Abstract
The sliding compression device, a widely used implant in unstable proximal femoral fractures, suffers from two major limitations: excessive collapse and screw cut-out. Commonly attributed reasons for these are lateral wall comminution and single-point fixation, respectively. We report our experience of stabilising 74 unstable trochanteric fractures, of which 46 cases underwent lateral wall reconstruction using a trochanteric stabilising plate (TSP) in combination with a dynamic hip screw (DHS), and 34 cases with an intact lateral wall had a DHS with an additional anti-rotation screw providing two-point fixation. Fracture consolidation was observed in all cases at an average of 13.56 weeks. Overall functional hip score as per the Salvati and Wilson scoring system was >30 points in 55 patients. Lateral wall reconstruction is an important component in stabilisation of unstable trochanteric fractures and a combination of TSP with a DHS appears to be a useful device to achieve this. Addition of an antirotation screw is likely to enhance the stability further by providing two-point fixation.
Résumé
Le matériel à compression est largement utilisé dans les fractures de l’extrémité supérieure du fémur avec deux limites, d’une part une impaction des fragments et, d’autre part, l’absence de fixité de la vis. Les raisons en sont l’importante communication du mur latéral avec un seul point de fixation. Nous rapportons notre expérience de la stabilisation de 74 fractures trochantériennes instables parmi lesquelles 46 ont bénéficié d’une reconstruction du mur latéral intact et en utilisant une plaque trochantérienne de stabilisation TSP combinée à la DHS et 34 cas présentant un mur latéral ayant bénéficié d’une DHS avec un système de vis anti rotation avec deux points de fixation. La consolidation de la fracture a toujours été observée avec une moyenne de 13,56 semaines. Cependant, le score fonctionnel de la hanche selon Salvati et Wilson était supérieur de 30 points chez 55 patients. La reconstruction du mur latéral est un élément important de la stabilisation des fractures trochantériennes instables. La combinaison d’une plaque TSP avec la vis DHS est un artifice utile pour améliorer cette stabilité. L’ajout d’une vis anti rotation est également profitable de façon à améliorer la stabilité du fait de deux points de fixation.
Introduction
Intertrochanteric fractures of the hip continue to be a challenge for orthopaedic surgeons. Surgical management of trochanteric fractures aims at restoring the prefracture functional status of patients as far as ambulation skills are concerned. A variety of implants of internal fixation have been employed to achieve this goal with variable success. The diversity of fixation devices available for treatment of trochanteric fractures illustrates the difficulties encountered in the actual treatment, and the discussion about ideal implant for such cases still continues. From a mechanical point of view, the dynamic hip screw (DHS), a sliding screw device, has many advantages such as controlled impaction and short operation time. However, use of this device in unstable trochanteric fractures has also been reportedly associated with significant medial displacement of the shaft resulting from excessive sliding of screw within the barrel and a higher incidence of screw cut-out [3, 5, 14]. The intact lateral wall plays a key role in stabilisation of unstable trochanteric fractures by providing a lateral buttress for the proximal fragment, and its deficiency leads to excessive collapse and varus malpositioning [4, 6]. Therefore, maintaining the integrity of this structure should be an important objective in all stabilisation procedures for unstable trochanteric fractures. Moreover, up to 12% of unstable trochanteric fractures show radiologically identifiable rotation of the proximal fragment, when fixed with DHS alone, as DHS provides only single-point fixation over which the proximal fragment can rotate with the movement of hip [13]. This can result in a significant number of nonunions and malunions due to poor bony contact between two fragments [11, 18].
