Abstract
There is controversy as to whether operative treatment in Legg–Calvé–Perthes (LCP) disease improves the outcome obtained by conservative treatment. This article describes a paired study of mature patients, diagnosed with LCP disease before the age of 8 years, to compare the radiological results after conservative or surgical management. Patients were paired with strict matching of gender, body mass index, age at onset, disease stage at the first visit, necrotic area, and radiological at-risk signs. Each pair was assessed by comparing the values of five radiological measurements. Fourteen pairs (28 hips) fitted the criteria. The only radiological measure which showed a statistically better result in the surgical group was femoral head sphericity as measured by Mose’s method. However, there was no difference between the two groups for Stulberg class. Our study supports the hypothesis that for hips affected with LCP disease under the age of 8 years, surgery does not improve the outcome.
Résumé
Il existe une controverse dans le traitement de la maladie de Perthes, notamment lorsque l’on affirme que le traitement opératoire améliore l’évolution obtenue après traitement conservateur. Matériel et méthode : nous avons réalisé une étude comparative de patients en fin de croissance dont le diagnostic de la maladie de Perthes avait été réalisé avant l’âge de 8 ans avec comparaison des résultats radiologiques et après traitement conservateur ou chirurgical. Ces patients ont été appariés de façon stricte par âge, DMI, sexe, lors de la première visite. De même, en ce qui concerne les zones nécrotiques et les signes radiologiques de tête à risque. Pour chaque groupe on a évalué cinq critères radiologiques. 14 paires de patients (28 hanches) ont ainsi été étudiés. Résultats, la seule mesure radiologique qui permet d’avoir le meilleur résultat sur le plan statistique est celle dont le groupe présente des têtes fémorales strictement sphériques, selon la technique mesurée de Mose. Cependant, il n’y a pas de différence entre les deux groupes qui sont classés selon Stulberg. Conclusion : notre étude, permet de démontrer l’hypothèse suivante pour les hanches atteintes d’une maladie de Perthes à l’âge de 8 ans, la chirurgie n’améliore pas les résultats.
Introduction
There is controversy as to whether operative treatment in Legg–Calvé–Perthes (LCP) disease improves the outcome obtained by conservative treatment. Controlled trials are lacking. Comparative studies to date have used simplistic and varying criteria to assess the groups [2, 3, 8, 11, 12, 18]. In particular, patients are not matched with regard to severity of the disease.
Herring et al. [6] recently concluded that the lateral pillar classification and age at the time of onset of the disease correlated strongly with outcome in patients with LCP disease. They found that group B hips in children younger than 8 years at the time of onset have a favourable outcome, which was unrelated to treatment. They also found that group C hips in children of all ages frequently have a poor outcome, irrespective of the method of treatment.
This study was designed to test this hypothesis with a paired study, which compared the outcome of conservative and surgical treatment of patients aged less than 8 years at onset who were matched for severity of the disease, gender, physique, age at onset, disease-stage at the first visit, necrotic area, and radiological signs.
Patients and methods
We examined a cohort of 345 patients with LCP disease (on our departmental database) of whom 270 were male and 75 female. The right side was affected in 152 hips, the left in 165 hips, and 28 were bilateral. We selected patients with unilateral disease, who were less than 8 years of age at the time of onset of the disease and only those patients who were mature at the last follow-up. This produced 14 pairs of matched patients. Abduction plasters were used in the treatment of the conservative group. The duration of plaster immobilisation varied from 7 to 19 months. The surgical group had been treated by femoral varus osteotomy (eight patients), Shelf procedure (five patients), and Salter innominate osteotomy (one patient) between 1990 and 1995.
The decision to treat was based on age at onset, the Catterall grade [1], persistent limitation of movement of the hip (particularly if there was less than 30° of abduction), and severe subluxation and/or a metaphyseal cyst. Severe subluxation was defined by a difference in the teardrop distance of more than 3 mm between the affected and unaffected sides. The choice between conservative or operative treatment depended on parental and surgeon preference.
Patients from each group were matched for gender, body mass index within ±2, age at onset, stage at the first visit (initial, necrotic, or regenerative), Herring group [5], Catterall group (III, IV, head-at-risk), and severe subluxation and/or a metaphyseal cyst [1]. Radiographs of each pair were assessed at maturity by Mose’s method for femoral head sphericity [13], by measurement of the acetabular head index (AHI), the slope of the acetabular roof (SAR) [16], the articulo-trochanteric distance (ATD), and by the classification of Stulberg et al. [17].
