Abstract
A preoperative quantitative evaluation of soft tissues is helpful for planning total knee arthroplasty, in addition to the conventional clinical examinations involved in moving the knee manually. We evaluated preoperative coronal laxity with osteoarthritis in patients undergoing total knee arthroplasty by applying a force of 150 N with an arthrometer. We examined a consecutive series of 120 knees in 102 patients. The median laxity was 0° in abduction and 8° in adduction. The femorotibial angle on non-weight-bearing standard anteroposterior radiographs was 180° and correlated with both abduction (r = −0.244, p = 0.007) and adduction (r = 0.205, p = 0.025) laxity. The results of a regression analysis suggested that the femorotibial angle is helpful for estimating both laxities. Considering the many reports on how to obtain well-balanced soft tissues, stress radiographs might help to improve the preoperative planning for gaining the optimal laxity deemed appropriate by surgeons.
Résumé
Une analyse avec évaluation quantitative préopératoire des tissus mous est nécessaire dans la planification d’une prothèse totale de genou, ceci en plus des examens cliniques conventionnels, notamment en ce qui concerne l’évaluation de la mobilité. Nous avons évalué, en préopératoire, les laxités ainsi que les stades de l’arthrose chez les patients qui ont bénéficié d’une prothèse totale du genou. Ces résultats ont été réalisés à l’arthromètre. Nous avons réalisé une série consécutive de 120 genoux chez 102 patients. La laxité moyenne était de 0° en abduction et de 8° en adduction. L’angle fémoro tibial, sans appui, sur les radiographies de face et de profil était de 180° et a été corrélé avec la laxité en abduction (r = −0.244, p = 0.007) et en adduction (r = 0.205, p = 0.025). Les résultats nous montrent que l’angle fémoro tibial est utile pour estimer les laxités. Si l’on considère les différentes études et la meilleure manière d’obtenir une bonne balance ligamentaire, les radiographies en stress permettent d’optimiser le planning opératoire et d’avoir une bonne idée des laxités.
Introduction
Preoperative planning for the hard and soft tissues in total knee arthroplasty is important for obtaining good long-term clinical results. Unlike bone deformities or defects, it is difficult to evaluate the soft tissue conditions from standard X-rays alone. Previous studies have tried to evaluate this using stress X-rays, but most involve standing views with the knee in some degree of flexion [2, 3, 16]. Frequently, studies do not evaluate the soft tissue conditions, but focus instead on the degree of osteoarthritis. Although several studies have examined how to correct varus or valgus deformities of contracted knees in cadavers or primary or revision total knee arthroplasty, few papers have discussed the preoperative soft tissue conditions [8, 13, 22–24]. Two recent papers reported that the most common reason for total knee arthroplasty revision within 5 years is symptomatic instability [4, 18]. Ridgeway and Moskal [15] stated that instability most commonly presents within the early postoperative period in mobile-bearing total knee arthroplasty. The preoperative soft tissue assessment is usually performed clinically, i.e. by manually placing stress on the knee to determine whether a deformity is fixed or correctable. Correctable deformities do not necessitate as much soft tissue release as a fixed deformity. Therefore, we quantified the preoperative soft tissue conditions in Japanese patients who underwent total knee arthroplasty by applying a force of 150 N with an arthrometer, which is believed to simulate dynamic conditions, such as walking and stair climbing [7, 14]. As a result, this may help surgeons to plan the surgical procedure in relation to soft tissues, as well as to bone.
Materials and methods
We evaluated 120 consecutive knees in 102 patients who underwent total knee arthroplasty. In all patients, the preoperative diagnosis was osteoarthritis. The clinical characteristics of the patients are summarised in Table 1. The degree of osteoarthritis was evaluated with the Kellgren and Lawrence radiographic grade[9] using the Rosenberg view [16] (weight-bearing), in which 0=normal I=possible osteophytic lipping, II=definite osteophytes and possible joint space narrowing, III=moderate/multiple osteophytes and definite joint space narrowing, some sclerosis and possible bony attrition, and IV=large osteophytes, marked joint space narrowing, severe sclerosis and definite bony attrition. We measured the tibiofemoral angle under a non-weight-bearing condition to clarify the relationship between alignment and knee joint laxity, and determined the angle resulting from the intersection of the femoral and tibial shaft axes.