Patients and method
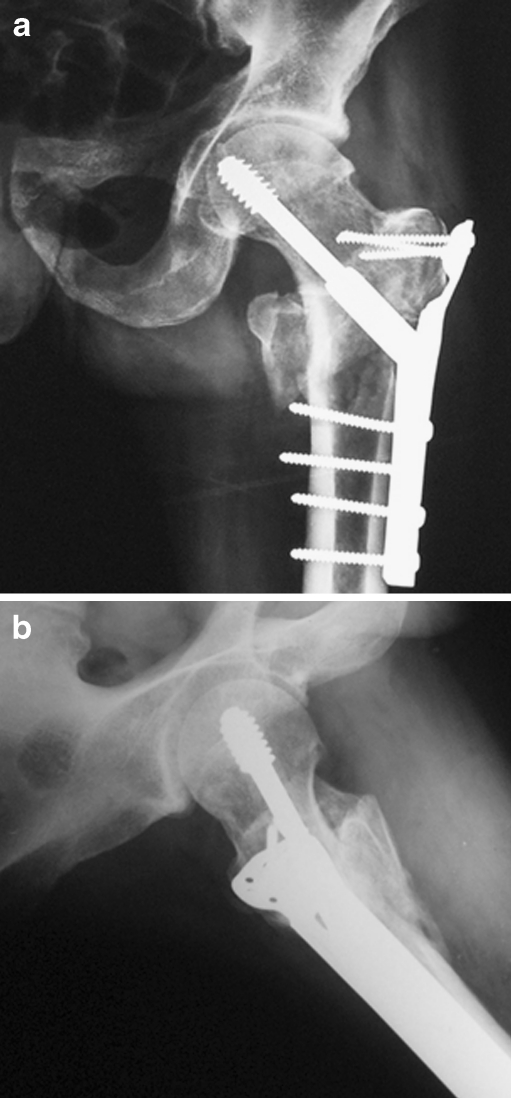
This prospective study comprised 80 consecutive patients, of all ages and either gender with trochanteric fracture. Exclusion criteria included patients with an open fracture, subtrochanteric fracture, intracapsular hip fracture, dementia and previous history of surgery on the proximal femur. All patients were subjected to detailed clinical and radiological examination. Their prefracture ambulatory status was ascertained using Parker’s mobility score [15]. All fractures were classified on the basis of AO Muller classification. Informed consent was obtained from all patients. Closed reduction was done in most of the cases with the exception of seven, which required open reduction to achieve anatomical or near anatomical reduction. All fractures were stabilised with a DHS, which was supplemented with a trochanteric stabilisation plate (TSP) in the presence of lateral wall comminution (46 cases) (Fig. 1a,b). An additional 6.5-mm screw was passed parallel to the DHS through the TSP to act as an antirotation screw while permitting sliding collapse (Fig. 2a, b). If the lateral wall was observed to be intact (34 cases), the DHS was supplemented with a single superiorly placed antirotation screw (Fig. 3). All patients were allowed nonweight-bearing ambulation under the guidance of a physiotherapist on the third postoperative day and began partial weight bearing as soon as possible depending on the quality of bone, stability of biomechanical construction and tolerance of the patient. Patients were followed-up clinically and radiologically in the fracture clinic at regular intervals for possible complications, progress of union and physiotherapy. All patients were followed-up for a minimum period of six months, when they were subjected to final clinical and radiological evaluation, until either the fracture united or fixation failed. Patients were also examined for abductor weakness by performing Trendelenberg’s test as suggested by Hardcastle and Nade [7]. Overall, the clinical outcome was rated as per the Salvati and Wilson scoring system [17] at the time of final follow-up. Final radiological evaluation included any nonunion, malunion, screw cut-out, implant breakage, avascular necrosis of femoral head and excessive sliding of screw.
Fig. 1.
Dynamic hip screw (DHS) supplemented by trochanteric stabilisation plate (TSP). a AP view. b Lateral view
Fig. 2.
Trochanteric stabilisation plate (TSP) with antirotation screw. a AP view. b Lateral view
Fig. 3.

Antirotation screw with dynamic hip screw (DHS) for intact lateral wall
Results
Seventy-four patients were available for the outcome analysis. There were 34 males and 40 females; the average age was 72 years. Fall on a level surface was the most common mode of trauma, accounting for 85% of the cases, with the remainder sustained in high energy road traffic accidents. Prior to injury, 62 of the patients were ambulatory without any walking aid. Average delay to operation from the time of injury was three days (range 2–12 days), which was mostly due to delay in reporting to the hospital. Postoperative X-ray examination showed anatomical reduction in 68 cases, and nonanatomical reduction in six cases. There were two local complications, as well as some systemic complications (Table 1). Clinico-radiological consolidation of the fracture was observed in all cases at an average of 13.56 weeks. Three of the patients complained of persistent pain in the hip region because of impingement of the proximal part of the TSP and were scheduled for hardware removal. Two patients had moderate persistent pain due to varus malunion. The average sliding of the DHS in this study was observed to be 3.4 mm. No limb length discrepancy was observed in any of our cases with anatomical reduction. Six cases had less than anatomical reduction observed in the immediate postoperative period resulting in 7–9 mm of shortening, but none of these cases required a shoe raise. Identifiable rotation on X-rays of the proximal fragment was not observed in any of our cases.
Table 1.
