Abstract
This paper presents a clinical and functional assessment of the cases of osteochondritis dissecans (OCD) treated with small mosaicplasty type osteochondral grafts. Between 1999 and 2004, we operated on 12 knees with OCD stages III and IV. They were assessed using the International Cartilage Research Society (ICRS) scale, the Visual Analogue Scale (VAS) scale, X-ray and magnetic resonance imaging (MRI). The study was carried out using a clinical series, was retrospective and had a level of evidence of 4. Before surgery, all patients were in classes III and IV on the ICRS scale (four in class III and eight in class IV). At the time of surgery, the patient age was 27.5 ± 7.9 years, with male predominance (75%). Eleven of the cases were assessed as classes I and II on the ICRS scale (seven in class I and four in class II), with one patient in class IV. X-ray assessment was less favourable, revealing alterations in the articular space in 75% of cases. The results show that this technique enables the biological fixation of fragments and, functionally, the clinical results obtained were very good. The osteochondral grafts avoid the implantation of foreign material and make use of bone fragments of the same rigidity as the OCD fragment. We conclude that the technique described is an excellent alternative to the techniques normally used for the fixation of stage III and IV OCD.
Résumé
Les auteurs présentent une évaluation clinique et fonctionnelle des malades avec ostéochondrite disséquante du genou (OCD) traitées avec des greffons osteochondrales (mosaicplasty-lie).Entre 1999 et 2004, nous avons opéré 12 genoux avec ostéochondrite disséquante (étage 3 et 4). Ils ont été évaluées en utilisant l’échelle d'ICRS, VAS, les radiographies et la résonance magnétique. Série clinique, rétrospectif, niveau de évidence 4.Avant la chirurgie, tous les malades étaient dans les groupes III et IV de l'échelle ICRS (4 á l’étage III ; 8 à IV). Au moment de la chirurgie, l'âge moyen était de ± 27.5 7.9 ans et prédominance masculine (75%). Au moment de la révision 11 des malades étaient dans les groupes I et II d'ICRS (7 I et 4 II), 1 malade dans le groupe IV. L'évaluation radiographique montrait altérations arthrosiques avec pincement d’interligne articulaire en 75% des cas.Cette technique permet la fixation biologique des fragments. Fonctionnellement, les résultats cliniques obtenus étaient très bons. Elle peut dispenser l'implantation d’autre matériel (un corp étranger) en même que les greffes de fixation présentent la même rigidité du fragment osteochondral.La technique décrite est une excellente alternative aux techniques normalement utilisées pour la fixation des Osteochondritis disséquantes dégrée III et IV.
Introduction
Osteochondritis dissecans (OCD) is an acquired condition of the subchondral bone and adjacent joint cartilage, and is potentially reversible if healing occurs. In the absence of healing, the development of necrosis, instability and the release of an osteochondral (OC) fragment occurs [14].
For the treatment of cases involving the release or detachment of an OC fragment, various techniques have been described. Drilling [1, 3], transposition from the posterior zone of the femoral condyles [18, 24] and mosaicplasty [8–11] are some solutions to this condition. Refixing of the fragment, which is often more complex, has also been done using screws, biodegradable rods [21], Kirschner wires [20] or Herbert compression screws [22]. Berlet described a mosaicplasty-type refixing technique using OC fragments [5]. This type of solution was also being used at the same time in our department. OC grafts are harvested in the same way as for mosaicplasty but are used to fix the unstable OCD fragment.
Materials and methods
Stage III and IV cases of knee OCD that had undergone surgery in our department between 1999 and 2004 were assessed for this study. A total of 12 patients were involved. All surgery was carried out by the senior author using the Berlet [5] technique.
