Abstract
We performed an opening wedge osteotomy of the first cuneiform for the correction of all degrees of hallux valgus deformities. A wedge-shaped graft maintained the open wedge osteotomy and decreased the metatarsocuneiform joint inclination to correct the main angles of the hallux valgus. This procedure was performed for 101 feet of 63 patients (two men and 61 women). Fifteen feet benefited from a shortening of P1. The average age was 42 (16 to 84) years with a mean follow-up of 7.7 (1.5 to 14.8) years. We evaluated the M1-P1 and the M1-M2 angles, the joint congruency and the position of the lateral sesamoid. The clinical examination was graded by the AOFAS score which includes comprehensive assessment of pain, function and alignment and the subjective assessment of patients. The clinical AOFAS score improved from 35.24 points preoperatively to 86.36 postoperatively and from 33.25 to 88.03 points in severe deformity. The subjective rating was 44.44% excellent, 41.27% good, 9.52% fair and 4.76% poor. The M1-P1 angle improved from 29.38° to 16.28° and the M1-M2 angle from 14.36° to 10.34°. In the 42 severe feet deformity, these angles improved respectively from 45.58° to 19.58° and from 18.51° to 11.16°. This technique allowed an accurate correction of the main angles of hallux valgus with different degrees of deformity and avoided the complications related to different types of osteotomies achieved along the first metatarsal. After a long follow-up, we demonstrated a durable result while 86% of patients proved excellent and good results according to the AOFAS score.
Introduction
Surgical correction of hallux valgus has remained a challenge over the last century such that more than 100 procedures have been described. The aim of the surgery is to achieve correction of the metatarsus primus varus, which is an important component of the hallux valgus. However, all techniques have addressed the first metatarsal and the first phalanx. Different sites for osteotomy have been suggested, e.g. proximal [1–5] or distal [6–9], and different types of osteotomies, e.g. opening wedge [1, 2, 10], closing wedge [3, 4, 11], Z-shape cut [12–16], chevron [6, 7, 17] or crescentic osteotomy [18].
The choice of procedure remains controversial, but it is well accepted that distal osteotomies of the first metatarsal are unable to achieve a high degree of correction, and proximal osteotomies are therefore more often recommended for severe hallux valgus deformities. While distal osteotomies are at risk of avascular necrosis of the first metatarsal head and shortening as a result of excessive bone loss, it is also logical to perform proximal osteotomy for mild and moderate hallux valgus.
In our series, for the correction of all degrees of hallux valgus deformities, we performed an osteotomy more proximal than those described above—by doing an opening wedge osteotomy of the first cuneiform. This procedure allows an accurate correction of the metatarsus primus varus and helps avoid the complications that can occur along the first metatarsal with other types of osteotomies.
Technique
A dorsomedial incision was performed just proximal to the interphalangeal joint on the dorsomedial aspect of the great toe. The capsule is incised in a V-shaped pattern pointed proximally and sutured in a Y-shaped pattern at the end of the operation. The medial eminence is not removed.
A dorsal longitudinal incision was made to the dorsal aspect of the first web space. It allowed a release of both insertions of the adductor tendon (on the base of the proximal phalanx and into the lateral sesamoid) and incision of the lateral capsule. The great toe was forcefully bent toward the medial side to completely sever the remainder of the lateral capsule of the metatarsophalyngeal joint.
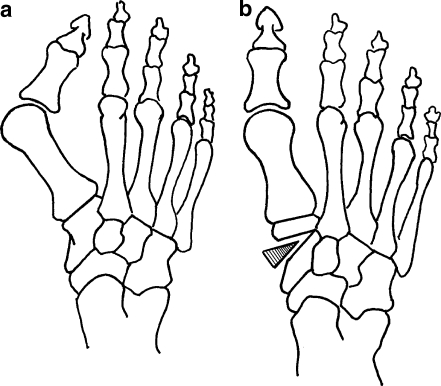
For osteotomy of first cuneiform, we performed a longitudinal incision measuring 20 mm and beginning over the cuneiform-first metatarsal joint (Fig. 1). The tibialis anterior tendon is oblique and located under a thin aponeurosis; it was lifted posteriorly with an elevator. The cuneiform-first metatarsal joint was identified, and the osteotomy was performed 10 mm proximal to the joint, at the groove of the tibialis anterior tendon. This definite level of osteotomy was marked on the X-ray as a varus wedge shape at the medial aspect of the first cuneiform (Fig. 2a). Using a 5-mm wide saw blade, the osteotomy was performed at the distal part of the cuneiform, parallel to the cuneiform-first metatarsal joint, making an angle of 20 degrees with the frontal plane. The dorsal and plantar aspects of the osteotomy were completed using a small osteotome.
