Abstract
Depression, somatisation and pain beliefs influence outcome of several painful musculoskeletal disorders. Their influence on the postoperative outcome of total hip replacement was investigated. A total of 79 patients who underwent primary total hip replacement completed questionnaires preoperatively and six weeks postoperatively addressing depression (Hospital Anxiety and Depression Scale–German version), pain beliefs (Pain Beliefs Questionnaire) and somatisation (Screening of Somatoform Disorders-2) as well as outcome [Western Ontario McMaster Universities Osteoarthritis Index (WOMAC), Medical Outcomes Study 36-Item Short Form (SF-36)]. Depressive patients showed a median preoperative WOMAC sum score of 30 compared to 45 in other patients and a postoperative score of 72 compared to 85, and patients with somatoform disorder of 32 compared to 46 preoperatively and 73 versus 86 postoperatively. Patients with high somatisation and depression scores feel worse in their hips and in general well-being before and after surgery, but they experienced the same benefit from total hip replacement as those with low scores.
Keywords: Total hip arthroplasty, Depression, Somatisation, Pain beliefs, WOMAC, SF-36
Résumé
La dépression due à la somatisation et les douleurs résiduelles peuvent influencer le devenir instantané des troubles musculo-squelettique douloureux des prothèses totales de hanches. 79 patients ont bénéficié d’une prothèse totale de hanche et ont rempli un questionnaire préopératoire et à six mois post-opératoire en ce qui concerne la dépression (HADS-D), les douleurs résiduelles (Pain Beliefs Questionnaire) et la somatisation (SOMS-2). Ils ont également rempli le questionnaire WOMAC et le SF-36. Les patients dépressifs montrent un score moyen WOMAC à 30 et ceci peut être comparé au score de 45 pour les autres patients en préopératoire. En postopératoire le score est à 72 comparé aux autres patients qui sont à 85. Les patients somatisant leurs problèmes ont un résultat à 32 comparés à 46 en préopératoire de même en postopératoire, 76 versus 86. Les patients qui présentent une somatisation importante avec une dépression ont une aggravation de leur score avant et après l’intervention mais ils auront le même bénéfice de la prothèse totale de hanche que ceux qui ont un score inférieur.
Introduction
Total hip replacement (THR) normally leads to a considerable increase in quality of life resulting in a decrease of pain and in an increase of functional ability of the hip joint. But some patients are not satisfied with the outcome of hip arthroplasty although there are neither clinical nor radiological reasons for this. Janis [11] in general surgery and Kimball [12] in heart surgery were perhaps the first to point out the relation between psychological disorders and surgical results. Several authors [10, 13–17] have shown the influence of depression on recovery after treatment of hip fractures. Brander et al. [3] showed that preoperative depression and anxiety were associated with elevated pain at one year after total knee replacement. Pacault-Legendre et al. showed recently that of 64 patients after THR with pain without physical causes a psychiatric origin could be identified in all but one case [19]. To our knowledge, this relationship has not yet been investigated in a longitudinal study of THR.
The aim of this study is to analyse whether psychological influences such as depression, somatisation and pain beliefs have an influence on the postoperative outcome of THR surgery.
Patients and method
The cohort study was approved by the local Ethics Committee (UN 1818 number 207/4.3). Before inclusion, the patients signed an informed consent.
Patients scheduled for elective THR were recruited consecutively. The conditions for inclusion were age over 18 years and the intellectual and linguistic ability to complete the questionnaires. Patients with revision surgery, infection of the hip joint, rheumatic diseases, fractures of the hip and cancer were excluded from the study. Of 139 patients 105 agreed to participate in the study (48 men, 57 women) with an average age of 68 years. The oldest was 81 and the youngest 28 years old. Two of these patients could not be operated upon due to their health status; two were excluded from the study because of rheumatoid arthritis and psoriatic arthritis, respectively, so that 101 completed the questionnaires at baseline investigation. Nineteen did not send back the questionnaires for follow-up examination. Therefore, at follow-up six to eight weeks after surgery 82 patients (78%) had returned the completed questionnaires. In 79 patients (75%) there was complete information on preoperative and postoperative data. Usually patients returned the questionnaires within two weeks. Only two came back half a year later.
The day before surgery at baseline examination the patients had to complete five self-reporting measures.
HADS (Hospital Anxiety and Depression Scale [26]) for depression, in the validated German version [7] (HADS-D). The two subscales (depression, anxiety) of the HADS allow scores of 0–21 points each. A subscore of 7 or less in the subscale depression means that there is no depression, 8–11 means a borderline depression and 12 and more points means that the patient suffers a manifest depression [8].