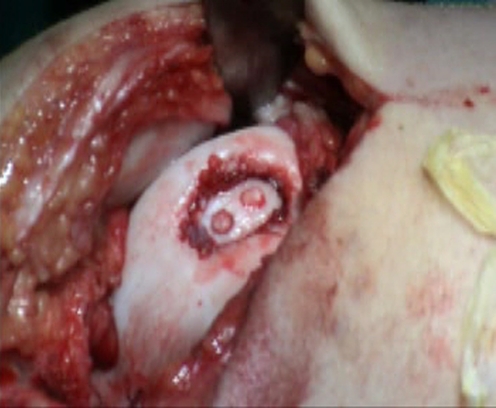
Under general or regional anaesthesia, a tourniquet was placed at the root of the thigh. Arthroscopy was performed first, which confirmed the type of OC lesion and showed its area (Fig. 1). With arthroscopic control or by mini-arthrotomy, two or three osteochondral autografts with a diameter of between 2.7 and 3.5 mm and 25 mm in length, were harvested from the medial femoral condyle (intercondylar notch) of the same knee using the mosaicplasty system (Smith & Nephew Endoscopy, London, UK). For stage IV, the osteochondral fragment was placed into its bed, two or three holes were drilled through the fragment and its bed, and then fixed with the osteochondral autografts (Figs. 1, 2 and 3). The depth of holes in the fragment and the osseous bed was 25 mm, and at least 15 mm inside the femoral condyle. For OCD stage III, the holes are made in situ with a 25-mm depth without leaving the fragment. Figure 3 shows the final result of a stage IV fragment located at the femur trochlea fragment fixed with two OC plugs.
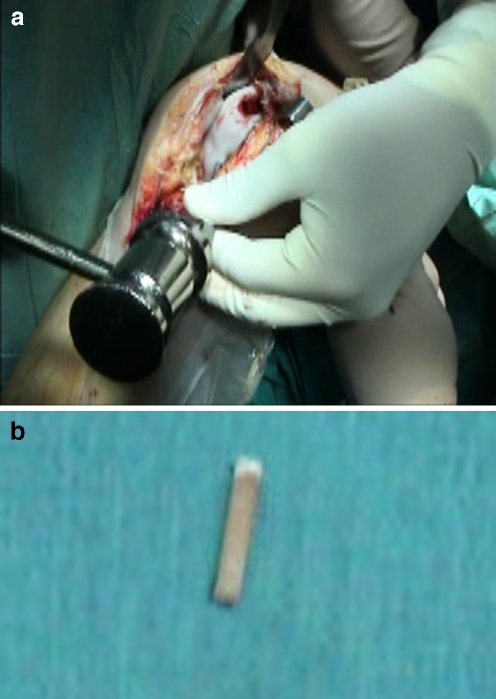
Fig. 1.
Trochlear osteochondritis dissecans (OCD) stage IV
Fig. 2.
a Harvesting of the osteochondral (OC) graft. b The OC graft
Fig. 3.
Inlay fixation of OCD with the OC graft
Postoperatively therapy was initiated the next day with a range of motion exercises and isometric quadriceps strengthening. An emphasis was placed on regaining the range of motion. The patient was permitted only touch-down weight-bearing for the first 6 weeks. Weight-bearing was allowed between the 7th and 10th week.
Patients were assessed pre-operatively by clinical examination (range of motion, effusion, tenderness, meniscal signs, instability tests (drawer test), Lachman’s test, pivot shift). For clinical evaluation, the International Cartilage Research Society (ICRS) protocol1 was adopted. Data such as the cause of the lesion, the onset of symptoms, sporting activity, the age of the patient at the time of trauma, subjective functioning of the knee (as a percentage in relation to the other knee, prior to surgery) and the level of physical activity were included. The depth of cartilage implication is also assessed on a scale of four grades [17]. All of these items are categorised into four groups from A (better) to D (worse). The final classification corresponds to the worst classification obtained by the items assessed.
For pain assessment, a simple visual analogue scale (VAS) was used involving a 10-cm line, one end of which (0) was labelled “pain-free” and the other (10) “intolerable pain.” The patient was asked to indicate the point on the line that corresponded to the exact level of pain experienced. The point indicated was then measured from point 0 and the result was recorded in mm.
