” test and non-parametric Wilcoxon test were used. A p-value ≤0.05 was considered significant, p ≤ 0.01 and p ≤ 0.001 as highly and very highly significant, respectively.
Operative technique
Operative technique was the same in both groups except the distal fixation.
All patients were operated upon with a single-incision arthroscopic technique. The ST and GR tendons were harvested through the mid-anterior approach. Both tunnels were prepared by the transtibial technique. An EndoButton (Smith & Nephew, Andover, MA) loop for proximal fixation of the quadrupled ST + GR graft in the control and study group was used. The distal diameter of the graft did not differ between the groups and was between 8 and 10 mm. For the distal fixation either poly L-lactide bioabsorbable interference screw in the study group or post-screw fixation in the control group were used.
Rehabilitation protocol
There were no differences in rehabilitation protocol in both groups. The protocol was an authors’ modification of protocols described by Shelbourne [9, 24]. The key factors to monitor were: joint effusion, pain during motion, quadriceps and hamstring strength. Both groups of patients were advised to use long braces allowing for 0–30° ROM immediately after surgery and then as tolerated. Two-crutch, non-weight-bearing for the first 7–14 days gradually increasing to full weight-bearing after 4–6 weeks, was advised. CPM was applied 24–48 h after surgery in the painless range with full extension and flexion as tolerated. All patients were encouraged to do quadriceps and hamstring closed chain exercises, isometric exercises and manual patella and LP self-mobilisation. Proprioreception and co-ordination exercises were introduced 6–8 weeks after the reconstruction.
Results
In the study group the preoperative assessment score in the Lysholm-Gillquist scale was 55.4 (±4.88) points, the postoperative assessment score was 94.46 (±2.99) points, and the mean points gained were 38.9 (±3.18 SD). In the Marshall scale the preoperative assessment score was 33.33 (±2.12 SD), the postoperative assessment score was 46.15 (±2.51 SD), and the mean points gained were 12.89 (±2.47 SD). The average KT-1000 134N side-to-side difference was 2.46 mm (±1.78) at the final assessment. There was one traumatic graft failure in the study group caused by a twisting injury during a basketball game 32 months after operation.
In the control group the preoperative assessment score in the Lysholm-Gillquist scale was 59.4 (±6.52) points, the postoperative assessment score 92 (±6.15) points, and the mean points gained were 32.93 (±9.8 SD) points. In the Marshall scale the preoperative assessment score was 33.4 (±2.55 SD), the postoperative assessment score was 44.5 (±3.74 SD), and the mean points gained were 11.47 (±4.12 SD). The average KT-1000 134N side-to-side difference was 2.5 mm (±1.68) at the final assessment. There were two traumatic graft ruptures caused by twisting injury during basketball and soccer games 24 and 19 months postoperatively. The reason for one additional graft failure was unclear, with no correlation to significant injury noted in the control group.
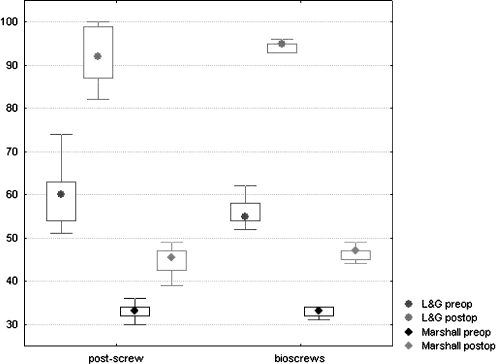
There were no statistically important differences between the study and control group regarding the above-mentioned assessments (Fig. 1).
Fig. 1.
Wilcoxon test for L&G and Marshall pre- and postoperative assessments
Fourteen out of 20 patients in the study group complained of prominent clinical symptoms, either local or distant from the bioabsorbable screw. Those 14 individuals suffered permanent and prolonged pain that did not subside after regular doses of non-steroidal anti-inflammatory medication. In this subgroup MRI assessment between 16 and 30 months after implantation was performed. On every MRI scan the screw was visible with the thread details, in six cases accompanied by large cyst formation (Figs. 2 and 3). Ten patients complained of minor to moderate pain and discomfort in the operated knee. In four cases the symptoms were severe and followed by medical sequelae.
