Abstract
The aim of this study was to compare the component positioning of Birmingham Hip Resurfacings implanted through a posterolateral approach with those inserted via a direct lateral approach. Sixty-four hip resurfacings for osteoarthritis were carried out by a single surgeon: 23 through a direct lateral approach and 41 through a posterolateral approach. No significant differences in implant survival, Oxford Hip Scores or complications were found. The mean abduction angle for the acetabular component was lower (p < 0.007) with a posterior approach (mean: 37.5°; range 26–50°) than the lateral approach (mean: 43°; range 30–56°). There was no significant difference in stem orientation, either in flexion/extension or varus/valgus, between the two groups. This study demonstrates that components can be implanted in an acceptable orientation through either approach but that the posterior approach results in greater closure of the acetabular component.
Résumé
Le but de cette étude est de comparer la position de l’implant de resurfaçage de la hanche de type Birmingham, mis en place après abord postéro externe comparé à la voie directe latérale. 64 resurfaçages de hanche pour coxarthrose ont été réalisés par un seul chirurgien, 23 par voies latérales et 41 par voies postéro latérales. Il n’y a pas de différence significative dans la survie de l’implant, ni dans le score d’Oxford et les complications. La position du composant acétabulaire est beaucoup plus basse (p < 0.007) par abord postérieur (angle moyen 37.5° entre 26 à 50) que par voie latérale (angle moyen 43° entre 30 à 56). Il n’y a pas de différence significative dans l’orientation de la pièce fémorale ni en flexion, ni en extension et ni en varus ni en valgus. Cette étude démontre que les composants peuvent être implantés de façon acceptable par une des deux abords mais, l’abord postérieur entraîne une position plus basse de l’implant acétabulaire.
Introduction
The last ten years has seen a resurgence of interest in hip resurfacing techniques. The developers of the modern metal-on-metal hip resurfacing have favoured the posterolateral approach for implantation [1, 20]. Many surgeons prefer to perform arthroplasty of the hip through a direct lateral approach [9, 12, 18] and, therefore, have adopted this approach for resurfacing [9, 13]. Debate continues regarding the advantages and disadvantages of the two approaches.
Hip resurfacing presents one major technical difficulty that conventional total hip replacement does not—that of preparing the acetabulum while the femoral head remains in situ. The results of different approaches should be reproducible without any increase in complications. There has been no research published on the effect of surgical approach on implant positioning for hip resurfacing.
A number of authors have raised concerns on the effect of surgical approach on blood supply to the femoral head following resurfacing [2, 7, 21] but have not looked at the effect on implant position. This study was carried out to compare the direct lateral approach with the posterolateral approach for metal-on-metal hip resurfacing, with the aim of answering the question: “Does the surgical approach used for hip resurfacing affect implant positioning?”
Materials and methods
The study period was from January 2000 to January 2007. All hip resurfacings performed by the senior author at a single institution during this period were reviewed. The study was limited to cases of osteoarthritis. Of the 78 cases identified, there were 64 (7 bilateral, a total of 57 patients) for whom full operative reports and radiological records could be retrieved. The 14 cases in which complete data was not available were excluded from further analysis. There were 23 cases (18 males and 5 females) performed on through a direct lateral approach and 41 (26 male and 15 females) via a posterolateral approach. The senior author initially used the posterior approach (2000 to November 2003), then the lateral approach (December 2003 to September 2004), reverting back to the posterior approach and, from November 2005, has used the lateral approach. The mean age at operation was 60 years (range 51 to 70) for the direct lateral group and 53 years (range 28 to 71) for the posterolateral group.
The Birmingham Hip Resurfacing (Smith and Nephew, London, UK) was used in all cases. Surgery was carried out in a lateral position in a laminar airflow theatre using an exhaust suit system. Antibiotic prophylaxis was given pre-operatively and was followed by two post-operative doses. Thromboprophylaxis was administered by TED stockings and mechanical foot pumps. Post-operative rehabilitation regimens were the same for both groups with full weight bearing on day one post-operatively as comfort allowed.
In cases performed via a posterolateral approach, the fascia lata was divided, followed by splitting of the gluteus maximus in the line of its fibres. The external rotators were reflected from the piriformis to the gluteus maximus. A posterior capsulectomy was performed and the femoral head dislocated. The head was further delivered into the wound by an anterior capsular release. After reduction, the posterior repair was carried out with Vicryl sutures. In those cases where the Hardinge lateral approach was used [9], the joint capsule was incised and a capsular release was performed; closure was performed with Vicryl sutures.
