Abstract
The Wagner cone prosthesis is indicated in uncemented total hip replacement of cases with cylinder-shaped femurs, deformed femurs, femurs with increased antetorsion, and in conditions of intramedullary bony scar tissue after previous osteotomies. The objective of this study is to present long-term results. From January 1, 1993 to December 31, 1995, 132 implantations were made with the Wagner cone prosthesis. We report the clinical and radiographic results of 94 cone prostheses with a mean observation period of 11.5 years. The Merle d’Aubigné score improved from a preoperative mean value of 8.8 to a postoperative mean of 16.3. The radiographic evaluation revealed 32 cases with cortical hypertrophy, 73 cases with atrophy of the proximal femur, and 18 cases with complete pedestal formation. Radiolucencies over Gruen zones 1 and 7 occurred in 42 cases; only zone 1 was affected in 24 cases. Complications included three deep infections, three acetabular revisions, five total joint revisions, one recurrent luxation, and three heterotopic ossifications. In spite of the fact that the examined cohort often included patients who had undergone multiple previous operations (a maximum of six) of the proximal femur or the acetabulum, the long-term results of the Wagner cone prostheses were very promising.
Résumé
Un cône fémoral de type Wagner est indiqué pour la réalisation de prothèses sans ciment pour les fémurs cylindriques déformés avec une augmentation de l’antéversion ou après ostéotomie. Le but de cette étude est d’en évaluer les résultats à long terme. Du 1er janvier 1993 au 31 décembre 1995, 132 implantations de ce type de prothèses ont été réalisées. Nous rapportons les résultats cliniques et radiographiques de 94 prothèses avec un suivi moyen de 11,5 ans. Le score de Merle d’Aubigné a été amélioré de 8,8 en préopératoire à 16,3 en post-opératoire. L’évaluation radiographique montre 32 cas d’hyperthrophie corticale, 73 cas d’atrophie du fémur proximal et 18 cas d’ossification en bout de queue. Des liserés dans les zones de Gruen 1 à 7 ont été observés dans 42 cas avec une atteinte isolée en zone 1 dans 24 cas. Les complications sont les suivantes : 3 infections profondes, 3 reprises acétabulaires, 5 reprises de prothèse, 1 luxation récidivante et 3 ossifications hétérotopiques. Du fait que ce groupe de patients incluait un nombre important de patients ayant bénéficié d’interventions chirurgicales antérieures à la prothèse (de 1 à 6) on peut considérer que les résultats à long terme de cette prothèse sont prometteurs.
Introduction
Total hip replacement in patients with dysplastic coxarthrosis is a challenge. On the one hand, hypoplasia of the acetabulum often requires reconstruction with bone grafts and osteosynthesis by means of an augmentation device, and on the other hand, dysplastic hips involve a pathological antetorsion of the proximal—often small—femur [13, 17]. Furthermore, by the time a total hip replacement is undertaken in order to treat the dysplastic coxarthrosis, frequently several operations in the proximity of the hip joint have already been undertaken, i.e. corrective surgery of the acetabulum or corrective osteotomies of the proximal femur, such as an intertrochanteric osteotomy, with ensuing bony scar tissue formation in the femoral canal. Today, thanks to their modular neck components [2, 6, 11, 12], modular stems allow continuous adjustment of the antetorsion, and thereby offer a possible solution to address these challenges. Implants with rectangular cross-section are available in smaller sizes [16] to treat cases of dysplastic coxarthrosis. However, a rectangular cross-section does not always achieve an anatomical reconstruction of the correct antetorsion. In 2004, Perka published a surgical technique [15], which enabled the implantation of a Zweymüller prosthesis with its known rectangular cross-section in patients with a dysplastic coxarthrosis by means of a three-dimensional, subtrochanteric, derotational, and—if necessary—a corrective shortening osteotomy.