Statistical analysis
We used the Wilcoxon signed-rank test (software from SAS Institute Inc., Cary, NC). The results were expressed as the mean. A p value <0.05 was considered to be significant.
Results
Fourteen pairs fitted the criteria. Twelve pairs were male and two pairs were female. At the first visit nine pairs were in the necrotic stage and five pairs were in the fragmentation stage. Nine pairs were classified as Catterall group III and five as group IV. Five pairs were classified as Herring B and nine pairs as Herring C. Subluxation and a metaphyseal cyst were seen in nine pairs, and subluxation alone in five (Table 1).
Table 1.
Details of the 14 pairs of patients (pairs 1, 2, 3, 6, 8—shelf; pairs 4, 5, 7, 9, 10, 12, 13, 14—varus osteotomy; pair 11—innominate osteotomy; pairs 7 and 9 are females)
| Number of pair | Body mass index | Age at onset | Stage | Catterall group | Herring group | Head-at-risk sign | |||
|---|---|---|---|---|---|---|---|---|---|
| Conservative | Surgery | Conservative | Surgery | Subluxation | Metaphyseal cyst | ||||
| 1 | 21.6 | 20.7 | 7.00 | 7.30 | Fragmentation | 4 | C | + | + |
| 2 | 16.8 | 18.1 | 6.50 | 7.25 | Necrotic | 3 | B | + | − |
| 3 | 18.3 | 19.1 | 7.25 | 7.10 | Necrotic | 3 | C | + | − |
| 4 | 18.5 | 19.1 | 7.40 | 7.40 | Fragmentation | 4 | C | + | + |
| 5 | 20.5 | 20.8 | 7.70 | 7.90 | Necrotic | 3 | B | + | + |
| 6 | 18.7 | 17.5 | 6.60 | 6.00 | Necrotic | 3 | C | + | + |
| 7 | 19.5 | 18.8 | 6.4 | 6.50 | Fragmentation | 3 | B | + | − |
| 8 | 18.2 | 19.2 | 7.40 | 7.50 | Necrotic | 3 | C | + | + |
| 9 | 18.6 | 18.8 | 8.00 | 7.80 | Necrotic | 4 | B | + | + |
| 10 | 18.8 | 19.6 | 7.80 | 7.25 | Necrotic | 3 | C | + | + |
| 11 | 15.7 | 15.7 | 4.00 | 4.00 | Fragmentation | 3 | C | − | − |
| 12 | 18.9 | 18.7 | 4.30 | 5.00 | Fragmentation | 4 | C | + | + |
| 13 | 18.1 | 17.1 | 7.10 | 7.75 | Necrotic | 3 | B | + | − |
| 14 | 19.3 | 19.3 | 5.80 | 6.20 | Necrotic | 4 | C | + | + |
| Mean | 18.7 | 18.8 | 6.70 | 6.80 | |||||
| p | 0.2 | 0.35 | |||||||
Results of the radiological measurements are given in Table 2. The findings were significantly better for the surgical group when compared with the conservative group for femoral head sphericity as assessed by Mose’s method (p = 0.019) and the AHI (p = 0.034). However, after excluding the five pairs that had undergone a shelf procedure there was no statistical difference between the two groups (p = 0.19) for AHI. By definition, the AHI would be better after a shelf procedure.
Table 2.