The radiographic protocol included X-rays of the knee in the anteroposterior (AP), lateral and patellar views at 30° flexion of the knee. Bedouelle’s radiological classification of OCD lesions [24] was used for the X-ray associated with the ICRS classification. With the ICRS X-ray protocol, the patients are divided into four groups, in accordance with the degenerative changes that are present (normal, light narrowing of the femoral tibial (FT), narrowing of the FT more than 50%, narrowing of the FT and other degenerative changes). This assessment is useful for medium- and long-term postoperative follow-up, since it enables possible alterations (such as degenerative changes) to be identified.
Magnetic resonance imaging (MRI) was performed at 12 months and at the 2006 examination. The most important points to assess are the state of the joint cartilage, the bone status and the vitality of the fragment [13, 14].
All patients were monitored in outpatient consultations at 3 months, 6 months and 1 year, and then annual visits thereafter. On all visits, patients were assessed using the overall global assessment protocol described above, except for MRI, which was performed after the first year. In 2006, all patients were requested for an appointment and global protocol assessment, including MRI.
For the study, the hypothesis to be tested (H0) was formulated as “the absence of any difference between the operated knee and the opposing one in the ICRS and VAS assessment.” The patients’ records were fed into a database and processed statistically; the chi-squared test was used for the categorical variables (ICRS scale) and Student’s t-test for the continuous variables (VAS scale). A score of p < 0.05 was considered as an alpha error.
Results
Table 1 shows the patient profile. There was a predominance of male patients (75%), with an average age of 27.5 years and a standard deviation (s.d.) of 7.9 years. In most cases (11 out of 12), the OC lesion was located in the medial femoral condyle and the average size was 2.3 cm2 with an s.d. of 0.5 cm2. In one case, the fragment was located in the femoral trochlea (Fig. 1). On the VAS scale, the average score was 71 mm with an s.d. of 22 mm. In the pre-operative assessment, four patients were considered as class III and 8 as class IV, according to the ICRS classification system.
Table 1.
The patient profile of this study
| Case | Sex | Age | OCD stage | Size (cm2) | Cause | Onset of symptoms | X-ray ICRS | Final ICRS | |
|---|---|---|---|---|---|---|---|---|---|
| Pre-operative | 2006 | ||||||||
| 1 | Male | 42 | III | 2.5 | ADL | Gradual | II | II | II |
| 2 | Male | 18 | III | 2.0 | Sports | Gradual | I | I | I |
| 3 | Male | 33 | IV | 2.3 | ADL | Gradual | I | II | I |
| 4 | Female | 36 | IV | 2.1 | ADL | Gradual | I | II | II |
| 5 | Female | 37 | III | 2.1 | ADL | Gradual | I | I | I |
| 6 | Male | 18 | IV | 3.0 | Sports | Gradual | I | I | I |
| 7 | Male | 21 | III | 2.9 | Sports | Gradual | I | I | II |
| 8 | Female | 23 | IV | 2.3 | ADL | Gradual | I | II | IV |
| 9 | Male | 21 | III | 2.5 | ADL | Gradual | I | I | II |
| 10 | Male | 30 | III | 3.1 | ADL | Gradual | I | II | I |
| 11 | Male | 26 | III | 2.1 | ADL | Acute | I | I | I |
| 12 | Male | 25 | III | 1.1 | ADL | Gradual | I | I | I |
Two OC grafts were used in almost all of the cases (11 out of 12).
In 2006, the average follow-up was 4.3 years with an s.d. of 2.1 years, with a maximum of 7 years and a minimum of 2 years. At the time of the final assessment, seven patients were in class I, four in class II and one in class IV. The only case in class IV had had a stage IV lesion pre-operatively.
At the review, the VAS scale average was 20 mm with an s.d. of 9 mm. This was statistically significantly different (p < 0.05) from the pre-operative classification.
When the operated knee was compared with the opposite knee, nine of the cases reported no difference between them according to the ICRS classification. The opposite knee was considered to be better than the operated knee in only three cases.