In the 1990s, when the Wagner revision stem, with its outstanding rotational stability [1, 7, 18], achieved excellent results not only in revision arthroplasty, but also in primary joint replacement, the development of the cone prosthesis was a logical consequence. The Wagner cone prosthesis has a tapered configuration with a taper angle of 5° and is equipped with sharp longitudinal ribs, which ensure a high degree of rotational stability and good osseointegration. The implant is made from TiAl6Nb7 alloy and is rough-blasted with corundum. Indications for the cone prosthesis are femurs with a slim, rather cylindrical configuration, such as in dislocation or dysplastic coxarthrosis, congenital coxa vara, deformation and intramedullary bony scarring of the proximal end of the femur after previous osteotomies, fractures or growth disturbances, and congenital deformities. With the awls, the medullary canal can be prepared in relatively simple steps and without risk [19] compared to conventional rasps. Characteristic of the cone prosthesis is the pronounced proximal, “continuous” transmission of load, which gradually diminishes towards the metaphysis. Initial studies document excellent short- and medium-term results of the cone prosthesis, particularly in cases of dysplastic coxarthrosis [3, 9, 17, 19]. The objective of this study is to report, for the first time, the long-term results of the Wagner cone prosthesis.
Materials and method
From January 1, 1993 to December 31, 1995, 98 patients were operated upon by the designer, Professor Heinz Wagner and received 132 total hip replacements involving the cone prosthesis. Of this patient population, six patients died and another five could not be contacted for follow-up examinations. After an average follow-up time of 11.5 years (range: 10–14 years), 94 cases (87 patients) were available for clinical and radiographic analysis.
The mean age of the patients was 50.3 years (range: 16–70 years), mean height 164.7 cm (range: 148–185 cm), and mean weight 67.9 kg (range: 46–105 kg).
Sixty-four cases were treated with a Wagner revision cup, 15 cases with an uncemented Wagner primary cup, and three cases with an uncemented Wagner standard cup. Another 12 cases required an acetabular reconstruction with an augmentation device.
In 44 cases, a polyethylene/ceramic articulation was inserted, in 38 cases a metal/metal articulation, and in 12 cases a polyethylene/metal articulation.
Twenty-eight cases were operated upon by means of a anterior approach while 66 were posterior. The indication for total hip replacement was primary coxarthrosis in 18 cases, dysplastic coxarthrosis in 69 cases, infected destructive coxarthrosis in two cases, necrosis of the femoral head in two cases, and femoral neck fracture in three cases (Figs. 1, 2 and 3).
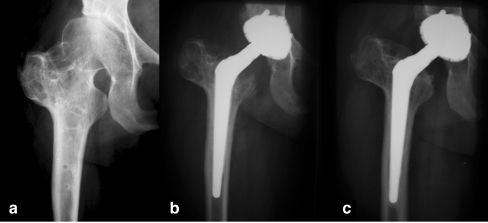
Fig. 1.
a The a/p X-ray of the right hip of a 44-year-old female patient shows an advanced dysplastic coxarthrosis following a corrective intertrochanteric osteotomy and displacement of the greater trochanter. b The a/p X-ray one week after total hip replacement documents the treatment with a Wagner Cone prosthesis and primary cup. c On the a/p X-ray at 11 years p/o, cup and stem are stable and osseointegrated. There are no lucent lines; however, there is an indication of distal socket formation
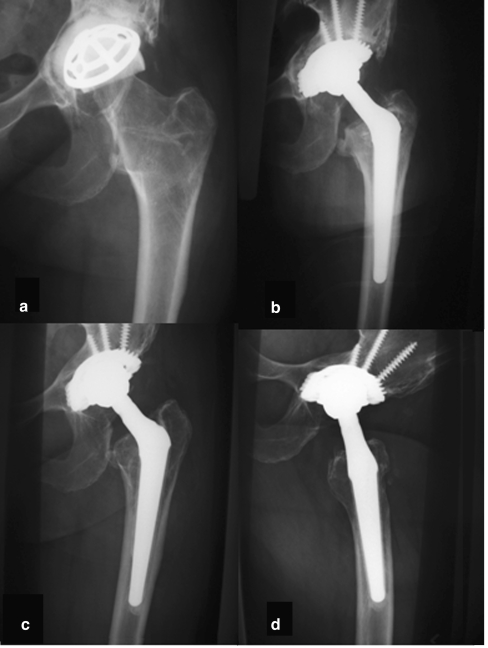
Fig. 2.
