Abstract
The literature has described different indications for pelvic fixation in neuromuscular scoliosis. We retrospectively evaluated changes in pelvic obliquity for a minimum of two years among three groups: group I (initial pelvic obliquity >15°; with pelvic fixation), group II (initial pelvic obliquity >15°; without pelvic fixation), and group III (initial pelvic obliquity <15°; without pelvic fixation). We used iliac screws for pelvic fixation in group I. There was significant postoperative improvement (p < 0.0001) in Cobb’s angle and pelvic obliquity. There was no significant loss of correction in Cobb’s angle, thoracic kyphosis, and lumbar lordosis among all three groups; however, group II showed significant correction loss in pelvic obliquity compared to groups I and III at final follow-up (p < 0.0001). Our results indicate that patients who have pelvic obliquity >15° require pelvic fixation to maintain the correction and balance over time while obliquity <15° does not require pelvic fixation.
Résumé
La littérature décrit les différentes indications de la fixation pelvienne dans les scolioses neuro-musculaires. Nous avons revu, de façon rétrospective, les modifications observées sur l’obliquité pelvienne après un recul de deux ans minimum sur trois groupes de patients. Le groupe 1 présentait une obliquité pelvienne initiale supérieure à 15° traitée par fixation pelvienne. Le groupe 2 une obliquité pelvienne supérieure également à 15° mais sans fixation pelvienne post-opératoire, le groupe 3 avec une obliquité pelvienne inférieure à 15°, traitée sans fixation pelvienne. Pour la fixation pelvienne ont été utilisées des vis illiaques dans le groupe 1. Nous avons observé des modifications significatives des corrections post-opératoires (p < 0,0001) au niveau de l’angle de Cobb et de l’obliquité pelvienne. Il n’y a pas de pertes significatives au niveau de l’angle de Cobb, de la cyphose thoracique, de la lordose lombaire, dans les trois groupes, cependant, au dernier suivi, le groupe 2 montre de façon significative une perte de correction au niveau du bassin oblique, plus importante que dans les groupes 1 et 3 (p < 0,0001). Ces résultats nous permettent de penser qu’une obliquité pelvienne supérieure à 15° nécessite une fixation pelvienne de façon à maintenir la correction. Les obliquités inférieures à 15° ne nécessitent pas de correction.
Introduction
The goals of surgery for neuromuscular scoliosis include safe correction of deformity, solid fusion of fixed levels to make the spine balanced, and provide sitting balance. Fixed pelvic obliquity is a frequent feature associated with neuromuscular scoliosis [18]. Several authors recommended pelvic fixation along with scoliosis correction for neuromuscular scoliosis. Methods of pelvic fixation have included the Galveston (L-rod) technique, Dunn-McCarthy (S-rod) technique, transiliac screws, intrasacral screws, iliosacral fixation, and iliac screws [1, 5, 8, 9, 12]. However, all of these techniques of pelvic fixation carry implant related complications [4]. Therefore, other authors have called into question the need to extend the instrumentation caudally in the lumbar spine. They suggested that there is no need of pelvic fixation in neuromuscular scoliosis and reported good correction in Cobb’s angle and pelvic obliquity [7, 15, 19]. Although good results have been reported for each technique, uniform consensus regarding pelvic obliquity and pelvic fixation is still lacking. There is a definite indication for pelvic fixation in neuromuscular scoliosis from the available literature, in which optimal use of the instrumentation avoids undue complications associated with pelvic fixation.
Here, we retrospectively followed neuromuscular scoliosis patients, for a minimum period of two years, based on the severity of initial pelvic inclination, we evaluated the difference in pelvic obliquity on regular follow-up in patients who had pelvic fixation versus those who did not have pelvic fixation. Similarly, we also reviewed Cobb’s angle and tried to find out whether it has any relation with pelvic obliquity. In our study we did not use pelvic fixation in those neuromuscular scoliosis patients who had initial pelvic obliquity less than 15°. For patients who had initial pelvic obliquity more than 15°, we fixed the pelvis with iliac screws in some patients whilst the remainder did not undergo pelvic fixation during the scoliosis operation. We postulated that patients who had pelvic obliquity less than 15° would have a stable pelvis over a long period; however, those patients who had pelvic obliquity more than 15° and did not receive pelvic fixation eventually would show deterioration in initial pelvic correction, assuming that in neuromuscular scoliosis the need for pelvic fixation is indicated only in those patients who have pelvic obliquity more than 15° regardless of severity of Cobb’s angle.
Materials and methods
Patient population
Between 2002 and 2006, 55 neuromuscular scoliosis patients underwent operation for correction and fusion for scoliosis with pedicle screw instrumentation. None of our patients received an anterior procedure. There were 28 patients with cerebral palsy (CP), 17 with Duchenne muscular dystrophy (DMD), and ten with spinal muscular atrophy (SMA). Mean age at the time of operation was 19.3 ± 8.2 years (range, 8–43). There were 34 male and 21 female patients.