For radiological assessment, five patients (41.6%) showed, at revision, alterations, with interline narrowing (Group II of the ICRS classification; Table 1). There was no statistical correlation between the X-Ray ICRS group and the ICRS clinical result, nor with the pre-operative OCD stage.
According to the MRI scanning, 71.4% of the cases showed alterations in the 2006 review not only with cartilage irregularity but also with the presence of signs of the harvesting of the OC grafts for fixation. Figure 4 shows a case after 4 years and Fig. 5 a case after 6 years.
Fig. 4.
Magnetic resonance imaging (MRI) T1 follow-up at 4 years
Fig. 5.
MRI T2 follow-up at 6 years
Discussion
OCD of the knee is a relatively rare lesion amongst the population as a whole, with a prevalence of between 0.01% and 0.06% [15]. It affects predominantly males aged between 16 and 36 years, with a 70% incidence in the 5–20 years age range.
It is found mostly in the knee (in around 75% of cases), with the medial femoral condyle being the most prevalent location (70– 200%) and in the juvenile population [2]. There is a traditional division between the juvenile and adult forms of the condition. Pappas [19] suggested a classification system for prognosis based on factors of natural history. Category I includes children without total skeletal maturity, Category II involves young people up to the age of 20 and Category III is for all patients over the age of 20. Adult forms have a worse prognosis, with a greater propensity for instability. Cases that do not heal may develop late sequelae, such as early degenerative joint disease [18, 19, 22].
Bedouelle’s radiological classification [4] is accepted due to its simplicity. Stage I and II lesions are considered to be stable and susceptible to conservative treatment, while stages III and IV as unstable, requiring a more aggressive intervention.
MRI is, nowadays, current practice for the diagnosis of OCD, for therapeutic planning and for monitoring the development of the lesion [14].
Surgical treatment for OCD of the knee is still controversial [6]. Arthroscopic assessment is generally accepted as an initial approach, though lesions with a surface area of more than 240 mm2 and which involve subchondral bone loss, involving weight-bearing areas of the knee, are particularly problematic [1, 7, 17]. One of the main points of the arthroscopy is to establish the status of the joint cartilage, as well as diagnosing and determining the severity of concomitant lesions, which are much more frequent in arthroscopic assessment than in other diagnostic methods [2]. For stage III OCD, drilling is other solution but in the adult form of OCD, it may have a failure rate of around 50% [1, 19]. In 1957, Smillie described fixation using wires [20], which was followed by other techniques involving screws [16], Herbert screws [22] or even the use of biodegradable materials [21]. Other widely divulged techniques include Wagner’s procedure [24], involving four different means of fixation and repair of the OC. Here too, the results were not very good, particularly in patients nearing adult age [23].
Versier and Breda [23], in a multi-centre retrospective study, assessed 95 cases of fixation with an average follow-up of 5 years. The results were considered fair, with 67% of cases in class III or IV. In assessing the different fixation techniques, the results have only been reasonable in cases using biodegradable materials.
There is no fixation technique that guarantees a completely satisfactory result. The aim is to maintain the fragment stability, and with compression of the OC fragment in its previously debrided bed, with a fixation that should be long-lasting. In cases involving large OCD fragments, mosaicplasty [9, 10, 21, 22, 10] has been used. But if the fragment is loose, intact and congruent with the crater or still in its own bed, we believe that curettage, with debridement or drilling as far as the bleeding subchondral bone, followed by fixation of the fragment should be performed. Mosaicplasty has the advantage of being technically easier to perform and allows greater stability but it is more difficult to reconstruct a good curvature. Fixation is technically more difficult and provides only precarious stability but allows better cover of the whole defect and better reconstitution of the curvature of the affected area, as described by Berlet [5] and Kobayashi et al. [13].
Kazutomo et al. [12] review 12 cases treated with the Berlet technique and a follow-up of 54 months. Excellent and good results were reported for 11 of the patients assessed. Like Kazumoto et al., our series also has 12 patients. The small number of cases in our study may affect the interpretation of the results and could be considered as a weak point. However, we should remember that this type of pathology is infrequent and that we work and reside in a country of 10 million inhabitants. Even Kazutomo et al. [12], in a country with a much bigger population, present a similar number of cases.