Fig. 1.
To approach the first cuneiform, an incision of 20 mm was performed longitudinally over the first cuneiform, beginning at the cuneiform-first metatarsal joint
Fig. 2.
a The level of osteotomy is defined as the varus wedge shape at the medial aspect of the first cuneiform. b A wedge-shaped graft maintains the opening wedge osteotomy and reduces the first metatarsal varus
A Kirschner wire 20/10 fixed temporary in the distal fragment allowed the opening of the osteotomy, leaving the site of osteotomy free of instruments. This manoeuvre was facilitated with lateral displacement of the first metatarsal head by pushing it toward the fifth metatarsal bone. The width of the open wedge is related to the angle of correction, 1 mm for each degree of correction. A 5–10-mm wedge-shaped graft, cut from a neck of the femur allograft, maintained the opening wedge osteotomy and reduced the first metatarsal varus (Fig. 2b).
To reinforce the stability of the osteotomy, a mini-plate of a staple shape was used to avoid the removal of the device, but in many cases when this was not available two K-wires 20/10 were introduced from the distal wedge across the graft and removed after six weeks. The presence of stiffness at the metatarso-phalangeal joint in patients with long first ray indicates the need for a shortening first phalangeal osteotomy. This is achieved, without varisation effect, at the proximal shaft of the phalanx and fixed with two pins. At this stage, the hallux valgus deformity should be adequately corrected without performing traction at the medial metatarso-phalangeal capsule.
Materials and methods
Between 1993 and 2006, an opening wedge osteotomy of the first cuneiform in combination with lateral soft-tissue release and suture of the medial aspect of the capsule were performed for 101 feet of 63 patients (14 right side, 11 left side, 38 bilateral) for the correction of hallux valgus and metatarsus primus varus. Fifteen feet benefited from a shortening osteotomy of P1 without producing a varus deviation by this procedure. The mean age of two men (2 feet) and 61 women (99 feet) was 42 (range, 16–84) years, and the mean follow-up at the time of the study was 7.7 (range, 1.5–14.8) years. All procedures were performed by the senior author, and the mean operating time decreased significantly with his experience (range, 40–80 min).
Dorsoplantar and lateral weight bearing radiographs were performed preoperatively, at different intervals and at the last follow-up. The following criteria were evaluated: the hallux valgus angle (M1-P1 angle), which is formed by the axes of the first metatarsal and the first proximal phalanx; the first intermetatarsal angle (M1-M2 angle), formed by the axes of the first and the second metatarsal; the joint congruency [19]; the position of the lateral sesamoid [20]; and the presence of osteoarthritis of the cuneiform-first metatarsal joint and the metatarso-phalangeal joint. All the measurements were performed by the second author, without participation of the surgeon. According to Mann and Coughlin [21], a mild hallux valgus is characterised by an M1-P1 angle of less than 20 degrees, or M1-M2 angle of less than 11 degrees and subluxation of the lateral sesamoid of less than 50%, moderate hallux valgus by M1-P1 from 20–40 degrees, M1-M2 from 11–16 degrees, subluxation of the lateral sesamoid from 50–75 degrees and severe hallux valgus by M1-P1 of more than 40 degrees, M1-M2 of more than 16 degrees, or subluxation of the lateral sesamoid of more than 75%.
