Abstract
The problem of early mechanical stability of cemented and cementless keels of the tibial component in total knee arthroplasty (TKA) is controversial. The purpose of this study was to assess clinical and radiographic outcomes of a cohort of 51 TKAs using a cemented platform with cementless keel fixation. At a mean follow-up of 10.4 years (range, 7 to 14 years), the mean Knee Society Score (KSS) was 93 points (range, 59 to 100 points), and the mean functional score was 73 points (range, 0 to 100 points). Only one patient demonstrated progressive tibial radiolucencies at 13.1 years follow-up, which resolved with a revision with an exchange of components. The results of this study suggest that a proximally cemented tibial tray with a press-fit keel TKA provides excellent mean 10-year outcomes.
Résumé
Le problème de la stabilité précoce immédiate de la quille du composant tibial d’une prothèse totale du genou est sujet à controverse. Le propos de cette étude est d’étudier le devenir clinique et radiographique d’une cohorte de 51 prothèses totales du genou, avec un plateau cimenté sans fixation cimentée de la quille. Après un suivi moyen de 10,4 ans (de 7 à 14 ans), le score de la Knee Society a été de 93 points (59 à 100 points) et le score fonctionnel moyen de 73 points (de 0 à 100 points). Seulement un patient a présenté un liseré tibial progressif 13,1 ans après l’intervention avec une nécessité de révision et de changement prothétique. Le résultat de cette étude permet de penser qu’un plateau tibial cimenté avec une quille en press-fit permet d’obtenir de bons résultats avec au moins 10 ans de recul.
Introduction
There is controversy concerning the best techniques and prosthetic designs to ensure fixation and mechanical stability of the tibial component for total knee arthroplasty (TKA). Solid tibial tray fixation is crucial to avoid the risk of failure due to the high torque stresses at the bone–prosthesis interfaces. To date, the majority of TKAs in the United States are implanted using cemented tibial components [9, 19, 23]. However, there have also been some studies that have assessed the use of cementless tibial fixation [3, 10–12, 18]. Many of these cementless implant designs use additional devices, such as screws, pegs or keels, on the tibial component to improve fixation, and some designs allow for cementation of the tibial tray only while press-fitting the stem or keel of the tibial component.
The various design specifications for knee prostheses have evolved in an effort to provide patients with the best functional outcomes after TKA. Several factors may influence prosthetic survival, particularly in terms of aseptic loosening and wear. These include component alignment, fixation and load distribution [4, 5, 16, 20]. There is no consensus as to whether the use of cement around the tibial keel or post is the most advantageous technique for promoting these factors and subsequent long-term prosthetic survival [8, 15]. Proponents of cementing the entire tibia, including the keel or stem, argue that this technique provides better fixation and prevents aseptic loosening. Others authors believe that future revision will be made more difficult by metaphyseal cement if the tibial post, stem, fin or keel is cemented [4]. This study was undertaken because of the limited studies with divergent view points that have evaluated the clinical outcomes of patients who had TKAs which were performed using cemented tibial bone-plates with cementless keels or stems. The purpose of this study was to assess the 10-year results of total knee replacements that were performed using a proximally cemented tibial tray design and a cementless keel.
Materials and methods
We reviewed the clinical and radiographic outcomes of 51 consecutive knees (42 patients) that underwent TKA using a press-fit keel stem design with cementation of the tibial tray only. No keels or stems during this study period were cemented due to poor bone quality. Following institutional review board approval, all of the patient data was prospectively collected and entered into a database. Patients were included if they had a minimum of 7 years of final follow-up (mean 10 years, up to 14 years).
The pre-operative evaluation included the collection of demographic data, medical history, primary diagnosis, prior treatment of the affected joint and Knee Society Scores (KSS). The study cohort included 20 men and 22 women who had a mean body mass index (BMI) of 30.9 (range, 21.4 to 45.7). The patient mean age at the time of surgery was 74 years (range, 45 to 84 years). The underlying diagnosis was osteoarthritis in 50 knees and osteonecrosis in one knee. All procedures were performed using a posterior cruciate-retaining total knee (Series 7000, Stryker® , Mahwah, New Jersey).
