Abstract
The objective of this study is to report the clinical and radiological long-term follow-up evaluation of young patients arthroscopically treated for anterior tibial eminence fracture. Ten patients (mean age: 13.5 years) were treated between 1992 and 2006. At follow-up they were clinically and radiologically evaluated. Moreover, they underwent assessment with the International Knee Documentation Committee (IKDC) forms, Lysholm and Tegner knee scales and measurement with the KT-1000 arthrometer. At a mean follow-up of 85.8 months, all of the patients reported a subjective good-excellent outcome. Objectively, the Lachman test was negative in seven patients and positive in three patients; six patients (60%) registered a slight (+) to mild (++) pivot-glide test. The mean value of KT-1000 arthrometer measurements was 3 mm; all knee scales showed satisfactory results. Radiological exam always showed good healing of the fracture. Fractures of the tibial spine often lead to anterior and rotational knee laxity. However, despite this instrumental finding, patients usually do not report any type of restriction in their functional or sports activities.
Résumé
Le but de cette étude est de rapporter le suivi clinique et radiologique à long terme de jeunes patients traités par arthroscopie pour fracture des épines tibiales. 10 patients (d’âge moyen de 13,5 ans) ont été traités entre 1992 et 2006 et évalués sur le plan clinique et radiologique par IKDC, par l’échelle de Lysholm et de Tegner ainsi qu’avec une évaluation avec le KT-1000. Après un suivi moyen de 85,8 mois, tous les patients présentent un excellent résultat sur le plan clinique. Objectivement, le test de Lachman reste négatif pour 7 patients et positif pour 3 patients. 6 patients (60%) ont un pivot shift léger (+) et moyen (++). Le tiroir antérieur évalué par le KT-1000 était en moyenne de 3 mm. Toutes les évaluations par les échelles cliniques sont satisfaisantes de même sur le plan radiologique avec une bonne consolidation de la fracture. En conclusion, la fracture des épines tibiales peut laisser une petite laxité antérieure et rotatoire, cependant, malgré ces constatations, les résultats cliniques restent tout à fait satisfaisants et n’entraînent aucune restriction pour les activités sportives de même sur le plan fonctionnel.
Introduction
Tibial eminence fractures are typical of early age and they are generally considered analogous to the anterior cruciate ligament (ACL) rupture in the adult [4, 14, 15]. Typically they occur in children between eight and 14 years of age as a consequence of a fall from a bicycle or from a motorcycle [4, 16, 20].
The type of mechanism involved in tibial spine fractures is usually the same as that involved in a complete ACL rupture in an adult. It is commonly believed [14, 15, 23] that this phenomenon is due to the higher fragility of the tibial eminence (not yet completely ossified in the young) compared to the ACL fibres; in addition, Noyes et al. [18] proposed that this kind of injury could even be due to the very high elasticity of the ligaments in childhood. Indeed, from a biomechanical point of view, the growing metaphysis seems to have about one third of the resistance of the ligaments.
The goal of the treatment is to obtain an anatomical reduction of the tibial eminence. In theory an over-reduction should be avoided to prevent the risks of excessive tension of the ACL and a loss of mobility of the knee [10]; likewise, an inadequate repositioning of the tibial spine could lead to knee instability. However, between these two possibilities, some authors have stated that a certain elongation of all the fibres of the ACL takes place in all cases, thus leading one to assume that an over-reduction could be wiser to perform.
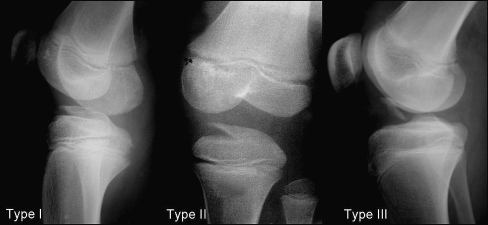
The most common type of classification used for these fractures was described in 1959 by Meyers and McKeever [14, 15] with three different types of fractures (Fig. 1); in 1997 Zaricznyj et al. [25] proposed a type IV fracture to better identify the comminuted fractures.
