Abstract
A soft tissue defect is one of the most difficult problems that may accompany bone defects. Plastic surgery is often required. During distraction osteogenesis, not only the bone but also the soft tissues are lengthened, which may help in spontaneous closure of the soft tissue defects. This study examines 11 cases of composite bone and soft tissue defects which were managed by distraction osteogenesis. After debridement of the necrotic tissues, the soft tissue defects ranged from three by four centimetres to five by 14 centimetres and the bone defects ranged from four to 12 centimetres. All the soft tissue defects healed during the process of bone transport without the need for plastic surgery, except in one case. The complications were successfully managed during the course of treatment. Distraction osteogenesis is a good method for simultaneous treatment of composite bone and soft tissue defects.
Résumé
La perte de substance tissulaire est un des problèmes les plus difficile à traiter lorsque cette perte de substance est associée à une perte de substance osseuse. Dans ce cas là, la chirurgie plastique est parfois nécessaire. Durant l’ostéogenèse en distraction, l’allongement ne concerne pas seulement l’os mais également les tissus mous, celle-ci pouront entraîner une cicatrisation spontanée des pertes de substances tissulaires.11 cas de perte de substances osseuses associés à des pertes de substances tissulaires ont été traitées par ostéogenèse en distraction. Après nettoyage et excision des tissus nécrotiques la perte de substance tissulaire était comprise entre 3 × 4 et 5 × 14 cm et la perte de substance osseuse de 4 à 12 cm. Toutes les pertes de substances tissulaires ont cicatrisé durant le processus de transport osseux sans nécessiter une chirurgie reconstructrice plastique en dehors d’un seul cas. Toutes les complications ont été traitées avec succès au cours de l’allongement. L’ostéogenèse en distraction est une excellente méthode pour traiter de façon simultanée les pertes de substances osseuses et les pertes de substances tissulaires.
Introduction
Segmental skeletal defects may result from high energy trauma, debridement of osteomyelitis, or tumour resection. Sometimes the defects are associated with soft tissue injuries that make reconstruction very difficult and limit the functional outcome [4]. Restoration of a healthy soft tissue envelope is a very important step for the proper management of bone defect. This can be achieved by split thickness skin graft, local myocutaneous flap, or distant myocutaneous flaps [1].
Some authors believe that restoration of the soft tissue envelope must be done before or at the time of osseous reconstruction [3, 6, 7].
During distraction osteogenesis, not only the bone but also the soft tissues are lengthened, and this may help in spontaneous closure of the soft tissue defects without the need for major plastic surgery.
In this study we assess the results of distraction osteogenesis in management of composite bone and soft tissue defects. Also we raise the question: “Is it necessary to restore the soft tissue envelop before osseous reconstruction or not?”
Patients and methods
Between March 2002 and December 2006, 11 cases with composite bone and soft tissue defects were managed by distraction osteogenesis in our institution. The ages of the patients ranged from five to 56 years with an average of 27.5 years. Eight were males and three were females. The soft tissue defects were located on the upper third of the leg in five cases, middle third of the leg in three cases, lower half of the leg in one case, and on the ulnar side of the forearm in two cases. The causes of bone and soft tissue defects were trauma in six cases, infection nonunion in three cases, and tumour resection in two cases. After debridement of the infected and necrotic tissues, the soft tissue defects ranged from three by four centimetres to five by 14 centimetres and the bone defects ranged from four to 12 centimetres with an average of seven centimetres.
Acute shortening of the limb was done in two cases to help in rapid closure of both the bone and soft tissue defects, then relengthening was done from a distant corticotomy to restore the limb lengths. In the rest of the cases the exposed bone ends were resected till they became covered by the soft tissue, then bone transport was carried out to close both the bone and soft tissue defects. The care of the pins and wires was done in the usual manner.
Results
The treatment period ranged from eight to 14 months with an average of 10.5 months. The follow-up period ranged from 13 to 38 months with an average of 19 months. The healing index ranged from one to 1.8 months/centimetre with an average of 1.2 months/centimetre. All the soft tissue defects healed during the process of bone transport without the need for plastic surgery, except in one case. This was a five-year-old boy with G III open fracture left tibia and fibula with infection and soft tissue loss over the antromedial aspect of the lower half of the leg. Resection of the necrotic bone ends, acute shortening of the leg, then relengthening from a proximal corticotomy were performed. These led to partial closure of the soft tissue defect, but the lower part of the tibia remained exposed and required muscle flap for its coverage.
The bone defects were eliminated in all cases (Fig. 1). Bone graft was required at the docking site in four cases to treat delayed union. The LLD did not exceed two centimetres in any of our cases. One case was complicated by protrusion of the bone end through the wound. This patient was managed by resection of the protruded part until it became sufficiently covered by the skin, then bone transport was resumed. The other complications included pin tract infection in eight cases (all managed by local care and systemic antibiotic therapy), premature consolidation in one case (managed by osteoclasis under general anaesthesia), and soft tissue invagination at the docking site in three cases (treated by surgical elevation of the skin and soft tissue from the docking sites).