a The a/p X-ray of the left hip of a 49-year-old female patient exhibits pronounced loosening of the Wagner resurfacing cup, with destruction of the acetabulum. b The X-ray exam one week after surgery shows the reconstruction of the acetabulum with autologous bone and implantation of a Wagner threaded cup and a cone prosthesis. After 14 years in situ, the cup and the stem are stable and osseointegrated as shown in the a/p view (c), and lateral X-ray (d). There are no lucent lines; however, a socket formation, which indicates distal transmission of load, can be noted
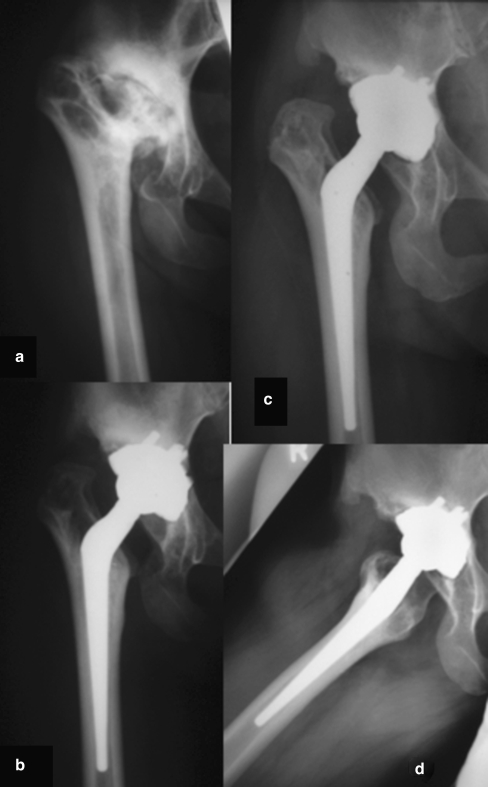
Fig. 3.
a The a/p X-ray of the right hip of a 33-year-old female patient indicates an advanced dysplastic coxarthrosis. b The a/p X-ray one week after total hip replacement shows the treatment with a Wagner cone prosthesis and a primary cup. After 13 years, cup and stem are stable and osseointegrated as shown in the a/p view (c), as well as on the lateral X-ray (d). There are lucent lines in DeLee zone III and in the area of the prosthetic shoulder
Previous operations included nine pelvic osteotomies, 33 corrective intertrochanteric osteotomies, ten resurfacing implants and eight trochanter displacements.
Thrombo-embolic prophylaxis during the period of treatment at the hospital included low-molecular Heparin medication and stockings for thrombo-prophylaxis. For the duration of 12 weeks, partial weightbearing of 20 kg, with the help of a pair of forearm crutches, was prescribed.
At both three and twelve months after surgery, the patients underwent a clinical and radiographic examination, and they were subsequently followed up at regular intervals once a year.
For the clinical assessment, the Merle d’Aubigné score was used. The radiographic analysis was done on the basis of standard a/p X-rays, as well as images in the Lauenstein position. Radiolucencies were assessed according to the Gruen scheme and heterotopic ossifications were classified according to Brooker.
Results
The Merle d’Aubigné score improved from a preoperative mean of 8.8 (range: 3–14) to a postoperative mean of 16.3 points (range: 7–18).
Nonprogressive radiolucent lines were found in Gruen zone 1 in 19 cases, in zone 7 in one case, in both zones 1 and 7 in 37 cases, in zones 1 and 2 in one case, in zones 1, 2 and 7 in 2 cases, in zones 1, 2, 6 and 7 in one case , and in zones 1, 6 and 7 in 3 cases.
In one case, stem subsidence of 2 mm with secondary stabilisation was observed. Distal cortical hypertrophy was seen in 32 cases, including 18 cases with pedestal formation around the distal tip of the prosthesis. All patients were free of pain and other symptoms.
