Abstract
We reviewed the results of 17 consecutive revision total hip arthroplasties performed with the use of freeze-dried irradiated bone allograft in 15 patients. These allografts were used in conjunction with five Kerboull rings, two steel meshes and ten cemented isolated cups. All the patients have had a follow-up of at least 5 years. The patients were evaluated clinically and radiographically. No revisions were necessary and X-rays confirmed partial or total ingrowth of the allografts. In acetabular revision surgery, hip reconstruction can be successfully treated by freeze-dried irradiated and chemically treated allografts. Additional studies with longer term follow-up are necessary to confirm this outcome.
Résumé
Nous avons revu les résultats de 17 reprises consécutives de prothèses totales de hanche réalisées chez 15 patients. Nous avons utilisé pour toutes ces reprises des allogreffes lyophilisées irradiées. Ces reprises ont été réalisées de la façon suivante: 5 avec anneaux de Kerboull, 2 avec fonds de cotyle grillagés et 10 cupules cimentées sur lit d’allogreffes. Tous les patients ont été revus avec un minimum de 5 ans et ont été évalués sur le plan clinique et radiographique. Aucune re-révision n’a été nécessaire. L’analyse radiographique a confirmé l’incorporation partielle ou totale de ces allogreffes. La chirurgie de reprise acétabulaire des prothèses totales de hanche, en utilisant ce type d’allogreffes lyophilisées irradiées et rendues inertes chimiquement nous a donné de bons résultats. Une étude à plus long terme sera nécessaire pour déterminer de façon précise le niveau d’incorporation de ces allogreffes et leur devenir.
Introduction
Frequency of revision hip arthroplasty has progressively increased in the last 25 years and it is expected to continue to increase between 2005 and 2030 [12]. During these revision procedures, acetabular bone deficiency is a major challenge. Irradiated allograft bone gives mechanical support for acetabular components in revision surgery. Few reports are available on the outcome of freeze-dried irradiated allograft in hip surgery beyond 5 years [2, 6, 10]. These bone grafts are in theory a good biological solution to reconstruct the bone stock loss. Their use seems to be correlated with a low risk of disease transmission. Since 1994, we have used freeze-dried irradiated and chemically treated allograft in revision acetabular hip arthroplasty. The purpose of this study was to determine the clinical and radiographic results of this technique after a follow-up of at least 5 years.
Materials and methods
Graft preparation
Freeze-dried irradiated bone grafts were subjected to a treatment which included a devitalisation, prions, viral inactivation and freeze drying before being treated by irradiation. Cortical bone was excised to allow a good solvent penetration. The solvents used according to an industrial protocol were ethanol, chloroform, hydrogen peroxide and sodium hypochlorite. Following this, the grafts were freeze dried by a technique similar to that used in the food preparation industry by a system that combines pressure and cold to eject the water molecules. Once the allografts were freeze dried, they were sterilised by gamma rays. The final graft was double packed and stored at ambient temperature within the operating theatre. The allograft bone was processed by TBF-Banque de Tissus (Phoenix® Mions France).
Patients
Between 1994 and 2001, 18 acetabular revisions using of freeze-dried irradiated allograft were performed at our institution by the same surgeon (J.C.). We selected only the patients who had revision of the acetabular implant with use of a freeze-dried irradiated allograft. All the patients had a minimal follow-up of 5 years. Acetabular revision also included isolated cemented cup or accessory implants such as Kerboull rings or steel meshes. The surgical approach initially used for all the patients was a posterior approach without trochanteric osteotomy. Pre- and post-operative clinical assessments were evaluated according to the criteria of Postel/Merle d’Aubigné [15] with scoring of pain, mobility of the hip and walking. Impaction bone-grafting technique with morselised allograft was used depending on the acetabular defect. Pre-operative radiological acetabular defects were assessed and classified by the AAOS system [3]. The patients were examined radiologically after 3 months, 1 year, 3 years and 5 years. We looked for complications with a particular interest in the specific complications of the implant: loosening of the socket, absence of stabilisation, loss and fractures of the allograft, radiographic aspect of the allograft and lucency of the defect margins. Radiological demarcation was evaluated according to De Lee and Charnley [4]. The Brooker classification was used for evaluation of heterotopic ossification [1].