Operation and evaluation
All patients underwent a radiograph preoperatively, immediately postoperatively, and at final follow-up. In addition, preoperatively, all patients underwent a bending radiograph to demonstrate flexibility of the curve. A spine fellow (HNM) calculated all measurements. Cobb’s angle was measured by Cobb’s method and pelvic obliquity was measured by Allen and Ferguson’s method from a horizontal line. Thoracic kyphosis was measured between upper and lower endplates of T4 and T12, respectively; and lumbar lordosis was calculated from the upper endplate of L1 to the upper endplate of S1. All patients received fixation from T2/T3/T4 proximally to L4/L5 distally, with or without pelvic fixation. Iliac screws were used for pelvic fixation throughout the study. The decision for pelvic fixation was made by a senior author (SWS) for the few patients who had pelvic obliquity more than 15°. Pelvic fixation was not done in patients with pelvic obliquity less than 15°. The fusion was achieved using local bone grafts from spinous processes which were mixed with cadaveric allograft. The results were analysed on radiographs taken preoperatively, immediately postoperatively, and at final follow-up for Cobb’s angle, pelvic obliquity, thoracic kyphosis, and lumbar lordosis. We paid particular attention to the progression of pelvic obliquity at follow-up with respect to the pelvic fixation. We divided the patients into three groups: group I comprised 16 patients who underwent pelvic fixation and the initial pelvic obliquity was more than 15°, group II comprised 16 patients who did not receive pelvic fixation and the initial pelvic obliquity was more than 15°, and group III comprised 23 patients who received no pelvic fixation and whose initial pelvic obliquity was more than 15°.
Statistical analysis
We analysed the postoperative correction in Cobb’s angle and pelvic obliquity using paired t-test and compared the correction rate. We used the paired t-test to observe the maintenance of the correction in Cobb’s angle, pelvic obliquity, thoracic kyphosis, and lumbar lordosis in each group. We also compared the preoperative flexibility in each group with the ANOVA test to discover any difference. To determine any difference in severity of initial curve, the preoperative Cobb’s angle among the three groups was analysed using the ANOVA test.
Results
Mean follow-up was 30.1 ± 7.0 months (range, 24–60 months). Average preoperative, immediate postoperative, and at last follow-up Cobb’s angles were 82.3°, 35.1°, and 36.8°, respectively, while pelvic obliquity was 15.7°, 6.4°, and 9.1°, thoracic kyphosis was 27.9°, 23.4°, and 23.5°, and lumbar lordosis was 1.5°, 27.9°, and 26.6°, respectively. Average preoperative flexibility was 19.6 ± 9.0° or 26.4%. Mean ages for groups I, II, and III were 16.6 ± 7.0, 22.5 ± 10.4, and 19.1 ± 7.3 years, respectively. Average preoperative flexibility of curve was 29.9% (20.8°), 23.1% (21.5°), and 26.3% (17.4°) for groups I, II, and III, respectively, which did not reveal any significant differences (p = 0.41, ANOVA test). Similarly, preoperative Cobb’s angle among all three groups did not exhibit any significant difference (p = 0.06, ANOVA test).
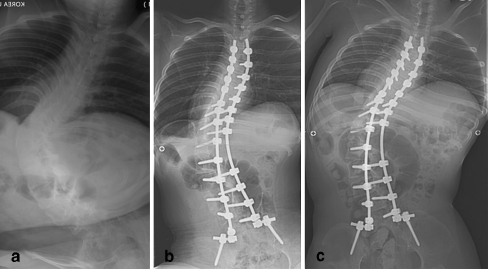
Group I (pelvic obliquity >15° and with pelvic fixation, Fig. 1) had 16 patients who had average preoperative pelvic obliquity of 21.3°. Immediate postoperative and final follow-up pelvic obliquity were 7.4° (65.1% postoperative correction) and 7.1° (66.6% final correction), respectively, which showed 1.5% (0.3°) improvement. On the other hand, preoperative, postoperative, and final follow-up Cobb’s angles were 77.6°, 35.9° (53.7% postoperative correction), and 36.7° (52.6% final correction), respectively, which showed only 1.1% (0.9°) loss of correction. Average preoperative, postoperative, and final follow-up thoracic kyphosis measurements were 17.1°, 20.7°, and 19.7°, and lumbar lordosis was −20°, 24.1°, and 22.2°, respectively (Table 1).
Fig. 1.
Preoperative (a), immediate postoperative (b), and final follow-up (c) anteroposterior and lateral radiograms of a 17-year-old Duchenne muscular dystrophy (DMD) boy from group I. Correction in Cobb’s angle and pelvic obliquity are well maintained with pelvic fixation
Table 1.