Fig. 1.
Tibial spine fracture classification by Meyers and McKeever
According to many authors [3, 14, 15], type I fractures can be successfully treated conservatively with immobilisation of the limb in full extension while types III and IV have to be treated surgically to gain a satisfactory reduction of the tibial eminence. Differing opinions exist about the best treatment to perform in cases of type II fractures. While some authors state that immobilisation in full extension or even in mild hyperextension can be sufficient to allow a satisfactory reduction of the fracture [11], other authors [1, 5, 8, 11] complain about the unsatisfactory results arising from such a conservative treatment, stating that an arthroscopic evaluation is always necessary to gain a suitable reduction as well as to evaluate and adequately treat any potential concomitant associated lesions.
Aim of the study
The aim of this study is to report the clinical and radiological mid- to long-term follow-up of patients surgically treated with arthroscopic reduction of an anterior tibial eminence fracture.
Materials and methods
At our institution ten patients (seven male and three female adolescents) were surgically treated for fractures of the anterior tibial eminence between November 1992 and October 2006. The mean age was 13.5 years (range: 12–15 years); the mean follow-up was 85.8 months (range: 20–188 months). Six patients (60%) experienced the injury during sports activities (three during skiing, one playing soccer, one playing professional soccer and one playing basketball), while in the other four patients (40%) the trauma was due to a fall from a motorcycle. According to Meyers and McKeever classification [14, 15], of these ten patients, there were three cases of type II fractures (30%) and seven cases of type III fractures (70%) (Table 1).
Table 1.
Main data of the study
| Men | 7 |
| Women | 3 |
| Mean age | 13,5 |
| Operated knee | 3 right, 7 left |
| Mean follow-up | 85,8 months (20–188) |
| Type of fracture | 3 type II, 7 type III |
At the physical examination, acute pain, mild to severe reduction of the range of motion (ROM) of the knee and inability to bear weight was detected in all cases. All of these patients with type II and type III fractures of the anterior tibial eminence were surgically treated by an arthroscopic technique.
Subjectively, all patients were clinically followed up with an accurate physical examination to verify the stability and the overall function of the knee. Objectively they underwent assessment with the most common international knee evaluation scales [Lysholm knee score, Tegner activity level and International Knee Documentation Committee (IKDC) forms] and the KT-1000 arthrometer measurement [manual maximum (MM) in a side-to-side (S/S) comparison]. Moreover, all of the patients underwent a radiological evaluation with an X-ray examination in two planes.
Statistical analysis was performed using a paired t-test. A value of less than 0.05 was considered significant.
Surgical procedure
All of the patients considered in this study were treated surgically with an arthroscopically assisted reduction and fixation of the bone fragment using reabsorbable polydioxanone (PDS) sutures. The mean time between the trauma and the surgical procedure was three days (range: 2–4 days).
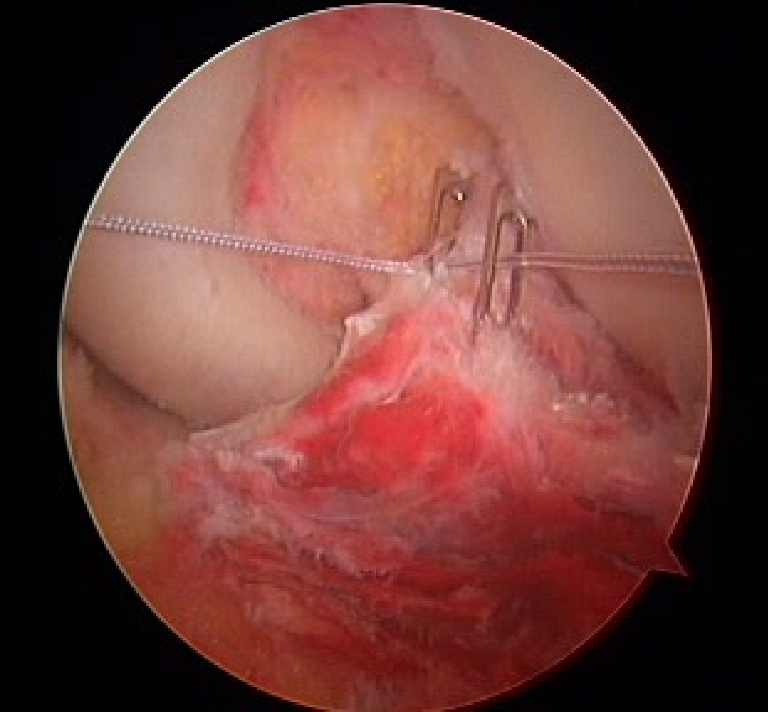
The first step of the operation consisted in all cases of an arthroscopic débridement of the fracture in order to sufficiently visualise the bone fragment, stage the type of fracture and to determine where to insert the Kirschner wires (Fig. 2). Particular attention was always focused on any associated chondral or meniscal lesions.