Radiological findings in the 14 pairs (pairs 1, 2, 3, 6, 8—shelf; pairs 4, 5, 7, 9, 10, 12, 13, 14—varus osteotomy; pair 11—innominate osteotomy; pairs 7 and 9 are females)
| Number of pair | Mose (mm) | AHI (%) | SAR (°) | ATD (mm) | Stulberg | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Conservative | Surgery | Conservative | Surgery | Conservative | Surgery | Conservative | Surgery | Conservative | Surgery | |
| 1 | 5 | 6 | 79 | 78 | 7 | 10 | 26 | 21 | 3 | 3 |
| 2 | 5 | 4 | 80 | 100 | 5 | 3 | 20 | 25 | 3 | 4 |
| 3 | 9 | 2 | 77 | 89 | 5 | 5 | 26 | 23 | 3 | 2 |
| 4 | 10 | 5 | 73 | 75 | 5 | 8 | 17 | 19 | 3 | 3 |
| 5 | 9 | 5 | 77 | 77 | 4 | 10 | 25 | 21 | 3 | 3 |
| 6 | 1 | 5 | 81 | 93 | 5 | 10 | 18 | 22 | 2 | 3 |
| 7 | 4 | 1 | 74 | 82 | 5 | 5 | 27 | 10 | 3 | 2 |
| 8 | 9 | 5 | 63 | 73 | 15 | 5 | 12 | 22 | 3 | 3 |
| 9 | 10 | 4 | 66 | 100 | 3 | 5 | 38 | 5 | 5 | 3 |
| 10 | 2 | 3 | 95 | 69 | 3 | 10 | 9 | 3 | 2 | 3 |
| 11 | 2 | 1 | 98 | 98 | 10 | 3 | 24 | 17 | 2 | 2 |
| 12 | 18 | 10 | 63 | 71 | 12 | 12 | 10 | 12 | 5 | 3 |
| 13 | 7 | 7 | 66 | 78 | 5 | 4 | 27 | 10 | 3 | 3 |
| 14 | 11 | 1 | 64 | 84 | 4 | 12 | 25 | 28 | 4 | 1 |
| Mean | 7.3 | 4.2 | 75.4 | 83.4 | 6.3 | 7.3 | 21.7 | 17 | ||
| Median | 8 | 4.5 | 75.5 | 80 | 5 | 6.5 | 24.5 | 18 | ||
| p | 0.019 | 0.034 | 0.37 | 0.17 | ||||||
AHI acetabular head index, SAR slope of acetabular roof, ATD articulo-trochanteric distance
No statistical difference was seen between the conservative and surgical groups in the SAR (p = 0.37) and ATD (p = 0.17). Stulberg’s classification showed no significant difference (p = 0.2) in the two groups. Five pairs had a better Stulberg result in the operative group. Four patients in the operative group had femoral osteotomies and one patient had a Shelf procedure. Three of these five pairs were less than 6.5 years at the time of their surgical procedure (pairs 7,11, and 14). Three pairs had a better Stulberg result in the conservative group (pairs: 2, 6, and 10). Six pairs had no difference between the groups (Table 2).
Pair presentation
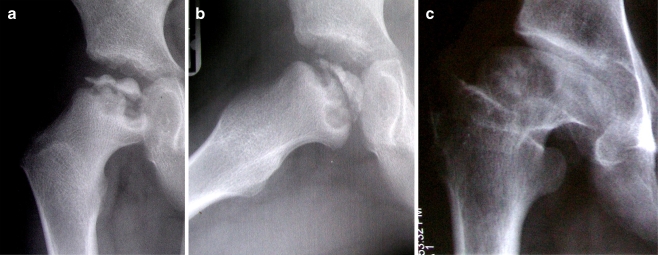
Pair 5 The radiographs at presentation of a 7.7-year-old patient in the conservative group showed Catterall group III/Herring group B with positive signs of subluxation and a metaphyseal cyst (Fig. 1a, b). At skeletal maturity the patient was classified as Stulberg class III with 9 mm loss of sphericity by Mose’s method and an AHI of 77% (Fig. 1c). The radiograph of the paired surgical patient who was treated with a varus osteotomy at the age of 7.9 years showed a more spherical femoral head (5 mm loss of sphericity by Mose’s method) but similar acetabular cover (AHI of 77%). The appearance of this hip at onset is shown in Fig. 2a and b. At skeletal maturity the patient was classified as Stulberg class III (Fig. 2c).
Fig. 1.
Radiographs of a 7.7-year-old boy (pair 5) in the conservative group with Catterall classification III/Herring B and positive signs of subluxation and a metapyhseal cyst showing anteroposterior view (a), lateral view (b), and the same patient at skeletal maturity (c) classified as Stulberg class III
Fig. 2.
Radiographs of the paired surgical patient with Catterall classification III/Herring B and positive signs of subluxation and a metapyhseal cyst (pair 5) showing anteroposterior view (a), lateral view (b), and the same patient at skeletal maturity (c) classified as Stulberg class III
Discussion
The extent of the necrotic area and head-at-risk signs are generally accepted as two of the most influential factors affecting the prognosis in LCP disease after age. In our study, we used the Catterall and Herring classifications to assess the patient’s prognosis. For the Catterall classification, the amount of viable bone and the height of the femoral head on the lateral view were measured in the necrotic or fragmentation stage and any head-at-risk signs were identified. For the Herring classification [5], the height of the lateral part of the epiphysis (lateral pillar) was estimated during the fragmentation stage. The Herring classification has been widely accepted because of its simplicity and reproducibility. However, Lappin et al. [9] have suggested that the Herring grade changes with time, especially in the early stages of the disease. We therefore decided to classify our patient’s with both the Catterall and the Herring classifications.