Demographics and preoperative, postoperative, and final follow-up Cobb’s angles and pelvic obliquity of group I patients (who had pelvic obliquity >15° and underwent pelvic fixation)
| Patient number | Age (y) | Gender | Diagnosis | Follow-up (mo) | Flexibility (°) | Cobb’s angle | Pelvic obliquity | Thoracic kyphosis | Lumbar lordosis | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op | Final | Pre-op | Post-op | Final | Pre-op | Post-op | Final | Pre-op | Post-op | Final | ||||||
| 1 | 9 | F | SMA | 41 | 25 | 44 | 4 | 5 | 23 | 5 | 3 | 3 | 10 | 10 | −14 | 27 | 24 |
| 2 | 14 | F | SMA | 35 | 12 | 95 | 66 | 63 | 17 | 1 | 2 | 3 | 16 | 14 | 10 | 31 | 26 |
| 3 | 21 | M | SMA | 35 | 20 | 66 | 44 | 43 | 25 | 15 | 14 | 41 | 29 | 29 | −33 | 19 | 10 |
| 4 | 10 | M | SMA | 34 | 18 | 52 | 17 | 20 | 16 | 2 | 6 | 15 | 23 | 16 | −13 | 42 | 38 |
| 5 | 13 | F | SMA | 39 | 42 | 112 | 24 | 25 | 20 | 9 | 7 | 35 | 16 | 17 | −39 | 36 | 32 |
| 6 | 13 | F | SMA | 25 | 10 | 110 | 42 | 45 | 22 | 18 | 14 | 33 | 25 | 24 | −26 | 35 | 33 |
| 7 | 13 | M | DMD | 34 | 15 | 40 | 8 | 10 | 16 | 1 | 1 | 15 | 13 | 14 | −50 | 17 | 16 |
| 8 | 17 | M | DMD | 33 | 13 | 95 | 58 | 54 | 30 | 10 | 9 | −35 | 20 | 14 | −98 | 6 | 7 |
| 9 | 14 | M | DMD | 31 | 20 | 69 | 28 | 28 | 20 | 10 | 7 | 4 | 16 | 14 | −28 | 23 | 26 |
| 10 | 14 | M | DMD | 25 | 30 | 60 | 13 | 15 | 17 | 5 | 5 | 2 | 10 | 10 | −20 | 17 | 14 |
| 11 | 14 | M | DMD | 25 | 36 | 100 | 38 | 41 | 26 | 11 | 12 | 8 | 7 | 8 | −68 | 16 | 15 |
| 12 | 17 | F | CP | 32 | 21 | 64 | 27 | 30 | 19 | 4 | 3 | 41 | 59 | 58 | 25 | 27 | 26 |
| 13 | 25 | M | CP | 31 | 20 | 108 | 76 | 77 | 39 | 16 | 16 | 23 | 16 | 14 | −48 | 28 | 18 |
| 14 | 26 | F | CP | 28 | 15 | 84 | 38 | 40 | 18 | 6 | 9 | 4 | 27 | 17 | 32 | 24 | 13 |
| 15 | 35 | M | CP | 38 | 18 | 102 | 76 | 77 | 17 | 4 | 5 | 67 | 30 | 31 | 31 | 27 | 28 |
| 16 | 10 | M | CP | 60 | 18 | 40 | 15 | 15 | 16 | 2 | 1 | 15 | 15 | 25 | 19 | 11 | 30 |
SMA spinal muscular atrophy, DMD Duchenne muscular dystrophy, CP cerebral palsy
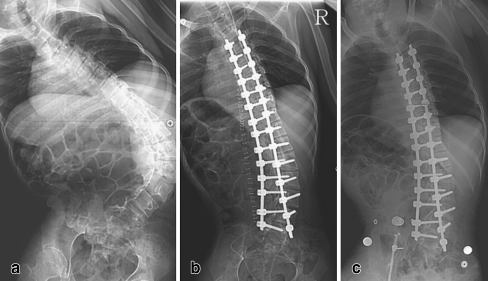
Group II (pelvic obliquity >15° and without pelvic fixation, Fig. 2) had 16 patients who had preoperative pelvic obliquity of 21.6°. Immediate postoperative and final follow-up pelvic obliquity were 10° (53.9% postoperative correction) and 19.4° (10.9% final correction), respectively, which exhibit 43.1% (9.3°) loss of correction. While preoperative, immediate postoperative, and final follow-up Cobb’s angles were 96.5°, 48.1° (50.2% postoperative correction), and 49.8° (48.3% final correction), respectively, which show only 1.9% (2.1°) loss of correction. Average preoperative, postoperative, and final follow-up thoracic kyphosis were 29.7°, 22.6°, and 22.8°, respectively, and lumbar lordosis was 0.8°, 24.5°, and 23.1°, respectively (Table 2).
Fig. 2.
Preoperative (a), immediate postoperative (b), and final follow-up (c) anteroposterior and lateral radiograms of a 21-year-old cerebral palsy (CP) male from group II. Correction in Cobb’s angle is maintained, however, correction in pelvic obliquity deteriorated without pelvic fixation
Table 2.