Table 1.
Patient characteristics
| Parameter | |||
|---|---|---|---|
| Knees/patients | 120/108 | ||
| Gender: male/female | 5/115 | ||
| Mean age (range) | 72 (56–83) years | ||
| Mean flexion (SD) | 90° (15°) | ||
| HSS score* (SD) | 48 (23) | ||
| OA grade** | II: 1 | III: 30 | IV: 89 |
*The Hospital for Special Surgery score
**Osteoarthritis grade was evaluated using the Kellgren and Lawrence radiographic grade [9]
The laxity of abduction and adduction were measured with a Telos arthrometer (Fa Telos; Medizinisch-Technische Gerätebau GmbH, Sulzbach, Germany) with the patient lying on a table with the knee extended as much as possible. In the abduction/adduction stress test, a force of 150 N was applied just above the joint on the lateral (Fig. 1a) or medial (Fig. 2a) femoral condyle. The patella was facing forward to minimise the rotational effect. The patient was told to relax and standard radiographs were taken after the force had been applied for 1 min. To measure the abduction and adduction angles, the femoral boundary used was the distal convex margin of the condyles. The tibial boundary was the outer margin of the condyles. Thirty knees (15 healthy males; average age 28 years) with no complications affecting the activities of daily life were used as a control group (Figs. 1b and 2b). One observer (Y.M.) performed all of the tests. The intra-subject error was less than 1°. Informed consent, including a description of the protocol and the potential arthrometer-related complications, was obtained from all of the patients. The non-parametric Mann-Whitney U-test was used for the statistical analysis. Spearman’s correlations were calculated to determine the association between the tibiofemoral angle on standard radiographs and coronal joint laxity. The significance level was set at p<0.05.
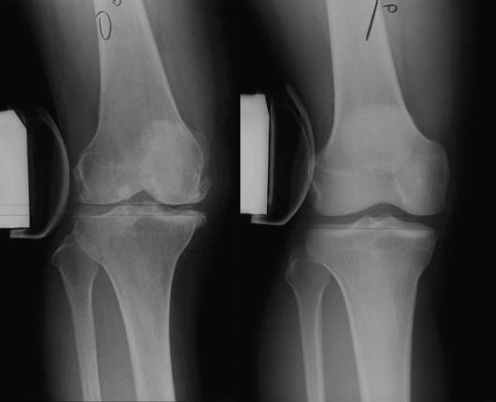
Fig. 1a, b.
Abduction (a osteoarthritis and b control) was measured with a Telos arthrometer at between 0° and 20° of flexion while applying a force of 150 N
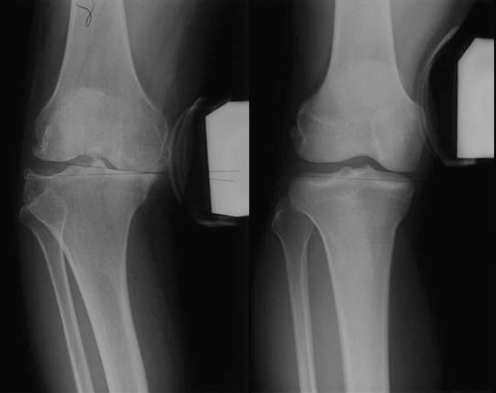
Fig. 2a, b.