Following the initial surgical exposure, the same technique was used for bone preparation and implantation in both groups. First, the femoral head was prepared. The manufacturer’s targeting devices were not used. Diathermy was used to make a “cross-hair” on the femoral head, with lines marking the centre of the femoral neck in both the antero-posterior and lateral planes. The guide wire was inserted “free hand” through this mark. The femoral component was implanted with Simplex bone cement (Stryker, Newbury, Berkshire, UK). The acetabulum was prepared as recommended by the manufacturer using sequential reaming with hemispherical acetabular reamers. The acetabulum was under-reamed by 2 mm relative to the definitive acetabular component.
The Oxford Hip Score (OHS) [5] questionnaire, a subjective functional scoring system, was completed by the patient pre-operatively. In May 2007, patients were contacted by postal or telephone questionnaire to complete a second OHS. At this stage, it was confirmed whether they had suffered any complications or undergone further surgery. Statistical analysis was carried out using MedCalc software (MedCalc Software, Broekstraat 52, 9030, Mariakerke, Belgium) with confidence intervals derived from the two-sample t-test for continuous variables, the chi-squared test for dichotomous variables and the Mann-Whitney test used where appropriate.
The initial post-operative antero-posterior and lateral radiographs of the operated hips were reviewed. The following parameters were recorded from the antero-posterior radiograph: seating of the acetabular component, abduction angle of the acetabular component, notching of the femoral neck, varus or valgus positioning of the femoral component (relative to the patient’s femoral neck). The abduction angle was measured by drawing a line across the tear drops and bisecting this with a line across the open face of the acetabular component. The varus/valgus angulation was measured by drawing a line down the axis of the femur bisected by: (1) a line down the axis of the stem of the femoral component (for component stem-shaft orientation) and (2) lines drawn along the superior and inferior aspects of the femoral neck, which allowed a line to be drawn equidistant to these two lines, creating a line down the centre of the femoral neck (for anatomical neck-shaft orientation). The lateral radiographs were assessed for: notching of the femoral neck and flexion or extension of the femoral component. All radiographs were independently reviewed by two of the authors, blinded to the surgical approach used. The inter-observer variability in observations was recorded. In those cases where the observers did not agree, repeat measurement was carried out in the presence of both observers (Figs. 1, 2 and 3).
Fig. 1.
Measurement of the abduction angle of the acetabular component
Fig. 2.
Measurement of the varus/valgus orientation of the femoral component
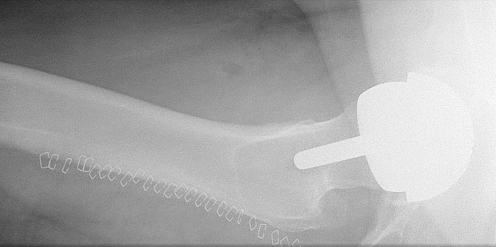
Fig. 3.
Post-operative radiograph showing the tip of the femoral component in the central one-third of the femoral neck
Results
The posterior approach group contained a greater proportion of female patients and was younger than the anterolateral group (p < 0.005). Pre-operative Oxford Hip Scores were available in 51 cases; 57 of the 63 surviving cases completed a follow-up OHS (one patient has undergone revision to a total hip replacement, carried out for ongoing pain in the hip; no evidence of infection/avascular necrosis/loosening was found but symptoms were resolved by revision). In three patients, lateral radiographs were not available for review; antero-posterior radiographs were available in all cases. There has been one death in the posterior approach group unrelated to the surgery. One documented deep vein thrombosis occurred in the posterior group. There have been no nerve palsies or deep infections.
Using the 51 cases where complete pre-operative and post-operative Oxford Hip Scores were available, analysis was performed. The pre-operative mean Oxford Hip Score for the direct lateral group was 42.5 (range 18–57) and 44 (range 16–60) for the posterolateral group. No significant difference between the two groups was found. At an average follow-up of 3 years 0 months (range 4 months to 6 years and 1 month), there was no significant difference in the Oxford Hip Scores: direct lateral 20 (range 13–40) and posterolateral 20 (range 12–45).
Radiology
Three acetabular components inserted through the lateral approach were not fully seated, nor were two from the posterior approach. There was a significant difference in the mean abduction angle of the acetabular components (p < 0.007). Mean abduction via the posterior approach was 37.5° (range 26–50°) and 43° (range 30–56°) through the lateral approach. Seventy percent (70%) of the stems inserted through the lateral approach were neutral or in valgus (>10° valgus: n = 1; 0–10° valgus: n = 15; 1–5° varus: n = 5; >5° varus: n = 2), as compared to 74% through the posterior approach (>10° valgus: n = 4; 0–10° valgus: n = 28; 1–5° varus: n = 8; >5° varus: n = 1). Two stems in the lateral group were in more than 5° of varus, as was one in the posterior group. When comparing the varus/valgus angle of the stems, there was no statistically significant difference between the two groups. The Kappa value for observation of the abduction angle for the two reviewers was 0.84 and 0.76 for the varus/valgus angulation.
