Abstract
The objective of this paper was to investigate the surgical strategy of the selection of the lowest instrumented vertebrae (LIV) in anterior correction for adolescent idiopathic scoliosis (AIS) and to discuss the relationship between the LIV and trunk balance. From 1998 to 2004, 28 patients with thoracolumbar/lumbar AIS (Lenke 5 type) were treated by anterior correction and fusion with a mean follow-up of 1.5 years. Specific radiographic parameters were observed respectively and the correlation between disc wedging immediately below the LIV and these parameters was analysed. The mean corrective rate of major curves was 74.84%. The preoperative disc angle distal to LIV was 2.96 ± 1.43° and postoperatively it was −3.60 ± 1.75°. The postoperative disc wedging was most correlated with LIV obliquity. The postoperative LIV–CSVL (centre sacral vertical line) distance, which reflects regional balance, was correlated with various preoperative parameters. LIV determination was correlated with multiple preoperative radiographic parameters. Disc wedging distal to LIV occurs most often when a short fusion excluding the lower end vertebra (LEV) and the subjacent disc are nearly parallel.
Résumé
L’objectif de cette étude est de mettre en évidence la meilleure stratégie chirurgicale lors de l’instrumentation des vertèbres lombaires dans la correction antérieure d’une scoliose idiopathique de l’adolescent, pour laquelle il est nécessaire de corréler l’instrumentation basse et la balance rachidienne. Méthode : De 1998 à 2004, 28 patients présentant une scoliose thoracolombaire ou lombaire idiopathique (Lenke type 5) ont été traités par correction avec fusion antérieure avec un recul minimum de 1.5 ans. Nous avons réalisé une évaluation radiologique très sévère avec une évaluation du disque immédiatement sous-jacent à l’arthrodèse. Résultats : la correction moyenne de la courbe principale a été de 74.84%. L’angulation préopératoire du disque immédiatement sous-jacent à la scoliose était de 2.96 et en post opératoire de 3.60. La distance post opératoire CSVL – LIV qui reflète la balance rachidienne était corrélée avec différents paramètres. En conclusion : la fusion distale de la courbure lombaire a lieu le plus souvent lorsque cette arthrodèse exclut les disques sous-jacents et lorsque celui-ci reste parallèle.
Introduction
Thoracolumbar/lumbar scoliosis is a common type of adolescent idiopathic scoliosis (AIS) which is classified as Lenke type 5. Anterior spinal fusion (ASF) with single- or dual-rod constructions has been used for many years and has become a common method of correction over the past 20 years. Compared to posterior correction and spinal fusion (PSF), ASF has the great advantages of short fusion and preservation of the mobility of the lumbar spine [4]. However, we observed clinically that some patients developed trunk imbalance at an early stage or in the long-term due to the short fusion, and which was beyond the compensative ability of unfused levels. To our knowledge, few studies have investigated the relationship between preserving fusion levels and trunk balance regarding anterior correction. This study analysed the radiographic parameters of 28 thoracolumbar/lumbar AIS patients who had complete follow-up data. The surgical strategy of the selection of lower instrumented vertebra (LIV) was evaluated to find the criteria for choosing the LIV preoperatively.
Materials and methods
From 1998 to 2004, 58 patients with a diagnosis of thoracolumbar/lumbar AIS were treated by one doctor in one hospital with anterior correction and spinal fusion, among which, 28 patients who had complete follow-up data were evaluated retrospectively. The average follow-up period was 3.5 years (range 2–8 years). Six patients were male and 22 were female and the average age at operation was 13.96 ± 1.37 years. All of the patients were thoracolumbar/lumbar left scoliosis.
Radiographic evaluation
Standing anteroposterior and lateral X-ray film and supine bending film were taken before surgery. Standing long cassette anteroposterior and lateral radiographs were taken 2 weeks after operation and during follow-up. The radiographic parameters were observed and recorded as follows:
Coronal plane. Cobb angle of the major curve, apex vertebra (Apex), lower end vertebra (LEV), disc angle (DA), lowest instrumented vertebra tilt (LIV obliquity), distance of T1, LIV and Apex to the centre sacral vertical line (CSVL).