Adduction (a osteoarthritis and b control) was measured with a Telos arthrometer at between 0° and 20° of flexion while applying a force of 150 N
Results
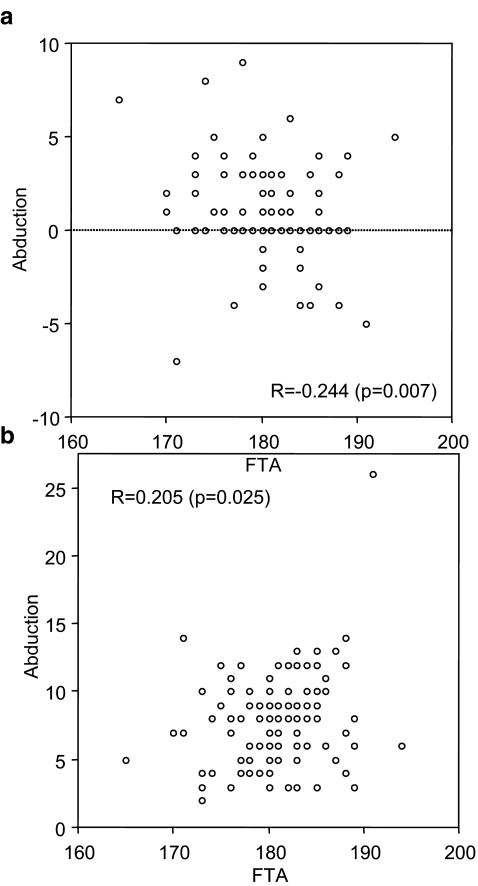
According to the Kellgren and Lawrence radiographic grade [9], we found 1, 30 and 89 grade II, III and IV knees, respectively (Table 1). The femorotibial angle (FTA) was 180° [179°, 184°], given as the median [25th percentile, 75th percentile], and was significantly related to the laxity in abduction (r = −0.244, p = 0.007; abduction=19.495−0.104FTA) (Fig. 3a) and adduction (r = 0.205, p = 0.025; adduction=−22.368+0.167FTA) (Fig. 3b). The laxity was 0° [0°, 2°] in abduction and 8° [6°, 9°] in adduction. Table 2 shows the distributions of the laxity in abduction and adduction. The normal controls had a laxity of 2° [0.25°, 3°] in abduction and 4° [3°, 4°] in adduction. The patient and control groups differed significantly in both abduction (p = 0.003) and adduction (p<0.0001).
Fig. 3a, b.
The relationship between the femorotibial angle (FTA) and preoperative (a) abduction laxity and (b) abduction laxity. A significant correlation was observed between the FTAand joint laxity
Table 2.
Magnitudes and distributions of abduction and adduction
| θ<−4° | −4°≤θ<0° | 0°≤θ≤4° | 4°<θ≤8° | 8°<θ≤12° | 12°<θ | |
|---|---|---|---|---|---|---|
| Abduction | 1 | 8 | 84 | 6 | 1 | |
| Adduction | 15 | 47 | 36 | 4 |
Discussion
It is important for the surgeon performing total knee replacement to form a preoperative plan to gain good long-term clinical results after surgery. The evaluation of hard tissues, such as bone or cartilage loss, osteophytes and bone cysts, is straightforward using only standard X-rays. However, it is difficult to evaluate the soft tissues correctly, such as the degree of contracture or attenuation, from only standard X-rays. Therefore, the preoperative information is usually obtained from standing X-rays, such as the Rosenberg [16], medial tibial plateau (MTP) [2] and Lyon Schuss [3, 24] radiographic views. However, the procedures are intended to evaluate the degree of osteoarthritis and not the soft tissue conditions. Moreover, they only simulate static conditions, and information on the soft tissue conditions, including dynamic conditions, is crucial for improving the preoperative planning. To our knowledge, this is the first study to focus on the quantitative preoperative joint laxity of patients undergoing total knee arthroplasty using an arthrometer, although many studies have evaluated the soft tissue laxity after total knee arthroplasty using this instrument [11, 12, 21].
Before total knee arthroplasty, the osteoarthritic knees had significantly greater laxity in adduction than normal. The main cause of this might have been the defects in the femoral and tibial medial condyles in the degenerative joints versus the control group. The geometry might have acted as a positive factor resulting in the greater adduction. Sharma et al. [19] reported that a loss of cartilage/bone height is associated with greater varus-valgus laxity in comparison to the laxity in healthy and osteoarthritic knees. Markolf et al. [10] also reported that condylar geometry is one of the factors providing knee stability in the loaded state.