Fig. 2.

Arthroscopic view of a type III tibial spine fracture
An incision of about 1 cm in length was made over the metaphyseal plate of the tibia: number two fenestrated K-wires were then introduced into the proximal third of the tibia at the tibial insertion of the ACL. The growing cartilage was only minutely damaged by the passage of such small hardware. Through the hole at the extremity of one of the two K-wires, a PDS suture was introduced into the joint and subsequently passed through the second K-wire hole (Fig. 3); the suture was then pulled through the joint upon removal of the K-wires. The osteochondral fragment was consequently fixed by pulling the two sutures and tightening them tightly together outside the proximal third of the tibia (Fig. 4). From time to time, the PDS suture was passed around the ACL before being pulled out of the knee joint. After fixation of the bone fragment, the knee stability was always evaluated in order to verify any residual laxity of the joint.
Fig. 3.
Passage of the PDS suture through the two K-wire holes
Fig. 4.
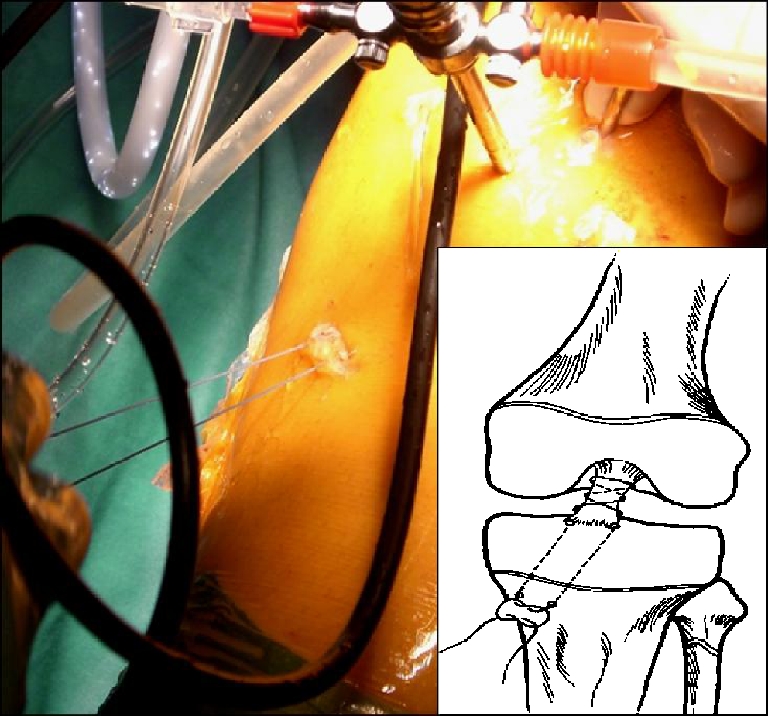
PDS suture out of the proximal third of the tibia ready to be tightened under arthroscopic visualisation
Post-operative rehabilitation protocol
The inferior limb was placed in a full extension brace, with the instruction to avoid weight-bearing for the first two weeks. Isometric exercises for quadriceps strengthening and hamstrings stretching protocol were started by the second post-operative day.