Complications
| Complications | No. of patients |
|---|---|
| Systemic | |
| Chest infection | 7 |
| Urinary tract infection | 3 |
| Urinary retention | 3 |
| Local | |
| Superficial wound infection | 1 |
| Wound haematoma | 1 |
Average score for pain according to the Salvati and Wilson criteria was 8.6 out of 10. Normal walking was resumed in 58 patients, six patients needed a walking aid for long distances and the remaining ten patients required a walking aid even for short distances. Postoperative Parker’s mobility score [15] in our patients was almost comparable to the status before trauma apart from six cases where the score was reduced by one level at the time of final follow-up. Normal range of hip movements and full muscle power was achieved in 34 patients while 25 patients had slight decrease in range of hip movement and the rest of the 15 patients had limited flexion and abduction with fair muscle power. Hip abductor function was observed to be adequate in most of the cases at final follow-up. Normal function was regained in 34 patients, while very little restriction was observed in 26 patients and the remaining 14 patients had restricted normal activities but were able to do most of the housework and shop freely. The Salvati and Wilson score for overall hip function was >30 points in 55 patients and >20 points in the remaining 19 patients.
Discussion
Most authors have reported some incidence of failure of union in their series of trochanteric fractures following the use of DHS [8, 16]. The primary complications of trochanteric fractures fixed with DHS are postoperative late collapse leading to shortening of the limb and screw cut-out resulting in coxa vara [2, 10, 19]. The mean sliding in our study was an average of 3.4 mm which was significantly lower than previous studies using DHS alone. Jacobs et al. [9] have reported an average sliding of 5.3 mm in stable fractures and 15.7 mm in unstable fractures. Similarly, Larson et al. [12] have reported average sliding of 6.3 mm in stable fractures and 12.4 mm in unstable fractures. Hardy et al. and Steinberg et al. [18] have reported an average sliding of 10.2 mm and 9.3 mm, respectively. No significant limb length discrepancy was observed in our study, which compares favourably to the reports in literature by Frohlich and Benko et al. [3] (>1 cm shortening in half of their cases) and Ecker et al. [3] (average 2 cm shortening in 12 out of 62 cases). These figures do highlight the importance of anatomical reduction at the time of surgery but this is possible only if stability of these fractures is achieved by buttressing the lateral wall. These findings reinforce the results of Babst et al. [1], who also reported significant reduction in excessive collapse and subsequently reduced limb length discrepancy by using a TSP in combination with the DHS. The stability may also have been further improved by the additional superiorly placed 6.5 mm cancellous lag screw providing two point fixation. The results of assessment for hip abductor function at final follow-up were significantly better, and this is supportive of the view that the DHS in combination with TSP is likely to ensure a better abductor function due to stability provided to the greater trochanter.
A shorter learning curve is consistent with a better outcome of the procedure since it reduces the operative time and the incidence of operative complications. For surgeons familiar with the DHS, the additional surgical time for adding modular TSP over DHS will only be marginal. However, theoretically, the slight increase in the operative time and a wider exposure required for a DHS and TSP may also marginally increase the blood loss. The mechanism of action of the TSP has not been properly evaluated in biomechanical studies. However, TSP seems to act as a buttress plate against the medialisation of the distal fracture fragment often seen in unstable fractures stabilised with the sliding screw plate systems alone. In unstable trochanteric fractures owing to posterior, medial and lateral comminution, the collapse at the fracture site that occurs with sliding hip screw fixation may be more than usual. In such a situation abductor muscle weakness and its consequent fatigability is likely to be greater. The functional results in this study were graded as excellent in 74% of the cases and good in 26% of the cases according to the Salvati and Wilson scoring system. These observations do indicate that lateral wall reconstruction significantly lessened the incidence of lateralisation of the greater trochanter with limited telescoping of comminuted fragments following weight bearing. These two factors resulted in better hip abductor function and final Salvati-Wilson functional score with restoration of prefracture mobility. This study therefore does indicate that addition of a TSP over DHS is likely to improve the stability of fracture fixation, while at the same time permitting a controlled sliding collapse. Improved bony contact between proximal and distal fragments by stabilisation of the comminuted lateral wall is likely to improve the chances of union and maintenance of adequate lever arm. An additional antirotation screw effectively prevents the rotation of the proximal fragment.
Conclusion
The combination of TSP and DHS is a useful technique in the treatment of unstable trochanteric femoral fractures. It creates a biomechanically stable construction allowing reconstruction of the lateral wall to maintain adequate lever arm and abductor strength. In addition it allows passage of an antirotation screw, thereby providing two-point fixation with additional rotational stability. Superior overall functional and radiological outcome in patients with unstable trochanteric fractures does indicate that the combination of DHS and modular TSP is likely to be a better option in the management of these fractures as compared to DHS alone.