At the end of the follow-up, patients were clinically examined and graded by a hallux metatarsophalangeal interphalangeal scale recommended by the American Orthopaedic Foot and Ankle Society (AOFAS-score) [22] which includes comprehensive assessment of pain (max 40), function (max 45) and alignment (max 15). For the patients operated upon before the determination of the AOFAS score, the preoperative examination was assumed from the clinical records. For subjective assessment, the patients were also asked, by an independent investigator, to compare their pain, cosmetic, and functional results to their preoperative situations, using the statements 'excellent', 'good', 'fair' and 'poor', according to Coughlin [23]. We considered this method of self-assessment more sensitive in evaluating changes than a scale with different values for different evaluations.
Results
Clinical outcome
At the end of the follow-up, the mean AOFAS score improved from 35.24 (standard deviation 16.83) preoperative to 86.36 (SD 18.59) postoperative points. When the different subgroups of the global AOFAS had been defined, we found an improvement of the pain score from 6.06 (SD 10.86) to 33.53 (SD 10.52) points, the function score from 26.91 (SD 8.09) to 38.45 (SD 9.59) points and the alignment score from 1.85 (SD 3.39) to 14.47 (SD 1.79) points. In patients with severe deformity, the score improved from 33.25 (SD 14.72) to 88.03 (SD 18.36) points.
The different subgroups of the function score showed that daily activities improved from 6.1 preoperative to 9 postoperative points, the footwear score improved from 6.5 to 9.2 points; only ten patients (15%) still required comfort footwear at last follow-up, but no notable custom-made shoes. Metatarsalgia and mobility of the big toe had a preoperative score of 12 points and a postoperative score of 16.74 points. Callus formation underneath the big toe and adjoining metatarsal heads was noted preoperatively in 32 patients; at last follow-up it was still observed in 16 patients and it appeared secondarily in two patients.
The patients who benefited from an osteotomy of P1 (15 feet) had a mean age of 46.5 years. They showed an improvement of the AOFAS score from 35.75 (SD 14.62) preoperative to 88.08 (SD 11.79) postoperative points, the pain score from 8 to 36 points, the function score from 26.9 to 39.7 points and the alignment score from 0.8 to 13.6 points.
In the three age groups—under 30 years old (19 patients; first group), 30–50 years old (22 patients; second group) and above 50 years old (22 patients; third group)—the AOFAS scores improved, respectively, from 36.39 (SD 12) preoperative to 90.02 (SD 12.81) postoperative points (first group), from 35.7 (SD 21.92) to 79.4 (SD 24.81) points (second group) and from 30.39 (SD 12.29) to 89.96 (SD 9.00) points (third group). Considering that the second age group displayed a lower score, the pain score improved from 9.09 to 31.37 points, the function score from 27.09 to 34.32 points and the alignment score from 2.55 to 14.46 points.
Subjective outcome
The subjective ratings of the operation by the patients for global results was excellent in 28 patients (44.44%) with 17 bilateral deformities, indicating that the patients were very satisfied with mild or no pain and could walk without difficulty; 26 patients (41.27%) with 15 bilateral deformities considered the result as good, indicating that the patient was satisfied, had mild pain and could walk without or with mild difficulty; it was fair in six patients (9.52%) with moderate pain and some difficulty in walking; and it was poor in three patients (4.76%) because they continued to have pain and regretted having had the surgery.
The patients who benefited from a shortening of P1, considered the result to be excellent in six cases, good in eight cases and fair in one case.
Comparing the three age groups described above, 18 of 19 patients of less than 30 years old claimed to have good and excellent results. This is also true for 14 of 22 patients between 30 and 50 years old and 17 of 22 patients over 50 years old. The other patients in the three different groups (14%) considered their results fair and poor.
Radiological outcome
Considering the values of preoperative M1-P1 and M1-M2 angles and the position of the lateral sesamoid, we had mild deformity in 4%, moderate in 54% and severe in 42% of cases. The radiological evaluation revealed an improvement of M1-P1 angle from 29.38 (SD 9.25) degrees preoperatively to 16.28 degrees (SD 9.45) postoperatively, and M1-M2 angle from 14.36 (SD 4.77) to 10.34 (SD 3.55) degrees. Considering the 42 severely deformed feet, the mean M1-P1 angle improved from 45.58 (SD 6.75) to 19.55 (SD 16.20) degrees, and M1-M2 angle from 18.51 (SD 3.53) to 11.16 (SD 4.04) degrees. Incongruent first metatarsophalangeal joint was observed in 85 feet preoperatively and it was still present in six feet postoperatively.