From the second to the fourth post-operative week, with the limb always locked in full extension, progressive weight-bearing was allowed, as tolerated by the patient. After the first post-operative month, the brace was removed and a careful rehabilitation protocol was started to regain a complete ROM and to further strengthen the quadriceps muscular tone. Return to sports activity was never allowed before the fifth post-operative month.
Results
At a mean follow-up of 85.8 months, all ten patients were clinically and radiologically evaluated.
Subjectively, six patients (60%) reported an excellent outcome and four patients (40%) reported a good result; no one reported fair or poor results. The ROM registered was complete (in a S/S evaluation) in all cases with a complete recovery of both flexion and extension.
Objectively, the Lachman test was negative (−) in seven patients, while the other three patients registered a positive (+) Lachman test; these same three patients also registered a mild (++) pivot-glide test, while three other patients with a negative Lachman test registered a slight (+) positive pivot-glide test.
The results of the international knee evaluation scales used showed an overall satisfactory outcome of the surgical procedure performed, as shown in Table 2.
Table 2.
Analytic results of the knee evaluation scales used and KT-1000 measurements
| Patient | Sex | Age (years) | Cause of injury | Follow-up | Lachman | Jerk | KT-1000 | Tegner | Lysholm | Sub. IKDC | Obj. IKDC |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 14 | Soccer | 51 | + | ++ | 6 | 9–9 | 99 | 94 | C |
| 2 | M | 14 | Motorcycle | 53 | + | ++ | 6 | 7–7 | 100 | 95 | C |
| 3 | M | 12 | Ski | 28 | – | – | 4 | 6–3 | 95 | 93 | B |
| 4 | M | 13 | Basketball | 98 | – | + | 3 | 6–6 | 99 | 94 | B |
| 5 | M | 13 | Ski | 109 | – | – | 1 | 7–7 | 94 | 85 | A |
| 6 | F | 15 | Motorcycle | 188 | – | – | 1 | 3–3 | 94 | 90 | A |
| 7 | M | 13 | Motorcycle | 100 | – | – | 1 | 8–7 | 97 | 91 | A |
| 8 | F | 14 | Ski | 113 | – | + | 1 | 6–6 | 94 | 93 | B |
| 9 | M | 13 | Soccer | 98 | + | ++ | 6 | 7–7 | 97 | 91 | C |
| 10 | F | 14 | Motorcycle | 20 | – | + | 1 | 7–6 | 90 | 98 | B |
The mean value of the KT-1000 arthrometric measurements (S/S) was 3 mm post-operatively. In particular, patients who registered a mild (++) pivot-glide test always registered a value of 6.0 mm, while patients with slight (+) or negative (−) pivot-glide test had a mean of 1.7 mm (range: 1–4 mm) (Table 2).
No concomitant meniscal or chondral lesions were ever detected during the surgical procedures.
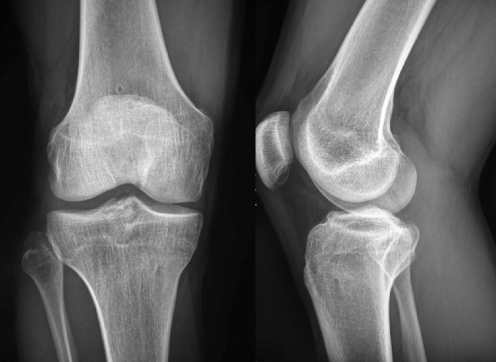
Radiological examinations did not show any type of enlargement of the tibial eminence or as any other kind of malunion of the tibial fracture in the S/S evaluation: indeed, the shape of the tibial eminences appeared to be similar to the contralateral side in all cases, therefore showing a satisfactory consolidation of the fracture (Figs. 5 and 6, pre-operative and post-operative X-rays, respectively, of the same patient).