References
- 1.Babst R, Renner N, Biedermann M, Rosso R, Hebere M, Harder F, Regazzoni P. Clinical results using the trochanter stabilizing plate (TSP): the modular extension of the dynamic hip screw (DHS) for internal fixation of selected unstable intertrochanteric fractures. J Orthop Trauma. 1998;12:392–399. doi: 10.1097/00005131-199808000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Davis TRC, Sher JL, Horsman A, Simpson M, Porter BB, Checketts RG. Intertrochanteric femoral fractures: mechanical failure after internal fixation. J Bone Joint Surg. 1990;72B:26–31. doi: 10.1302/0301-620X.72B1.2298790. [DOI] [PubMed] [Google Scholar]
- 3.Ecker ML, Joyce JJ, Kohl JE. The treatment of trochanteric hip fractures using a compression screw. J Bone Joint Surg. 1975;87-A(1):23–27. [PubMed] [Google Scholar]
- 4.Frohlich P, Benko T. DHS (dynamic hip screw) osteosynthesis in the management of femoral fractures in the hip region and the place of this method in the treatment of such injuries. Magy Traumatol Ortop Kezseb Plasztikai Sch. 1993;36(1):59–64. [PubMed] [Google Scholar]
- 5.Gadegone WM, Salphale YS. Proximal femoral nail—an analysis of 100 cases of proximal femoral fractures with an average follow up of 1 year. Int Orthop. 2007;31(3):403–408. doi: 10.1007/s00264-006-0170-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gotfried Y. The lateral trochanteric wall: a key element in the reconstruction of unstable pertrochanteric hip fractures. Clin Orthop Relat Res. 2004;425:82–86. doi: 10.1097/01.blo.0000132264.14046.c2. [DOI] [PubMed] [Google Scholar]
- 7.Hardcastle P, Nade S. The significance of the Trendelenburg test. J Bone Joint Surg. 1985;67-B:741–746. doi: 10.1302/0301-620X.67B5.4055873. [DOI] [PubMed] [Google Scholar]
- 8.Hardy DC, Descamps PY, Krallis P, Fabeck L, Smets P, Bertens CL, et al. Use of an intramedullary hip screw compared with a compression hip screw with a plate for intertrochanteric femoral fractures: a prospective, randomized study of one hundred patients. J Bone Joint Surg Am. 1998;80(5):618–630. doi: 10.2106/00004623-199805000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Jacobs RR, Armstrong JH, Whitaker JH, Pazell J. Treatment of intertrochanteric hip fractures with a compression hip screw and a nail plate. J Trauma. 1976;16(8):599–602. doi: 10.1097/00005373-197608000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Jones HW, Johnston P, Parker M. Are short femoral nails superior to the sliding hip screw? A meta-analysis of 24 studies involving 3279 fractures. Int Orthop. 2006;30(2):69–78. doi: 10.1007/s00264-005-0028-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kyle RF, Gustilo RB, Premer RF. Analysis of six-hundred and twenty-two intertrochanteric hip fractures. J Bone Joint Surg. 1979;61-A:216–221. [PubMed] [Google Scholar]
- 12.Larsson S, Friberg S, Lars-Ingvar H. Trochanteric fractures: influence of reduction and implant position on impaction and complications. Clin Orthop Relat Res. 1990;259:130–139. [PubMed] [Google Scholar]
- 13.Lustenberger A, Ganz R. Epidemiologie trochanterer femur fracturen uber 2 jahrzehnte (1972–1989) Unfallchirurg. 1995;98:278–282. [PubMed] [Google Scholar]
- 14.Madsen JE, Naess L, Aune AK, Alho A, Ekeland A, Stromsoe K. Dynamic hip screw with trochanteric stabilzing plate in the treatment of unstable proximal femoral fractures: a comparative study with the Gamma nail and compression hip screw. J Orthop Trauma. 1998;12(4):241–248. doi: 10.1097/00005131-199805000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Parker MJ, Palmer CR. A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg. 1993;75-B:797–798. doi: 10.1302/0301-620X.75B5.8376443. [DOI] [PubMed] [Google Scholar]
- 16.Rha JD, Kim YH, Yoon SI, Park TS, Lee MH. Factors affecting sliding of the lag screw in intertrochanteric fractures. Int Orthop. 1993;17:320–324. doi: 10.1007/BF00181709. [DOI] [PubMed] [Google Scholar]
- 17.Salvati EA, Wilson PD. Long term results of femoral head replacement. J Bone Joint Surg Am. 1973;55A:516–524. [PubMed] [Google Scholar]
- 18.Steinberg GC, Desai SS, Kornwitz NA, Sullivan TJ. The intertrochanteric hip fracture. A retrospective analysis. Orthopaedics. 1988;11:265–273. doi: 10.3928/0147-7447-19880201-06. [DOI] [PubMed] [Google Scholar]
- 19.Swiontkowski MF, Harrington RM, Keller TS. Torsion and bending analysis of internal fixation techniques for femoral neck fractures: the role of implant design and bone density. J Orthop Res. 1987;5(3):433–444. doi: 10.1002/jor.1100050316. [DOI] [PubMed] [Google Scholar]