PBQ (Pain Beliefs Questionnaire) for pain beliefs [5, 24] using a Likert scale, in a translated version, because a German version did not exist. Four individuals translated the questionnaire independently into German, resulting in marginal differences which were discussed with them. The PBQ contains two subscales: organic beliefs (0–32 points) and psychological beliefs (0–16 points). Organic beliefs are preferred by patients who suffer from pain. Walsh and Radcliffe [24] used the PBQ as an instrument to evaluate the quality of pain treatment in patients with low back pain which has no radicular origin. They showed that a decrease of pain goes together with a shift from organic to psychological beliefs.
SOMS-2 (Screening of Somatoform Disorders) for somatisation, which has the identical items as SOMS-7 [21]. SOMS-2 is a symptom list with yes/no answers related to the last two years, whereas SOMS-7 is related to the last seven days. The validated German version was used [20]. SOMS-2 is related to two years and was therefore used at baseline examination. The maximum scores in this questionnaire are 9 points for the subscale pain, 22 for gastrointestinal, 2 for sexual and 14 for pseudoneurological symptoms. The symptom count of the 47 items (sum score) was used.
SF-36 (Medical Outcomes Study 36-Item Short Form) for the quality of life [25], in the validated German version [4]. The SF-36 measures three major health attributes (functional status, well-being and overall health) on eight subscales. These include physical function, role limitations due to physical health, bodily pain, general health, vitality, social function, role limitations due to emotional health and mental health. The scores are calculated on a 0–100 worst to best scale, with 100 being best.
WOMAC (Western Ontario McMaster Universities Osteoarthritis Index), containing the subscales for pain, stiffness and physical function of the hip joint [1, 2], in the validated German version [23]. The WOMAC is a disease-specific, self-administered instrument for evaluation of osteoarthritis in the lower extremities and for evaluating outcome after THR. It consists of 24 items grouped in the three categories of pain (5 items), stiffness (2 items) and physical function (17 items). It was transformed to a 0–100 worst to best scale, with 100 being best.
WOMAC and SF-36 were recently recommended as the most frequently used outcome measures after total hip and knee arthroplasty [6]. Somatisation has been shown to be associated with poor outcome especially in treatment of low back pain [18].
Statistical analysis All data were analysed by means of SPSS (Statistical Package for the Social Sciences 11.0, SPSS Inc., Chicago, IL, USA), using a t-test, Levene’s test for differences of variation and Pearson’s correlation coefficient. The significance level was set at 0.05.
Results
Within the follow-up time there were no dislocations of the hip joints. One patient suffered a deep wound infection and underwent exploration, spacer implantation and replacement. This patient completed the follow-up questionnaire when he was in traction after prosthesis explantation waiting for staged implantation in another hospital.
Table 1 shows the main results of the entire cohort of patients. The HADS values in the subscores depression and anxiety showed no significant difference between baseline and follow-up examination. Taking the cut-off scores for HADS depression subscale by Herrmann [8], seven patients suffered a borderline and nine patients a manifest depression before surgery as well as seven and five, respectively, at follow-up. PBQ scores did not significantly change after surgery.
Table 1.
Baseline and follow-up parameters of the entire collective (N = 79)
| Mean/SD/min./max. | Baseline 1 day preoperatively | Follow-up 8 weeks postoperatively |
|---|---|---|
| HADS, depression | 5.4 ± 3.6 (0–17) | 4.5 ± 3.8 (0–20) |
| HADS, anxiety | 6.1 ± 3.8 (0–15) | 5.4 ± 3.9 (0–21) |
| SOMS-2 | 9.2 ± 6.2 (0–33) | – |
| PBQ, organic | 20.3 ± 4.2 (7–29) | 19.3 ± 4.3 (6–32) |
| PBQ, psychological | 10.0 ± 3.0 (2–16) | 10.7 ± 2.9 (3–16) |
| SF-36, functional status | 30.7 ± 8.7 (16.3–56.7) | 38.9 ± 8.9 (22.2–58.4) |
| SF-36, physical function | 39.4 ± 25.3 (0–100) | 57.5 ± 24.0 (0–100) |
| SF-36, bodily pain | 28.7 ± 15.6 (0–84) | 58.4 ± 21.4 (0–100) |
| WOMAC, sum score | 41.5 ± 20.8 (0–82) | 77.9 ± 17.3 (10–100) |
| WOMAC, pain | 44.6 ± 22.8 (0–96) | 84.2 ± 17.8 (6–100) |
| WOMAC, stiffness | 38.5 ± 24.7 (0–80) | 71.8 ± 22.1 (10–100) |
| WOMAC, physical function | 41.9 ± 24.0 (0–95) | 77.3 ± 18.6 (9–100) |
The SF-36 questionnaire showed a clear postoperative amelioration of all subscales with the exception of role limitations due to emotional and mental health. In particular the subscales pain (+30 points) physical function (+18) and vitality (+10 points) improved considerably. The WOMAC score showed a significant improvement in the subscales and in the total score.