The advantages of surgical treatment of LCP disease remain controversial despite several reports comparing the results of conservative and surgical treatment [2, 3, 8, 11, 12, 18]. Lloyd-Roberts et al. [11] stated that containment by femoral osteotomy was the treatment of choice in patients with at-risk signs provided that severe deformity had not already occurred. However, their study was based on a simplistic standard of patient selection and only excluded Catterall group I patients. Yet most Catterall group II patients do well without any treatment in this age group. Marklund and Tilberg [12] compared conservative treatment in one institute and surgical treatment in another with differing guidelines of treatment. They concluded that there was no evidence that varus femoral osteotomy interrupted LCP disease or accelerated healing. Lahdes-Vasama et al. [8] compared the outcome between conservative and surgical groups in terms of the femoral sphericity, acetabular cover, and acetabular direction. They concluded that varus femoral osteotomy did not improve the radiographic results in limited epiphyseal involvement or have an effect on the acetabular direction in severe LCP disease. However, they used the Salter and Thompson classification to grade patients. This classification has limited application because only 15% of subchondral fractures are visible on radiographs [14].
Simple case series do not allow useful comparison of different treatment modalities because of multiple confounding factors. The use of carefully matched pairs of conservatively and surgically-treated patients in our study eliminates most confounding factors and more useful information can be obtained regarding the efficacy of one treatment compared to another. By using matched pairs in our study we have tried to obtain a more rigorously controlled comparison between the surgical and conservatively treated groups. We included only patients classified at presentation as Catterall groups III and IV. Kamegaya et al. [7] reported on a paired study of patients predominantly over the age of 8 years and found that the surgically treated group had improved sphericity of the femoral head and greater acetabular cover. In addition 12 of the 18 surgically treated patients had a better Stulberg classification than the conservatively treated group. Our study also showed a statistically significant improvement in sphericity of the femoral head and greater acetabular cover in the surgically treated group. However, we could not demonstrate a statistically significant improvement in the Stulberg classification in the surgically treated group. In our study only five pairs had a better Stulberg classification in the operative group. Four patients in the operative group had femoral osteotomies and one patient had a Shelf procedure. We could not detect a significant difference in Stulberg classification based on the surgical procedure owing to the small numbers involved.
Some authors have reported that the most important factor for the long-term prognosis is the sphericity of the femoral head [13, 17, 20]. In our study sphericity of the head measured by Mose’s method was significantly better in the surgical group. Although the AHI, which reflects acetabular cover, was also significantly better in the entire surgical group, the difference lacked significance once the five patients who had a shelf procedure were excluded from the statistical analysis.
Lecuire [10] has stated in a follow-up study of more than 50 years that normal or flattened spherical heads present few problems, but irregular or very irregular heads are associated with a poor result. There was no statistical difference in SAR or ATD between our groups, but these measures do not seem to correlate with the clinical outcome.
Weiner et al. [19] recommended a postoperative femoral varus angle of more than 105°. Heikkinen and Puranen [4] suggested that 100–110° of varus were optimal for obtaining good containment of the femoral head in the acetabulum. We usually performed osteotomies with about 40° of varus, which resulted in a neck-shaft angle of approximately 100°. This did not affect our ATD as the value of the ATD in both surgical and conservative treatment groups did not show a statistical difference (p = 0.17).
Intertrochanteric osteotomy combined with acetabular roof plasty and/or advancement of the greater trochanter is also useful in the treatment of painful hip secondary to LCP disease. Pécasse et al. [15] report improvement in clinical function, pain reduction, and delay in progression of joint degeneration in young adults operated for sequelae of LCP disease.
We conclude that surgical treatment improves the sphericity of the femoral head compared to conservative treatment in hips of patients less than 8 years of age at the onset of LCP disease. However, the Stulberg grading was not affected. Our study supports the hypothesis that for hips affected with LCP disease under the age of 8 years, surgery does not improve the outcome.