Early postoperative complications included one case each of a temporary lesion of the nervus femoralis, the nervus cutaneus femoris lateralis, as well as a recurrent luxation.
Late postoperative complications were three deep infections following a condition of multiple corrective osteotomies (identified germs: 2× Staphylococcus aureus and 1× Escherichia coli). Due to pronounced granuloma formation around metal/metal articulations, three acetabular revisions were performed. Three revisions were necessary because of heterotopic ossifications (Brooker IV), which impeded joint function. Two stems were revised for periprosthetic fracture, and three total hip revisions were undertaken to treat aseptic loosening.
In this recent study, the survival rate of the cone prosthesis was 91.5% (86/94) after a mean follow-up of 11.5 years.
Discussion
Total joint replacement in cases of dysplastic coxarthrosis can pose a challenge. On the one hand, the acetabular roof is insufficient, or there is formation of a secondary socket. This makes an osteosynthesis reconstruction with acetabular augmentation devices necessary. On the other hand, a pathological, increased antetorsion of the proximal femur usually goes hand in hand with a dysplastic hip. Thus, it can be difficult to use standard implants with a rectangular cross-section in such a situation [15, 16]. Current studies favour, in the case of dysplastic coxarthrosis, the use of modular implants such as the S-ROM prosthesis, which enables a distal as well as a proximal anchorage, and which, by means of its “sleeve”, allows a continuous adjustment of the antetorsion [2, 6, 10–12]. Another possibility is the use of what is known as “custom-made prostheses” [12, 20]. In 1999, Zadeh [20] published the results of seven cases after an average of 31 months in which custom-made prostheses had been implanted in combination with a corrective subtrochanteric, derotational osteotomy to treat a pronounced femoral antetorsion. He obtained a good result in all cases; at the time of the last follow-up, the Harris hip score had improved from a preoperative 44 points to 91 points.
Several authors reported on the possibility of cemented stems in dysplastic osteoarthritis [5, 8, 14]. DiFazio [5] described the long-term results of a cemented femoral implant with swan-neck design in cases of dysplastic coxarthrosis. With its varus-shaped configuration, this implant attempts to reconstruct offset and leg length. In this small series, 14 of 15 cases were clinically and radiographically re-examined after a mean follow-up time of 13.4 years. In three cases, a localised femoral osteolysis was perceived. The survival rate in this very small series after a mean follow-up of 13 years was 94%.
Since patients presenting a dysplastic coxarthrosis usually require a prosthetic treatment at a younger age, we feel that a cemented joint replacement could prove problematic. On the one hand, chances that a revision will become necessary are very high, while on the other hand, uncemented stems are considered to be the optimum therapeutic treatment in young patients today [16].
For the treatment of pathological configurations of the proximal femur in patients with dysplastic coxarthrosis, there is, furthermore, the possibility to perform a corrective bone osteotomy within the framework of a total joint replacement [4, 15]. This is often necessary using an uncemented stem with a rectangular cross-section shape.
Perka described the results of his operations with the uncemented Zweymüller stem with a rectangular cross-section and distal anchorage properties [15]. The total patient population included in this study was 93 patients, i.e. 121 uncemented hip prostheses with a mean follow-up of 9.3 years. Only 17 of the cases analysed had an underlying dysplastic coxarthrosis Crowe grade IV. In 10 of the 17 cases, a derotational shortening osteotomy was performed. Another six patients underwent a femoral shortening osteotomy after a leg lengthening of more than 4 cm was discovered during preoperative planning. In ten cases, intraoperative complications were encountered, and in seven a fracture of the proximal femur was involved, which was treated with an appropriate cerclage. Perka attributes the high rate of femoral fractures to the increased antetorsion of the proximal femur and to the narrow intramedullary canal. However, this complication does not have a negative impact on the survival rate of the Zweymüller stem. Another complication following derotational osteotomy is pseudarthrosis, which has been reported recently [4].