Preoperative and postoperative PBQ scores were correlated neither with outcome nor with the other psychological parameters (Figs. 1 and 2).
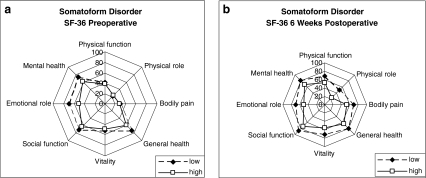
Fig. 1.
SF-36 sum score and subscores in relation to preoperative somatisation measured by the SOMS-2. High somatoform disorder values (squares) were those in the worst 25 percentiles of the cohort (SOMS-2 score 12 as threshold value). Preoperatively and postoperatively the health status of patients with somatoform disorder was worse in most subscales. a Preoperative SF-36 scores in relation to preoperative somatisation. b Postoperative SF-36 scores at 6 weeks in relation to preoperative somatisation
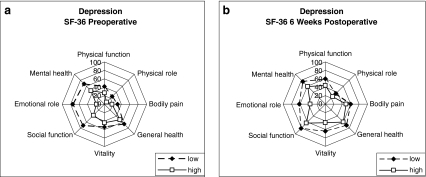
Fig. 2.
SF-36 sum score and subscores in relation to preoperative depression measured by the HADS-D. High depression values (squares) were those defined by Herrmann et al. [9] as borderline depression or manifest depression (threshold value was 8). Preoperatively and postoperatively the health status of patients with depression was worse in all subscales. a Preoperative SF-36 scores in relation to preoperative depression. b Postoperative SF-36 scores at 6 weeks in relation to preoperative depression
The pre- and postoperative HADS-D scores for depression and anxiety correlated with the SOMS-2 somatisation symptom count (p < 0.01). Patients with somatisation or depression had lower scores on the SF-36 scales and a lower WOMAC score preoperatively as well as after surgery (Figs. 3 and 4).
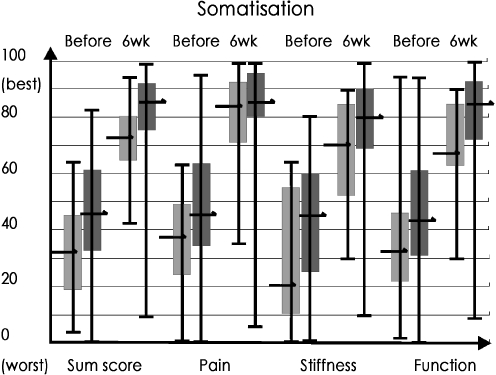
Fig. 3.
WOMAC sum score and subscores preoperative (Before) and 6 weeks postoperative (6 wk) in relation to preoperative somatisation measured by the SOMS-2. High somatoform disorder values were those in the worst 25 percentile (SOMS-2 score 12 as threshold value). Pre- and postoperatively all median WOMAC scores of patients with somatoform disorder (N = 19) were significantly worse than those of other patients (N = 60) on all scales, with the exception of postoperative pain
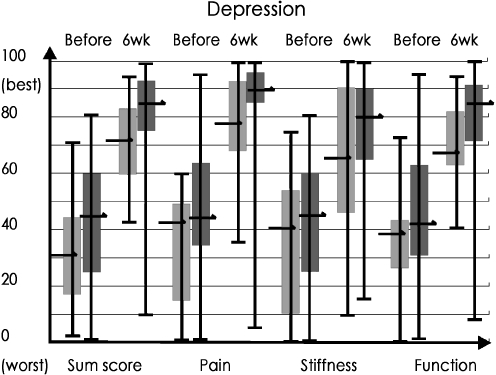
Fig. 4.
