Abstract
Classical ballet is an art form requiring extraordinary physical activity, characterised by rigorous training. These can lead to many overuse injuries arising from repetitive minor trauma. The purpose of this paper is to report our experience in the diagnosis and treatment of stress fractures at the base of the second and third metatarsal bones in young ballet dancers. We considered 150 trainee ballet dancers from the Ballet Schools of "Teatro Alla Scala" of Milan from 2005 to 2007. Nineteen of them presented with stress fractures of the base of the metatarsal bones. We treated 18 dancers with external shockwave therapy (ESWT) and one with pulsed electromagnetic fields (EMF) and low-intensity ultrasound (US); all patients were recommended rest. In all cases good results were obtained. The best approach to metatarsal stress fractures is to diagnose them early through clinical examination and then through X-ray and MRI. ESWT gave good results, with a relatively short time of rest from the patients’ activities and a return to dancing without pain.
Introduction
Classical ballet is a popular but physically high demanding activity. As most repetitive activities, overuse injuries are relatively common in classical ballet dancers. As reported by many authors, 50% of all sports injuries are secondary to overuse [1]. The most common overuse injuries involve the lower leg (20%), ankle (15%) and foot (15%) [1–3]. Overuse can alter the biological and biomechanical properties of the bone and its cellular composition, leading to a mismatch between overload and recovery. Two important risk factors can be distinguished, namely, intrinsic and extrinsic.
Intrinsic factors are related to the physical characteristics of the athlete and include malalignments, muscle imbalance, inflexibility, weakness and instability [4]. Some other factors may exist such as high longitudinal arch of the foot, leg-length inequality, and excessive forefoot varus [3]. Amenorrhea was found to be an important risk factor in the development of stress fractures in females [5], as reported also by Bennel [6, 7] and Marcus [8].
Extrinsic factors include poor technique, improper equipment, and improper changes in training [4, 9].
The most common overuse lesions of the foot are stress fractures and soft tissue problems. A stress fracture can be a partial or a complete interruption of the bone that results from a repeated force lower than the force required to fracture the bone in a single load [6]. Stress fractures located closer to the shaft of the metatarsal bones are very common overuse injuries in the general population, but stress fractures localised in the base of the second or third metatarsals are a prerogative of ballet dancers. Micheli et al. [10] first wrote about stress fractures at the base of the second metatarsal in ballerinas in 1985. The largest series was published in 1996 by O’Malley, who reported 64 fractures treated nonoperatively [11]. The extreme plantar flexion of the foot and ankle for en pointe position and the unique locking configuration of the second metatarsal and cuneiforms have been proposed as causes of this injury [10, 12, 13]. Frequently the diagnosis is delayed because the description of pain is ill defined, minimal swelling is present, physical examination findings are often indeterminable and plain radiography is usually negative [11]. In this paper, we describe our experience in the diagnosis and treatment of stress fractures at the base of the second and third metatarsals in young trainee ballet dancers.
Materials and methods
We considered 150 trainee ballet dancers (80 males, 70 females) belonging to the Ballet Schools of “Teatro Alla Scala” of Milan, aged between ten and 21 years. From September 2005 to September 2007, a database was created retrospectively by collecting clinical examinations and imaging studies of the dancers (informed consent had been previously obtained).
Nineteen dancers (nine males, ten females) presented stress fractures in the base of the metatarsal bones (Table 1). The average age of the patients was 16.4 years (range 14–20 years). All the males and seven female ballet dancers had a fracture of the second metatarsal base, while in only three female dancers the fracture was located in the third metatarsal base. All of them complained of gradual onset of pain and/or discomfort unilaterally in the metatarsal region, related to specific foot positions and increased training sessions. After 11 days (range 7–20 days), a standard radiograph was done. The radiographs were negative in ten cases (grade 1 in one dancer, grade 2 in nine dancers [11]), in eight cases they showed a cortical reaction (grade 3) and only in one case did we notice a stress fracture (grade 4). When a stress fracture was clinically suspected, an MRI was always performed. A CT scan was necessary only on patient no. 2, as the MRI showed a fracture line going through the metatarsal cartilage plate. A stress fracture and intramedullary oedema was always evident on MRI and CT scans. All patients were treated nonoperatively with rest and external shockwave therapy (ESWT). We use medium energy shock waves (Wolf Piezoson 300 lithotripter, with 6.5 MHz ultrasounds; 2,000 pulses 0.06–0.28 mJ/mm2, three to five times in a month), depending on clinical and anatomical factors, age of the dancers and type of stress fracture. Dancer no. 2 could not follow ESWT because the stress fracture passed through the growing cartilage of the second metatarsal. We recommended for him pulsed electromagnetic fields (EMF) and low-intensity ultrasound (US) [14, 15]. No cast or hard-sole shoes were required. Whilst the dancers followed the period of rest, they were allowed to perform stretching exercises and isometric exertion without weight bearing. This period generally lasted for three to five weeks after the diagnosis.