Thus we prefer the use of a stem with a star-shaped, rounded cross-section, such as the Wagner cone prosthesis, which is a simple, time-saving and cost-efficient implant [3, 9, 17, 19].
Wagner et al. published the results of the first 100 cone prostheses implanted at their institution [19]. He reported six intraoperative fissures. At the last follow-up examination, a distal transmission of load with thickening of the femoral cortex could be distinguished. Subsidence of the cone prosthesis was observed in two cases; in one case, the subsidence was 2 mm with secondary stabilisation, and in the other case, the subsidence was 5 mm following septic loosening. In this study only one revision was necessary.
Analysing 60 Wagner cone prostheses, Kim [9] found only one case of a clinically irrelevant subsidence of the cone prosthesis with subsequent secondary stabilisation and concluded that the cone prosthesis should be the implant of choice for patients with a dysplastic coxarthrosis.
In this study we found comparable results with only one case of stem subsidence of 2 mm with secondary stabilisation. According to Strom [17] the mean subsidence of the cone prosthesis is 0.27 mm after 5 years. By means of X-ray stereometry analysis, he noted that the subsidence occurred primarily within the first 4 months following implantation.
To our knowledge, this study is the first to involve long-term results of the cone prothesis. The survival rate was 91.5% (86/94) after a mean follow-up of 11.5 years. There was no case of thigh pain. There were numerous previous operations before total hip replacement. Therefore, the survival rate should be discussed briefly.
After the first implantations of the cone prosthesis by Prof. Heinz Wagner, there was a certain euphoria, especially because of the absence of thigh pain. This led to the indication in the current study—in retrospect—being extended at times beyond its limits. It is important that the configuration of the femur establishes a tight contact with the mid-third portion of the prosthetic stem, and that not just the stem tip sits firmly in the medullary canal. In order to ensure this, a precise preoperative plan is necessary. On the planning template, the contour of the stem must overlap the inner contour of the cortex in the mid-third portion of the stem by 1 mm.
In spite of the fact that the examined patient population had often undergone multiple previous surgeries of the proximal femur or the cup, very good results of the Wagner cone prosthesis can be reported. In particular, a very reliable primary stability without subsidence was achieved in all cases but one. While the first implantations often yielded a diaphyseal anchorage, the change of the awls (with a proximal taper angle of 4° and a distal taper angle of 2°) permitted an improved adaptation of the prosthesis to the proximal medullary canal with a decreasing anchorage from the proximal to the distal stem. Further studies should attempt to prove that stricter indications will lead to even better results and better survival rates.
References
- 1.Böhm P, Bischel O. Femoral revision with the Wagner SL revision stem: evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J Bone Joint Surg Am. 2001;83-A:1023–1031. [PubMed] [Google Scholar]
- 2.Buly R. The S-ROM stem: versatility of stem/sleeve combinations and head options. Orthopedics. 2005;289(suppl):1025–1032. doi: 10.3928/0147-7447-20050902-04. [DOI] [PubMed] [Google Scholar]
- 3.Castelli CC, D’angelo F, Molina M, Ferrario A, Cherubino P. Radiographic evaluation of the “conus” uncemented stem. Hip Int. 1999;9:133–138. [Google Scholar]
- 4.Valle CJ, Berger RA, Rosenberg AG, Jacobs JJ, Sheinkop MB, Paprosky WG. Extended trochanteric osteotomy in complex primary total hip arthroplasty. A brief note. J Bone Joint Surg Am. 2003;85-A:2385–2390. doi: 10.2106/00004623-200312000-00017. [DOI] [PubMed] [Google Scholar]