Results
Between 1994 and 2000, 18 acetabular reconstructions with the use of freeze-dried irradiated allograft were done in 16 patients. One hip was lost because the patient could not be located. The remaining 17 hips (15 patients) have been followed clinically and radiographically for at least 5 years. There were ten women (66.6%) and five men (33.3%) with a mean age at surgery of 63 years (range, 50–80 years). One patient died more than 5 years after the revision. The indication for the revision hip arthroplasty was aseptic loosening of the acetabular component in 13 hips and polyethylene wear for 4 hips. The average age at the time of the first operation was 55 years. The mean follow-up was 7.8 years (range, 5–11 years). The pre-operative Merle d’Aubigné/Postel score was 10.3 (5–18). At 3 months, this score was 15.2 (12–18). At 1 year, it was 16.2 (15–18), and at 5 years it was 17.2 (16–18). The pre-operative acetabular radiological defects were classified according to the AAOS classification as type I (n=5), type II (n=5) and type III (n=7). We used five Kerboull rings, two steel meshes and ten cemented isolated allografts. We recorded one early dislocation without further revision (in recovery room), one haematoma requiring a surgical procedure and two venous thromboses without pulmonary embolism that resolved under treatment. Two patients had moderate peri-acetabular ossifications classified Brooker I. No hip required further revision of the acetabular component after our surgical procedure at the last follow-up. We observed a rupture of one Kerboull ring, without instability of the implant (Fig. 1). Radiographic evaluation after 5 years (as defined by DeLee and Charnley) shows that allografts were replaced by new bone formation with a trabecular structure of the bone for six hips, ten hips have a radiological demarcation <2 mm diameter at the defect margins without instability of the implant, and a patient has a marginal lucency type I of approximately 5 mm around the implant without clinical symptomatology (Fig. 2).
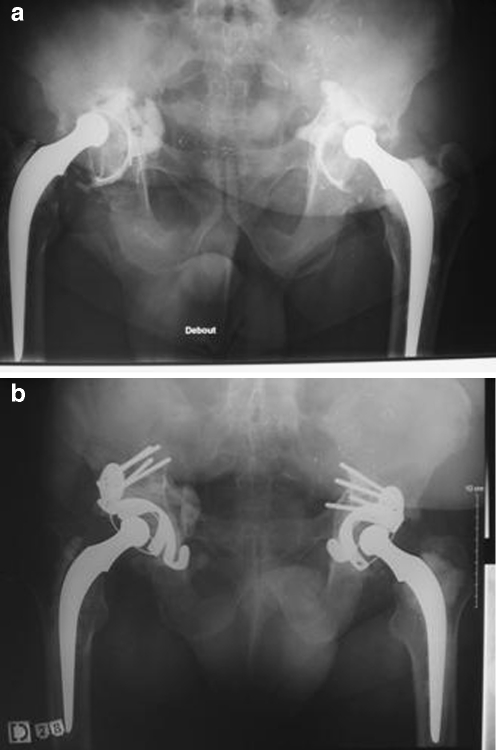
Fig. 1.
A: Post-operative AP radiograph of the pelvis after allograft with a Kerboull ring. B: Radiographs at 5 years after the revision. The rupture of the ring is observed without instability of the implant
Fig. 2.
Radiograph obtained 7 years post-operatively of a patient who had a cemented implant with a metal mesh and allograft. There is a small marginal lucency. The hip continues to function well
Discussion
Allografts are recommended for revision hip arthroplasty to replace the acetabular bone deficiency encountered at revision. These allografts help to restore anatomy or bone stock for future revisions as patients are living and functioning longer. Defects of bone, particularly in hips that have had multiple revisions, could make these reconstructions very difficult. We believed that allografts are a very good biological solution to the bone stock loss giving a good acetabular bone bed (Fig. 3).
Fig. 3.