In the group of 15 feet who benefited from an osteotomy of P1, the M1-P1 angle improved significantly from 30.81 (SD 10.17) degrees preoperatively to 14.83 (SD 4.44) degrees postoperatively and M1-M2 angle from 12.81 (SD 5.68) to 8.58 (SD 5.68) degrees. Five feet had osteoarthritis of M1-P1 articulation before the operation and three feet developed osteoarthritis secondarily. In the three age groups, the M1-P1 angle decreased from 28.38 (SD 7.44) to 18.4 (SD 7.44) degrees in the first group, from 29.38 (SD 9.69) to 15.15 (SD 9.69) degrees in the second group and from 29.65 (11.45) to 20.47 (SD 8.47) degrees in the third group.
Osteoarthritis of the M-P joint was noted in 27 feet, 15 of them appeared after the operation (nine cases stage 2 and six stage 3 of osteoarthritis) with an average age of 47.3 (range, 19–70) years at the time of the surgery. Osteoarthritis of the cuneiform-first metatarsal joint appeared in eight cases: five cases with subchondral sclerosis and one case with severe osteophytes. Three of them benefited from a shortening of P1. We did not observe any migration of the grafts or non-union; there were no differences in the stability between pins and mini staple fixation.
Discussion
Hallux valgus is characterised by a lateral deviation of the great toe; it is a clinical deformity which requires the measurement of many angles on the foot X-ray to determine the site of the deformity and the relationships of the different bones. It has been proven by many authors [24–27] that the mean angle of M1-M2 in patients with hallux valgus is greater than 9 degrees, and the M1-P1 angle is more than 15 degrees. They also concluded a significant relationship between these two defined angles, but the mean angle between the axes of M1-M5 was comparable to that of normal feet.
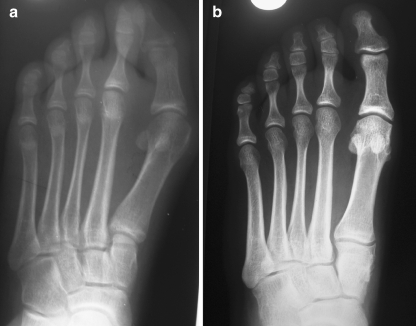
Tanaka et al. [26] confirmed these findings and reported, using an interesting two-dimensional coordinate system, that the surface of the first metatarsocuneiform joint is inclined medially in patients who have hallux valgus (Fig. 3). This finding was also confirmed in an anatomical study carried out by Haines and McDougall [28]. According to radiographic analysis of a group of normal feet and a group with hallux valgus, Tanaka et al. concluded that the site of origin of metatarsus primus varus in patients who had hallux valgus is the first metatarsocuneiform joint. Several kinds of hallux valgus operative techniques do not take into consideration the medial inclination of the first metatarsocuneiform joint and do not allow restoration of its normal anatomy. However, all the osteotomies performed along the first metatarsal to correct the varus create necessary deformities at their different levels, even the basal wedge osteotomies (opening or closing) which are performed close to the metatarsocuneiform joint. The opening wedge osteotomy of the first cuneiform is the procedure of choice to decrease the metatarsocuneiform joint inclination (Figs. 4, 5 and 6) because it allows reduction of the main angles of the hallux valgus and avoids creating malunion of M1 [14] or other deformities of the first ray evident in other osteotomies.