However, although the amount of abduction was significantly smaller than in normal knees, the difference was only 2°. Two possible explanations exist. First, geometrically, the cartilage wear mainly affected the medial condyles of the femur and tibia, while the geometry of the lateral condyles was similar to that of the normal controls. Second, the medial soft tissue structures might have preserved this property in extension, although some deterioration, such as contraction with aging, was observed relative to the controls [5]. Harman et al. [6] reported a mechanism based on the amount and the location of articular cartilage wear on osteoarthritic tibial plateaus resected during total knee arthroplasty. Intact cruciate ligaments, acting with the preserved articular surfaces of the lateral compartment, together allow the medial femoral condyle to roll back in flexion, out of the anterior depression and onto the intact cartilage of the posterior plateau. Therefore, as the patient flexes the knee, the medial collateral ligament is stretched to its proper length.
Two recent papers have analysed the failure mechanism in patients who underwent revision surgery of their index arthroplasty [4, 18]. Sharkey et al. [18] reported that the primary causes of total knee arthroplasty failure were polyethylene wear (25%), aseptic loosening (24.2%), instability (21.2%), infection (17.5%), arthrofibrosis (14.6%), malalignment or malposition (11.8%), extensor mechanism deficiency (6.6%), avascular necrosis in the patella (4.2%), periprosthetic fracture (2.8%) and the resurfacing of an unsurfaced patella (0.9%) in their 212 cases. Fehring et al. [4] reported that 74 (27%) patients underwent revision surgery because of instability and 37 (13%) because of the failure of ingrowth of a porous-coated implant within the first 5 years after surgery. They concluded that the total number of early revisions would have decreased by approximately 40%, and the overall failures would have been reduced by 25%, if all of the arthroplasties in the patients in the early failure group were cemented routinely and balanced carefully. Since the surgical technique controls instability and component malalignment or malposition, the preoperative soft tissue evaluation is critical for the preoperative planning.
Several papers have reported on how to obtain or acquire well-balanced soft tissues in the knee joint quantitatively [8, 13, 22–24]. Matsueda et al. [13] reported a change in the coronal angle between 10 N·m varus and valgus moments in extension in vitro. The coronal angle increased from 0.9° with a 2-cm anterior sleeve release to 7.7° with an 8-cm anterior sleeve release of the medial collateral ligament (MCL). Whiteside et al. [23] reported that the release of the posterior oblique portion of the MCL in vitro caused an increase in valgus laxity in full extension (3.4°) and 30° of flexion (3.6°). Release of the anterior portion of the MCL resulted in approximately 4° of valgus laxity between full extension and 30° of flexion. Kanamiya et al. [8] used 17 knees from cadavers to evaluate stability at various degrees of flexion after total knee arthroplasty and re-evaluated the stability after releasing selected ligaments. The iliotibial band and posterior capsule were effective lateral stabilisers in full extension only. The lateral collateral ligament had a major stabilising effect throughout the arc from 0° to 90° of flexion. The popliteus tendon exerted its effect mostly from 60° to 90° of flexion. The posterolateral corner capsule was effective mostly at 0° to 30° of flexion. The iliotibial band had a significant stabilising effect from 0° to 30° of flexion. Considering these relationships, it might be much easier for surgeons to plan the amount of soft tissue release preoperatively using a standardised step-by-step medial or lateral release technique. A computer-assisted navigation surgery might be improved if information pertaining to the preoperative soft tissue conditions and the degree of soft tissue release were included, in addition to the optimal bone cutting, which is presently well established [1].