Fig. 2.

MRI scan with visible screw threads and large bone cyst
Fig. 3.

Large pretibial cyst filled with contrast media
In two patients the screws had to be removed 16 and 20 months after the operation. The reason was intolerable pain on the mid-anterior aspect of the knee in the scar and implantation area. In the first case continuous effusion without any symptoms of infection was present. The symptoms worsened with any strenuous physical activity. Three months after reconstruction the cyst was palpable on the mid-anterior aspect of the knee, and over the next 3 months a large Baker cyst appeared. The patient was given two courses of steroids to the joint. This procedure diminished symptoms for 4–6 weeks. Finally, 16 months after the operation the bioabsorbable screw was easily unscrewed and the Baker cyst excised. The screw was undamaged at least to the naked eye and it was sent to the manufacturer for examination. All symptoms resolved within 4 weeks after removal (Fig. 4).
Fig. 4.
Undamaged screw before removal. Patient was lying prone during concomitant Baker cyst excision
In the second case 4 months after implantation a painful cyst in the mid-anterior aspect of the knee was palpable. Twenty months after the primary procedure, revision was carried out. The screw visible on the MRI broke while being unscrewed. It was removed together with a cyst that had formed around it. The initial size of the screw was 9 mm, and on the MRI scan the cyst was 16 mm in diameter (Fig. 5).
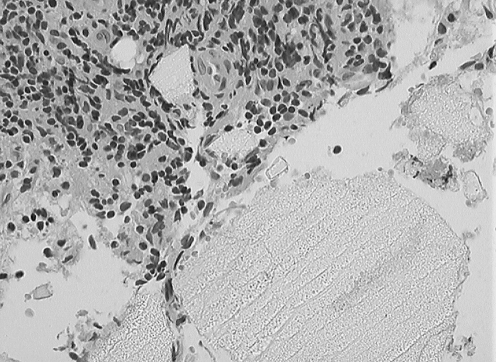
Fig. 5.
Fragment of the screw (porous structure) surrounded by inflammatory response tissue (H&E staining, ×20 magnification)
Two other patients in the study group complained of severe discomfort and pain in the screw area. The first refused revision surgery and was lost to follow up. The second one is postponing his revision procedure due to personal work problems. We did not observe breakage of any of the screws on MRI.
There was only one distal fixation screw removal in the control group 22 months after the operation due to skin irritation. The patient was a very thin person and the screw caused visible and palpable painful problems on the mid-anterior side of the knee. The remaining 21 patients did not develop any clinical symptoms despite mild pain during palpation over the screw head area.
Discussion
Bioabsorbable material in orthopaedic surgery was expected to overcome several disadvantages of metal devices. Inherent to metal screw fixation are the permanent nature causing complications during revision, stiffness, the potential to migrate, inflammatory and allergic reactions and the impossibility to perform clear MRI assessments [16]. After encouraging reports were published bioabsorbable screws gained wide acceptance in ACL surgery [7].
We did not find any important differences in clinical results between the distal fixation systems with regard to Lysholm-Gillquist, Marshall and KT-1000 assessments. Both post-screws and bioabsorbable screws assured good or very good clinical results in relation to knee stability. Both are easy to use and we did not find any important problems during insertion. These findings were in keeping with those of other authors [13, 21].
The high complication rate in the group of patients with bioabsorbable screws was quite surprising. Numerous complaints of pain and discomfort were noted. Even from the very beginning Barber reported some complications as follows: 7% broken screws and 1 in 42 cases of “unexpected anterior and medial knee pain” that required arthroscopy [4]. A critical attitude is presented by many others [13, 15].
The manufacturer claimed complete screw incorporation during the first year, and this was expected by the patients. Growing numbers of patient complaints, some severe in nature, emerged 4–6 months after surgery. These findings parallel those of another study by Ma [13]. The tunnel enlargement observed on MRI scans is a finding similar to other authors [13] and the aperture fixation advantage seems to be in doubt from that point of view.
Although initially considered to be a remedy for all problems with metal fixation devices, ultimately bioabsorbable interference screws seem to have only achieved limited success. Many reports concerning cyst formation, tunnel enlargement, inflammatory reactions and mechanical failures have been published [3, 19, 20, 22, 23]. Doubts still exist about whether PLLA degrades completely at all [16].
