Abstract
There is currently an increased interest in the use of electro surgery in arthroscopy. Since the introduction of the bipolar arthroscopic radiofrequency (RF) wand, it has started to replace the classic Bovie monopolar probe on the assumption that the new technology provides multifunctional devices, combining both tissue removal and haemostasis into one instrument. The more efficient tissue ablation and precise haemostasis achieved with these instruments should result in a significant reduction in the operative time and cost. We ran a prospective comparative randomised study to test this hypothesis. Forty patients underwent arthroscopic subacromial decompression, randomised into two groups. The group treated with bipolar RF was associated with an average operative time saving of 8 min (P < 0.0001) and an average cost saving of £83 (€111) per case (P < 0.003), compared to monopolar RF. Bipolar RF is the instrument of choice in arthroscopic shoulder surgery, as it saves time and money.
Résumé
L’utilisation du bistouri électrique en arthroscopie est d’un intérêt croissant. Depuis l’introduction du bistouri bipolaire radio-fréquence RF, il est nécessaire de remplacer la classique sonde monopolaire Bovie en se basant sur l’hypothèse que les nouvelles technologies permettent, avec les nouveaux matériels multi fonctions de combiner résections tissulaires et l’hémostase avec la même sonde. Une bonne hémostase et une bonne résection par bistouri électrique permettent d’avoir des résultats significatifs notamment en ce qui concerne la diminution du temps opératoire et des côuts. Matériel et méthode: nous avons réalisé une étude randomisée prospective pour tester cette hypothèses 40 patients ont bénéficié d’une décompression sous acromiale arthroscopique et ont été randomisés en deux groupes. Résultat, le groupe traité avec bistouri bipolaire radio-fréquence est associé à un gain opératoire de 8 minutes (P < 0,0001) et, à une diminution du coût de 83 £ (111 euros) par patient (P < 0,003) comparé au bistouri monopolaire. En conclusion, le bistouri électrique bipolaire radio-fréquence RF est l’instrument de choix dans la chirurgie arthroscopique et permet à la fois de gagner du temps et de diminuer les coûts.
Introduction
Arthroscopic subacromial decompression (ASD) is a well accepted and successful technique for the treatment of chronic impingement syndrome of the shoulder [2–4]. Resection of the coracoacromial ligament and debridement of all soft tissues on the under surface of the acromion and the bursa is the first step of this procedure. This is typically accomplished with the alternating use of a soft tissue shaver and the electrocautery device, which is often an inefficient and time-consuming component of the procedure [6].
New technique
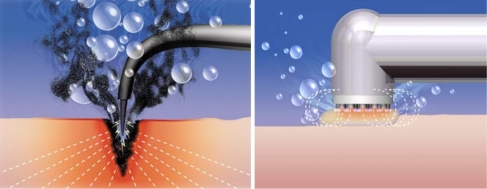
However, there are now multifunctional surgical devices that combine tissue removal and haemostasis into a single instrument; the bipolar radiofrequency (RF) devices introduced to clinical practice in 1998 [7]. In this series, we used the Coblation—plasma-mediated cold ablation—device which employs a novel bipolar surgical wand powered by enhanced RF energy. The Coblation method replaces the cellular pyrolysis and thermal cutting of standard monopolar electro surgery with a cool ablative process that produces molecular dissociation, cellular disintegration and volumetric tissue removal with little collateral soft-tissue damage [1]. Because the current does not pass directly through the tissue during the Coblation process, tissue heating is minimal (Fig. 1). The surface tissue temperature when using the Coblation device is usually between 40–70°C, compared to the standard electrocautery device, which could reach >400°C [1] (Table 1).
Fig. 1.
Difference in the mechanism of actions between monopolar versus bipolar radiofrequency (RF)
Table 1.
Difference between monopolar and bipolar radiofrequency (RF)
| Monopolar RF | Bipolar RF |
|---|---|
| Significant collateral damage | Minimal collateral damage |
| Surface tissue temperature >400°C | Surface tissue temperature 40–70°C |
| Rapid and deep tissue heating | Surface tissue heating |
| Tissue disintegration and pyrolysis | Volumetric tissue removal |
Mechanism of action
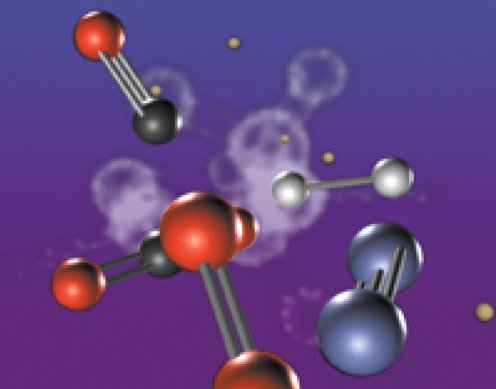
This is achieved by employing electro conductive fluid (e.g. isotonic saline) in the physical gap between the electrode and the tissues. Upon applying a sufficiently high voltage difference between these structures, the electrically conducting fluid is converted into an ionised vapour or plasma. As a result of the voltage gradient across the plasma layer, charged particles are accelerated towards the tissues. At a sufficiently high voltage gradient, the particles gain adequate energy and bombard tissue in their path, causing the molecular bonds simply to break apart [5] (Fig. 2).