Sagittal plane. Cobb angle of the thoracic kyphosis (T4-T12), lumbar lordosis (L1-L5), thoracolumbar lordosis (T12-L2), number of vertebra between Apex to LIV, relationship of LIV with LEV (LIV equalled LEV, LIV=LEV; LIV was one vertebrae below LEV, LIV=LEV+1; LIV was one vertebrae above LEV, LIV=LEV−1), fusion levels.
Surgical technique
All patients received anterior spinal fusion with single-rod instrumentation (Moss Miami, Isola, TSRH). After exposure of the anterior and lateral aspects of the vertebral bodies to be fused, convex annulus and anterior portions of discs were removed. The remaining disc on the concave side can prevent overcorrection and hold the bone graft in place. Bicortical screws (6.0 or 6.5 mm in diameter) were placed in each segment of the fusion levels. An autogenous bone graft from iliac bone was placed in each disc space. An appropriately sized corrective rod was pre-contoured to the coronal and sagittal alignment and then placed from proximal to distal. After all of screws were connected, the rod was turned to the ventral side to restore the lordosis of thoracolumbar/lumbar spine while correcting the coronal curve. Then, inter-segmental compression was applied from the apex to the ends. Overcorrection of the major curve may lead to imbalance of the adjacent curve. Thus, during the operation, fluoroscopy was used to confirm the location of instrumentation and maintenance of the global balance. At the same time, care was taken not to wedge open the distal disc space below the LIV.
Statistical analysis
After anterior surgery, the distal disc adjacent to LIV may undergo two types of change: a parallel disc preoperatively (disc angle was near 0°), may appear wedged postoperatively; a preoperatively wedged disc with the open end towards the concavity may reverse the direction of wedging. In general, a disc angle (DA) of more than 8° and/or LIV obliquity of more than 10° will result in the compensative ability of distal vertebra below the fusion site to decrease and the possibility of imbalance postoperatively in the long term will significantly increase. When the surgical strategy and LIV are being decided preoperatively, the aforementioned factors should be considered. This study evaluated the LIV selection by three statistical analyses as follows:
The disc angle (DA) and absolute disc angle at two weeks postoperatively and up to 5 years of follow-up were analysed with regard to their influence by the LIV relative to the LEV with analyses of variance (ANOVA). Mixed-model repeated measures ANOVA was used if these data changed over time.
Univariate repeated analysis was used to compared LEV–LIV correlation (+1, 0, −1) and various preoperative radiographic parameters. LIV selection was assessed through postoperative parameters.
Coronal balance was demonstrated by three parameters at the final follow-up: disc angle, LIV translation and global balance (T1-CSVL). The correlation of each radiographic parameter and these three parameters were analysed respectively by the use of Pearson’s correlation and stepwise multiple linear regression. The stepwise regression selected independent variables for inclusion or exclusion from the model based on entry criteria of 0.15 and removal criteria of 0.15. All statistical analyses were treated by the Statistical Analysis System (SAS).
Results
The Cobb angle of the major curve was corrected from preoperative 48.82 ± 8.31° to postoperative 12.28 ± 6.16° and 15.37 ± 9.05° in the final follow-up. The mean corrective rate of the major curve was 74.84%. Disc angle (DA) below LIV was 2.96 ± 1.43° preoperatively and −3.60 ± 1.75° postoperatively. There were two patients whose DA of more than 8° appeared as trunk imbalance in the follow-up. The detailed statistical analyses are shown in Tables 1, 2, 3 and 4.
Table 1.