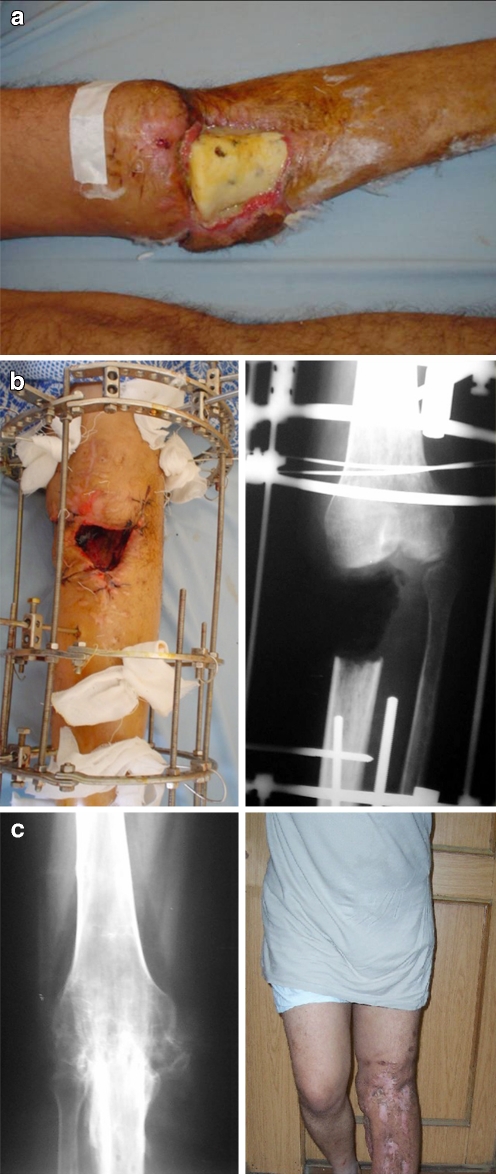
Fig. 1.
a A 24-year-old male patient with GCT proximal tibia. He was managed by excision and bone cement, but complications occurred including infection and sloughing of the skin over the bone cement. b The cement and unhealthy tissues were removed, then bone transport was carried out to bridge the bone and soft tissue defects. c After removal of the frame with complete healing of the bone and soft tissue defects shown clinically (right) and under X-ray (left) after two years
Discussion
Composite bone and soft tissue defects represent a true challenge for orthopaedic surgeons. Besides osseous reconstruction, major plastic surgery in the form of local or distant myocutaneous flaps may be required to reconstruct the soft tissue defects. Unfortunately these flaps remove motor units from their normal position and may produce donor site morbidities [1, 3, 4]. Yazar et al. [7] reported on 62 cases with post-traumatic composite bone and soft tissue defects that were treated by one stage vascularised osteocutaneous flaps. Donor-site problems were noted in nine cases. The fibular donor-site problems were foot drop in one patient, superficial peroneal nerve palsy in one patient, contracture of the flexor hallucis longus muscle in two patients, and skin necrosis after split-thickness skin grafting in two patients. The iliac flap donor-site problems were temporary flank pain in one patient and lateral thigh numbness in the other. One rib flap transfer patient had pleural fibrosis.
During distraction osteogenesis the bone ends carry the surrounding soft tissues, which helps in spontaneous closure of the soft tissue defect without the need for major plastic surgery. Paley and Maar [4] reported on eight cases with soft tissue defects that were treated by soft tissue transport in concert with bone transport.
In our study 11 cases with composite bone and soft tissue defects were treated by distraction osteogenesis. All the soft tissue defects healed during the process of bone transport without the need for plastic surgery, except in one case. In that case the initial defect was large (5 × 14 cm), but after bone resection and acute shortening of the limb, the defect was reduced to three by four centimetres and was easily covered by local muscle flap. Complications were reported in most of our cases but they were successfully managed during the course of treatment and did not affect the final results.
Some surgeons [2, 5] prefer to do acute shortening to produce rapid closure of both the bone and soft tissue defects then relengthening from a distant corticotomy to restore the limb length. We used this technique in only two of our cases in which the bone defects were small (4 and 5 cm). Sometimes, acute shortening of the limb is not feasible and may produce vascular compromise, especially in patients with large defects. In most of our cases the defects were left open to drain while bone transport was carried out. The soft tissues spread gradually during distraction until they completely healed. We found that restoration of the soft tissue envelope is not necessary before the distraction process. The most important thing to observe is that the bone ends must be buried under the soft tissue so that they will carry their soft tissue coverage when bone transport is started, and both the bone and soft tissue defects will heal simultaneously (Fig. 2). If the bone ends are not well covered by the soft tissue they will protrude through the wound during bone transport (Fig. 3). We had one case that was complicated by protrusion of the bone end through the wound due to insufficient soft tissue coverage. He was managed by resection of the protruded part until it became sufficiently covered by the skin, then bone transport was resumed. Both the bone and soft tissue defects healed without further complications in that patient.
