Abstract
This study reports the results of the clinical use of a new tourniquet system for surgery of foot and ankle that can determine tourniquet pressure in synchrony with systolic blood pressure (SBP). We prospectively applied additional pressure of 100 mmHg based on the SBP recorded before the skin incision in 100 consecutive procedures. There were 34 open reduction internal fixation procedures, 26 lateral colateral ligament repair or reconstruction, 16 Achilles tendon repairs, nine arthroscopic procedures such as removal of loose body or accessory bone and synovectomy, seven corrective osteotomy and eight others such as removal of tumour, ankle fusion, and bone graft. The average initial tourniquet pressure was 211 mmHg. The average maximum SBP change during surgery was 28 mmHg. All cases maintained an excellent operative field without measurable bleeding and there were no postoperative complications. Fifty-five cases had a lower intra-operative SBP than the initial value. Since a tourniquet should be applied at the lowest pressure possible for maintaining a bloodless surgical field, the new system appears to be practical and reasonable, as compared to conventional tourniquets, which maintain the initial pressure.
Introduction
The use of tourniquet in foot and ankle surgery has been controversial [5, 6, 12]. Advantages have been noted in terms of postoperative pain, swelling, rehabilitation, etc. without the use of tourniquets. Nevertheless, a pneumatic tourniquet is commonly used in foot and ankle surgery [15, 17] to provide a clean, dry operative field, which improves visualisation of anatomical structures and reduces operating time. Great effort has been invested in reducing the required tourniquet pressure [2, 3, 8–11, 13, 16, 18] to eliminate complications attributable to the high inflation pressures associated with pneumatic tourniquets. Some reports have outlined the advances in tourniquet design [2, 3, 9–11, 13, 16, 18], which include increased width and number of cuffs [16, 18], to increase tourniquet pressure until the arterial pulsations in the finger or toe of the operated limb disappear on an oscilloscope or plethysmographic system. These studies have used the conventional tourniquet system that remains at the initial setting pressure. However, blood pressure is not always constant and can vary with conditions, and these tourniquets can not respond to blood pressure changes; any necessary adjustments have to be made manually. This study reports the results of the clinical use of a new tourniquet system for foot and ankle surgery that can determine tourniquet pressure in synchrony with systolic blood pressure to maintain a bloodless surgical field.
Patients and methods
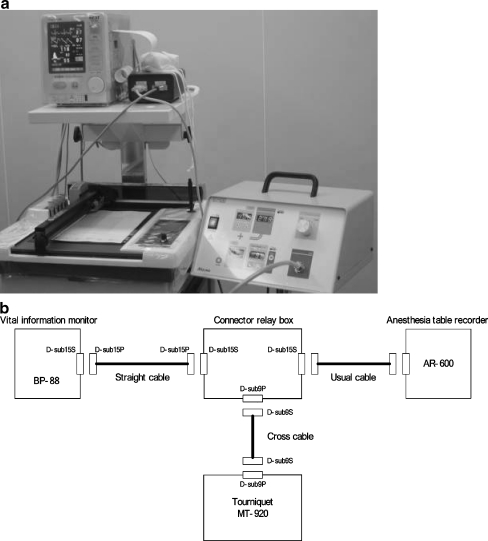
We used a new tourniquet system in which the pressure is synchronised to 0–300 mmHg above systolic blood pressure (SBP), using a vital information monitor. In clinical practice, the level of additional pressure is determined as deemed appropriate by the surgeon. In our study, we applied 100 mmHg as the additional pressure. We routinely used an MT-920 tourniquet system (Mizuho-Ika, Tokyo, Japan) (Fig. 1a, b). The tourniquet was inflated to the desired pressure based on the SBP recorded before the skin incision. The limb was prepared and exsanguinated by elevation and an Esmarch bandage. After surgery began, the tourniquet pressure was automatically synchronised with the SBP. The actual pressure produced with this system is within 10 mmHg of the displayed pressure. The interval of the measurement of blood pressure was every 2.5 minutes in both groups. The tourniquet cuff was 86 cm long and 10.5 cm wide in both groups. A single layer of cast padding was applied between the skin and cuff. The same surgical team performed all of the operations, in a laminar-flow operating room.
Fig. 1.
a. The MT-920 tourniquet system (Mizuho-Ika, Tokyo, Japan) (right) and the vital information monitor (left). b Scheme of the MT-920 tourniquet system (Mizuho-Ika, Tokyo, Japan). The blood pressure of a patient is monitored by the living body information monitor BP-88. The monitor adopts a simple arm cuff since this system is a cuff sphygmomanometer. The information is recorded by the anaesthesia notation record device AR-600 since it can be transmitted as a digital (RS232C) signal. In the MT-920 system, the monitored systolic blood pressure is used. The MT-920 system acquires the information with a CRB (a connector broadcast box). The timing and frequency of the measurement are controlled by the BP-88. The data are always updated when each measurement is finished. Since the MT-920 system constantly reads data, it operates in real-time with a change in the blood pressure
For this study, 100 patients, aged 12–81 years (average age 36 years), were recruited. None had any neurovascular disease. All patients were scheduled to have foot and ankle procedures performed by one senior author (H.N.), using a thigh tourniquet and either general (80) or spinal (20) anaesthesia (Table 1). The procedures included 34 open reduction internal fixation, 26 lateral colateral ligament repair or reconstruction, 16 Achilles tendon repairs, nine arthroscopic procedures such as removal of loose body or accessory bone and synovectomy, seven corrective osteotomies and eight others such as removal of tumour, ankle fusion, and bone graft, etc. All of the patients signed a consent form that included a description of the protocol and the potential tourniquet-related complications.