Correlation of lowest instrumented vertebrae–lower end vertebra (LIV–LEV) and disc angle (DA)
| DA | DA | |||
|---|---|---|---|---|
| LIV–LEV | P value | |||
| −1 (n=6) | 0 (n=19) | +1 (n=3) | ||
| Preoperation | −1.35 ± 1.26 | 4.08 ± 3.97 | 12.40 ± 4.08 | <0.01 |
| Final follow-up | −8.75 ± 2.47 | −5.21 ± 3.03 | 1.65 ± 5.24 | |
| DA | Absolute DA | |||
| LIV–LEV | P value | |||
| −1 (n=6) | 0 (n=19) | 1 (n=3) | ||
| Preoperation | 1.40 ± 1.64 | 5.48 ± 4.02 | 12.40 ± 4.08 | <0.01 |
| Final follow-up | 8.75 ± 2.47 | 6.17 ± 3.17 | 4.96 ± 1.98 | |
−1 means LIV=LEV—1; 0 means LIV=LEV; +1 means LIV=LEV+1
LIV=lowest instrumented vertebra; LEV=lower end vertebra
Table 2.
Correlation of preoperative parameters and DA at the final follow-up
| Variable | Partial R-square | Model R-square | C(p) | F value | P value |
|---|---|---|---|---|---|
| DA | 0.0432 | 0.4027 | 12.1350 | 2.15 | 0.0053 |
| T12-L2 | 0.2209 | 0.2209 | 24.6322 | 7.37 | 0.0116 |
| T4-T12 | 0.1701 | 0.3911 | 16.0114 | 6.99 | 0.0140 |
| L1-L5 | 0.0638 | 0.4549 | 14.0260 | 2.81 | 0.0166 |
| Apex-CVSL | 0.1297 | 0.5846 | 7.9313 | 7.18 | 0.0134 |
| Apex-LIV | 0.0492 | 0.6337 | 6.8628 | 2.95 | 0.0398 |
| LIV obliquity | 0.0378 | 0.6716 | 6.5011 | 2.42 | 0.0078 |
Table 3.
Correlation of preoperative parameters and LIV-CSVL distance at the final follow-up
| Variable | Partial R-square | Model R-square | C(p) | F value | P value |
|---|---|---|---|---|---|
| Fusion levels | 0.4859 | 0.4859 | 49.0480 | 24.58 | <0.001 |
| T12-L2 | 0.1271 | 0.6130 | 32.9903 | 8.21 | 0.0083 |
| Apex-LIV | 0.0756 | 0.6886 | 24.2475 | 5.83 | 0.0238 |
| Preoperative DA | 0.0372 | 0.7258 | 20.9579 | 3.12 | 0.0205 |
| LIV obliquity | 0.0831 | 0.8090 | 11.1426 | 9.58 | 0.0053 |
| T1-CSVL | 0.0669 | 0.8759 | 3.6334 | 11.33 | 0.0029 |
Table 4.
Correlation of preoperative parameters and T1-CSVL distance at the final follow-up
| Variable | Partial R-square | Model R-square | C(p) | F value | P value |
|---|---|---|---|---|---|
| LIV-CSVL | 0.0086 | 0.9822 | 732.652 | 12.47 | 0.0016 |
| Fusion levels | 0.0083 | 0.9905 | 382.135 | 21.92 | <0.0001 |
| Preoperative DA | 0.0047 | 0.9952 | 185.837 | 23.35 | <.0001 |
| Apex-LIV | 0.0024 | 0.9976 | 87.3886 | 22.35 | <.0001 |
| LIV obliquity | 0.0007 | 0.9982 | 61.0231 | 8.32 | 0.0086 |
| L1-L5 lordosis | 0.0004 | 0.9986 | 45.3919 | 6.45 | 0.0191 |
| T4-T12 | 0.0002 | 0.9995 | 14.0143 | 5.70 | 0.0275 |
| T1-CSVL | 0.0004 | 0.9990 | 31.5501 | 7.70 | 0.0113 |
The correlation of three different types of LIV–LEV and disc angle preoperativly and during the final follow-up respectively is shown in Table 1. It can be seen that the patients showed large disc wedging at the final follow-op when fused to one vertebrae proximal to LEV and the disc space was near parallel when fused to one vertebrae distal.