Demographics and preoperative, postoperative, and final follow-up Cobb’s angles and pelvic obliquity of group II patients (who had pelvic obliquity >15° and did not receive pelvic fixation)
| Patient number | Age (y) | Gender | Diagnosis | Follow-up (mo) | Flexibility (°) | Cobb’s angle | Pelvic obliquity | Thoracic kyphosis | Lumbar lordosis | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op | Final | Pre-op | Post-op | Final | Pre-op | Post-op | Final | Pre-op | Post-op | Final | ||||||
| 17 | 29 | F | SMA | 28 | 9 | 92 | 55 | 59 | 27 | 18 | 28 | 27 | 26 | 27 | 54 | 40 | 37 |
| 18 | 14 | F | SMA | 25 | 36 | 130 | 65 | 68 | 20 | 9 | 19 | 13 | 8 | 11 | -54 | 37 | 34 |
| 19 | 8 | M | DMD | 31 | 12 | 50 | 40 | 43 | 16 | 6 | 12 | 38 | 25 | 25 | -28 | 20 | 22 |
| 20 | 13 | M | DMD | 32 | 20 | 84 | 45 | 46 | 29 | 20 | 20 | 14 | 4 | 4 | -57 | 3 | 8 |
| 21 | 15 | M | DMD | 6 | 16 | 102 | 28 | 27 | 24 | 15 | 15 | 22 | 10 | 8 | -51 | 13 | 14 |
| 22 | 17 | M | DMD | 26 | 28 | 81 | 59 | 60 | 22 | 12 | 18 | 28 | 15 | 12 | -23 | 19 | 16 |
| 23 | 13 | M | DMD | 27 | 33 | 66 | 28 | 34 | 26 | 8 | 24 | 6 | 12 | 11 | 10 | 19 | 16 |
| 24 | 16 | M | DMD | 27 | 20 | 83 | 26 | 30 | 16 | 8 | 19 | 29 | 11 | 13 | -29 | 5 | 7 |
| 25 | 23 | F | CP | 28 | 20 | 75 | 33 | 33 | 17 | 12 | 25 | 23 | 22 | 20 | 27 | 20 | 13 |
| 26 | 32 | M | CP | 24 | 39 | 120 | 78 | 75 | 35 | 11 | 42 | 5 | 15 | 13 | 25 | 30 | 20 |
| 27 | 43 | F | CP | 29 | 21 | 93 | 44 | 45 | 19 | 16 | 17 | 70 | 36 | 36 | 3 | 3 | 3 |
| 28 | 21 | M | CP | 27 | 26 | 121 | 47 | 50 | 26 | 3 | 20 | 34 | 22 | 22 | 32 | 38 | 30 |
| 29 | 43 | F | CP | 31 | 23 | 120 | 78 | 81 | 17 | 3 | 11 | 49 | 53 | 54 | 60 | 40 | 40 |
| 30 | 18 | F | CP | 26 | 9 | 81 | 28 | 30 | 16 | 3 | 10 | 50 | 40 | 40 | 45 | 36 | 35 |
| 31 | 30 | M | CP | 29 | 17 | 140 | 67 | 66 | 18 | 8 | 14 | 61 | 31 | 38 | 63 | 45 | 51 |
| 32 | 25 | M | CP | 29 | 15 | 106 | 48 | 51 | 19 | 8 | 16 | 7 | 31 | 32 | -65 | 25 | 25 |
SMA spinal muscular atrophy, DMD Duchenne muscular dystrophy, CP cerebral palsy
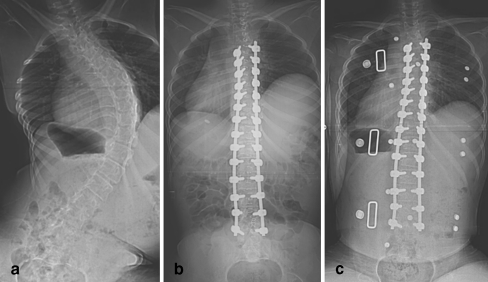
Group III (pelvic obliquity <15° and without pelvic fixation, Fig. 3) had 23 patients who had preoperative obliquity of 7.7°. Immediate postoperative and final follow-up pelvic obliquity were 3.1° (59.0% postoperative correction) and 3.4° (55.6% final correction), respectively, which showed only 3.4% (0.3°) loss of initial correction. Similarly, preoperative, immediate postoperative and final follow-up Cobb’s angle was 75.7°, 25.7° (66.1% postoperative correction), and 27.8° (63.2% final correction), respectively, which again exhibited only 2.9% (2.2°) loss of initial correction. Average preoperative, postoperative, and final follow-up thoracic kyphosis measurements were 34.1°, 25.8°, and 26.5°, and lumbar lordosis were 17°, 32.9°, and 32°, respectively (Table 3).
Fig. 3.
Preoperative (a), immediate postoperative (b), and final follow-up (c) anteroposterior and lateral radiogram of a 14-year-old Duchenne muscular dystrophy (DMD) boy from group III. Correction in Cobb’s angle and pelvic obliquity are well maintained without pelvic fixation
Table 3.