Spinal anaesthesia, including intrathecal bupivacine and morphine, was used and intravenous cefazolin was administered for surgical prophylaxis. A midline incision was made and parapatellar arthrotomy was performed under tourniquet haemostasis. The tibia was prepared for the press-fit technique using a keel punch designed specifically for the press-fit technique. The knee system also had a separate punch that allowed for a 2-mm mantle of cement, though this was not used in this study. The keel of the tibial component was press-fitted into the proximal tibia and the baseplate was cemented onto the proximal tibial surface (Fig. 1). The femoral and all polyethylene patellar components were also cemented. The tourniquet was released after the wound was closed, and a dressing and compression stocking were then applied. The mean operating time was 68 min (range, 41 to 140 min). There were no surgical complications. Post-operatively, patients were allowed immediate, full weight-bearing activities. A standardised physical therapy program was begun on the first post-operative day, but no continuous passive motion machine was used.
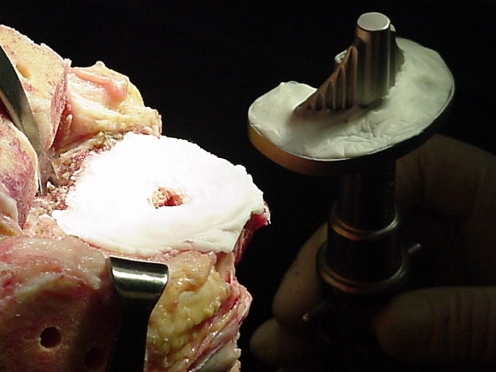
Fig. 1.
Intraoperative picture demonstrating the surgical technique. The tibial tray is cemented in place with a minimum cement mantle of 2 mm and the keel is inserted in a press-fit manner
The post-operative clinical assessment included the evaluation of pain and function using the Knee Society’s objective rating system. Evaluations were done at annual or biannual intervals. Post-operative scores were assigned based on each patient’s clinical status at the time of the latest follow-up.
Routine X-rays, including standing anteroposterior and lateral, were done at each follow-up. A zonal analysis was performed to assess for the presence of progressive radiolucent lines. Lucent lines were assigned to zones using recommended Knee Society guidelines by width and location, and the lines were noted to be progressive or stable. Pre- and post-operative mechanical alignments were examined and recorded using full-length mechanical axis radiographs of the operative extremity.
A Kaplan-Meier survival analysis was performed using either aseptic loosening requiring revision or definitive radiographic evidence of loosening as the endpoint. All data were subjected to averaging and analysis using the SPSS version 13.0 software package (SPSS Inc., Chicago, Illinois).
Results
Overall, the mean KSS improved from 44 points (range, 23–70 points) pre-operatively to 93 points (range, 59–100 points) at a mean follow-up of 10.4 years (range, 7 to 14 years). The functional scores showed similar improvements. There were no manipulations under anaesthesia, infections, extensor mechanism problems or neurovascular complications.
The post-operative prosthetic alignment averaged less than 1° of deviation from the mechanical axis. For those patients with valgus deformity, the mean mechanical valgus was measured at 3.86°. Following TKA, the mean mechanical valgus decreased to 0.92°. For those patients with varus deformity, the mean mechanical varus prior to surgery was 7.07°, which decreased to 0.76° post-operatively.
Radiographic analysis revealed that 31 knees (61%) had no radiolucent lines (Fig. 2). Of the 20 knees (39%) that had one or more radiolucent line, only one patient showed signs of progression. This patient required a revision TKA of the tibial component at 13.1 years. Table 1 provides a complete analysis of the number and zones of the radiolucent lines.
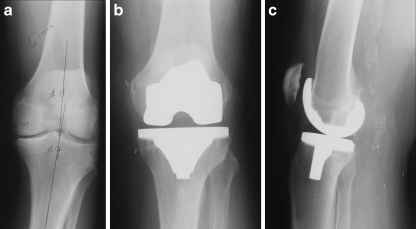
Fig. 2.
An 83-year-old man. a Preoperative anteroposterior view. Thirteen-year follow-up b Anterior/posterior and c lateral views of the left knee
Table 1.