Postoperative AP radiograph of the pelvis showing complete and stable reconstruction of a Type-II defect six years after surgery. The component is stable and well-fixed
Impaction bone grafting with irradiated or non-irradiated bone gives new bone formation and provides stability of the defect area [11, 18]. Morselised fresh-frozen allograft has been considered as the standard graft [5, 19], but recent series using irradiated allograft show good results in a medium- and long-term follow-up [2, 6, 10].
Irradiation of the allograft has been suggested as an answer to concerns about sterility. Recently, in 2002, the American Center for Disease Control and Prevention has reported around 25 cases of allograft-related infection or illness [13]. Irradiation and chemical treatment of bone grafts could reduce the risks of disease transmission such as infections from donor to recipient, but could not affect the risk of viral and prion transmission. Nevertheless, from a biomechanical point of view, irradiation might cause an alteration in the bone matrix of allograft bone, giving a reduction in strength [8]. Irradiation of an osseous graft at ambient temperature produces a denaturalisation of collagen as a consequence of the release of free oxygen radicals during the irradiation. This irradiation destroys the bonds inside collagen at the level of peptide bonds. Destruction of these peptide bonds is prevented by cold temperatures [9]. In this study, allografts were always irradiated after being freeze dried. They were also chemically treated. To our knowledge, there are no studies about the effect of chemical treatment of allograft. It is not yet clear if this irradiation and chemical treatment could affect long-term graft incorporation.
Assessment of bone graft incorporation after impaction bone grafting is still unclear. Radiological examination remains the standard method of evaluating the grafts, but the correlation between histological and radiological fusion is not clear [11, 17]. A good radiographic incorporation must be considered when there is trabecular remodelling and cortical healing [16]. Absence of demarcation lines is considered as a positive point, but the width of the demarcation line says little about the stability of the implant [4].
Histological evidence from human biopsies have demonstrated remodelling of bone and at least partial restoration of bone stock after an allograft [7, 14]. Allograft examination shows that the cemented grafts are organised in three zones: a zone of regenerated cortical bone, an interface between cement and bone, and nonviable trabecular bone embedded in cement. In a long-term follow-up, the majority of the grafted bone is viable (more than 90%).
Few reports are available on the outcome of irradiated allograft beyond 5 years. In a study of 153 patients, Buckley et al. [2] noted a survivorship of 88% after a mean of 5 years using irradiated allograft. Hassabala et al. [10] describe a series of 58 patients followed up over a period of 48–90 months without re-revision for loosening of the cup. Our series had a medium-term follow-up of only 5 years. None of the patients has required further revision surgery (Fig. 4). In one case of our series, a rupture of the Kerboull ring was observed. The implant shows a minimal displacement after this rupture. Nevertheless, this patient does not have any clinical signs of implant instability or pain. The implant is still in the same position at the last follow-up and seems to be stable more than 12 months after the rupture. We have not planned a new operation for this patient. Certainly, a ring rupture could be a sign of preceding acetabular instability. We remain attentive to the possibility that a further operation could be needed.
Fig. 4.
a: Preoperative radiograph of a 56-year-old man who presented a failed cemented total hip arthroplasty on both sides. b: Radiograph obtained at 5-years follow up, the components are stable and well-fixed
These mid-term outcomes of revision have been encouraging. Despite the satisfactory early clinical results, we remain concerned about the long-term follow-up. Further studies will be needed to confirm these promising results.
Acknowledgments
Disclosure The authors did not receive any outside funding or grants in support of their research for or preparation of this work. Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, division, center, clinical practice, or other charitable or non-profit organisation with which the authors, or a member of their immediate families, are affiliated or associated.