Fig. 2.
Mechanism of action of the Coblation bipolar RF device
Materials and methods
This study prospectively randomised 40 patients undergoing ASD for chronic impingement syndrome between June 2004 and February 2005 into two groups, each consisting of 20 cases. One group was treated using the plasma-mediated ablation (Coblation) bipolar device and will be referred to as group C. The other group was treated using standard monopolar diathermy and a soft-tissue shaver, and will be referred to as group M. All patients were operated by the same surgeon, who is beyond the learning curve for this procedure. All patients had chronic impingement syndrome that had failed to respond to conservative treatment for 3 to 6 months in the form of non-steroidal anti-inflammatory drugs (NSAIDs), physiotherapy and at least one steroid injection in the subacromial space.
Randomisation
The 40 patients were randomised via numbers stored in four opaque envelopes, each containing a number from 1 to 10. The odd numbers were assigned to group M (monopolar RF) and the even numbers were assigned to group C (bipolar RF). On the day of surgery, a number was drawn from an envelope and the technique was carried out accordingly.
Operative technique
All patients had the procedure performed under general anaesthetic. The standard technique was carried out as described by Ellman [2]. We used the lateral decubitus position. The Coblation device was used in group C, while a monopolar diathermy probe and a soft-tissue shaver were used in group M. Normal saline was used in both groups as the irrigation fluid and all other equipment were standard for both groups, including the pump pressure.
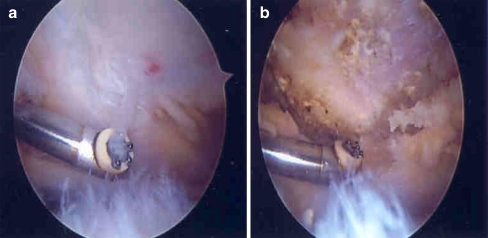
The procedure time was calculated after the routine glenohumeral arthroscopy, and the timing was started with the insertion of the camera in the subacromial space and finished with the end of complete decompression (Fig. 3a,b).
Fig. 3.
The Coblation probe in the subacromial space before (a) and after (b) the ablation of soft tissues from under the surface of the acromion
Statistical analysis
The mean and standard deviation were calculated, and unpaired two-sample Student’s t-test was used to analyse the operative time and cost differences between both groups. A P-value of less than 0.05 was considered to be significant.
Results
Operative time
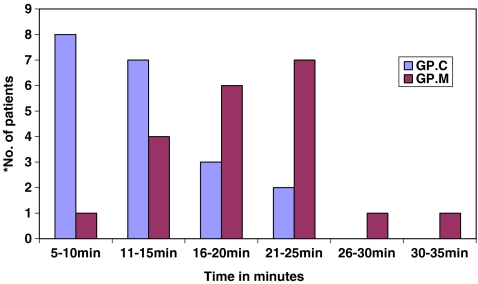
The average procedure time in the Coblation group was 13 minutes (5–25 min), compared with 21 min (10–35 min) for the monopolar RF group. There was an average of 8 min difference between both groups (P-value < 0.0001; Table 2 and Fig. 4).
Table 2.
Operative time and the number of patients in each group
| Operative time | No. of patients in group C | No. of patients in group M |
|---|---|---|
| 5–10 min | 8 | 1 |
| 11–15 min | 7 | 4 |
| 16–20 min | 3 | 6 |
| 21–25 min | 2 | 7 |
| 26–30 min | 0 | 1 |
| 30–35 min | 0 | 1 |
Group C=Coblation); group M=monopolar)
Fig. 4.
Operative time in group C (Coblation) and group M (monopolar)
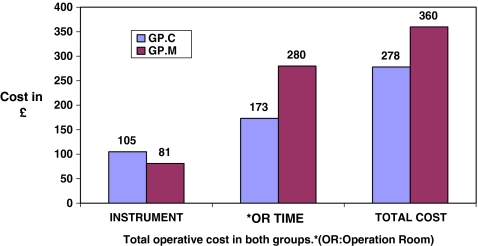
Cost difference
The cost of the Coblation wand is £105 (€141). The cost of the monopolar diathermy arthroscopic probe is £20 (€27). The cost of the soft-tissue shaver is £61 (€82). The last two items were both used for group M, so the total cost of the instruments for this group was £81 (€109) (Table 3).
Table 3.
The operative cost difference per case in each group
| Costs per case | Bipolar RF | Monopolar RF |
|---|---|---|
| Instruments | £105 (€140) | £81 (€108) |
| OR cost/min | £800 ÷ 60 × 13 = £173 (€232) | £800 ÷ 60 × 21 = £280 (€375) |
| Total costs | 105 + 173 = £278 (€373) | 81 + 280 = £361 (€484) |
| Cost difference | −£83 (€111) | +£83 (€111) |
| % of cost saving | −23% | +23% |
| % of time saving | −38% | +38% |
OR=operation room
The average total operating room cost at our institution—which includes personnel cost and other equipment—is approximately £800 (€1,072) per hour (60 min) of operating time. All other disposable materials were standardised for both groups.