Number and zones of radiolucent lines
| Radiolucent lines | Medial | Lateral | Anterior | Posterior |
|---|---|---|---|---|
| Present | 16 (80%) | 8 (40%) | 2 (10%) | 1 (5%) |
| Average size | 3 mm | 4 mm | 4 mm | 7 mm |
| Range | (1–6) | (2–6) | (3–5) |
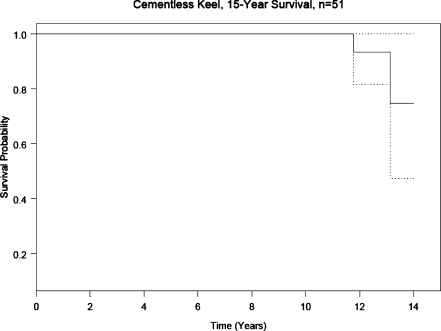
There was 100% survival at 10 years. Following this there were two revisions (one at 11.8 years and the previously reported one at 13.1 years). Revisions were done for a loose patella and extensive tibial component failure in one knee and tibial polyethylene wear in the other knee. In the worst case, survival probabilities at 2, 5 and 7 years were 100%, 100% and 96%, respectively. No deaths were reported during the follow-up period. Figure 3 shows the Kaplan-Meier survival curves for both normal and worst cases.
Fig. 3.
Fifteen-year Kaplan-Meier survival curves for both normal and worst cases
Discussion
Aseptic loosening of tibial components due to degradation of the interface between the bone cement and the metallic tibial shaft remains a persistent problem. The cementation of components in TKA has important clinical significance in revision and the avoidance of stress shielding. The findings of our study demonstrate excellent 10-year clinical results using a hybrid fixation technique with a proximally cemented tibial tray (minimum 2-mm cement mantle) and a cementless press-fit tibial keel design.
Cement versus cementless fixation for TKA continues to be a topic of debate and has received much attention in the literature [2, 4, 6, 13]. However, little data exists concerning the issue of cement or cementless keel/stem fixation in association with cemented tibial tray fixation. Many factors affect the stability of the tibial component, and different designs may have substantially differing degrees of stability, regardless of cement fixation [1, 6, 7, 11, 14, 22, 25]. Several clinical studies have addressed these issues with conflicting results. In a study using a keel design tibial component (Advantim Knee®; Wright Medical Technology, Arlington, Tennessee) in bone models, Bert and McShane [4] demonstrated increased micro-motion with a cementless keel and a 1-mm proximal cement mantle versus cemented keels. However, no significant differences in micro-motion were noted between cemented and cementless keel fixation if the proximal cemented mantle was increased to 3 mm.
Peters et al. [19] compared the full versus surface cement techniques for initial tibial component fixation in a cadaveric model . They found no difference between these modes of fixation using either an I-beam or cruciate type base plate, regardless of whether a full or surface cement technique was used. The researchers achieved an average of 3.6 mm of cement penetration into the tibial surface, with no significant differences between the surface or full cement techniques. The investigators concluded that there was no difference in initial fixation between the surface cement technique and the full cement technique with these two designs. However, their study only ran to 6,000 cycles [19]. Clinical failures with the surface cement technique have taken 2 to 3 years, which is greater than a million cycles.
In a randomised study using either a cemented or cementless tibial post, Sekundiak [21] found a statistically significant higher early failure rate, with debonding at the cement prosthesis interface, using the cementless technique. Sekundiak’s report revealed a lack of radiographic findings in these failures because the bone–cement interface was well maintained. Wall and Branson [24] reported excellent mid-term survival using a press-fit tibial keel and a cemented tray. The average proximal cement mantle was 2.9 mm and the authors reported a failure rate of <0.1% at an average of 75 months. Naima et al. [17] reported no tibial loosening in a group of 207 knees at 10 years using cementless stems and cemented tibial trays. However, they also reported 11 tibial revisions due to osteolysis and asserted that this was caused by increased polyethylene wear from loosening of the femoral component. Mikulak et al. [15], in a prospective study of bilateral total knee replacements, using the same tibial design and hybrid technique as in the current study, demonstrated a nearly 10% tibial loosening rate at an average of 22 months. The authors recommended cementing the keel in all primary total knee replacements. This is quite different from our current study, which demonstrates excellent 10-year clinical and radiographic results (98% survival) using a proximally cemented tibial tray with a press-fit tibial keel design. Comparison studies of cementless TKA are summarised in Table 2.
Table 2.