References
- 1.Brooker AF, Bowerman JW, Robinson RA, Riley LH. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg. 1973;55 A:1629–1632. [PubMed] [Google Scholar]
- 2.Buckley SC, Stockley I, Hamer AJ, Kerry RM. Irradiated allograft bone for acetabular revision surgery: Results at a mean of five years. J Bone Joint Surg. 2005;87-B(3):310–313. doi: 10.1302/0301-620X.87B3.14690. [DOI] [PubMed] [Google Scholar]
- 3.D’Antonio JA, Capello WN, Borden LS, et al. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop. 1989;243:126–137. [PubMed] [Google Scholar]
- 4. Lee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop. 1976;121:20–32. [PubMed] [Google Scholar]
- 5. Reock NJ, Drabu KJ. Impaction bone grafting using freeze-dried allograft in revision hip arthroplasty. J Arthroplasty. 2001;16:201–206. doi: 10.1054/arth.2001.20250. [DOI] [PubMed] [Google Scholar]
- 6.Garneti N, Davies AP, Smith EJ, Learmonth ID. Medium term results of impaction bone grafting with irradiated allograft bone. J Bone Joint Surg. 2003;85-B(Supplement. II):159. [Google Scholar]
- 7.Hamadouche M, Blanchat C, Meunier AP, Kerboull L, Kerboull M. Histological findings in a proximal femoral structural allograft ten years following revision total hip arthroplasty: a case report. J Bone Joint Surg. 2002;84-A(2):269–273. doi: 10.2106/00004623-200202000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Hamer A, Stockley I, Elson RA. Changes in allograft bone irradiated at different temperatures. J Bone Joint Surg. 1999;81(B):342–344. doi: 10.1302/0301-620X.81B2.9083. [DOI] [PubMed] [Google Scholar]
- 9.Hamer A, Suvarna SK, Stockley I. Histologic evidence of cortical allograft bone incorporation in revision hip surgery. The Journal of Arthroplasty. 1997;12(7):785–789. doi: 10.1016/S0883-5403(97)90009-7. [DOI] [PubMed] [Google Scholar]
- 10.Hassaballa M, Mehandale S, Smith EJ, Learmonth ID. Use of irradiated bone graft for impaction grafting in acetabular revisions. J Bone Joint Surg. 2006;88-B(Supplement I):66–67. [Google Scholar]
- 11.Holt GM, Stockley I, Elson RA, Ibbotson C. A comparison of the performance of irradiated and non-irradiated bone graft in hip surgery. Hip. 2001;11:18–24. doi: 10.1002/1098-1063(2001)11:1<18::AID-HIPO1016>3.0.CO;2-5. [DOI] [Google Scholar]
- 12.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 13.Laurencin C, Khan Y (2006) Bone Graft Substitute Material. http://www.emedicine.com/orthoped/topic611.htm. Last Updated: Dec. 15,2006.
- 14.Linder L. Cancellous impaction grafting in the human femur: histological and radiographic observations in 6 autopsy femurs and 8 biopsies. Acta Orthop Scand. 2000;71(6):543–552. doi: 10.1080/000164700317362154. [DOI] [PubMed] [Google Scholar]
- 15.Merle d’Aubigné R. Numerical classification of the function of the hip. Rev Chir Orthop Reparatrice Appar Mot. 1970;76(6):371–374. [PubMed] [Google Scholar]
- 16.Nelissen RG, Bauer TW, Weidenhielm LR, LeGolvan DP, Mikhail WE. Revision hip arthroplasty with the use of cement and impaction grafting. Histological analysis of four cases. J Bone Joint Surg. 1995;77-A(3):412–422. doi: 10.2106/00004623-199503000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Pitto RP, Muria GV, Hohmann D. Impaction grafting and acetabular reinforcement in revision hip replacement. Int orthopaedics. 1998;22:161–164. doi: 10.1007/s002640050232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schreurs BW, Slooff TJ, Gardeniers JM, Buma P. Acetabular reconstruction with bone impaction grafting and a cemented cup: 20 years’ experience. Clin Orthop. 2001;393:202–215. doi: 10.1097/00003086-200112000-00023. [DOI] [PubMed] [Google Scholar]
- 19.Toms A, Barker RL, Jones RS, Kuiper JH. Impaction bone grafting in revision joint replacement surgery. J Bone Joint Surg. 2004;86-A(9):2050–2060. doi: 10.2106/00004623-200409000-00028. [DOI] [PubMed] [Google Scholar]