Fig. 5.
Pre-operative X-ray of a patient with a type III fracture
Fig. 6.
Follow-up X-ray at 98 months
No cases of intra- or post-operative complications were ever detected. All ten patients were able to return to their pre-injury activity levels.
Discussion
Although a few studies have shown no difference in outcome of displaced tibial spine fractures treated conservatively versus surgically [2, 4, 17, 23, 24], many other authors advocate the surgical option so as to treat possible associated lesions, like meniscal tears or osteochondral injuries [12, 13]. Moreover, they support the opinion that the surgical option facilitates a more satisfactory reduction of the fracture, thus avoiding the possible risk of a meniscal entrapment under the fractured tibial eminence or a possible healing of the fracture in a non-anatomical position, with the consequence of further instability or loss of extension of the knee [4, 6, 13, 19].
Indeed, fractures of the tibial eminence in the developing years often lead to an anterior knee laxity, regardless of the type of treatment performed [1, 2, 7, 22–24].
At a mean follow-up of seven years, Smith [22] showed how in all patients, both conservatively and surgically treated, there was a residual laxity of the knee: as a consequence, they stated that, since the tibial spine had consolidated in the right position, the residual laxity could be attributed to the elongation of the ACL fibres which occurs at the time of the trauma. However, this theory is in contrast with the theory that during physical development the ligaments are more resistant than the underlying osteochondral tibial spine. Noyes et al. [18], in a biomechanical study, confirmed the pathogenetic mechanism proposed by Smith showing the occurrence of an elongation of more than 50% of the original length of the fibres of the ACL before the tibial fracture subsequently happened. Therefore, even though the ACL ligament appeared to maintain its continuity externally, the authors stated that it is very hard to adequately restore the pre-traumatic stability of the knee. This could be one of the possible reasons for the unsatisfactory outcomes of this type of pathological condition in terms of post-operative anterior knee stability.
Grönkvist et al. [4] have shown how continued growth of the tibial bone can compensate for the residual post-operative anterior knee laxity arising from the elongation of the ligament fibres. Consequently, the authors stated that the younger the patient the better the outcome. These results were successively confirmed by Hunter and Willis [5] and by Janarv and Hirsch [7].
The results of our study are consistent with the above-mentioned studies, since our analytic evaluation shows better results in patients younger than 13 years of age, in terms of improved knee stability; however, these better results were not statistically significant when compared to the results of the patients older than 13 years (p > 0.05).
Moreover, it has been widely shown how the residual laxity differs depending on the type of fracture treated. For instance, Baxter and Wiley [2] showed how patients with a type I fracture [14, 15] reported a minimal residual laxity, while patients with type II or type III fractures registered a higher post-operative laxity. In accordance with these studies, our results confirm this phenomenon, since the worst results in our study occurred specifically in patients with type III fractures. Indeed, three patients of the three who registered a type II fracture (100%) reported a negative (−) Lachman test; whereas, of the remaining seven patients with a type III fracture, three patients (42.8%) had a positive (+) Lachman test. Post-operative KT-1000 arthrometer evaluation confirmed our clinical results: patients with a type II fracture showed a mean of 2.7 mm (S/S) at MM, while patients with a type III fracture showed a mean of 3.3 mm (S/S).
However, among the patients with these two types of fractures, no statistically significant differences were detected. Unfortunately, in the group of patients of our study, no cases of type I fractures were detected, so we were not able to make a comparison regarding the post-operative knee stability in treatment of type I fractures.
Nevertheless, it is important to underline how the laxity clinically detected by all of the above-mentioned authors, and even confirmed in this study, was always an instrumental result, without a corresponding clinical or subjective feeling of real instability [1, 2, 6, 7, 20, 22–24]. Indeed, at final follow-up, all of the patients reported a good or excellent feeling of stability of the operated knee, without any kind of restriction in practising their daily or sports activities. All of the patients returned to their pre-injury sports activity and denied any kind of restriction.