Table 1.
Patients demographics
| Parameter | Value (mean ± standard deviation) |
|---|---|
| Age (y) | 36 ± 19 |
| Gender (male:female) | 58:42 |
| Weight (kg) | 60 ± 10 |
| Height (cm) | 163 ± 9 |
| BMI | 22.5 ± 2.6 |
| Tourniquet time (minutes) | 48 ± 26 |
| Operation time (minutes) | 46 ± 27 |
BMI body mass index
The surgeon rated the quality of the bloodless field as poor, fair, good, or excellent, and noted any changes in the quality of the bloodless field throughout the procedure. A poor field was one in which blood obscured the view; a fair field had blood present but not significantly interfering with surgery; a good field had some blood with no interference with the procedure; and an excellent field had no blood present.
Results
The average duration of the operation and tourniquet use was 46 (range, 10–150) and 48 (range, 12–155) minutes, respectively. The average initial blood pressure was 111 mmHg (range, 80–189) systolic and 58 mmHg (range, 30–110) diastolic. Fifty-five out of 100 cases showed lower systolic blood pressure during surgery than at pre-surgery. The average maximum pressure change during surgery was 28 mmHg (range, 5–78) systolic and 18 mmHg (range, 3–60) diastolic (Table 2). Seventeen cases displayed the changes in systolic pressure over 40 mmHg during surgery (Table 3). Additionally, the average maximum systolic pressure change during a 2.5-minute interval was 14 mmHg (range, 0–33). No cases exhibited a sharp rise (over 40 mmHg) in this study during a 2.5-minute interval (Table 4). An excellent bloodless surgical field was obtained in almost all patients.
Table 2.
Tourniquet conditions in this study
| Patients (N = 100) | Value (mean ± SD) |
|---|---|
| Initial TP | 211 ± 18 mmHg |
| Maximum change in systolic BP during surgery | 28 ± 13 mmHg |
| Maximum change in diastolic BP during surgery | 18 ± 10 mmHg |
| Maximum TP through surgery | 233 ± 18 mmHg |
| Maximum change in systolic BP in each measurement (2.5 minutes) | 14 ± 7 mmHg |
TP tourniquet pressure, BP blood pressure, SD standard deviation
Table 3.
Distribution of maximum change of systolic blood pressure during surgery
| Pressure (mmHg) | Cases |
|---|---|
| 0–10 | 5 |
| 11–20 | 28 |
| 21–30 | 29 |
| 31–40 | 21 |
| 41–50 | 12 |
| 51–60 | 2 |
| 61–70 | 1 |
| 71–80 | 2 |
| Total | 100 |
Table 4.
Distribution of maximum change (increase) of systolic blood pressure during a 2.5-minute interval
| Pressure (mmHg) | Cases |
|---|---|
| 0–5 | 11 |
| 6–10 | 23 |
| 11–15 | 34 |
| 16–20 | 14 |
| 21–25 | 11 |
| 26–30 | 6 |
| 30–35 | 1 |
| Total | 100 |
Complications
No complications associated with this system, such as compartment syndrome, deep vein complications, skin troubles, paresis, or nerve complications, etc. arose either during or after surgery.
Discussion
The effect of tourniquet use in foot and ankle surgery has been controversial [5, 6, 12]. Omeroglu et al. [12] reported a relationship between the use of tourniquet and the intensity of postoperative pain in surgically treated malleolar fractures. They recommended no tourniquet for male patients and patients older than 30 years. Maffulli et al. [6] reported that a higher prevalence of postoperative complications and a longer time to recovery for the patients operated on using a tourniquet. They did not recommend using a tourniquet in the operative treatment of simple, isolated fibular fractures. Furthermore, recently, Konrad et al. [5] recommended not using a tourniquet for osteosynthesis of ankle fractures, following a comparison of the clinical results (postoperative swelling and pain, ankle range of motion) with (26 cases) and without (28 cases) a thigh tourniquet. Nevertheless, a pneumatic tourniquet is commonly used in foot and ankle surgery according to the recent survey of tourniquet use in orthopaedic foot and ankle surgeons [15, 17] to provide a clean, dry operative field, which improves visualisation of anatomical structures and reduce operation time.