Demographics and preoperative, postoperative, and final follow-up Cobb’s angle and pelvic obliquity of group III patients (who had pelvic obliquity <15° and did not receive pelvic fixation)
| Patient number | Age (y) | Gender | Diagnosis | Follow-up (mo) | Flexibility(°) | Cobb’s angle | Pelvic obliquity | Thoracic kyphosis | Lumbar lordosis | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op | Final | Pre-op | Post-op | Final | Pre-op | Post-op | Final | Pre-op | Post-op | Final | ||||||
| 33 | 10 | F | SMA | 25 | 19 | 71 | 5 | 7 | 4 | 1 | 0 | 66 | 32 | 28 | 31 | 30 | 26 |
| 34 | 18 | F | SMA | 25 | 16 | 108 | 30 | 36 | 10 | 6 | 11 | 46 | 28 | 27 | −44 | 36 | 32 |
| 35 | 12 | F | DMD | 60 | 16 | 68 | 35 | 37 | 9 | 6 | 6 | 4 | 11 | 8 | −78 | 10 | 8 |
| 36 | 11 | M | DMD | 34 | 15 | 93 | 22 | 25 | 8 | 2 | 4 | 31 | 18 | 19 | −32 | 19 | 21 |
| 37 | 12 | M | DMD | 27 | 28 | 70 | 14 | 20 | 14 | 2 | 4 | 46 | 22 | 27 | −40 | 38 | 34 |
| 38 | 11 | M | DMD | 27 | 30 | 46 | 13 | 15 | 8 | 6 | 5 | 52 | 35 | 32 | 39 | 42 | 39 |
| 39 | 18 | M | DMD | 26 | 11 | 40 | 17 | 19 | 12 | 12 | 9 | 12 | 10 | 11 | −58 | 17 | 16 |
| 40 | 14 | M | DMD | 28 | 10 | 91 | 15 | 18 | 11 | 4 | 9 | −27 | 1 | 7 | 28 | 42 | 41 |
| 41 | 15 | F | CP | 26 | 7 | 86 | 31 | 33 | 6 | 2 | 2 | 34 | 41 | 41 | 29 | 42 | 41 |
| 42 | 14 | M | CP | 29 | 5 | 90 | 41 | 40 | 14 | 3 | 5 | 45 | 34 | 42 | 56 | 56 | 57 |
| 43 | 37 | F | CP | 27 | 12 | 25 | 5 | 5 | 3 | 3 | 3 | 59 | 36 | 36 | 54 | 37 | 37 |
| 44 | 22 | M | CP | 28 | 23 | 40 | 17 | 18 | 6 | 2 | 3 | 50 | 40 | 40 | 35 | 32 | 35 |
| 45 | 18 | M | CP | 28 | 9 | 70 | 20 | 22 | 9 | 2 | 0 | 15 | 15 | 25 | 19 | 11 | 30 |
| 46 | 23 | M | CP | 25 | 32 | 65 | 8 | 9 | 11 | 4 | 1 | 66 | 51 | 52 | 41 | 43 | 43 |
| 47 | 20 | M | CP | 30 | 13 | 52 | 6 | 9 | 6 | 1 | 2 | 37 | 39 | 40 | 26 | 23 | 17 |
| 48 | 34 | M | CP | 26 | 26 | 66 | 18 | 22 | 2 | 1 | 0 | 22 | 14 | 17 | 46 | 31 | 29 |
| 49 | 18 | F | CP | 27 | 4 | 41 | 10 | 13 | 2 | 1 | 2 | 30 | 17 | 15 | 16 | 25 | 15 |
| 50 | 30 | F | CP | 27 | 30 | 130 | 55 | 58 | 5 | 5 | 6 | 36 | 24 | 15 | 49 | 49 | 42 |
| 51 | 21 | M | CP | 24 | 36 | 108 | 39 | 40 | 15 | 3 | 0 | 24 | 34 | 34 | 73 | 65 | 66 |
| 52 | 28 | F | CP | 26 | 18 | 150 | 74 | 75 | 10 | 3 | 5 | 67 | 30 | 31 | 31 | 27 | 28 |
| 53 | 17 | M | CP | 26 | 20 | 90 | 39 | 40 | 3 | 2 | 2 | 27 | 29 | 29 | 23 | 25 | 25 |
| 54 | 16 | F | CP | 32 | 13 | 51 | 21 | 24 | 7 | 1 | 0 | 37 | 14 | 15 | 6 | 4 | 4 |
| 55 | 20 | M | CP | 30 | 8 | 90 | 55 | 55 | 3 | 1 | 0 | 7 | 19 | 20 | 42 | 54 | 50 |
SMA spinal muscular atrophy, DMD Duchenne muscular dystrophy, CP cerebral palsy
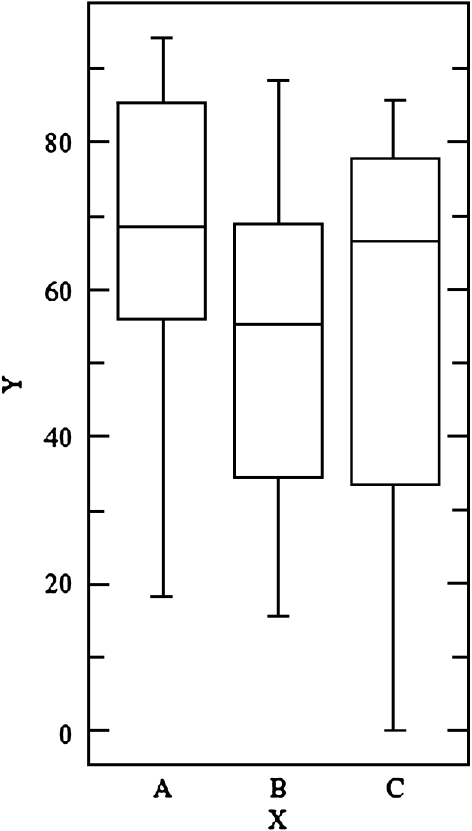
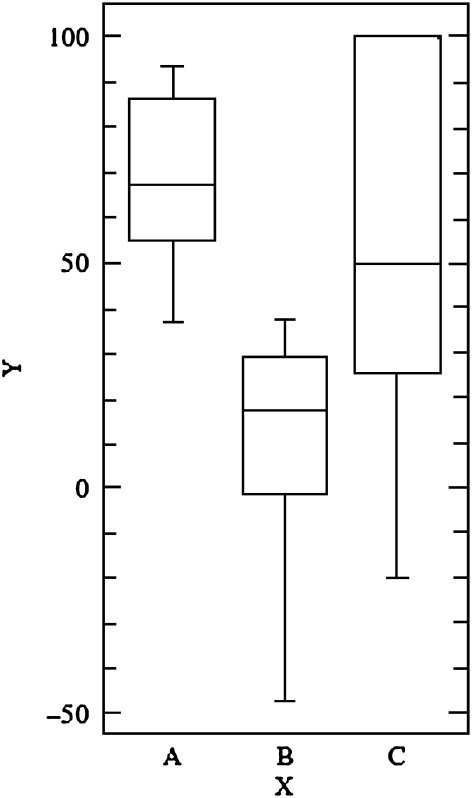
Comparing the Cobb’s angle correction among all three groups reveals that there is a significant correction postoperatively and at final follow-up. At final follow-up Cobb’s angle was maintained in all three groups (p = 0.26, ANOVA). However, when pelvic obliquity was compared, all three groups displayed significant correction postoperatively (p = 0.21, ANOVA, Fig. 4); but group II exhibited significant loss of correction at final follow-up when compared with groups I and III (p < 0.0001, ANOVA, Fig. 5). We also compared the thoracic kyphosis and lumbar lordosis in each group postoperatively and at final follow-up using a paired t-test. In each group neither thoracic kyphosis nor lumbar lordosis showed any significant difference statistically (p = 0.35, 0.61, and 0.38 for groups I, II, and III, respectively, for thoracic kyphosis and p = 0.29, 0.23, and 0.40 for lumbar lordosis).