Table 1.
Patient characteristics
| Patient (gender) | Age (y) | Leg length R/L (cm) | Foot | Onset of symptoms | Time of Rx (days) | Rx aspect | MRIa | Treatment | Return to full activity after onset of the symptoms (weeks) |
|---|---|---|---|---|---|---|---|---|---|
| 1 (F) | 17 | 83/83 | Normal | Gradual | 7 | Normal | Grade 1 | ESWT | 5 |
| 2 (M) | 16 | 90.5/90.5 | Pronated | Gradual | 10 | Cortical reaction | Grade 3 (and CT) | US + EMF | 11 |
| 3 (M) | 20 | 88/89 | Cavus | Gradual | 20 | Cortical reaction | Grade 3 | ESWT | 8 |
| 4 (F) | 15 | 82/83 | Pronated | Gradual | 15 | Cortical reaction | Grade 3 | ESWT | 7 |
| 5 (F) | 16 | 85/85 | Pronated | Gradual | 10 | Normal | Grade 2 | ESWT | 6 |
| 6 (M) | 17 | 84/85 | Normal | Gradual | 12 | Cortical reaction | Grade 3 | ESWT | 8 |
| 7 (F) | 16 | 85/85 | Normal | Gradual | 7 | Cortical reaction | Grade 3 | ESWT | 7 |
| 8 (F) | 17 | 83/83 | Normal | Gradual | 9 | Normal | Grade 2 | ESWT | 5 |
| 9 (M) | 16 | 90.5/90.5 | Pronated | Gradual | 10 | Cortical reaction | Grade 3 | ESWT | 6 |
| 10 (M) | 20 | 88/89 | Cavus | Gradual | 20 | Cortical reaction | Grade 3 | ESWT | 8 |
| 11 (F) | 15 | 82/83 | Pronated | Gradual | 16 | Cortical reaction | Grade 3 | ESWT | 7 |
| 12 (F) | 16 | 85/85 | Pronated | Gradual | 10 | Normal | Grade 2 | ESWT | 5 |
| 13 (M) | 17 | 84/85 | Pronated | Gradual | 10 | Normal | Grade 2 | ESWT | 6 |
| 14 (F) | 16 | 85/85 | Normal | Gradual | 9 | Stress fracture | Grade 4 | ESWT | 8 |
| 15 (F) | 16 | 85/86 | Pronated | Gradual | 8 | Normal | Grade 2 | ESWT | 6 |
| 16 (M) | 17 | 85.5/85.5 | Normal | Gradual | 11 | Normal | Grade 2 | ESWT | 5 |
| 17 (M) | 16 | 87/87 | Pronated | Gradual | 8 | Normal | Grade 2 | ESWT | 5 |
| 18 (M) | 14 | 87/87 | Normal | Gradual | 6 | Normal | Grade 2 | ESWT | 6 |
| 19 (F) | 15 | 85/85 | Normal | Gradual | 10 | Normal | Grade 2 | ESWT | 5 |
M male, F female, Rx radiograph, ESWT external shockwave therapy, US ultrasound therapy, EMF electromagnetic fields
a Grade 1: Rx negative but STIR images positive; Grade 2: Rx negative but STIR and T2 positive; Grade 3: cortical reaction and T1 and T2 positive; Grade 4: Rx positive for fracture or cortical reaction and fracture line in T1 and T2
We monitored the progress of the patients weekly by testing the tenderness in the area localised over the metatarsal. When local pain lessened, we allowed return to activity gradually, avoiding jumps and pirouette en pointe. Resolution of tenderness is considered the indicator for return to normal activities and dancing, with completely pain-free movements. Pointe and demi-pointe work was permitted only if the patients were pain-free. An MRI was performed one month after the end of the treatment proposed in this paper in order to assess the healing process of the bone.