Our clinical results were similar, to most of the patients assessed as ICRS classes III and IV to classes I and II. The only case that remained in class IV had suffered various postoperative complications, including a reflex sympathetic dystrophy, which may largely explain the result.
The true weak point of the work is the lack of any comparison with a different technique. However, this is due to the small number of cases that appeared since we started using this type of fixation. However, comparison with the opposite knee, which served as a standard, showed that, clinically, the patients felt the operated knee was just as good.
Despite the good clinical results, X-ray and MRI have poor results. Almost all MRI scans confirmed the integration of the OC graft and the fragment (11/12) but they showed alteration at the chondral line. This observation should be interpreted as the presence of a scar but without clinical implication.
On X-ray, we saw a narrowing of the FT line, showing a progressive degeneration and evolution to osteoarthritis. Despite the MRI and X-ray results, patients were satisfied with the treatment.
The question is, though, for how long?
Conclusion
Fixation of the osteochondritis dissecans (OCD) fragment with cylindrical osteochondralfragment (OC) grafts is a valid option, with good clinical results. Evaluation with X-ray and magnetic resonance imaging (MRI) shows that, despite the good clinical results, the worst prognosis for adult OCD is true and that we have to be prudent and expectant with long-term results. This technique is a good alternative but has no effect on the natural history of adult OCD.
Acknowledgement
The authors would like to thank Francisco Balacó for the interpretation and critical review of the statistical analysis.
Conflict of interest statement There are no conflicts of interest of any of the authors.
Footnotes
The cartilage standard evaluation form/knee. ICRS Newsletter, Spring 1998.
References
- 1.Aglietti P, Buzzi R, Bassi PB, Fioriti M. Arthroscopic drilling in juvenile osteochondritis dissecans of the medial femoral condyle. Arthroscopy. 1994;10:286–291. doi: 10.1016/S0749-8063(05)80113-6. [DOI] [PubMed] [Google Scholar]
- 2.Årøen A, Løken S, Heir S, Alvik E, Ekeland A, Granlund OG, Engebretsen L. Articular cartilage lesions in 993 consecutive knee arthroscopies. Am J Sports Med. 2004;32:211–215. doi: 10.1177/0363546503259345. [DOI] [PubMed] [Google Scholar]
- 3.Bandi W, Allgoewer M. On the therapy of osteochondritis dissecans (in German) Helv Chir Acta. 1959;26:552–558. [PubMed] [Google Scholar]
- 4.Bedouelle J (1988) L’ostéochondrite disséquante des condyles fémoraux chez l’enfant et l’adolescent. In: Cahiers d’enseignement de la SOFCOT. Expansion Scientifique Française, Paris, France, pp 61–93
- 5.Berlet GC, Mascia A, Miniaci A. Treatment of unstable osteochondritis dissecans lesions of the knee using autogenous osteochondral grafts (mosaicplasty) Arthroscopy. 1999;15:312–316. doi: 10.1016/S0749-8063(99)70041-1. [DOI] [PubMed] [Google Scholar]
- 6.Cahill B. Osteochondritis dissecans of the knee: treatment of juvenile and adult forms. J Am Acad Orthop Surg. 1995;3:237–247. doi: 10.5435/00124635-199507000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Duchow J, Hess T, Kohn D. Primary stability of press-fit-implanted osteochondral grafts. Influence of graft size, repeated insertion, and harvesting technique. Am J Sports Med. 2000;28:24–27. doi: 10.1177/03635465000280011601. [DOI] [PubMed] [Google Scholar]