The femorotibial angle on non-weight-bearing standard anteroposterior radiographs was 180.8° [179°, 184°] and was correlated with both abduction and adduction laxity, although the correlations were weak. The regression analysis suggested that the value of the femorotibial angle might be helpful for estimating both adduction and abduction laxity postoperatively. Tew and Waugh [20] reported that the postoperative femorotibial angle reflected the clinical results. Yagishita et al. [25] revealed that the preoperative femorotibial angle affected the postoperative ligament balance after knee arthroplasty. In addition, Schurman et al. [17] found that a preoperative varus femorotibial angle of −6.5° was predictive of a lower postoperative range of motion. Our results suggest that the femorotibial angle is an accurate indicator for estimating both laxities preoperatively.
We recognise the limitations of this study. Measurements were made in knee extension due only to the characteristics of the arthrometer. We are well aware of the importance of evaluating laxity over the entire range of knee flexion and plan to determine the proper tension in the coronal direction. In addition, we have not clearly demonstrated the superiority of this quantitative approach over a simple physical examination, since various degrees of preoperative contracture due to peripheral osteophytes, which often make a large contribution to “fixed deformities,” are corrected once the standard bony cuts are made.
In summary, it is advantageous for surgeons to obtain the correct preoperative joint laxity under both static and dynamic conditions, since they could estimate the amount of soft tissue release preoperatively, in addition to the bone cuts to obtain the optimal bony alignment. Since a well-balanced knee after total knee arthroplasty is strongly correlated with good clinical results [12], the information from stress radiographs may help improve the preoperative planning to gain the optimal soft tissue laxity as deemed appropriate by the surgeon. It may be desirable for orthopaedic surgeons to take preoperative quantitative stress radiographs routinely in addition to the conventional manual assessment before total knee surgery.
References
- 1.Bolognesi M, Hofmann A. Computer navigation versus standard instrumentation for TKA: a single-surgeon experience. Clin Orthop Relat Res. 2005;440:162–169. doi: 10.1097/01.blo.0000186561.70566.95. [DOI] [PubMed] [Google Scholar]
- 2.Buckland-Wright JC, Wolfe F, Ward RJ, Flowers N, Hayne C. Substantial superiority of semiflexed (MTP) views in knee osteoarthritis: a comparative radiographic study, without fluoroscopy, of standing extended, semiflexed (MTP), and Schuss views. J Rheumatol. 1999;26:2664–2674. [PubMed] [Google Scholar]
- 3.Conrozier T, Favret H, Mathieu P, Piperno M, Provvedini D, Taccoen A, Colson F, Conrozier S, Vignon E. Influence of the quality of tibial plateau alignment on the reproducibility of computer joint space measurement from Lyon Schuss radiographic views of the knee in patients with knee osteoarthritis. Osteoarth Cartil. 2004;12:765–770. doi: 10.1016/j.joca.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 4.Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M. Early failures in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:315–318. doi: 10.1097/00003086-200111000-00041. [DOI] [PubMed] [Google Scholar]
- 5.Fishkin Z, Miller D, Ritter C, Ziv I. Changes in human knee ligament stiffness secondary to osteoarthritis. J Orthop Res. 2002;20:204–207. doi: 10.1016/S0736-0266(01)00087-0. [DOI] [PubMed] [Google Scholar]
- 6.Harman MK, Markovich GD, Banks SA, Hodge WA. Wear patterns on tibial plateaus from varus and valgus osteoarthritic knees. Clin Orthop Relat Res. 1998;352:149–158. [PubMed] [Google Scholar]
- 7.Harrington IJ. Static and dynamic loading patterns in knee joints with deformities. J Bone Joint Surg Am. 1983;65:247–259. doi: 10.2106/00004623-198365020-00016. [DOI] [PubMed] [Google Scholar]