Comparison of the results of the current study with the literature concerning cementless total knee arthroplasty (TKA)
| Author | Year | Prosthesis component | Number of knees | Follow-up (years) | Revision rate (% knee) | Survival |
|---|---|---|---|---|---|---|
| Whiteside et al. | 1994 | Ortholoc I | 163 | 9 to 11 | 6.7 | 94 at y 10 |
| Fanning et al. | 1996 | NA | 42 | 5 to 7 | 45 | NA |
| Baldwin et al. | 1996 | NA | 109 | 2 to 5 | 0.9 | NA |
| Krugluger et al. | 1998 | Miller-Galante | 61 | 6.2 | 19 | NA |
| Duffy et al. | 1998 | Press-fit condylar | 55 | 10 | 18.1 | 72 |
| Sorrrells et al. | 2004 | Low contact stress | 528 | 5 to 12 | 5.5 | 89.5 |
| Ali et al. | 2006 | Low contact stress | 109 | 4 to 12 | 0.9 | 99.1 at y 10 |
| Hardeman et al. | 2006 | Profix total knee system | 115 | 8 to 10 | 1.7 | 97.1 at y 10 |
| Current study | 2007 | Posterior cruciate-retaining total knee system | 51 | 10 | 0.04 | 100 |
One of the limitations of the study is that this was an older and less active patient population who had a mean age of 74 years. A younger, more active patient population might make this technique a less favourable option. Also, a randomised trial of this design comparing cemented versus cementless keels for tibial fixation has not been performed. These results may differ based on the implant design. Despite these limitations, the authors found that this approach was bone-conserving, which would limit bone loss in the case of revision, and the excellent results of this study suggests that this technique is a viable TKA option.
The results of the study must be interpreted specifically for the Series 7000, Stryker® TKR as these outcomes may not apply to other TKA prosthetic designs. Furthermore, it should be noted that there was excellent post-operative alignment in our study cohort, with a mean of less than 1° from the true mechanical axis. Patients with greater deviations may not fare as well as our cohort. Additional comparative studies should be carried out in order to effectively evaluate the efficacy of various designs of TKAs with a cementless keel and cemented tibial tray. This cohort will continue to be tracked to determine the further long-term survivorship of this technique with this design. The senior authors (FRK and MAM) continue to implant their primary knees with this technique.
Acknowledgement
Thanks to Colleen M. Kazmarek for her assistance with the manuscript preparation and editing. Thanks to Ken Davis for the statistical analysis. Thanks to Mark Kester and Michelle Lim for their constructive comments and suggestions.
Footnotes
Two of the authors (FRK and MAM) received financial support from Stryker Orthopaedics, Mahwah, New Jersey.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
The authors FRK and MAM contributed equally to this work.
References
- 1.Ali MS, Mangaleshkar SR. Uncemented rotating-platform total knee arthroplasty: a 4-year to 12-year follow-up. J Arthroplasty. 2006;21(1):80–84. doi: 10.1016/j.arth.2005.04.018. [DOI] [PubMed] [Google Scholar]
- 2.Bassett RW. Results of 1,000 performance knees: cementless versus cemented fixation. J Arthroplasty. 1998;13(4):409–413. doi: 10.1016/S0883-5403(98)90006-7. [DOI] [PubMed] [Google Scholar]
- 3.Berger RA, Lyon JH, Jacobs JJ, Barden RM, Berkson EM, Sheinkop MB, Rosenberg AG, Galante JO. Problems with cementless total knee arthroplasty at 11 years followup. Clin Orthop Relat Res. 2001;392:196–207. doi: 10.1097/00003086-200111000-00024. [DOI] [PubMed] [Google Scholar]
- 4.Bert JM, McShane M. Is it necessary to cement the tibial stem in cemented total knee arthroplasty? Clin Orthop Relat Res. 1998;356:73–78. doi: 10.1097/00003086-199811000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Dobzyniak M, Fehring TK, Odum S. Early failure in total hip arthroplasty. Clin Orthop Relat Res. 2006;447:76–78. doi: 10.1097/01.blo.0000203484.90711.52. [DOI] [PubMed] [Google Scholar]
- 6.Duffy GP, Berry DJ, Rand JA. Cement versus cementless fixation in total knee arthroplasty. Clin Orthop Relat Res. 1998;356:66–72. doi: 10.1097/00003086-199811000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Fanning JW, Joseph J, Jr, Kaufman EE. Follow up on uncemented total knee arthroplasty. Orthopedics. 1996;19(11):933–939. doi: 10.3928/0147-7447-19961101-06. [DOI] [PubMed] [Google Scholar]