Fig. 3.
a Preoperative anteroposterior weight bearing radiograghs of left foot of 16-year-old female shows the obliquity of the first metatarsomedial-cuneiform joint. b Twelve years after the open wedge osteotomy of the cuneiform, the radiograph shows the decrease of medial inclination of this joint
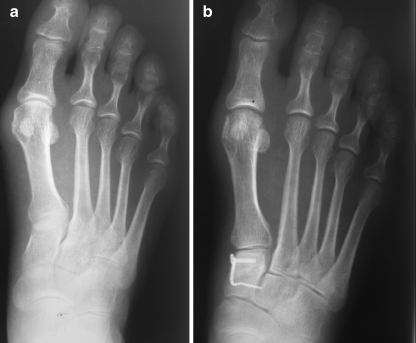
Fig. 4.
a Preoperative anteroposterior radiograph of left foot of 28-year-old female. b The result three years after open wedge osteotomy of the first cuneiform and fixation with staple
Fig. 5.
a Preoperative anteroposterior radiograph of right foot of 48-year-old female. b Postoperative radiograph shows the fixation of the open wedge osteotomy and bone graft by three pins. c The result five years after the surgery
Fig. 6.
a Preoperative anteroposterior radiograph of right foot of 50-year-old female. b The radiograph, four years after open wedge osteotomy stabilised with a staple, shows decrease of the medial inclination of the first metatarsomedial-cuneiform joint
Because the site of the cuneiform’s osteotomy is farther from the M1-P1 joint than other osteotomies, the open wedge allows greater lateral displacement of the first metatarsal head and important correction of deformities. The opening manoeuvre can be performed with accuracy to reduce the M1-M2 angle, whatever the preoperative value. However, the mean reduction of the M1-P1 angle was remarkable, 29.38 (SD 9.25) degrees preoperatively to 16.28 (SD 9.45) degrees at follow-up, and the M1-M2 angle from 14.36 (SD 4.77) to 10.34 (SD 3.55) degrees. Good results were also obtained in the severe deformity group for both angles: M1-P1 from 45.58 (SD 6.75) to 19.55 (SD 16.20) degrees and M1-M2 angle from 18.51 (SD 3.53) to 11.16 (SD 4.04) degrees. While all the extra-articular osteotomies do not change the articular orientation or the congruency of the metatarsophalangeal joint, we consider that soft tissue release, especially of the lateral capsule of the M1-P1 joint, was necessary to obtain a high rate of congruency (96%) postoperatively, but traction at the medial metatarsophalangeal capsule should be gently managed to avoid hypercorrection. In patients with long first ray (15 cases), shortening of P1 released the stiffness of the M-P joint and provided better correction of the M1-P1 hallux valgus angle; this was demonstrated by a mean postoperative value of 14.83 degrees, which was inferior to that of the whole group (16.28 degrees).
Taking into consideration that the shape of the great toe was the most frequent indication for surgery rather than the presence of pain in most of the cases, the subjective assessment particularly reflected the patients' cosmetic satisfaction, which was excellent or good in 86% of cases. Also, the mean global AOFAS score improved significantly from 35.24 (SD 16.83) to 86.36 (SD 18.59) points with a markedly satisfying result for pain from 6.06 (SD 10.86) to 33.53 (SD 10.52) points, function from 26.91 (SD 8.09) to 38.45 (SD 9.59) points and alignment from 1.85 (SD 3.39) to 14.47 (SD 1.79) points. The mean postoperative AOFAS score (86.36 points) is comparable to the results reported in the literature [12, 13] with a lower preoperative AOFAS score (35.24 points) in our series. The patients with severe deformity noted a remarkable clinical improvement, from 33.25 (SD 14.72) to 88.03 (SD 18.36) points, comparable to the results reported in the literature [13, 29].
When we consider the AOFAS scores of the three age groups at the time of the surgery, the differences between the pre and postoperative scores were comparable in the first group (54 points) and the third group (59 points), but this difference was lower in the second group (44 points) with a higher rate of poor and fair results (8 of 22). Although the second group (30–50 years old) had lower scores, the radiographic results demonstrated a better correction of M1-P1 angle from 29.38 (SD 9.69) to 15.15 (SD 9.69) degrees compared to group 1 which was from 28.38 (SD 7.44) to 18.4 (SD 7.44) degrees and group 3 from 29.65 (SD 11.45) to 20.47 (SD 8.47) degrees. Considering the postoperative AOFAS subscores of the second group, the pain score (31.37 points) and the alignment score (14.46 points) were comparable to the global results of our study (33.53 points and 14.47 points, respectively), but the function score (34.32 points) was particularly inferior to the mean value of the whole group (38.45 points). The latter result reflects the particular requests of the patients between 30 and 50 years of age for functional activity and specific footwear.