Table 2 shows the correlation of DA at the final follow-up with various preoperative parameters. The preoperative parameters correlated with postoperative DA were: preoperative DA, T12-L2 lordosis, T4-T12 kyphosis, L1-L5 lordosis, Apex-CSVL distance, segments of Apex-LIV and LIV obliquity. Among these factors, preoperative DA was the most correlated.
The correlation of postoperative LIV-CSVL distance, which reflects regional balance, with various preoperative parameters are listed in Table 3. In all of the preoperative parameters, fusion levels, T12-L2 lordosis, segments of Apex-LIV, preoperative DA, LIV obliquity and T1-CSVL distance were correlated.
The correlation of postoperative T1-CSVL distance, which reflects global balance, with various preoperative parameters are shown in Table 4. In all of the preoperative parameters, fusion levels, LIV-CSVL, segments of Apex-LIV, preoperative DA, LIV obliquity, L1-L5 lordosis, T4-T12 kyphosis and T1-CSVL distance were correlated.
Discussion
Since the anterior Dwyer and Ziekle system were introduced in scoliosis surgery, anterior correction and fusion has become an appropriate option for the surgical treatment of thoracolumbar/lumbar scoliosis [4]. Compared to posterior instrumentation, ASF can fuse fewer segments to maintain lumbar mobility. Furthermore, compressive force direct to the vertebra can prevent the potential risk of spinal cord injury, which is unlike the distraction force in the posterior approach [8, 9].
The general principles of anterior fusion levels selection was as follows. Confirmation of the horizontal position of the apex on the anteroposterior X-ray film then if the apex was a vertebra, one vertebra up and down should be fused. If the apex was a disk space, two vertebra up and down should be fused. The nearest opening disc to the apex when bending to the convexity can remain unfused. On the concave bending film, the vertebra below the LIV should be parallel or nearly parallel to the pelvis [5].
In most thoracolumbar/lumbar scoliosis patients, anterior correction and spinal fusion may save one or two levels compared to PSF. But in clinical practice, authors have found that some of the patients appeared to be imbalanced postoperatively. Short fusion concentrated too much force around the apex area, which may cause the compensated curve adjacent to the major curve to lose its ability to correct spontaneously [1].
Trunk balance included global balance and regional balance, which was generally evaluated by standing long cassette anteroposterior and lateral roentgenography. The distance of T1 to CSVL is the most important index to evaluate the global trunk balance, and regional balance was reflected by such indexes as the distance of Apex-CSVL or LIV-CSVL, DA, LIV obliquity, etc. This study analysed the correlation of LIV selection and trunk balance by the evaluation of these indices. The ideal outcome is to save as many fusion levels as possible whilst maintaining global and regional balance.
Correlative factors of postoperative DA and LIV
The study found that the preoperative DA itself is the most significant factor among all of the correlative indexes to postoperative DA below LIV by multiple regression analysis. The possibility of postoperative disc wedging beyond 5° is greater if the preoperative disc distal to LIV is nearly parallel.