Results
At 2.2 years mean follow-up (range 1.3–3.3 years) all dancers healed without any midfoot pain. Shockwave therapy allows dancers to return to practice about 4.6 weeks (range 3–5.3 weeks) after the first application. Dancer no. 2 had a good result, with a return to dancing in 11 weeks. Even if the dancers were completely pain-free, we recommended they return to dancing gradually. All of the dancers returned to full activities after a mean time of 18 days (range 14–23 days) following the end of treatment (6.3 weeks from the onset of the symptoms) (Table 1). No fractures developed nonunion and no refracture occurred.
Discussion
Metatarsal stress fractures represent about 9% of all stress fractures in athletes [14]. In our series, metatarsal stress fractures affected about 12.6% of the ballet dancers who had not yet reached skeletal maturity. Some authors reported that metatarsal stress fractures are common in military recruits with leg-length discrepancy [3]. In particular, a leg-length discrepancy of >0.5 cm was reported in 70% of women with stress fractures, compared with only 37% of women without stress fractures [16]. Other biomechanical characteristics related to a higher risk for stress fractures include external hip rotation greater than 65°, forefoot varus, and poor ankle joint dorsiflexion [7, 9]. A hard training surface is another risk factor for developing these lesions. We think that nutritional factors have a great role in determining stress fractures in ballerinas because of the implications for bone density [17, 18]. Different authors [7, 16, 18, 19] identified a “female triad”: eating disorder, amenorrhea and osteoporosis. Foot architecture in combination with other biomechanical factors play a crucial role in the development of stress fractures in young dancers. In our series (Table 1), leg-length discrepancy was noted in seven dancers. We think that leg-length discrepancy does not play a great role because dancers perform “demi-pointe” and “en-pointe”, so they balance their discrepancy with a different plantar flexion of the ankles. In our opinion, poor plantar flexion of the foot is a condition that can predispose to stress fracture because the dancers perform pointe work with a so-called “over-pointe” foot (Fig. 1). We also observed stress fractures in ballerinas with a pronated foot or with an “over-pointed” foot. In an “over-pointed” foot, the pointe is built at the tarsometatarsal level, so that an excessive strain is placed on the capsules and ligaments of the dorsum of the foot. This is due to the fact that the line of the centre of gravity falls in front of the toes. Because great stress is applied at the tarsometatarsal joints, a stress fracture can occur in this region. Furthermore, the ballerinas in our series had menstrual abnormalities and low body weight three to six months before the onset of symptoms. The males reported that they developed stress fractures when they intensified their activities, with a lot of time spent in pointe, demi-pointe work and jumps, and had a body weight loss in the previous three months.
Fig. 1.