The patients who underwent a shortening of P1 had a mean age of 46.5 years. They demonstrated a remarkable subjective assessment (14 of 15 cases had excellent or good results) and an improvement of the clinical assessment between pre and postoperative score (53 points) superior to that of the second group (44 points). Comparing the results of the P1 group versus the second group, the improvement of pain (28 points versus 22 points), function (12 points versus 7 points) and alignment score (13 points versus 12 points) could be related to the effect of shortening of the first ray [30], which allowed a more subjective and functional satisfaction for patients.
The concept of first ray sagittal hypermobility as a primary underlying factor predisposing to hallux valgus was accepted by many authors [31–33] who demonstrated a significant decrease of the metatarsocuneiform joint motion after surgery, while others denied the role of hypermobility of this joint in the genesis of hallux valgus [34]. Between these controversial hypotheses we consider that stabilisation of the metatarsocuneiform joint is an important objective in the surgical treatment. It was Lapidus [35] in 1934 who also suggested a relationship between metatarsocuneiform joint hypermobility and hallux valgus and recommended metatarsocuneiform arthrodesis to stabilise the first ray. The reorientation of medial inclination of the first metatarsocuneiform joint after opening wedge osteotomy of the cuneiform should decrease absolutely the mobility of the articulation. This manoeuvre could be at the origin of osteoarthritis of the first metatarsocuneiform joint developed in eight cases (12.69%), in spite of shortening of P1 in three of them. Concerning the osteoarthritis of the M-P joint (Fig. 7) observed in 15% of cases, it could be considered secondary to the lengthening of the first ray or an increased distal metatarsal articular angle, but it was also reported in the proximal crescentic osteotomy of the metatarsus with variable rates, e.g. 24% in a study by Mann et al. [5] and 12% in a study by Zettl et al. [36].
Fig. 7.
a Preoperative anteroposterior radiograph of a left foot of an 80-year-old female with incongruent M-P joint. b The radiograph four years after open wedge osteotomy shows conservation of the correction with mild osteoarthritis of the M-P joint
We did not observe complications, contrary to the currently popular technique of Scarf osteotomy which showed multiple perioperative pitfalls such as intraoperative split of the first metatarsal or postoperative stress fracture [14, 37]. Osteotomy of the first cuneiform also avoids the complications related to the fragility of bone in old patients; we emphasise the difficulty in correcting a failed distal, proximal or Scarf osteotomy, while cuneiform osteotomy does not break with other surgical procedures.
Conclusion
The opening wedge osteotomy of the first cuneiform is an original technique which has demonstrated, after a long follow-up, a lasting correction of the hallux valgus with different degrees of deformity. The opening manoeuvre is achieved with accuracy to reduce the medial inclination of the metatarsocuneiform joint avoiding complications and malunions of the first metatarsal which occur with other techniques of osteotomy. Considering the clinical and radiological assessments, this procedure has proved its efficacy, and confirmed by the subjective assessment of the patients, particularly in patients with severe deformities.