Fig. 4.
Postoperative correction rate in pelvic obliquity is similar in all three groups. The x-axis shows three groups: A (group I), B (group II), and C (group III). The y-axis shows percentage of correction
Fig. 5.
At final follow-up pelvic obliquity deteriorated in group II while groups I and III maintained the correction. The x-axis shows three groups: A (group I), B (group II), and C (group III). The y-axis shows percentage of correction
Regarding the complications, we did not see any case of implant loosening or breakage of screws. However, we had three patients with sacral sores due to impingement of the iliac screws, especially in group I. We noticed deterioration in sitting balance over a long period of time in patients from group II, while the sitting balance of patients from groups I and III did not deteriorate.
Discussion
This study confirms that neuromuscular scoliosis patients who have pelvic obliquity of more than 15° require pelvic fixation while those who have pelvic obliquity less than 15° do not require pelvic fixation. Though initial correction with the pedicle screw fixation without pelvic fixation is similar, loss of correction in pelvic obliquity can be expected in those who have pelvic obliquity more than 15°.
Neuromuscular scoliosis often requires a long fusion from the upper thoracic spine to the distal lumbar spine or pelvis. Usually, the upper level of fixation is at T2-T4 in literature [3, 5, 11, 14]; however, there are different opinions about the distal extent of fixation and fusion. We have extended spinal fusion to T2-T4 proximally in most of our cases. Few authors recommend pelvic fixation as a routine in all cases of neuromuscular scoliosis [1, 16]. Pelvic fixation, however, is a challenge to most surgeons because it carries a high rate of implant-related complications. Allen and Ferguson [1] popularised their Galveston method for pelvic fixation which has a high rate of complications including ‘wind shield wiper sign’, pressure sores, etc. On the other hand, the literature shows evidence that finishing the fixation at the lumbar spine corrects and maintains pelvic obliquity as well as Cobb’s angle very well [13, 17]. But they give no clear idea about the indication of pelvic fixation. In this paper, we studied three groups of neuromuscular scoliosis: group I who had pelvic obliquity more than 15° and received pelvic fixation, group II who had pelvic obliquity more than 15° and did not receive pelvic fixation, and group III who had pelvic obliquity less than 15° and did not receive pelvic fixation. We followed these groups over a minimum period of two years, observing the pelvic obliquity in all three groups, and tried to determine the correct indications for pelvic fixation. Thus, in this paper we tried to evaluate the effect of distal extent of fixation in neuromuscular scoliosis. All authors, whether they apply pelvic fixation or not, have patients with pelvic obliquity ranging from 3° to 40°.