In a four-year follow-up study, Willis et al. [24] showed that, despite the objective residual knee laxity, only 10% of their patients reported mild pain and no one reported any type of instability. Similarly, Kocher et al. [9] and Janarv et al. [6] reported a post-operative laxity in four of six patients (66.6%) and in 38% of 61 patients, respectively, with an excellent clinical outcome.
This lack of subjective instability could be due to both the integrity of the nervous fibres along the ACL ligament and the integrity of the neuromuscular feedback. Moreover, despite the possible elongation occurring in the ACL at the moment of the trauma, it is plausible that the presence of all of the fibres and their overall integrity allow the ACL to adequately accomplish its function.
An interesting finding arising from the analysis of our study, which differs from that found in some previously published studies [2, 20, 22], is the presence of a rotational knee laxity often associated with the anterior laxity. Indeed, three patients (30%) showed a positive (++) pivot-glide test along with a positive Lachman test, while another three patients (30%) showed merely a positive (+) pivot-glide test without a concomitant anterior drawer test. In theory, the presence of this rotational instability could be due to a concomitant peripheral knee capsular and ligamentous injury of the knee, perhaps not detected during the arthroscopic treatment. Unfortunately, we did not perform any type of magnetic resonance imaging study in our group of patients before the surgical treatment, so we are not able to retrospectively verify any kind of possible associated peripheral knee lesion.
Moreover, in our study, at the final follow-up, we did not find any reduction of the ROM, in either flexion or extension [2, 21]. The radiographs did not show any enlargement of the tibial eminence, probably confirming how a satisfactory reduction of the fracture can allow a complete recovery of the ROM without giving any guarantee regarding the post-operative knee stability.
Conclusions
Fractures of the anterior tibial spine often lead to an anterior knee laxity, despite the type of treatment performed. However, subjectively, this type of laxity was never registered as a discomfort and never led patients to restrict their functional or sports activities.
In contrast to the results reported by other authors, our study often registered a high percentage of residual rotational knee laxity, regardless of concomitant anterior knee laxity. None of the patients of our study exhibited lack of extension during physical examination, thus differing from the other studies.
References
- 1.Accousti WK, Willis RB. Tibial eminence fractures. Orthop Clin North Am. 2003;34:365–375. doi: 10.1016/S0030-5898(03)00004-X. [DOI] [PubMed] [Google Scholar]
- 2.Baxter MP, Wiley JJ. Fractures of the tibial spine in children. An evaluation of knee stability. J Bone Joint Surg Br. 1988;70:228–230. doi: 10.1302/0301-620X.70B2.3346294. [DOI] [PubMed] [Google Scholar]
- 3.Canale ST. Fractures and dislocation in children. Campbell’s operative orthopaedics. 9. Philadelphia: Mosby; 1998. pp. 2488–2490. [Google Scholar]
- 4.Grönkvist H, Hirsch G, Johansson L. Fracture of the anterior tibial spine in children. J Pediatr Orthop. 1984;4:465–468. doi: 10.1097/01241398-198408000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Hunter RE, Willis JA. Arthroscopic fixation of avulsion fractures of the tibial eminence: technique and outcome. Arthroscopy. 2004;20:113–121. doi: 10.1016/j.arthro.2003.11.028. [DOI] [PubMed] [Google Scholar]