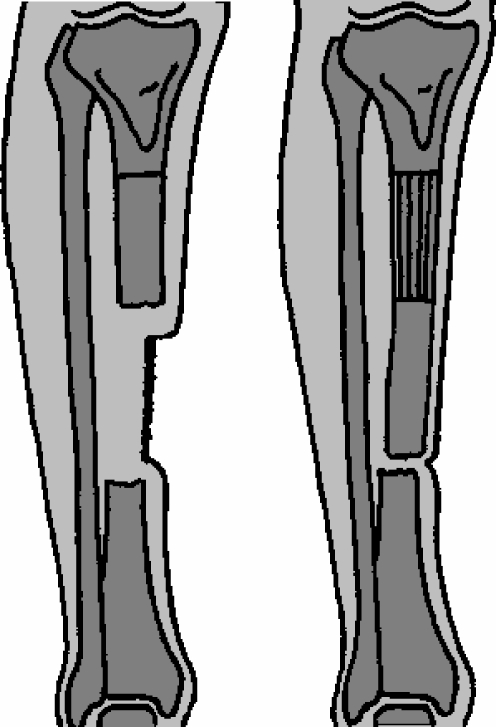
Fig. 2.
Schematic showing that If the bone ends are well covered by the soft tissues they will carry their soft tissue coverage during bone transport
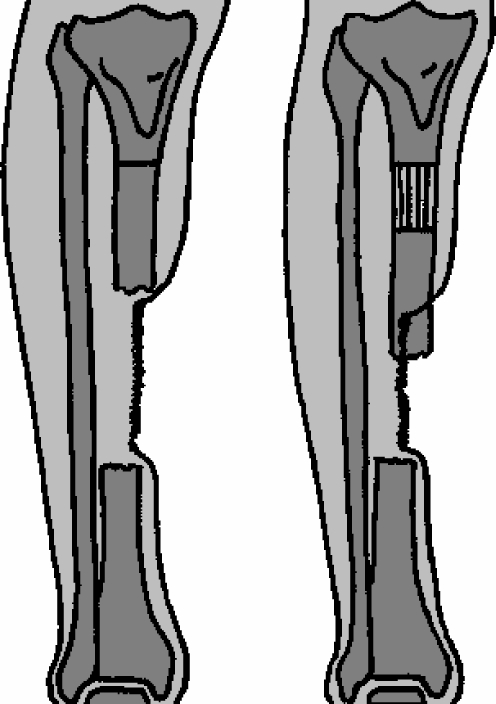
Fig. 3.
Schematic showing that If the bone end is not well covered by the soft tissue it will protrude through the wound during bone transport
Conclusion
Distraction osteogenesis is a good method for simultaneous treatment of composite bone and soft tissue defects. To achieve good results, any exposed bone ends must be resected until they become recessed behind the soft tissue before the beginning of bone transport. It is wise to delay any surgical procedure for soft tissue reconstruction until the end of the distraction process as it may be alleviated or at least minimised.
References
- 1.Edwards CC. Staged reconstruction of open tibial fractures using Hoffman external fixation; clinical decision and dilemmas. Clin Orthop. 1983;178:130–161. [PubMed] [Google Scholar]
- 2.El-Rosasy MA. Acute shortening and re-lengthening in the management of bone and soft-tissue loss in complicated fractures of the tibia. J Bone Joint Surg. 2007;89(Br):80–88. doi: 10.1302/0301-620X.89B1.17595. [DOI] [PubMed] [Google Scholar]
- 3.Gordon L, Chiu EJ. Treatment of infected nonunion and segmental defects of the tibia with staged microvascular muscle transplantation and bone grafting. J Bone Joint Surg. 1988;70A:377–385. [PubMed] [Google Scholar]
- 4.Paley D, Maar DC. Ilizarov bone transport for tibial defects. J Orthop Trauma. 2000;14:76–85. doi: 10.1097/00005131-200002000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Sen C, Kocaoglu M, Eralp L, Gulsen M, Cinar M. Bifocal compression-distraction in the acute treatment of grade III open tibia fractures with bone and soft-tissue loss: a report of 24 cases. J Orthop Trauma. 2004;18(3):150–157. doi: 10.1097/00005131-200403000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Schottle PB, Werner CM, Dumont CE. Two-stage reconstruction with free vascularized soft tissue transfer and conventional bone graft for infected nonunions of the tibia: 6 patients followed for 1.5 to 5 years. Acta Orthop. 2005;76(6):878–883. doi: 10.1080/17453670510045534. [DOI] [PubMed] [Google Scholar]
- 7.Yazar S, Lin CH, Wei FC. One-stage reconstruction of composite bone and soft-tissue defects in traumatic lower extremities. Plast Reconstr Surg. 2004;114(6):1457–1466. doi: 10.1097/01.PRS.0000138811.88807.65. [DOI] [PubMed] [Google Scholar]