There are various techniques for pelvic fixation such as the Galveston system, S-rod fixation, sacral screws, iliosacral fixation, the STIF technique, iliac fixation, etc., which show good results [1, 5, 8, 9, 12]. As pelvic fixation has a high complication rate, there are various papers reporting the different methods. Peelle et al. [11] suggested that the method of iliac screws has similar results compared to the Galveston system and fewer complications; therefore, we used iliac screw fixation in our study. Phillips [12] reported that use of two screws in each iliac wing provides stronger purchase than one screw in each iliac wing; however, we used one screw in each iliac wing and achieved good purchase. Miladi et al. [9] reported a long-term study in neuromuscular scoliosis patients with iliosacral fixation. They noted that pelvic fixation becomes easier with a connector between the rod and iliac screw. We have used a similar connector for pelvic fixation which was not difficult to assemble.
In the literature there are different indications for pelvic fixation. Lonstein and Akbarnia [6] published guidelines for arthrodesis ending in the lumbar spine but included patients without neuropathic or myopathic scoliosis. Mubarak et al. [10] suggested pelvic fixation when Cobb’s angle is more than 40° and pelvic obliquity >10°, especially in DMD patients. Whitaker et al. [19] studied selected neuromuscular scoliosis with a criteria of more than 15° pelvic obliquity for pelvic fixation and compared their results with that of fixation ending at the L5 level. They reported that selected patients with pelvic obliquity less than 15° can be managed without pelvic fixation. However, their average preoperative pelvic obliquity and final pelvic obliquity were the same and in a few cases they also performed the anterior procedure. In our study, none of our patients underwent an anterior procedure. Sengupta et al. [14] reported their results of 50 Duchene muscular dystrophy patients. They performed pelvic fixation in older patients who had pelvic obliquity around 20° and avoided pelvic fixation in younger patients who had pelvic obliquity around 10°. In the pelvic fixation group, they reported pelvic obliquity improved from 19.8° preoperatively to 11.6° at final follow-up, and in the lumbar fixation group it improved from 9° preoperatively to 2.9° at final follow-up. Islam et al. [4] mentioned that fixation to the pelvis with modern instrumentation in scoliosis surgery maintains a good balance and correction in curves; however, the complication rates remain high. McCall and Hayes [7] reported similar correction in pelvic obliquity in 55 CP patients between the lumbar fixation group and the pelvic fixation group. Their indication for pelvic fixation was 15° pelvic obliquity. In view of all the reports, we avoided pelvic fixation in patients who had less than 15° pelvic obliquity. In addition, we performed pelvic fixation in selected patients who had pelvic obliquity more than 15° and compared the results at 25 months follow-up in our paper.
Hahn [3] obtained 65% and 77% correction in pelvic obliquity and Cobb’s angle, respectively, with pedicle screw fixation and iliac screws in DMD patients. However, only six patients out of 20 had pelvic obliquity more than 15°. Brook et al. [2] achieved 63% correction in pelvic obliquity in 17 DMD patients with Galveston fixation. We achieved 65% correction in group I (pelvic fixation and pelvic obliquity >15°) and 59% correction in group III (without pelvic fixation and pelvic obliquity <15°), which is comparable to previous reports. However, the initial correction was not maintained in group II. Initial correction in group II was 53.8%; however, it deteriorated at final follow-up to only 10.7%. In spite of the change in pelvic obliquity, correction in Cobb’s angle remained unchanged in all three groups. In addition, we observed deterioration in sitting balance in patients from group II while patients from groups I and III maintained sitting balance over a long period. Though Cobb’s angle remains the same in all three groups at final follow-up, deterioration in pelvic obliquity could be the reason for the sitting imbalance in group II.
Looking at Cobb’s angle amongst the three groups, we observed that the preoperative Cobb’s angle was higher in group II than groups I and III, though it was statistically not significant (p = 0.06). We believe that it may have some effect on final outcome of pelvic obliquity, which is the defect of this paper. In addition we could not compare the results between the spastic and paralytic neuromuscular scoliosis groups due to insufficient patient numbers. However, we believe our results emphasise the need for pelvic fixation in patients with pelvic obliquity >15°. Additionally, groups I and III had longer follow-up (34.1 and 28.8 months, respectively) than group II (27.8 months) which showed deterioration in pelvic obliquity. Thus, this gives a clear message that patients in group II require pelvic fixation.
In conclusion, this paper evaluated the indications of pelvic fixation in neuromuscular scoliosis. Our study suggests that patients who have pelvic obliquity less than 15° and do not have pelvic fixation can maintain the correction over a long period, and patients who have pelvic obliquity more than 15° require pelvic fixation to maintain the correction and balance over a long time.