- 8.Kanamiya T, Whiteside LA, Nakamura T, Mihalko WM, Steiger J, Naito M. Effect of selective lateral ligament release on stability in knee arthroplasty. Clin Orthop Relat Res. 2002;404:24–31. doi: 10.1097/00003086-200211000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Kellgren JH, Lawrence JS. Radiological assessment of osteoarthritis. Ann Rheum Dis. 1957;16:494–501. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Markolf KL, Bargar WL, Shoemaker SC, Amstutz HC. The role of joint load in knee stability. J Bone Joint Surg Am. 1981;63:570–585. [PubMed] [Google Scholar]
- 11.Matsuda M, Ishii Y. In vivo laxity of low contact stress mobile-bearing prostheses. Clin Orthop Relat Res. 2004;419:138–143. doi: 10.1097/00003086-200402000-00022. [DOI] [PubMed] [Google Scholar]
- 12.Matsuda Y, Ishii Y, Noguchi H, Ishii R. Varus-valgus balance and range of movement after total knee arthroplasty. J Bone Joint Surg Br. 2005;87:804–808. doi: 10.1302/0301-620X.87B6.15256. [DOI] [PubMed] [Google Scholar]
- 13.Matsueda M, Gengerke TR, Murphy M, Lew WD, Gustilo RB. Soft tissue release in total knee arthroplasty. Cadaver study using knees without deformities. Clin Orthop Relat Res. 1999;366:264–273. doi: 10.1097/00003086-199909000-00034. [DOI] [PubMed] [Google Scholar]
- 14.Morrison JB. The mechanics of the knee joint in relation to normal walking. J Biomech. 1970;3:51–61. doi: 10.1016/0021-9290(70)90050-3. [DOI] [PubMed] [Google Scholar]
- 15.Ridgeway S, Moskal JT. Early instability with mobile-bearing total knee arthroplasty: a series of 25 cases. J Arthroplasty. 2004;19:686–693. doi: 10.1016/j.arth.2003.12.079. [DOI] [PubMed] [Google Scholar]
- 16.Rosenberg TD, Paulos LE, Paker RD, Coward DB, Scott SM. The forty-five-degree posteroanterior flexion weight-bearing radiograph of the knee. J Bone Joint Surg Am. 1988;70:1479–1483. [PubMed] [Google Scholar]
- 17.Schurman DJ, Matityahu A, Goodman SB, Maloney W, Woolson S, Shi H, Bloch DA. Prediction of postoperative knee flexion in Insall-Burstein II total knee arthroplasty. Clin Orthop Relat Res. 1998;353:175–184. doi: 10.1097/00003086-199808000-00020. [DOI] [PubMed] [Google Scholar]
- 18.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Sharma L, Lou C, Felson TD, Dunlop DD, Kirwan-Mellis G, Hayes KW, Weinrach D, Buchanan TS. Laxity in healthy and osteoarthritic knees. Arthritis Rheum. 1999;42:861–870. doi: 10.1002/1529-0131(199905)42:5<861::AID-ANR4>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 20.Tew M, Waugh W. Tibiofemoral alignment and the results of knee replacement. J Bone Joint Surg Br. 1985;67:551–556. doi: 10.1302/0301-620X.67B4.4030849. [DOI] [PubMed] [Google Scholar]
- 21.Warren PJ, Olanlokun TK, Cobb AG, Walker PS, Iverson BF. Laxity and function in knee replacements. A comparative study of three prosthetic designs. Clin Orthop Relat Res. 1994;305:200–208. doi: 10.1097/00003086-199408000-00024. [DOI] [PubMed] [Google Scholar]
- 22.Whiteside LA. Selective ligament release in total knee arthroplasty of the knee in valgus. Clin Orthop Relat Res. 1999;367:130–140. doi: 10.1097/00003086-199910000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Whiteside LA, Saeki K, Mihalko WM. Functional medical ligament balancing in total knee arthroplasty. Clin Orthop. 2000;380:45–57. doi: 10.1097/00003086-200011000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Yagishita K, Muneta T, Ikeda H. Step-by-step measurements of soft tissue balancing during total knee arthroplasty for patients with varus knees. J Arthroplasty. 2003;18:313–320. doi: 10.1054/arth.2003.50088. [DOI] [PubMed] [Google Scholar]
- 25.Yagishita K, Muneta T, Yamamoto H, Shinomiya K. The relationship between postoperative ligament balance and preoperative varus deformity in total knee arthroplasty. Bull Hosp Joint Dis. 2001;60:23–28. [PubMed] [Google Scholar]