- 6.Janarv PM, Westblad P, Johansson C, Hirsch G. Long-term follow-up of anterior tibial spine fractures in children. J Pediatr Orthop. 1995;15:63–68. doi: 10.1097/01241398-199501000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Janarv PM, Hirsch G. Growth influences knee laxity after anterior tibial spine fracture: a study on rabbits. Acta Orthop Scand. 2001;72:173–180. doi: 10.1080/000164701317323435. [DOI] [PubMed] [Google Scholar]
- 8.Kocher MS, Micheli LJ, Gerbino P, et al. Tibial eminence fractures in children: prevalence of meniscal entrapment. Am J Sports Med. 2003;31:404–407. doi: 10.1177/03635465030310031301. [DOI] [PubMed] [Google Scholar]
- 9.Kocher MS, Foreman ES, Micheli LJ. Laxity and functional outcome after arthroscopic reduction and internal fixation of displaced tibial spine fractures in children. Arthroscopy. 2003;19:1085–1090. doi: 10.1016/j.arthro.2003.10.014. [DOI] [PubMed] [Google Scholar]
- 10.Lubowitz JH, Grauer JD. Arthroscopic treatment of anterior cruciate ligament avulsion. Clin Orthop Relat Res. 1993;294:242–246. [PubMed] [Google Scholar]
- 11.Lubowitz JH, Elson WS, Guttmann D. Part II: arthroscopic treatment of tibial plateau fractures: intercondylar eminence fractures. Arthroscopy. 2005;21:86–92. doi: 10.1016/j.arthro.2004.09.031. [DOI] [PubMed] [Google Scholar]
- 12.Mah JY, Adili A, Otsuka NY, Ogilvie R. Follow-up study of arthroscopic reduction and fixation of type III tibial-eminence fractures. J Pediatr Orthop. 1998;18:475–477. doi: 10.1097/00004694-199807000-00014. [DOI] [PubMed] [Google Scholar]
- 13.McLennan JG. Lessons learned after second-look arthroscopy in type III fractures of the tibial spine. J Pediatr Orthop. 1995;15:59–62. doi: 10.1097/01241398-199501000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Meyers MH, McKeever FM. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am. 1959;41-A:209–222. [PubMed] [Google Scholar]
- 15.Meyers MH, McKeever FM. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am. 1970;52:1677–1684. [PubMed] [Google Scholar]
- 16.Micheli LJ, Kocher MS (2006) The pediatric and adolescent knee, Chap. 26. Saunders, Philadelphia, pp 400–420
- 17.Mulhall KJ, Dowdall J, Grannell M, McCabe JP. Tibial spine fractures: an analysis of outcome in surgically treated type III injuries. Injury. 1999;30:289–292. doi: 10.1016/S0020-1383(99)00084-4. [DOI] [PubMed] [Google Scholar]
- 18.Noyes FR, DeLucas JL, Torvik PJ. Biomechanics of anterior cruciate ligament failure: an analysis of strain-rate sensitivity and mechanisms of failure in primates. J Bone Joint Surg Am. 1974;56:236–253. [PubMed] [Google Scholar]
- 19.Oostvogel HJ, Klasen HJ, Reddingius RE. Fractures of the intercondylar eminence in children and adolescents. Arch Orthop Trauma Surg. 1988;107:242–247. doi: 10.1007/BF00449677. [DOI] [PubMed] [Google Scholar]
- 20.Owens BD, Crane GK, Plante T, Busconi BD. Treatment of type III tibial intercondylar eminence fractures in skeletally immature athletes. Am J Orthop. 2003;32:103–105. [PubMed] [Google Scholar]
- 21.Roberts JM, Lovell WW. Fractures of the intercondylar eminence of the tibia. J Bone Joint Surg Am. 1970;52:827. [PubMed] [Google Scholar]
- 22.Smith JB. Knee instability after fractures of the intercondylar eminence of the tibia. J Pediatr Orthop. 1984;4:462–464. doi: 10.1097/01241398-198408000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Wiley JJ, Baxter MP. Tibial spine fractures in children. Clin Orthop Relat Res. 1990;255:54–60. [PubMed] [Google Scholar]
- 24.Willis RB, Blokker C, Stoll TM, et al. Long-term follow-up of anterior tibial eminence fractures. J Pediatr Orthop. 1993;13:361–364. doi: 10.1097/01241398-199305000-00016. [DOI] [PubMed] [Google Scholar]
- 25.Zaricznyj B. Avulsion fracture of the tibial eminence: treatment by open reduction and pinning. J Bone Joint Surg Am. 1977;59:1111–1114. [PubMed] [Google Scholar]