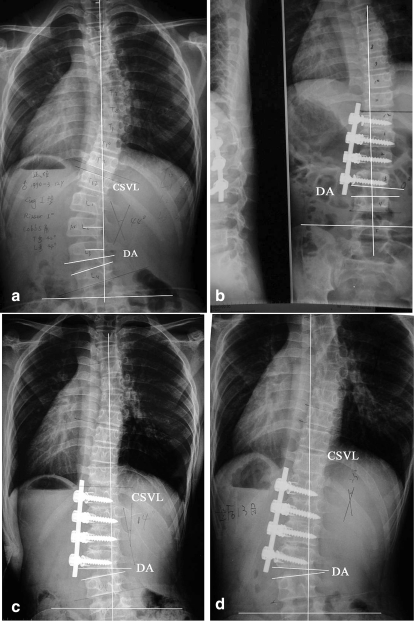
Other factors correlated to postoperative DA were all related to LIV. They were preoperative T12-L2 lordosis, T4-T12 kyphosis, L1-L5 lordosis, Apex-CVSL, Apex-LIV and LIV obliquity. We saw that the sagittal index was closely related to postoperative disc wedging, and Apex translation, vertebral numbers between LIV to Apex and LIV obliquity were all correlated with disc wedging significantly. Generally, short fusion may result in greater disc wedging (Fig. 1). In this study, less fusion levels (fewer levels of Apex-LIV, LIV=LEV–1) were significantly correlated with postoperative disc wedging. When LIV=LEV and the distal disc is near parallel, the disc wedging was less than that of LIV=LEV–1 (Fig. 1). T12-L2 represents the thoracolumbar sagittal alignment. Kyphotic T12-L2 means stiff upper lumbar spine, which may cause postoperative disc wedging. Because the derotation manoeuvre and compression forces were directly concentrated on LIV vertebrae, the disc below will experience wedging if the mobility of lower segments were poor or the compensation ability was poor.
Fig 1.
Male, 14-year-old patient with idiopathic lumbar scoliosis and 0° Risser sign. The lumbar curve was totally corrected (b) by short fusion from 44° preoperatively (a) with T12 to L3 fusion. LIV was L3 and LEV was L4. The disc angle was −8° and 2 weeks postoperatively was −5°, 6 months later −10° (c) and one year after operation it was −15° (d). Regional imbalance was noted
Recently, anterior short fusion involving only 3 to 4 vertebrae has been reported for some major TL/L curves of AIS [1, 2]. The advantage of a shorter fusion is the preservation of more mobile segments but some of the literature suggested that the possibility of disc wedging after shorter fusion increased [1]. Kaneda et al. [3] reported disc wedging in patients of TL/L AIS after ASF with the use of Kaneda’s dual--rod instrumentation. The disc angle of patients who received anterior short fusion 2 to 4 years postoperatively was 6.6° (similar with group LIV=LEV−1 of this study) (Fig. 1d) and those who were fused to LEV or LEV below was 3° (LIV=LEV, LEV+1). Bitan et al. [1] reported 5 of the 24 TL/L AIS patients who received short fusion appeared to have disc wedging below LIV postoperatively and no significant changes were observed in two years of follow-up.
Why does a short fusion generate disc wedging? We found the possible answer from the literature reviewed. In anterior correction of AIS using solid-rod instrumentation, the corrective forces include derotation forces converting scoliosis to lordosis and compression forces in convexity. And during the derotation manoeuvre, the corrective forces were thought to be distributed throughout the entire curve. However, compressive forces were directly applied to convexity, which tended to create disc wedging below the LIV by pulling the LIV to the Apex [1–3, 6]. Spiegel et al. [7] documented significantly higher strains at the bone–screw interface of both end vertebral screws in an ASF model using a calf spine when the length of the spine that is instrumented was shorter and the forces transmitted to the vertebrae were higher [7]. In anterior correction of AIS, compressive forces on inter-segmental convexity make postoperative disc wedging below LIV inevitable and the self-corrective ability of vertebra below LIV is significantly correlated with the amount of disc wedging.
Translation of LIV
The translation of the LIV is described by the distance between LIV and CSVL, which had correlation with the following factors: preoperative lordosis of T12-L2, distance between Apex to LIV, preoperative DA, LIV obliquity and T1-CSVL. Regional balance was bad when the preoperative lordosis of T12-L2 decreased with less segments between Apex to LIV, larger preoperative absolute DA, LIV obliquity and longer distance of T1-CSVL and LIV-CSVL postoperatively.
Global trunk balance
Postoperative global trunk balance is correlated with many preoperative factors. The distance between T1 to CSVL was improved from 0.93 ± 0.76 cm to 0.35 ± 0.40 cm. Three patients who received a short fusion appeared to experience regional imbalance after 6 months follow-up and exhibited mild global imbalance.