References
- 1.Limbird TJ, DaSilva RM, Green NE. Osteotomy of the first metatarsal base for metatarsus primus varus. Foot Ankle. 1989;9:158–162. doi: 10.1177/107110078900900402. [DOI] [PubMed] [Google Scholar]
- 2.Simmonds FA, Menelaus MB. Hallux valgus in adolescents. J Bone Joint Surg. 1960;42-B(4):761–768. [Google Scholar]
- 3.Resch S, Stenström A, Egund N. Proximal closing wedge osteotomy and adductor tenotomy for treatment of hallux valgus. Foot Ankle. 1989;9:272–280. doi: 10.1177/107110078900900604. [DOI] [PubMed] [Google Scholar]
- 4.Wanivenhaus AH, Feldner-Busztin H. Basal osteotomy of the first metatarsal for the correction of metatarsus primus varus associated with hallux valgus. Foot Ankle. 1988;8:337–343. doi: 10.1177/107110078800800610. [DOI] [PubMed] [Google Scholar]
- 5.Mann RA, Rudicel S, Graves SC. Repair of hallux valgus with a distal soft-tissue procedure and proximal metatarsal osteotomy. A long-term follow-up. J Bone Joint Surg. 1992;74A:124–129. [PubMed] [Google Scholar]
- 6.Mitchell LA, Baxter DE. The chevron-Akin double osteotomy for correction of hallux valgus. Foot Ankle. 1991;12:7–14. doi: 10.1177/107110079101200102. [DOI] [PubMed] [Google Scholar]
- 7.Wilson JN. Oblique displacement osteotomy for hallux valgus. J Bone Joint Surg. 1963;45B(3):552–556. [PubMed] [Google Scholar]
- 8.Coughlin MJ. Chevron procedure. Contemp Orthop. 1991;23:45–49. [Google Scholar]
- 9.Johnson KA, Cofield RH, Morrey BF. Chevron osteotomy for hallux valgus. Clin Orthop. 1979;142:44–47. [PubMed] [Google Scholar]
- 10.Scranton PE, Jr, Zuckerman JD. Bunion surgery in adolescents: results of surgical treatment. J Pediat Orthop. 1984;4:39–43. doi: 10.1097/01241398-198401000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Trnka H-J, Mühlbauer M, Zembsch A, Hungerford M, Ritschl P, Salzer M. Basal closing wedge osteotomy for correction of hallux valgus and metatarsus primus varus: 10- to 22-year follow-up. Foot Ankle. 1999;20(3):171–177. doi: 10.1177/107110079902000306. [DOI] [PubMed] [Google Scholar]
- 12.Jones S, Al Hussainy HA, Ali F, Betts RP, Flowers MJ. Scarf osteotomy for hallux valgus. J Bone Joint Surg. 2004;86B:830–836. doi: 10.1302/0301-620X.86B6.15000. [DOI] [PubMed] [Google Scholar]
- 13.Crevoisier X, Mouhsine E, Ortolano V, Udin B, Dutoit M. The scarf osteotomy for the treatment of hallux valgus deformity: a review of 84 cases. Foot Ankle Int. 2001;22(12):970–976. doi: 10.1177/107110070102201208. [DOI] [PubMed] [Google Scholar]
- 14.Coetzee JC. Scarf osteotomy for hallux valgus repair: the dark side. Foot Ankle. 2003;24(1):29–33. doi: 10.1177/107110070302400104. [DOI] [PubMed] [Google Scholar]
- 15.Meyer M. Eine neue modification der hallux-valgus-operation. Zen Fur Chir. 1926;53:3265–3268. [Google Scholar]
- 16.Barouk LS. Scarf osteotomy for hallux valgus correction: local anatomy, surgical technique, and combination with other forefoot procedures. Foot Ankle Clin. 2000;5:525–528. [PubMed] [Google Scholar]
- 17.Sammarco GJ, Brainard BJ, Sammarco VJ. Bunion correction using proximal chevron osteotomy. Foot Ankle. 1993;14:8–14. doi: 10.1177/107110079301400102. [DOI] [PubMed] [Google Scholar]
- 18.Lippert FG, III, McDermott JE. Crescentic osteotomy for hallux valgus: a biomechanical study of variables affecting the final position of the first metatarsal. Foot Ankle. 1991;11:204–207. doi: 10.1177/107110079101100403. [DOI] [PubMed] [Google Scholar]