Footnotes
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Contributor Information
S. Sharma, Email: sssharma2@yahoo.co.uk
M. Sibinski, Phone: +48-42-2585636, FAX: +48-42-2563604, Email: sibinek@poczta.onet.pl
References
- 1.Catterall A. The natural history of Perthes’ disease. J Bone Joint Surg Br. 1971;53:37–53. [PubMed] [Google Scholar]
- 2.Evans IK, Deluca PA, Gage JR. A comparative study of ambulation abduction bracing and varus derotation osteotomy in the treatment of severe Legg–Calvé–Perthes disease in children over 6 years of age. J Pediatr Orthop. 1988;8:676–682. doi: 10.1097/01241398-198811000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Fulford GE, Lunn PG, Macnicol ME. A prospective study of nonoperative and operative management for Perthes’ disease. J Pediatr Orthop. 1993;13:281–285. doi: 10.1097/01241398-199305000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Heikkinen E, Puranen J. Evaluation of femoral osteotomy in the treatment of Legg–Calvé–Perthes’ disease. Clin Orthop. 1980;150:60–68. [PubMed] [Google Scholar]
- 5.Herring JA, Neustatt JB, Williams JJ, Early JS, Browne RH. The lateral pillar classification of Legg–Calvé–Perthes disease. J Pediatr Orthop. 1992;12:143–150. doi: 10.1097/01241398-199203000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Herring JA, Kim HT, Browne R. Legg–Calvé–Perthes Disease. J Bone Joint Surg Am. 2004;86:2121–2134. [PubMed] [Google Scholar]
- 7.Kamegaya M, Saisu T, Ochiai N, Hisamitsu J, Moriya H. A paired study of Perthes’ disease comparing conservative and surgical treatment. J Bone Joint Surg Br. 2004;86:1176–1181. doi: 10.1302/0301-620X.86B8.14458. [DOI] [PubMed] [Google Scholar]
- 8.Lahdes-Vasama TT, Marttinen EJ, Merjkanto JEO. Outcome of Perthes disease in unselected patients after femoral varus osteotomy and splintage. J Pediatr Orthop B. 1997;6:229–234. doi: 10.1097/01202412-199710000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Lappin K, Kealey D, Cosgrove A. Herring classification: how useful is the initial radiograph. J Pediatr Orthop. 2002;22:479–482. doi: 10.1097/00004694-200207000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Lecuire F. The long-term outcome of primary osteochondritis of the hip (Legg–Calvé–Perthes disease) J Bone Joint Surg Br. 2002;84:636–640. doi: 10.1302/0301-620X.84B5.12124. [DOI] [PubMed] [Google Scholar]
- 11.Lloyd-Roberts GC, CatteralI A, Salamon PB. A controlled study of the indications for and the results of femoral osteotomy in Perthes’ disease. J Bone Joint Surg Br. 1976;58:31–36. doi: 10.1302/0301-620X.58B1.1270493. [DOI] [PubMed] [Google Scholar]
- 12.Marklund T, Tillberg B. Primary results of conservative treatment and osteotomy in coxa plana: a radiological comparison. Clin Orthop Relat Res. 1977;127:142–147. [PubMed] [Google Scholar]
- 13.Mose K, Hjorth L, Ulfeldt M, Christensen ER, Jensen A. Legg–Calvé–Perthes disease: the late occurrence of coxarthrosis. Acta Orthop Scand Suppl. 1977;169:1–39. [PubMed] [Google Scholar]
- 14.Salter RB, Thompson GH. Legg–Calvé–Perthes: the prognostic significance of the subchondral fracture and a two-group classification of the femoral head involvement. J Bone Joint Surg Am. 1984;66:479–489. [PubMed] [Google Scholar]
- 15.Pécasse GA, Eijer H, Haverkamp D, Marti RK. Intertrochanteric osteotomy in young adults for sequelae of Legg–Calvé–Perthes disease—a long term follow-up. Int Orthop. 2004;28:44–47. doi: 10.1007/s00264-003-0513-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stulberg SD, Harris WH (1974) Acetabular dysplasia and development of osteoarthritis of hip [abstract]. In: Proceedings of the 2nd open scientific meeting of the hip society, Mosby, St Louis, pp 82–93
- 17.Stulberg SD, Coopermann DR, Wallensten R. The natural history of Legg–Calvé–Perthes disease. J Bone Joint Surg Am. 1981;63:1095–1108. [PubMed] [Google Scholar]
- 18.Vukasinovic Z, Slavkovic S, Milickovic S, Siqeca A. Combined Salter innominate osteotomy with femoral shortening versus other methods of treatment for Legg–Calvé–Perthes disease. J Pediatr Orthop. 2000;9:28–33. doi: 10.1097/01202412-200001000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Weiner SD, Weiner DS, Riley PM. Pitfalls in treatment of Legg–Calvé–Perthes disease using proximal femoral varus osteotomy. J Pediatr Orthop. 1991;11:20–24. doi: 10.1097/01241398-199101000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Yrjönen T. Long-term prognosis of Legg–Calvé–Perthes disease: a meta-analysis. J Pediatr Orthop B. 1999;8:169–172. doi: 10.1097/01202412-199907000-00005. [DOI] [PubMed] [Google Scholar]