- 8.Hangödy L, Kish G, Karpati Z, Udvarhelyi I, Szigeti I, Bély M. Mosaicplasty for the treatment of articular cartilage defects: application in clinical practice. Orthopedics. 1998;21:751–756. doi: 10.3928/0147-7447-19980701-04. [DOI] [PubMed] [Google Scholar]
- 9.Hangödy L, Füles P. Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints. Ten years of experimental and clinical experience. J Bone J Surg Am. 2003;85:25–32. doi: 10.2106/00004623-200300002-00004. [DOI] [PubMed] [Google Scholar]
- 10.Jakob RP, Petek D (2003) Ostéochondrite disséquante du genou traité par la mosaicplasty. In: Cahiers d’enseignement de la SOFCOT. Expansion Scientifique Française, Paris, France, pp 15–30
- 11.Karataglis D, Learmonth DJ. Management of big osteochondral defects of the knee using osteochondral allografts with the MEGA-OATS technique. Knee. 2005;12(5):389–393. doi: 10.1016/j.knee.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 12.Kazutomo M, Yasuyuki I, Eiichi T, Hideki S, Satoshi T. Results of arthroscopic fixation of osteochondritis dissecans lesion of the knee with cylindrical autogenous osteochondral plugs. Am J Sports Med. 2007;35:216–222. doi: 10.1177/0363546506294360. [DOI] [PubMed] [Google Scholar]
- 13.Kobayashi T, Fujikawa K, Oohashi M. Surgical fixation of massive osteochondritis dissecans lesion using cylindrical osteochondral plugs. Arthroscopy. 2004;20(9):981–986. doi: 10.1016/j.arthro.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 14.Kocher MS, Tucker R, Ganley TJ, Flynn JM. Management of osteochondritis dissecans of the knee. Current concepts review. Am J Sports Med. 2006;34(7):1181–1191. doi: 10.1177/0363546506290127. [DOI] [PubMed] [Google Scholar]
- 15.Lefort G (2006) Ostéochondrite disséquante des condyles fémoraux. In: Symposium de la SOFCOT 2005, suppl au no 5. Rev Chir Orthop 92(2):S99 [PubMed]
- 16.Louisia S, Beaufils P, Katabi M, Robert H, French Society of Arthroscopy Transchondral drilling for osteochondritis dissecans of the medial condyle of the knee. Knee Surg Sports Traumatol Arthrosc. 2003;11(1):33–39. doi: 10.1007/s00167-002-0320-0. [DOI] [PubMed] [Google Scholar]
- 17.Makino A, Muscolo DL, Puiegdevall M, Costa-Paz M, Ayerza M. Arthroscopic fixation of osteochondritis dissecans of the knee. Clinical, magnetic resonance imaging, and arthroscopic follow-up. Am J Sports Med. 2005;33(10):1499–1504. doi: 10.1177/0363546505274717. [DOI] [PubMed] [Google Scholar]
- 18.Outerbridge HK, Outerbridge RE, Smith DE. Osteochondral defects in the knee: a treatment using lateral patella autografts. Clin Orthop. 2000;377:145–151. doi: 10.1097/00003086-200008000-00020. [DOI] [PubMed] [Google Scholar]
- 19.Pappas AM. Osteochondrosis dissecans. Clin Orthop. 1981;158:59–69. [PubMed] [Google Scholar]
- 20.Smillie IS. Treatment of osteochondritis dissecans. J Bone Joint Surg Br. 1957;39:248–260. doi: 10.1302/0301-620X.39B2.248. [DOI] [PubMed] [Google Scholar]
- 21.Tuompo P, Arvela V, Partio EK, Rokkanen P. Osteochondritis dissecans of the knee fixed with biodegradable self-reinforced polyglycolide and polylactide rods in 24 patients. Int Orthop. 1997;21:355–360. doi: 10.1007/s002640050184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thomson NL. Osteochondritis dissecans and osteochondral fragments managed by Herbert compression screw fixation. Clin Orthop Relat Res. 1987;224:71–78. [PubMed] [Google Scholar]
- 23.Versier G, Breda R. Traitement chirurgicale par fixation. Rev Chir Orthop. 2006;92:2S113–2S117. [Google Scholar]
- 24.Wagner H. Traitement opératoire de l’ostéochondrite disséquante, cause de l’arthrite déformante du genou. Rev Chir Orthop. 1964;50:335–352. [PubMed] [Google Scholar]