The higher number of graft ruptures in the control group, except for one case, might be related to the return to pivoting sport activity. On the other hand it may suggest biomechanically superior aperture fixation or preservation of the hamstring graft, despite local problems [4].
Conclusions
Bioscrews as a distal hamstring graft fixation device are similar to screw-post fixation with regard to clinical results and restored knee stability.
Many local complications may be encountered if one chooses a biodegradable screw for the distal fixation. Complete bioabsorption with no bone cyst formation is at least a slow process if it ever takes place at all.
The material of choice for distal graft fixation should be reconsidered.
Acknowledgements
Many thanks to Dr. Danuta Skomra, Department of Pathomorphology, Medical University of Lublin, for her help with the histopathology specimen preparation and interpretation and to Dr. Jacek Tabarkiewicz for statistical analysis.
Appendix
Table 1.
Mean gained points in Lysholm-Gillquist (L&G) and Marshall scale and average KT-1000 side-to side difference (millimeters)
| L&G preop | L&G final | L&G gained | Marshall preop | Marshall final | Marshall gained | KT-1000 | |
|---|---|---|---|---|---|---|---|
| Bioabsorbable screw (study group) | 55.4 | 94.46 | 38.9 | 33.33 | 46.15 | 12.89 | 2.46 |
| Screw-post (control group) | 59.4 | 92 | 32.93 | 33.4 | 44.5 | 11.47 | 2.5 |
References
- 1.Aglietti P, Giron F, Buzzi R, Biddau F, Sasso F. Anterior cruciate ligament reconstruction: bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. J Bone Joint Surg Am. 2004;86-A(10):2143–2155. [PubMed] [Google Scholar]
- 2.Ahmad CS, Gardner TR, Groh M, Arnouk J, Levine WN. Mechanical properties of soft tissue femoral fixation devices for anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(3):635–640. doi: 10.1177/0363546503261714. [DOI] [PubMed] [Google Scholar]
- 3.Asik M, Atalar AC. Failed resorption of bioabsorbable meniscus repair device. Knee Surg Sports Traumatol Arthrosc. 2002;10:300–304. doi: 10.1007/s00167-002-0310-2. [DOI] [PubMed] [Google Scholar]
- 4.Barber F, Elrod B, McGuire D, Paulos L. Preliminary results of an absorbable interference screw. Arthroscopy. 1995;11:573–588. doi: 10.1016/0749-8063(95)90129-9. [DOI] [PubMed] [Google Scholar]
- 5.Bostman OM. Osteolytic changes accompanying degradation of absorbable fracture fixation implants. J Bone Joint Surg Br. 1991;73-B:679–682. doi: 10.1302/0301-620X.73B4.1649195. [DOI] [PubMed] [Google Scholar]
- 6.Brand JC, Jr, Nyland J, Caborn DN, Johnson DL. Soft-tissue interference fixation: bioabsorbable screw versus metal screw. Arthroscopy. 2005;21(8):911–916. doi: 10.1016/j.arthro.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 7.Caborn DN, Coen M, Neef R, Hamilton D, Nyland J, Johnson DL. Quadrupled semitendinosus-gracilis autograft fixation in the femoral tunnel: a comparison between a metal and a bioabsorbable interference screw. Arthroscopy. 1998;14(3):241–245. doi: 10.1016/S0749-8063(98)70138-0. [DOI] [PubMed] [Google Scholar]
- 8.Ejerhed L, Kartus J, Sernert N, Köhler K, Karlsson J. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction? Am J Sports Med. 2003;31:19–25. doi: 10.1177/03635465030310011401. [DOI] [PubMed] [Google Scholar]
- 9.Gawęda K, Walawski J, Węgłowski R, Patyra M. Rehabilitation after one-stage anterior cruciate reconstruction and osteochondral grafting. Int Orthop. 2006;30(3):185–189. doi: 10.1007/s00264-005-0041-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herrington L, Wrapson C, Matthews M, Matthews H. Anterior cruciate ligament reconstruction, hamstring versus bone-patella tendon-bone grafts: a systematic literature review of outcome from surgery. Knee. 2005;12(1):41–50. doi: 10.1016/j.knee.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Kulkarni RK, Pani KC, Neuman C, et al. Polylactic acid for surgical implants. Arch Surg. 1966;93:839–843. doi: 10.1001/archsurg.1966.01330050143023. [DOI] [PubMed] [Google Scholar]