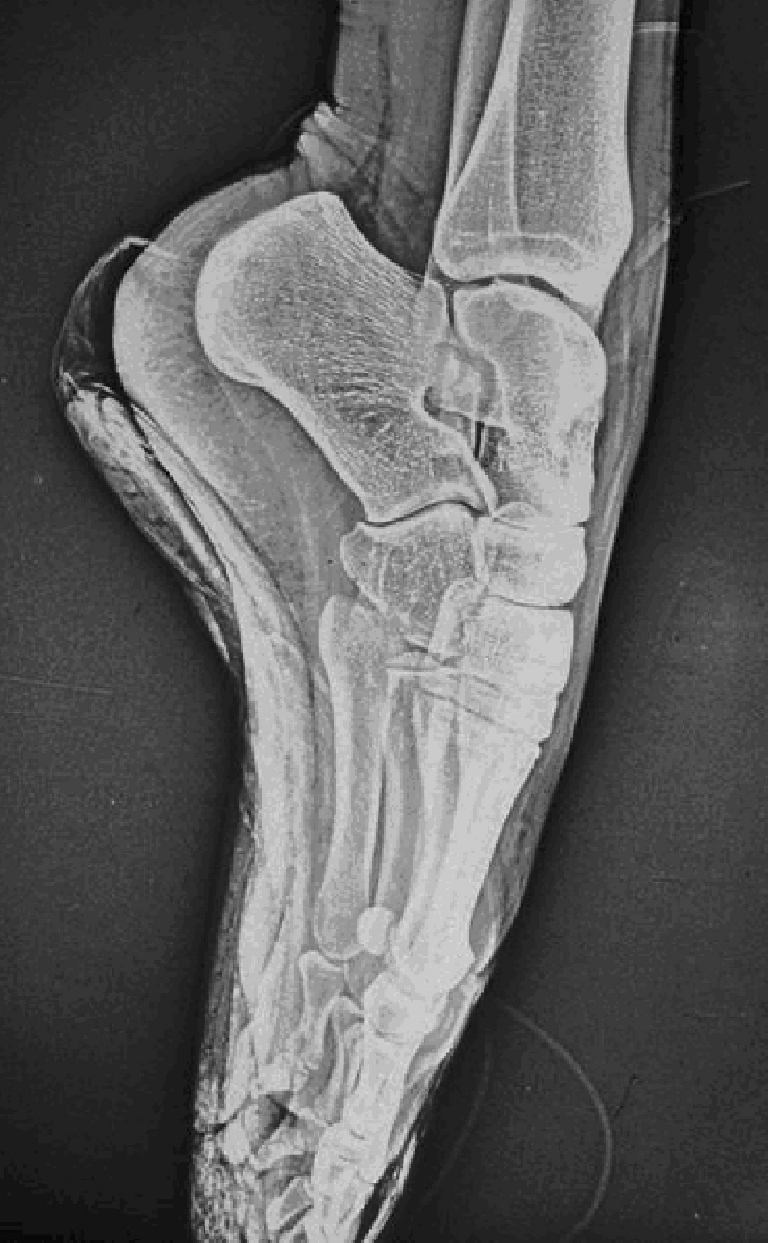
A so-called “over-pointe” foot
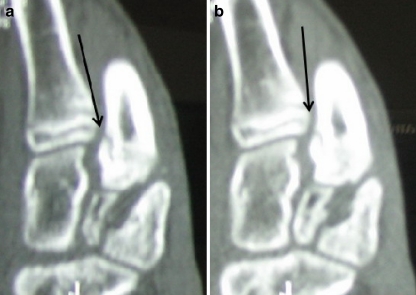
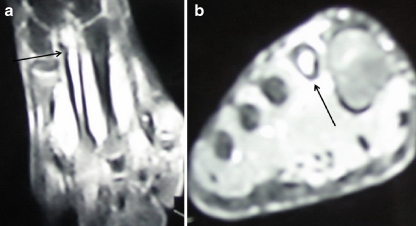
Early diagnosis is essential to avoid a prolonged delay of return to dancing [20]. We noticed that patients complained of an insidious onset of pain over a period of several days or weeks. Initially, the pain occurred only during activity and resolved with rest. Continuation of activity is associated with a progression of pain that becomes constant. This usually occurs seven to 20 days after the first onset of pain [21]. The dancer should be questioned about the nutritional history, training program, type of shoes and dancing surface, recent trauma and menstrual patterns. Changes in type, duration, or frequency of activity are very important risk factors. At physical examination we observed tenderness on the metatarsal and, sometimes, percussion at a distance from the suspected site of a stress fracture caused transmission of pain to the fracture site. Although a stress fracture can usually be suspected on the basis of the clinical examination, an X-ray should always be performed. It should, however, be borne in mind that radiographs can be normal for the first two to three weeks after the onset of symptoms. Sometimes it is possible to see a cortical reaction, a cortical lucency or even a small fracture line at the base of the metatarsal bone. When a fracture is suspected, an MRI or a CT scan should be performed [20, 22–24]. MRI and CT confirm the diagnosis as early as two to eight days after the onset of symptoms. A CT scan can be useful to accurately localise the fracture line (Fig. 2) [23]. MRI is a sensitive and specific investigation and we prefer it because this technique does not require irradiation and can be used frequently during the follow-up of patients (Fig. 3). Moreover, we prefer MRI when we compared it with the bone scan scintigraphy because it is not an invasive investigation and does not require the use of a radioactive tracer. The MRI done one month after the end of treatment showed a decreased intramedullary oedema and the presence of fibrous tissue in the stress fracture site.