There was no significant difference in the flexion or extension of the femoral component. On review of the lateral radiographs, the stem tips of 73% of femoral implants inserted through a lateral approach were within the middle third of the neck (three anterior, three posterior and 16 middle; radiograph unavailable for one case), compared with 64% for the posterior approach (14 anterior, 0 posterior and 25 middle; radiographs unavailable for two). There was minimal inferior notching in two cases performed through the posterior approach and zero through the lateral approach.
Discussion
Direct lateral approaches are used for the majority of total hip replacements in the United Kingdom [13]. They offer low dislocation rates in high-risk patients and a low incidence of leg length discrepancy [15]. Wagner advocated this approach in hip resurfacing and noted that it offered excellent visualisation of the femoral head and acetabulum [21]. However, the posterolateral approach is currently the most frequently used for hip resurfacing [13] but approximately one quarter of resurfacings in the United Kingdom are implanted through approaches other than this [13]. Therefore, it is important to know if approaches other than the posterior approach offer reliable implant positioning when compared to results published for the recommended technique [4, 20]. The posterior approach has the advantage of conserving the abductor group of muscles and is not proven to carry an excessive risk of dislocation in total hip replacement, provided an adequate posterior repair is performed [11]. Dislocation appears to be less common in hip resurfacing than in conventional total hip replacement [4, 20].
Over the last ten years, there has been a resurgence of interest in hip resurfacing techniques. There has also been renewed interest in the role of surgical approach on blood supply to the femoral head. Studies on this subject have been carried out by Wagner [21] and Freeman [7] and more recently by Beaulé et al. [2]. The majority of this work relates to the effect of surgical approach and femoral preparation on branches of the medial femoral circumflex artery. Advocates of the direct lateral approaches point out that the terminal ascending branches of the medial circumflex femoral artery are not disrupted and avascular necrosis of the head of the femur is rare through this approach [3, 6]. Concerns have been raised of a potential insult to these vessels during a posterior approach [8, 17]. It has been demonstrated by using surrogate markers that bone perfusion is reduced when a posterolateral approach has been used compared with a direct lateral approach [10]. Compensatory flow from inferior retinacular vessels is feasible and it remains to be shown whether any disruption is irreversible [14, 19]. A detrimental clinical effect has not been demonstrated in other published series [1, 16, 20]. Debate continues as to the effect of surgical exposure on vascularity but there has been no research published on the effect of surgical approach on implant positioning.
Hip resurfacing presents additional challenges to the arthroplasty surgeon when compared with conventional total hip replacement, in particular, the potential for the femoral head and neck to act as an obstacle to adequate acetabular preparation, cup orientation and impaction. This study is limited by the lack of comparison to results achievable using an anterior approach to hip arthroplasty. Figures from the National Joint Registry of England and Wales 3rd Annual Report show that 9% of resurfacings were implanted through an anterior approach [13]. The study was performed to ascertain whether there was any detriment to implant orientation and insertion through the lateral approach as compared to the posterior approach. The alternation between the two approaches during the study period limits the effect of a learning curve on the results, which would have been present if all cases performed through one approach had been followed by all cases via the second approach. An analysis of function as measured by the Oxford Hip Score was also recorded to further compare the two approaches. Despite concerns about rehabilitation following a direct lateral approach, both groups had excellent return to function following Birmingham Hip Resurfacing. It was the operating surgeon’s intent to place the acetabular component in the same amount of abduction through both approaches. Although the mean abduction angle achieved was acceptable in both groups, it was demonstrated that the acetabular component was implanted in a more closed orientation using a posterior approach. The authors postulate that the presence of the femoral head and neck in the line of preparation and insertion of the acetabular component, when using the lateral approach, resulted in greater abduction. It may be possible to reduce this affect by using the curved introducers now available from the manufacturer.
The designers of the Birmingham Hip Resurfacing continue to advocate a posterolateral approach. This study demonstrates that acceptable implant orientation can be achieved using a lateral approach but attention must be given to the orientation of the acetabular component.
Acknowledgments
Conflict of interest statement No benefits in any form have been received from a commercial party directly or indirectly related to the subject of this article.