- 12.Lysholm J, Gillquist J. Evaluation of the knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10:150–154. doi: 10.1177/036354658201000306. [DOI] [PubMed] [Google Scholar]
- 13.Ma CB, Francis K, Towers J, Irrgang J, Fu FH, Harner CH. Hamstring anterior cruciate ligament reconstruction: a comparison of bioabsorbable interference screw and endobutton-post fixation. Arthroscopy. 2004;20:122–128. doi: 10.1016/j.arthro.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 14.Marshall J, Fetto J, Botero P. Knee ligament injuries: A standardized evaluation method. Clin Orthop. 1977;123:115–129. [PubMed] [Google Scholar]
- 15.Martinek V, Seil R, Lattermann C, Watkins SC, Fu FH. The fate of the poly-L-lactic acid interference screw after anterior cruciate ligament reconstruction. Arthroscopy. 2001;17(1):73–76. doi: 10.1053/jars.2001.7797. [DOI] [PubMed] [Google Scholar]
- 16.Maurus PB, Kaeding CCh. Bioabsorbable implant material review. Oper Tech Sports Med. 2004;12:158–160. doi: 10.1053/j.otsm.2004.07.015. [DOI] [Google Scholar]
- 17.Robbe R, Paletta GA., Jr Soft-tissue graft fixation in anterior cruciate ligament reconstruction. Oper Tech Sports Med. 2004;12:188–194. doi: 10.1053/j.otsm.2004.07.010. [DOI] [Google Scholar]
- 18.Rodeo SA, Arnoczky SP, Torzilli PA, Hidaka C, Warren RF. Tendon-healing in a bone tunnel. A biomechanical and histological study in the dog. J Bone Joint Surg. 1993;75A(12):1795–1803. doi: 10.2106/00004623-199312000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Sanchis-Alfonso V, Tinto-Pedrerol M. Femoral interference screw divergence after anterior cruciate ligament reconstruction provoking severe anterior knee pain. Arthroscopy. 2004;20(5):528–531. doi: 10.1016/j.arthro.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 20.Scioscia TN, Giffin JR, Allen CR, et al. Potential complication of bioabsorbable screw fixation for osteochondritis dissecans of the knee. Arthroscopy. 2001;17(12):E7. doi: 10.1053/jars.2001.17995. [DOI] [PubMed] [Google Scholar]
- 21.Seil R, Rupp S, Dienst M, et al. Chondral lesions after arthroscopic meniscus repair using meniscal arrows. Arthroscopy. 2000;16(7):E17. doi: 10.1053/jars.2000.9244. [DOI] [PubMed] [Google Scholar]
- 22.Seil R, Rupp S, Krauss PW, Benz A, Kohn DM. Comparison of initial fixation strength between biodegradable and metallic interference screws and a press-fit fixation technique in a porcine model. Am J Sports Med. 1998;26(6):815–819. doi: 10.1177/03635465980260061301. [DOI] [PubMed] [Google Scholar]
- 23.Shafer BL, Simonian PT. Broken poly-L-lactic acid interference screw after ligament reconstruction. Arthroscopy. 2002;18(7):E35. doi: 10.1053/jars.2002.32197. [DOI] [PubMed] [Google Scholar]
- 24.Shelbourne KD, Gray T. Anterior cruciate ligament reconstruction with autogenous patellar tendon graft followed by accelerated rehabilitation. A two- to nine-year follow-up. Am J Sports Med. 1997;25(6):786–795. doi: 10.1177/036354659702500610. [DOI] [PubMed] [Google Scholar]
- 25.St Pierre P, Olson EJ, Elliot JJ, O’Hair KC, McKinney LA, Ryan J. Tendon-healing to cortical bone compared with healing to a cancellous trough. A biomechanical and histological evaluation in goats. J Bone Joint Surg. 1995;77:1858–1866. doi: 10.2106/00004623-199512000-00010. [DOI] [PubMed] [Google Scholar]