- 19.Piggot H. The natural history of hallux valgus in adolescence and early adults life. J Bone Joint Surg. 1960;42-B(4):749–760. [Google Scholar]
- 20.Coughlin MJ. Hallux valgus. J Bone Joint Surg. 1996;78-A(6):932–966. [PubMed] [Google Scholar]
- 21.Mann RA, Coughlin MJ. Adult hallux valgus. In: Mann RA, Coughlin MJ, editors. Surgery of the Foot and Ankle. 6. St Louis: Mosby-Year Book; 1993. pp. 167–296. [Google Scholar]
- 22.Mann RA (2000) Decision making the hallux valgus surgery. 4th international foot and ankle course, Bad Homburg, Germany
- 23.Coughlin MJ. Rheumatoid forefoot reconstruction. J Bone Joint Surg. 2000;82-A(3):322–340. [PubMed] [Google Scholar]
- 24.Antrobus JN. The primary deformity in hallux valgus and metatarsus primus varus. Clin Orthop. 1984;184:251–255. [PubMed] [Google Scholar]
- 25.Scott G, Wilson DW, Bentley G. Roengenographic assessment in hallux valgus. Clin Orthop. 1991;267:143–147. [PubMed] [Google Scholar]
- 26.Tanaka Y, Takakura Y, Kumai T, Samoto N, Tamal S. Radiographic analysis of hallux valgus. J Bone Joint Surg. 1995;77-A(2):205213. doi: 10.2106/00004623-199502000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Hardy RH, Clapham JCR. Observations on hallux valgus. Based on a controlled series. J Bone Joint Surg. 1951;33-B(3):376–391. doi: 10.1302/0301-620X.33B3.376. [DOI] [PubMed] [Google Scholar]
- 28.Haines RW, McDougall A. The anatomy of hallux valgus. J Bone Joint Surg. 1954;36-B(2):272–293. doi: 10.1302/0301-620X.36B2.272. [DOI] [PubMed] [Google Scholar]
- 29.Perugia D, Basile A, Gensini A, Stopponi M, Simeonibus AU. The scarf osteotomy for severe hallux valgus. Int Orthop. 2003;27(2):103–106. doi: 10.1007/s00264-002-0413-x. [DOI] [PubMed] [Google Scholar]
- 30.Munuera PV, Polo J, Rebollo J. Length of the first metatarsal and hallux in hallux valgus in the initial stage. Int Orthop. 2008;32:489–495. doi: 10.1007/s00264-007-0350-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klaue K, Hansen S, Masquelet A. Clinical, quantitative assessment of first tarsometatarsal mobility in the sagittal plane and its relation to hallux valgus deformity. Foot Ankle Int. 1994;15:9–13. doi: 10.1177/107110079401500103. [DOI] [PubMed] [Google Scholar]
- 32.Faber F, Faber M, Kleinrensink G, Verhoog M. Mobility of the first tarsometatarsal joint in relation to hallux valgus deformity: Anatomical and biomechanical aspects. Foot Ankle Int. 1999;20:651–656. doi: 10.1177/107110079902001007. [DOI] [PubMed] [Google Scholar]
- 33.Coughlin MJ, Carroll JP, Ramon V, Pau G, Brett GR. Hallux valgus and first ray mobility: A cadaveric study. Foot Ankle Int. 2004;25:537–544. doi: 10.1177/107110070402500805. [DOI] [PubMed] [Google Scholar]
- 34.Faber FW, Mulder PG, Verhaar JA. Role of the first ray hypermobility in the outcome of the Hohmann and the Lapidus procedure. J Bone Joint Surg. 2004;86-A(3):486–495. doi: 10.2106/00004623-200403000-00005. [DOI] [PubMed] [Google Scholar]
- 35.Lapidus P. The author’s bunion operation from 1931 to 1959. Clin Orthop. 1960;16:119–135. [PubMed] [Google Scholar]
- 36.Zettl R, Trnka H-J, Easley M, Salzer M, Ritschl P. Moderate to severe hallux valgus deformity: correction with proximal crescentic osteotomy and distal soft-tissue release. Arch Orthop Trauma Surg. 2000;120:397–402. doi: 10.1007/PL00013769. [DOI] [PubMed] [Google Scholar]
- 37.Smith AM, Alwan T, Davies MS. Perioperative complications of the Scarf osteotomy. Foot Ankle Int. 2003;24(3):222–227. doi: 10.1177/107110070302400304. [DOI] [PubMed] [Google Scholar]