A difference of 8 min in terms of money would equal 800 ÷ 60 (min) × 8 = £107 (€143), but as the cost difference of the instruments is £24 (€32) more for the Coblation group, so the final cost difference between both groups is 107−24 = £83 (€111) (P-value < 0.003; Fig. 5).
Fig. 5.
Operative cost for group C (Coblation) and group M (Monopolar)
Discussion
Coblation, a newly described method for soft-tissue ablation, uses plasma-mediated cold ablation to produce molecular dissociation that replaces the thermal tissue pyrolysis produced by the standard electro surgery tools.
The time saving associated with the use of the Coblation device was attributed to both the ablative efficiency and the simultaneous coagulation of the Coblation device. Secondly, the method avoids repeated instrument removal and reinsertion in group M patients, i.e. due to alternating use of the soft-tissue shaver and monopolar diathermy probe. Thirdly, due to difficulty in controlling the bleeding vessels and, consequently, difficult visualisation in some patients of group M.
If viewed in relation to the cost difference, there is an average saving of £83 (€111) per case in the Coblation group (P < 0.003). In this study, we restricted the evaluation of the time and cost to the component of the surgery dealing with subacromial decompression. However, in many cases of impingement syndrome, it is necessary to perform the Mumford procedure—excision of the lateral end of the clavicle. Because of the high vascularity of this tissue, bleeding is a frequent problem. The Coblation wand is well suited for this purpose because of its ability to establish haemostasis in both small and large blood vessels [7]. If the Coblation wand is used in this component of the procedure, additional time and cost savings could be added, with average savings of 8 min and £83 (€111), respectively, of the basic decompression procedure.
Very few papers in the orthopaedic literature have discussed the comparison between Coblation and standard electro surgical devices in arthroscopic subacromial decompression [7]. On the contrary, the orthopaedic literature is very rich in papers discussing the use of Coblation RF in arthroscopic surgery and the debridement of chondral flaps [8].
The benefits of Coblation are not just limited to those of time and cost. The technology enables the precise, well-controlled ablation of soft tissues that results in smoother, more anatomical surfaces than those produced by the conventional monopolar diathermy or mechanical shaver, while reducing the risk of thermal injury to the surrounding tissues. Clinically, these features should help to produce improved operative results, less postoperative pain and more rapid healing [7]. Also, the bipolar aspect of coblation eliminates the risk of electrical burns, which is one of the non-joint complications of conventional diathermy.
Conclusion
The use of the Coblation device for the soft-tissue resection and debridement in arthroscopic subacromial decompression reduces the procedure surgical time by 8 min, an average difference of 38% compared to the use of the shaver and the electro cautery diathermy probe. This can result in reducing the cost by £83 (€111), a difference of 23% per case based on common operating room and instruments costs. Coblation also is associated with a high level of ablative precision and control, the creation of smoother anatomical surfaces and the prevention of thermal injury to surrounding tissues. This combination of clinical and economical factors makes Coblation technology an instrument of choice in arthroscopic subacromial decompression.
Acknowledgements
No benefits of any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Eggers PE, Thapliyal HV, Matthew LS. Coblation: a newly described method for soft tissue surgery. Res Outcomes Arthrosc Surg. 1997;2(1):1–4. [Google Scholar]
- 2.Ellman H. Arthroscopic subacromial decompression: analysis of one- to three-year results. Arthroscopy. 1987;3:173–181. doi: 10.1016/s0749-8063(87)80061-0. [DOI] [PubMed] [Google Scholar]
- 3.Paulos LE, Harner CD, Parker RD. Arthroscopic subacromial decompressions for impingement syndrome of the shoulder. Tech Orthop. 1988;3(1):33–39. [Google Scholar]
- 4.Sampson TG, Nisbet JK, Glick JM. Precision acromioplasty in arthroscopic subacromial decompression of the shoulder. Arthroscopy. 1991;7:301–307. doi: 10.1016/0749-8063(91)90132-H. [DOI] [PubMed] [Google Scholar]
- 5.Sergeev VN, Belov SV. Coblation Technology: a new method for high-frequency electrosurgery. Biomed Eng. 2003;37(1):22–25. doi: 10.1023/A:1023729611717. [DOI] [PubMed] [Google Scholar]
- 6.Snyder SJ. Shoulder arthroscopy. New York: McGraw-Hill; 1993. pp. 150–152. [Google Scholar]
- 7.Stetson WB. Time and cost savings of coblation technology in subacromial decompression. Res Outcomes Arthrosc Surg. 1999;3(2):32–35. [Google Scholar]
- 8.Tasto JP, Ash SA. Current uses of radiofrequency in arthroscopic knee surgery. Am J Knee Surg. 1999;12(3):186–191. [PubMed] [Google Scholar]