- 5.DiFazio F, Shon WY, Salvati EA, Wilson PD., Jr Long-term results of total hip arthroplasty with a cemented custom-designed swan-neck femoral component for congenital dislocation or severe dysplasia: a follow-up note. J Bone Joint Surg Am. 2002;84-A:204–207. doi: 10.2106/00004623-200202000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Gacon G, Philippe MP, Ray A, Hummer J, Hourlier H, Dambreville A. Metaphyseal and diaphyseal modular femoral stems implanted without cement. Rev Chir Orthop Reparatrice Appar Mot. 2001;87:331–339. [PubMed] [Google Scholar]
- 7.Grunig R, Morscher E, Ochsner PE. Three-to 7-year results with the uncemented SL femoral revision prosthesis. Arch Orthop Trauma Surg. 1997;116:187–197. doi: 10.1007/BF00393708. [DOI] [PubMed] [Google Scholar]
- 8.Ito H, Matsuno T, Minami A, Aoki Y. Intermediate-term results after hybrid total hip arthroplasty for the treatment of dysplastic hips. J Bone Joint Surg Am. 2003;85-A:1725–1732. doi: 10.2106/00004623-200309000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Kim YY, Kim BJ, Ko HS, Sung YB, Kim SK, Shim JC. Total hip reconstruction in the anatomically distorted hip. Cemented versus hybrid total hip arthroplasty. Arch Orthop Trauma Surg. 1998;117:8–14. doi: 10.1007/BF00703431. [DOI] [PubMed] [Google Scholar]
- 10.Marega L. The management of version abnormalities and angular deformities in developmental dysplasia of the hip. Orthopedics. 2005;28(suppl):1097–1099. doi: 10.3928/0147-7447-20050902-19. [DOI] [PubMed] [Google Scholar]
- 11.Mattingly DA. The S-ROM modular femoral stem in dysplasia of the hip. Orthopedics. 2005;28(suppl):1069–1073. doi: 10.3928/0147-7447-20050902-14. [DOI] [PubMed] [Google Scholar]
- 12.McCarthy JC, Bono JV, O’Donnell PJ. Custom and modular components in primary total hip replacement. Clin Orthop Relat Res. 1997;344:162–171. doi: 10.1097/00003086-199711000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Noble PC, Kamaric E, Sugano N, Matsubara M, Harada Y, Ohzono K, Paravic V. Three-dimensional shape of the dysplastic femur: implications for THR. Clin Orthop Relat Res. 2003;417:27–40. [PubMed] [Google Scholar]
- 14.Papachristou G, Hatzigrigoris P, Panousis K, Plessas S, Sourlas J, Levidiotis C, Chronopoulos E. Total hip arthroplasty for developmental hip dysplasia. Int Orthop. 2005;14:1–5. doi: 10.1007/s00264-005-0027-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Perka C, Fischer U, Taylor WR, Matziolis G. Developmental hip dysplasia treated with total hip arthroplasty with a straight stem and a threaded cup. J Bone Joint Surg Am. 2004;86-A:312–319. doi: 10.2106/00004623-200402000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Schuh A, Ebert A, Holzwarth U, Zeiler G. Cementless Vektor-titan stem in total hip arthroplasty. Biomed Tech (Berl) 2005;50:30–34. doi: 10.1515/BMT.2005.006. [DOI] [PubMed] [Google Scholar]
- 17.Strom H, Mallmin H, Milbrink J, Petren-Mallmin M, Nivbrant B, Kolstad K. The cone hip stem: a prospective study of 13 patients followed for 5 years with RSA. Acta Orthop Scand. 2003;74:525–530. doi: 10.1080/00016470310017901. [DOI] [PubMed] [Google Scholar]
- 18.Wagner H, Wagner M. Femur revision prosthesis. Z Orthop Ihre Grenzgeb. 1993;131:574–577. doi: 10.1055/s-2008-1040074. [DOI] [PubMed] [Google Scholar]
- 19.Wagner H, Wagner M. Cone prosthesis for the hip joint. Arch Orthop Trauma Surg. 2000;120:88–95. doi: 10.1007/pl00021223. [DOI] [PubMed] [Google Scholar]
- 20.Zadeh HG, Hua J, Walker PS, Muirhead-Allwood SK. Uncemented total hip arthroplasty with subtrochanteric derotational osteotomy for severe femoral anteversion. J Arthroplasty. 1999;14:682–688. doi: 10.1016/S0883-5403(99)90223-1. [DOI] [PubMed] [Google Scholar]