References
- 1.Amstutz HC, Beaulé PE, Dorey FJ, Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg Am. 2004;86(1):28–39. [PubMed] [Google Scholar]
- 2.Beaulé PE, Campbell P, Shim P. Femoral head blood flow during hip resurfacing. Clin Orthop Relat Res. 2007;456:148–152. doi: 10.1097/01.blo.0000238865.77109.af. [DOI] [PubMed] [Google Scholar]
- 3.Bradley GW, Freeman MA, Revell PA. Resurfacing arthroplasty. Femoral head viability. Clin Orthop Relat Res. 1987;220:137–141. [PubMed] [Google Scholar]
- 4.Daniel J, Pynsent PB, McMinn DJW. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86(2):177–184. doi: 10.1302/0301-620X.86B2.14600. [DOI] [PubMed] [Google Scholar]
- 5.Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78(2):185–190. [PubMed] [Google Scholar]
- 6.Forrest N, Welch A, Murray DA, Schweiger L, Hutchison J, Ashcroft GP. Femoral head viability after Birmingham resurfacing hip arthroplasty: assessment with use of [18f] fluoride positron emission tomography. J Bone Joint Surg Am. 2006;88(Suppl 3):84–89. doi: 10.2106/JBJS.F.00877. [DOI] [PubMed] [Google Scholar]
- 7.Freeman MA. Some anatomical and mechanical considerations relevant to the surface replacement of the femoral head. Clin Orthop Relat Res. 1978;134:19–24. [PubMed] [Google Scholar]
- 8.Gautier E, Ganz K, Krügel N, Gill T, Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82(5):679–683. doi: 10.1302/0301-620X.82B5.10426. [DOI] [PubMed] [Google Scholar]
- 9.Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg Br. 1982;64(1):17–19. doi: 10.1302/0301-620X.64B1.7068713. [DOI] [PubMed] [Google Scholar]
- 10.Khan A, Yates P, Lovering A, Bannister GC, Spencer RF. The effect of surgical approach on blood flow to the femoral head during resurfacing. J Bone Joint Surg Br. 2007;89(1):21–25. doi: 10.1302/0301-620X.89B1.18330. [DOI] [PubMed] [Google Scholar]
- 11.Kwon MS, Kuskowski M, Mulhall KJ, Macaulay W, Brown TE, Saleh KJ. Does surgical approach affect total hip arthroplasty dislocation rates? Clin Orthop Relat Res. 2006;447:34–38. doi: 10.1097/01.blo.0000218746.84494.df. [DOI] [PubMed] [Google Scholar]
- 12.Minns RJ, Crawford RJ, Porter ML, Hardinge K. Muscle strength following total hip arthroplasty. A comparison of trochanteric osteotomy and the direct lateral approach. J Arthroplasty. 1993;8(6):625–627. doi: 10.1016/0883-5403(93)90010-2. [DOI] [PubMed] [Google Scholar]
- 13.NJR Steering Committee. National Joint Registry for England and Wales—3rd annual clinical report. February 2006. The NJR Centre, Hemel Hempstead, UK
- 14.Nötzli HP, Siebenrock KA, Hempfing A, Ramseier LE, Ganz R. Perfusion of the femoral head during surgical dislocation of the hip. Monitoring by laser Doppler flowmetry. J Bone Joint Surg Br. 2002;84(2):300–304. doi: 10.1302/0301-620X.84B2.12146. [DOI] [PubMed] [Google Scholar]
- 15.Pajarinen J, Savolainen V, Tulikoura I, Lindahl J, Hirvensalo E. Factors predisposing to dislocation of the Thompson hemiarthroplasty: 22 dislocations in 338 patients. Acta Orthop Scand. 2003;74(1):45–48. doi: 10.1080/00016470310013644. [DOI] [PubMed] [Google Scholar]
- 16.Pollard TCB, Baker RP, Eastaugh-Waring SJ, Bannister GC. Treatment of the young active patient with osteoarthritis of the hip. A five- to seven-year comparison of hybrid total hip arthroplasty and metal-on-metal resurfacing. J Bone Joint Surg Br. 2006;88(5):592–600. doi: 10.1302/0301-620X.88B5.17354. [DOI] [PubMed] [Google Scholar]
- 17.Steffen RT, Smith SR, Urban JPG, McLardy-Smith P, Beard DJ, Gill HS, Murray DW. The effect of hip resurfacing on oxygen concentration in the femoral head. J Bone Joint Surg Br. 2005;87(11):1468–1474. doi: 10.1302/0301-620X.87B11.16780. [DOI] [PubMed] [Google Scholar]
- 18.Stephenson PK, Freeman MA. Exposure of the hip using a modified anterolateral approach. J Arthroplasty. 1991;6(2):137–145. doi: 10.1016/s0883-5403(11)80008-2. [DOI] [PubMed] [Google Scholar]
- 19.Sugamoto K, Ochi T, Takahashi Y, Tamura T, Matsuoka T. Hemodynamic measurement in the femoral head using laser Doppler. Clin Orthop Relat Res. 1998;353:138–147. doi: 10.1097/00003086-199808000-00016. [DOI] [PubMed] [Google Scholar]
- 20.Treacy RBC, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty. A minimum follow-up of five years. J Bone Joint Surg Br. 2005;87(2):167–170. doi: 10.1302/0301-620X.87B2.15030. [DOI] [PubMed] [Google Scholar]
- 21.Wagner H. Surface replacement arthroplasty of the hip. Clin Orthop Relat Res. 1978;134:102–130. [PubMed] [Google Scholar]