Fig. 2.
CT scan showing a stress fracture of the base of the second metatarsal bone. The rim passes through the growing cartilage (patient no. 2)
Fig. 3.
MRI showing a stress fracture of the base of the second metatarsal bone
Few series published in the orthopaedic literature report a quick recovery of these fractures after nonoperative treatment [10, 11, 25]. In a series of 64 stress fractures of the base of the second metatarsal, all healed with conservative care. The patients were all classical ballet dancers [11]. If nonoperative management fails, surgery seems to give good results in most patients as reported by Sarimo et al. [26].
In conclusion, few studies of stress fractures in ballet dancers with immature skeletal systems have been published. The diagnosis of stress fracture is often delayed because of the gradual onset of symptoms and typically negative radiographs taken in the early phase [21]. When it is suspected, an MRI should be performed. The MRI should be considered the gold standard in confirming the diagnosis [20, 22], and CT scans should only be performed to pinpoint the location of the stress fracture. We believe that type of work (pointe), foot architecture (pronated foot, lack of ankle plantar flexion, and over-pointed foot), and menstrual patterns or diet habits are the most important causes of metatarsal stress fractures even in young dancers with elastic and deformable bone. When a stress fracture is diagnosed, rest should be recommended and, if possible, external shock wave therapy should be used. In our experience, medium energy external shockwave therapy always gives good results in young dancers. If properly diagnosed and treated early, stress fractures do not recur, and they only entail a relatively short period of rest from the patients’ activities.
Acknowledgments
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Dubravcic-Simunjak S, Pecina M, Kuipers H, et al. The incidence of injuries in elite junior figure skaters. Am J Sports Med. 2003;31(4):511–517. doi: 10.1177/03635465030310040601. [DOI] [PubMed] [Google Scholar]
- 2.Wilder RP, Sethi S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med. 2004;23:55–81. doi: 10.1016/S0278-5919(03)00085-1. [DOI] [PubMed] [Google Scholar]
- 3.Stuart J, David B, Brukner P. Stress fractures: pathophysiology, epidemiology, and risk factors. Curr Osteoporos Rep. 2006;4:103–109. doi: 10.1007/s11914-996-0029-y. [DOI] [PubMed] [Google Scholar]
- 4.Pecina MM, Bojanic I. Overuse injuries of the musculoskeletal system. 2. Boca Raton: CRC Press; 2003. pp. 316–318. [Google Scholar]
- 5.Milgrom C, Finestone A, Shlamkovitch N (1994) Youth is a risk factor for stress fracture. A study of 783 infantry recruits. J Bone Joint Surg Br 76(1):20–22. [PubMed]
- 6.Brukner P, Bennel K, Matheson G (1999) Stress fractures. Carlton, Victoria, Australia. Blackwell Science Asia, pp 15-40
- 7.Bennel K, Matheson G, Meeuwisse W. Risk factors for stress fractures. Sports Med. 1999;28:91–122. doi: 10.2165/00007256-199928020-00004. [DOI] [PubMed] [Google Scholar]
- 8.Marcus R, Cann C, Madvig P. Menstrual function and bone mass in elite women distance runners: Endocrine and metabolic features. Ann Intern Med. 1985;102:158–163. doi: 10.7326/0003-4819-102-2-158. [DOI] [PubMed] [Google Scholar]
- 9.Bennel K, Malcom S, Thomas S. Risk factors for stress fractures in track and field athletes. A twelve-month prospective study. Am J Sports Med. 1996;24(6):810–818. doi: 10.1177/036354659602400617. [DOI] [PubMed] [Google Scholar]