Footnotes
Each author certifies that he has no commercial associations (e.g. consultancies, stock ownership, equity interests, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Allen B, Ferguson R. The Galveston technique of pelvic fixation with Luque rod instrumentation of the spine. Spine. 1984;9:388–394. doi: 10.1097/00007632-198405000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Brook PD, Kennedy JD, Stern LM, Sutherland AD, Foster BK. Spinal fusion in Duchenne’s muscular dystrophy. J Pediatr Orthop. 1996;16(3):324–331. doi: 10.1097/00004694-199605000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Hahn F, Hauser D, Espinosa N, Blumenthal S, Min K. Scoliosis correction with pedicle screws in Duchenne muscular dystrophy. Eur Spine J. 2008;17(2):255–261. doi: 10.1007/s00586-007-0558-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Islam NC, Wood KB, Transfeldt EE, Winter RB, Denis F, Lonstein JE, Ogilvie JW. Extension of fusions to the pelvis in idiopathic scoliosis. Spine. 2001;26(2):166–173. doi: 10.1097/00007632-200101150-00011. [DOI] [PubMed] [Google Scholar]
- 5.King AG, Thomas KA, Eiserloh HL, Mills TE, Pisciotta DN. Analysis of the STIF technique for spino-pelvic fixation: clinical results in 19 patients with neuromuscular scoliosis. J Pediatr Orthop. 2000;20:667–676. doi: 10.1097/00004694-200009000-00023. [DOI] [PubMed] [Google Scholar]
- 6.Lonstein JE, Akbarnia BA. Operative treatment of spinal deformities in patients with cerebral palsy or mental retardation: an analysis of one hundred and seven cases. J Bone Joint Surg [Am] 1983;65:43–55. [PubMed] [Google Scholar]
- 7.McCall RE, Hayes B. Long-term outcome in neuromuscular scoliosis fused only to lumbar 5. Spine. 2005;30(18):2056–2060. doi: 10.1097/01.brs.0000178817.34368.16. [DOI] [PubMed] [Google Scholar]
- 8.McCarthy RE, Bruffett WL, McCullough FL. Rod fixation to the sacrum in patients with neuromuscular spinal deformities. Clin Orthop Relat Res. 1999;364:26–31. doi: 10.1097/00003086-199907000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Miladi LT, Ghanem IB, Draoui MM, Zeller RD, Dubousset JF. Iliosacral screw fixation for pelvic obliquity in neuromuscular scoliosis: a long-term follow-up study. Spine. 1997;22(15):1722–1729. doi: 10.1097/00007632-199708010-00007. [DOI] [PubMed] [Google Scholar]
- 10.Mubarak SJ, Morin WD, Leach J. Spinal fusion in Duchenne muscular dystrophy: fixation and fusion to sacropelvis. J Pediatr Orthop. 1993;13:752–757. doi: 10.1097/01241398-199311000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Peelle MW, Lenke LG, Bridwell KH, Sides B. Comparison of pelvic fixation techniques in neuromuscular spinal deformity correction: Galveston rod versus iliac and lumbosacral screws. Spine. 2006;31(20):2392–2398. doi: 10.1097/01.brs.0000238973.13294.16. [DOI] [PubMed] [Google Scholar]
- 12.Phillips JH, Gutheil JP, Knapp DR. Iliac screw fixation in neuromuscular scoliosis. Spine. 2007);32(14):1566–1570. doi: 10.1097/BRS.0b013e318067dcff. [DOI] [PubMed] [Google Scholar]
- 13.Schoenfelder K, Cheng CL, Hsu LCS, et al. Pelvic obliquity in poliomyelitic scoliosis: correction of pelvic obliquity without fusion to sacrum. Orthop Trans. 1987;11:123. [Google Scholar]
- 14.Sengupta DK, Mehdian SH, McConnell JR, Eisenstein SM, Webb JK. Pelvic or lumbar fixation for the surgical management of scoliosis in Duchenne muscular dystrophy. Spine. 2002;27(18):2072–2079. doi: 10.1097/00007632-200209150-00020. [DOI] [PubMed] [Google Scholar]
- 15.Sussman MD, Little DM, Alley RM, et al. Posterior instrumentation and fusion of the thoracolumbar spine for treatment of neuromuscular scoliosis. J Pediatric Orthop. 1996;16:304–313. doi: 10.1097/00004694-199605000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Weimann RL, Gibson DA, Moseley CF, et al. Surgical stabilization of the spine in Duchenne muscular dystrophy. Spine. 1983;8:776–780. doi: 10.1097/00007632-198310000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Wild A, Haak H, Kumar M, Krauspe R. Is sacral instrumentation mandatory to address pelvic obliquity in neuromuscular thoracolumbar scoliosis due to myelomeningocele. Spine. 2001;26(14):325–329. doi: 10.1097/00007632-200107150-00019. [DOI] [PubMed] [Google Scholar]
- 18.Winter RB. Classification and terminology. In: Lonstein J, Bradford D, Winter R, Ogilvie J, editors. Moe’s textbook of scoliosis and other spinal deformities. 3. Philadelphia, PA: W. B. Saunders; 1994. pp. 39–43. [Google Scholar]
- 19.Whitaker C, Burton DC, Asher M. Treatment of selected neuromuscular patients with posterior instrumentation and arthrodesis ending with lumbar pedicle screw anchorage. Spine. 2000;25(18):2312–2318. doi: 10.1097/00007632-200009150-00008. [DOI] [PubMed] [Google Scholar]