- 8.Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M. Early failures in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:315–318. doi: 10.1097/00003086-200111000-00041. [DOI] [PubMed] [Google Scholar]
- 9.Font-Rodriguez DE, Scuderi GR, Insall JN. Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res. 1997;345:79–86. doi: 10.1097/00003086-199712000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg VM, Kraay M. The outcome of the cementless tibial component: a minimum 14-year clinical evaluation. Clin Orthop Relat Res. 2004;428:214–220. doi: 10.1097/01.blo.0000148572.95121.f0. [DOI] [PubMed] [Google Scholar]
- 11.Hardeman F, Vandenneucker H, Lauwe J, Bellemans J. Cementless total knee arthroplasty with Profix: a 8- to 10-year follow-up study. Knee. 2006;13(6):419–421. doi: 10.1016/j.knee.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 12.Hofmann AA, Heithoff SM, Camargo M. Cementless total knee arthroplasty in patients 50 years or younger. Clin Orthop Relat Res. 2004;404:102–107. doi: 10.1097/00003086-200211000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Khaw FM, Kirk LM, Morris RW, Gregg PJ. A randomised, controlled trial of cemented versus cementless press-fit condylar total knee replacement. Ten-year survival analysis. J Bone Joint Surg Br. 2002;84(5):658–666. doi: 10.1302/0301-620X.84B5.12692. [DOI] [PubMed] [Google Scholar]
- 14.Krugluger J, Steinwenter A, Knahr K. Uncemented Miller-Galante total knee replacement. The influence of alignment on clinical and radiological outcome in a 5 to 8-year follow-up. Int Orthop. 1998;22(4):230–233. doi: 10.1007/s002640050248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mikulak SA, Mahoney OM, Rosa MA, Schmalzried TP. Loosening and osteolysis with the press-fit condylar posterior-cruciate-substituting total knee replacement. J Bone Joint Surg Am. 2001;83(3):398–403. doi: 10.2106/00004623-200103000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Murase K, Crowninshield RD, Pedersen DR, Chang TS. An analysis of tibial component design in total knee arthroplasty. J Biomech. 1983;16(1):13–22. doi: 10.1016/0021-9290(83)90042-8. [DOI] [PubMed] [Google Scholar]
- 17.Naima VS, Smith S, Freeman MA (1997) Proximal cementing of the tibial component in total knee replacement. JBJS Br 79:106
- 18.Parker DA, Rorabeck CH, Bourne RB. Long-term followup of cementless versus hybrid fixation for total knee arthroplasty. Clin Orthop Relat Res. 2001;388:68–76. doi: 10.1097/00003086-200107000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Peters CL, Craig MA, Mohr RA, Bachus KN. Cementless total knee arthroplasty in patients 50 years or younger. Clin Orthop Relat Res. 2004;409:158–168. doi: 10.1097/01.blo.0000058638.94987.20. [DOI] [PubMed] [Google Scholar]
- 20.Reilly D, Walker PS, Ben-Dov M, Ewald FC. Effects of tibial components on load transfer in the upper tibia. Clin Orthop Relat Res. 1982;165:273–282. [PubMed] [Google Scholar]
- 21.Sekundiak T (2001) Tibial component cement technique for longevity of total knee arthroplasty. Annual Meeting of the American Academy of Orthopaedic Surgeons, San Francisco, CA
- 22.Sorrells RB, Voorhorst PE, Murphy JA, Bauschka MP, Greenwald AS. Uncemented rotating-platform total knee replacement: a five to twelve-year follow-up study. J Bone Joint Surg Am. 2004;86(10):2156–2162. [PubMed] [Google Scholar]
- 23.Vince KG, Insall JN. Long-term results of cemented total knee arthroplasty. Orthop Clin North Am. 1988;19(3):575–580. [PubMed] [Google Scholar]
- 24.Wall R, Goldstein W, Branson JJ (2001) Incidence of tibial loosening in cemented total knee arthroplasty when a keeled stem is press fit and not cemented. Annual Meeting of the American Academy of Orthopaedic Surgeons, San Francisco, CA
- 25.Whiteside LA. Cementless fixation in revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:140–148. doi: 10.1097/01.blo.0000218724.29344.89. [DOI] [PubMed] [Google Scholar]