WOMAC sum scores and subscores preoperatively in relation to preoperative depression measured by the HADS-D. High depression values were those defined by Herrmann et al. [9] as borderline depression or manifest depression (threshold value was 8). Preoperatively and postoperatively the health status of patients with depression (N = 15) compared to those without (N = 64) was worse in all subscales, with the exception of preoperative stiffness and function
The preoperative and postoperative differences in the WOMAC score between patients with somatoform disorder (Fig. 3) or depression (Fig. 4) in comparison to the rest of the cohort are shown. Depressive patients had a lower median WOMAC sum score of 30 (versus 46) preoperatively and 72 (versus 85) postoperatively. However, the difference of more than 10 median WOMAC points between depressive and non-depressive patients did not change so much from preoperative to postoperative assessment.
Discussion
Some patients suffer from pain or show a relatively poor functional outcome after THR although the X-ray result may be excellent and no obvious adverse events have occurred. Even further examinations like bone scans, lab examinations and ultrasound do not reveal the cause of pain. This article suggests that depression and somatoform disorder may sometimes explain the relatively inferior outcome in some patients after THR.
Both depression and somatoform disorders can be diagnosed before surgery as well as after surgery and may cause an inferior health status, functional status or pain before as well as after operation. The tendency of somatisation is associated with depressive symptoms [22]. This study also shows that there is a significant correlation between preoperatively measured somatisation and preoperatively and postoperatively measured depression.
The presence of a psychological disorder is not a contraindication to an operative intervention. There is rather an independent effect of organic and psychological disorders on health status and hip function. In order to achieve the best result in our patients, both disorders have to be treated.
To our knowledge, this study is the first one dealing systematically with depression, somatisation and pain beliefs before and after THR. Lingard and Riddle [13] used the WOMAC and Beck’s Depression Inventory in total knee replacement patients. They found that psychological distress predicts pain and function subscales at all time points of their study. As in their study we could demonstrate that the changes in the WOMAC scores from preoperative to postoperative for the psychologically distressed patients were not significantly different from those for the non-distressed patients.
The patient can complete the questionnaires for depression and somatisation in 15 min, and the analysis requires two minutes of the surgeon’s or of an assistant’s time. Preoperative screening and the consecutive treatment may improve patient-perceived outcome and may reduce costs. Herrmann et al. [9] with regard to stroke, Mossey et al. [15] with regard to hip fractures as well as Brandner et al. [3] with regard to knee replacement have recommended such a screening in order to optimise treatment, to improve patient-perceived outcome and to reduce the costs of treatment.
Our study has a longitudinal design, showing that preoperative depression and somatisation are associated with a worse outcome at six weeks. The follow-up time in this study does not allow us to draw the conclusion that the difference will continue to exist for a longer time after surgery. However, our results add evidence that somatic pain and functional status are worse in depressive patients and those with somatoform disorder whether severe organic pain is present (preoperative) or ameliorated (six weeks follow-up).
Patients with high somatisation and depression scores felt worse in their hips and in general well-being before and after surgery, but they experienced the same benefit from THR as those with low scores.
Footnotes
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Bellamy N, Buchanan WW. Outcome measurement in osteoarthritis clinical trials: the case for standardisation. Clin Rheumatol. 1984;3:293–303. doi: 10.1007/BF02032334. [DOI] [PubMed] [Google Scholar]
- 2.Bellamy N (1982) Osteoarthritis—an evaluative index for clinical trials. MSc thesis, McMaster University, Hamilton, Ontario, Canada