- 10.Micheli LJ, Sohn RS, Solomon R. Stress fractures of the second metatarsal involving Lisfranc's joint in ballet dancers. J Bone Joint Surg Am. 1985;67:1372–1375. [PubMed] [Google Scholar]
- 11.O’Malley MJ, Hamilton WG, Munyak J. Stress fractures at the base of the second metatarsal in ballet dancers. Foot Ankle Int. 1996;17:89–94. doi: 10.1177/107110079601700206. [DOI] [PubMed] [Google Scholar]
- 12.Kadel NJ, Boenisch M, Teitz CC, Trapman Stability of Lisfranc joints in ballet pointe position. Foot Ankle Int. 2005;26:394–400. doi: 10.1177/107110070502600510. [DOI] [PubMed] [Google Scholar]
- 13.Dubravcic-Simunjak S, Kuipers H, Moran J, Simunjak B, Pecina M. Injuries in synchronized skating. Int J Sports Med. 2006;27(6):493–499. doi: 10.1055/s-2005-865816. [DOI] [PubMed] [Google Scholar]
- 14.Brand JC, Brindle T, Nyland J. Does pulsed low intensity ultrasound allow early return to normal activities when treating stress fractures? A review of one tarsal navicular and eight tibial stress fractures. Iowa Orthop J. 1999;19:26–30. [PMC free article] [PubMed] [Google Scholar]
- 15.Rue JP, Armstrong DW, Frassica FJ. The effect of pulsed ultrasound of tibial stress fractures. Orthopedics. 2004;27(11):1192–1195. doi: 10.3928/0147-7447-20041101-18. [DOI] [PubMed] [Google Scholar]
- 16.Bolin D, Kemper A, Brolinson PG. Current concepts in the evaluation and management of stress fractures. Current Sports Med Rep. 2005;4:295–300. doi: 10.1097/01.csmr.0000306289.98127.23. [DOI] [PubMed] [Google Scholar]
- 17.Tuan K, Wu S, Sennet B. Stress fractures in athletes: risk factors, diagnosis and management. Orthop. 2004;27(6):583–590. doi: 10.3928/0147-7447-20040601-15. [DOI] [PubMed] [Google Scholar]
- 18.Ivkovic A, Franic M, Bojanic I, Pecina M. Overuse injuries in female athletes. Croat Med J. 2007;48(6):767–778. doi: 10.3325/cmj.2007.6.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zeni AI, Street CC, Dempsey RL. Stress injury to the bone among women athletes. Phys Med Rehabil Clin N Am. 2000;11:929–947. [PubMed] [Google Scholar]
- 20.Harrington T, Crichton KJ, Anderson IF. Overuse ballet injury of the base of the second metatarsal. A diagnostic problem. Am J Sports Med. 1993;21(4):591–598. doi: 10.1177/036354659302100418. [DOI] [PubMed] [Google Scholar]
- 21.Morris G, Nix K, Goldman FD. Fracture of the second metatarsal base. An overlooked cause of chronic midfoot pain. J Am Podiatr Med Assoc. 2003;93(1):6–10. doi: 10.7547/87507315-93-1-6. [DOI] [PubMed] [Google Scholar]
- 22.Arendt EA, Griffiths HJ. The use of MR imaging in the assessment and clinical management of stress reactions of bone in high-performance athletes. Clin Sports Med. 1997;16:291–306. doi: 10.1016/S0278-5919(05)70023-5. [DOI] [PubMed] [Google Scholar]
- 23.Fottner A, Baur-Melnik A, Birkenmaier C, et al. Stress fractures presenting as tumours: a retrospective analysis of 22 cases. Int Orthop. 2007 doi: 10.1007/s00264-007-0488-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agarwal A, Gulati D. Dilemma in stress fractures. Int Orthop. 2008 doi: 10.1007/s00264-008-0635-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muscolo L, Migues A, Slullitel G, et al. Stress fracture nonunion at the base of the second metatarsal in a ballet dancer. A case report. Am J Sports Med. 2004;32(6):1535–1537. doi: 10.1177/0363546503262174. [DOI] [PubMed] [Google Scholar]
- 26.Sarimo J, Orava S, Alanen J. Operative treatment of stress fractures of the proximal second metatarsal. Scand J Med Sci Sports. 2007;17:383–386. doi: 10.1111/j.1600-0838.2006.00532.x. [DOI] [PubMed] [Google Scholar]