Conclusion
Anterior correction and fusion for adolescent idiopathic scoliosis (AIS) can preserve fusion levels and lumbar motion. But a fusion that is too short may lead to disc wedging distal to the lowest instrumented vertebra and trunk imbalance. Preoperative radiographic evaluation is important to predict postoperative lowest instrumented vertebrae (LIV) position and surgical planning is potentially more influential than the procedure itself. Shorter fusion (LIV=LEV−1) should not be chosen for patients whose disc angle between the lower end vertebra (LEV) and upper vertebra was large (more than 5°), segments of Apex to the vertebra to be chosen (LIV) was few, distance from CSVL to LIV was longer and LIV obliquity was bigger. The possibility of postoperative disc wedging has a high incidence if a preoperative parallel disc was not fused. Disc wedging should be avoided when the parallel disc is included with the sacrifice of one mobile segment.
Contributor Information
Yang Liu, Email: liuyangspine@hotmail.com.
Ming Li, Email: imhappyy2002@yahoo.com.cn.
Wen Yuan, Email: spine@citiz.net.
References
- 1.Bitan FD, Neuwirth MG, Kuflik PL, Casden A, Bloom N, Siddiqui S. The use of short and rigid anterior instrumentation in the treatment of idiopathic thoracolumbar scoliosis: a retrospective review of 24 cases. Spine. 2002;27:1553–1557. doi: 10.1097/00007632-200207150-00014. [DOI] [PubMed] [Google Scholar]
- 2.Hall JE, Millis MB, Snyder BD. Short segment anterior instrumentation for thoracolumbar scoliosis. In: Bridwell KH, DeWald RL, editors. The textbook of spinal surgery. 2. Philadelphia, PA: Lippincott-Raven; 1997. pp. 665–674. [Google Scholar]
- 3.Kaneda K, Shono Y, Satoh S, Abumi K. New anterior instrumentation for the management of thoracolumbar and lumbar scoliosis. Application of the Kaneda two-rod system. Spine. 1996;21:1250–1262. doi: 10.1097/00007632-199605150-00021. [DOI] [PubMed] [Google Scholar]
- 4.Majd ME, Castro FP, Jr, Holt RT. Anterior fusion for idiopathic scoliosis. Spine. 2000;25:696–702. doi: 10.1097/00007632-200003150-00008. [DOI] [PubMed] [Google Scholar]
- 5.Ouellet JA, Johnston CE., 2nd Effect of grafting technique on the maintenance of coronal and sagittal correction in anterior treatment of scoliosis. Spine. 2002;27:2129–2136. doi: 10.1097/00007632-200210010-00010. [DOI] [PubMed] [Google Scholar]
- 6.Potter BK, Kuklo TR, Lenke LG. Radiographic outcomes of anterior spinal fusion versus posterior spinal fusion with thoracic pedicle screws for treatment of Lenke Type I adolescent idiopathic scoliosis curves. Spine. 2005;30:1859–1866. doi: 10.1097/01.brs.0000174118.72916.96. [DOI] [PubMed] [Google Scholar]
- 7.Spiegel DA, Cunningham BW, Oda I, Dormans JP, McAfee PC, Drummond DS. Anterior vertebral screw strain with and without solid interspace support. Spine. 2000;25:2755–2761. doi: 10.1097/00007632-200011010-00007. [DOI] [PubMed] [Google Scholar]
- 8.Sweet FA, Lenke LG, Bridwell KH, Blanke KM, Whorton J. Prospective radiographic and clinical outcomes and complications of single solid rod instrumented anterior spinal fusion in adolescent idiopathic scoliosis. Spine. 2001;26:1956–1965. doi: 10.1097/00007632-200109150-00005. [DOI] [PubMed] [Google Scholar]
- 9.Turi M, Johnston CE, 2nd, Richards BS. Anterior correction of idiopathic scoliosis using TSRH instrumentation. Spine. 1993;18:417–422. doi: 10.1097/00007632-199318040-00001. [DOI] [PubMed] [Google Scholar]