- 3.Brander VA, Stulberg SD, Adams AD, Harden RN, Bruehl S, Stanos SP, Houle T. Predicting total knee replacement pain: a prospective, observational study. Clin Orthop. 2003;416:27–36. doi: 10.1097/01.blo.0000092983.12414.e9. [DOI] [PubMed] [Google Scholar]
- 4.Bullinger M, Kirchberger I. SF-36 Fragebogen zum Gesundheitszustand. Göttingen: Hofgrefe Verlag für Psychologie; 1998. [Google Scholar]
- 5.Edwards LC, Pearce SA, Turner-Stokes L, Jones A. The Pain Beliefs Questionnaire: an investigation of beliefs in the causes and the consequences of pain. Pain. 1992;51:267–272. doi: 10.1016/0304-3959(92)90209-T. [DOI] [PubMed] [Google Scholar]
- 6.Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster J. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86-A:963–974. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Herrmann C, Buss U, Snaith RP. HADS-D hospital anxiety and depression scale–Deutsche version. Bern: Hans Huber; 1995. [Google Scholar]
- 8.Herrmann C. International experiences with the Hospital Anxiety and Depression Scale—a review of validation data and clinical result. J Psychosom Res. 1997;42:17–41. doi: 10.1016/S0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- 9.Herrmann N, Black SE, Lawrence J, Szekely C, Szalai JP. The Sunnybroke Stroke Study: a prospective study of depressive symptoms and functional outcome. Stroke. 1998;29:618–624. doi: 10.1161/01.str.29.3.618. [DOI] [PubMed] [Google Scholar]
- 10.Holmes J, House A. Psychiatric illness predicts poor outcome after surgery for hip fracture: a prospective cohort study. Psychol Med. 2000;30:921–929. doi: 10.1017/S0033291799002548. [DOI] [PubMed] [Google Scholar]
- 11.Janis IL. Psychological stress. New York: Wiley; 1958. [Google Scholar]
- 12.Kimball CP. Psychological responses to the experience of open heart surgery. Am J Psychiatry. 1969;126:96–107. doi: 10.1176/ajp.126.3.348. [DOI] [PubMed] [Google Scholar]
- 13.Lingard EA, Riddle DL. Impact of psychological distress on pain and function following knee arthroplasty. J Bone Joint Surg Am. 2007;89:1161–1169. doi: 10.2106/JBJS.F.00914. [DOI] [PubMed] [Google Scholar]
- 14.Magaziner J, Simonsick EM, Kashner M, Hebel JR, Kenzora JE. Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol. 1990;45:M101–M107. doi: 10.1093/geronj/45.3.m101. [DOI] [PubMed] [Google Scholar]
- 15.Mossey JM, Knott K, Craik R. The effects of persistent depressive symptoms on hip fracture recovery. J Gerontol. 1990;45:M163–168. doi: 10.1093/geronj/45.5.m163. [DOI] [PubMed] [Google Scholar]
- 16.Mueller-Thomsen T, Tabrizian S, Mittermeier O. Depression bei geriatrischen Patienten mit hüftgelenksnahen Frakturen und deren Auswirkung auf den Rehabilitationsverlauf. Z Gerontol Geriatr. 2003;36:138–142. doi: 10.1007/s00391-003-0092-2. [DOI] [PubMed] [Google Scholar]
- 17.Mutran EJ, Reitzes DC, Mossey J, Fernandez ME. Social support, depression and recovery of walking ability following hip fracture surgery. J Gerontol B Psychol Sci Soc Sci. 1995;50:S354–S361. doi: 10.1093/geronb/50b.6.s354. [DOI] [PubMed] [Google Scholar]
- 18.Nickel R, Egle UT, Rompe J, Eysel P, Hoffmann SO. Somatisation predicts the outcome of treatment in patients with low back pain. J Bone Joint Surg Br. 2002;84:189–195. doi: 10.1302/0301-620X.84B2.12235. [DOI] [PubMed] [Google Scholar]
- 19.Pacault-Legendre V, Anract P, Mathieu M, Courpied JP (2008) Pain after total hip arthroplasty: a psychiatric point of view. Int Orthop. doi:10.1007/s00264-007-0470-2 [DOI] [PMC free article] [PubMed]
- 20.Rief W, Hiller W, Heuser J. SOMS – Das Screening für Somatoforme Störungen. Bern: Hans Huber; 1996. [Google Scholar]
- 21.Rief W, Hiller W. A new approach to the assessment of the treatment effects of somatoform disorders. Psychosomatics. 2003;44:492–498. doi: 10.1176/appi.psy.44.6.492. [DOI] [PubMed] [Google Scholar]
- 22.Sheehan B, Banerjee S. Review: somatization in the elderly. Int J Geriatr Psychiatry. 1999;14:1044–1049. doi: 10.1002/(SICI)1099-1166(199912)14:12<1044::AID-GPS55>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 23.Stucki G, Maier D, Stucki S, Michel BA, Tyndall AG, Dick W, Theiler R. Evaluation einer deutschen Version des WOMAC (Western Ontario and McMaster Universities) Arthroseindex. Z Rheumatol. 1996;55:40–49. [PubMed] [Google Scholar]
- 24.Walsh DA, Radcliffe JC. Pain beliefs and perceived physical disability of patients with chronic low back pain. Pain. 2002;97:23–31. doi: 10.1016/S0304-3959(01)00426-2. [DOI] [PubMed] [Google Scholar]
- 25.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]