Ideally, the tourniquet should be applied at the lowest pressure and for the shortest amount of time possible. Ishii and Matsuda [3] reported that the mean tourniquet pressure in the 100-mmHg above SBP group was 238 mmHg (range, 220–260) and was statistically indistinguishable from the group in which pressure was fixed at 350 mmHg to reduce postoperative pain and provide a bloodless operative field during cementless total knee arthroplasty. This pressure is very close to the 231 mmHg reported by Reid et al. [14], who found that this pressure provided adequate control of haemostasis in the lower extremities in 97.5 % of cases using a Doppler stethoscope. Tejwani et al. [15] stated that the minimum effective tourniquet pressure is 90–100 mmHg above systolic BP when applied at the thigh, and in a normotensive, nonobese, patient, pressure of 250 mmHg is sufficient. Based on these studies and the excellent results of the our study, we recommend the application tourniquet pressure at 100 mmHg above SBP at the thigh, rather than the conventional commonly used 300–350 mmHg reported by a couple of surveys [15, 17], to provide a sufficiently bloodless operative field and minimise potential complications in surgery of the foot and ankle.
The inflation of the tourniquet to a pressure based on the SBP recorded before the skin incision might allow blood to ooze into the operative field as the SBP gradually or sharply rises. Younger et al. [18] reported a poor bloodless field after a sharp rise (44 and 56 mmHg) in blood pressure during surgery using a new automated plethysmographic limb occlusion pressure measurement technique. They stressed the necessity of good anaesthetic technique rather than the efficacy of this system. However, it is nearly impossible that a patient’s blood pressure remain constant, but rather varies with their conditions. In our study, although 17 cases exhibited over 40 mmHg maximum change of systolic blood pressure during operation, the system could respond automatically to increasing changes in systolic blood pressure. However, the new system experienced no cases with a sharp rise (over 40 mmHg during 2.5-minute interval) in this series, five knees out of 36 cases in total knee arthroplasty exhibited excellent surgical field using this tourniquet in spite of a sharp rise [4]. Additionally, 55 out of 100 procedures showed lower systolic blood pressure during surgery than initial pressure in our study. It could also respond automatically to decreasing changes in systolic blood pressure. Since the new tourniquet synchronised with SBP, it needed less pressure than the conventional method. The new tourniquet can maintain a sufficiently bloodless operative field while minimising potential complications even at the lower tourniquet pressure. Thus, the new tourniquet system that maintains synchrony with SBP appears to be reasonable and safe for use in foot and ankle procedures because of the flexible accommodation to various changes of SBP.
This study has some limitations. Although we adopted a tourniquet pressure of 100 mmHg above SBP in all cases, we should consider the thigh girth to determine the optimal minimal pressure for each patient. For example, patients with thick fat or muscle layers may need an additional pressure greater than 100 mmHg, whereas slender patients may require lower pressures. In addition, we used a standard 10.5-mm-wide cylinder cuff and not a wide contoured (curved) cuff. If the latter cuff design were adopted, less additional pressure to maintain a bloodless surgical field might be needed as Younger et al. [18] reported. Furthermore, we might reduce the tourniquet pressure if this system were applied at calf or ankle. Massey et al. [7] reported mean arterial occlusion pressure of 161.7 mmHg by a pneumatic ankle tourniquet from 50 normotensive healthy subjects. This is approximately 50 mmHg lower than our results. We are currently undertaking new studies to keep the tourniquet pressure as low as possible using this design system.
In conclusion, this new tourniquet system that synchronises with SBP is a reasonable device for maintaining a bloodless surgical field in foot and ankle operations. Although some studies have shown advantages in not using a tourniquet in foot and ankle surgery [5, 6, 12], it seems likely that, for reasons of convenience and long-established practice, the general use of tourniquets will continue. Although the incidence of complications of tourniquet use is very rare (5 complications in 3,027 operations on the foot and/or ankle in a report from the United States [1]), surgeons should choose a more practical tourniquet such as this in foot and ankle surgery.
References
- 1.Derner R, Buckholts J. Surgical hemostasis by pneumatic ankle tourniquet during 3027 podiatric operations. J Foot Ankle Surg. 1995;34:236–246. doi: 10.1016/S1067-2516(09)80054-9. [DOI] [PubMed] [Google Scholar]
- 2.Graham B, Breault MJ, McEwen JA, McGraw RW. Occlusion of arterial flow in the extremities at subsystolic pressures through the use of wide tourniquet cuffs. Clin Orthop. 1993;286:257–261. [PubMed] [Google Scholar]
- 3.Ishii Y, Matsuda Y. Effect of tourniquet pressure on perioperative blood loss associated with cementless total knee arthroplasty: a prospective, randomized study. J Arthroplasty. 2005;20:325–330. doi: 10.1016/j.arth.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Ishii Y, Noguchi H, Matsuda Y, Takeda M, Higashihara T. A new tourniquet system that determines pressures in synchrony with systolic blood pressure in total knee arthroplasty. J Arthroplasty. 2008;23:1050–1056. doi: 10.1016/j.arth.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 5.Konrad G, Markmiller M, Lenich A, Mayr E, Rüter A. Tourniquets may increase postoperative swelling and pain after internal fixation of ankle fractures. Clin Orthop. 2005;433:189–194. doi: 10.1097/01.blo.0000151849.37260.0a. [DOI] [PubMed] [Google Scholar]
- 6.Maffulli N, Testa V, Capasso G. Use of a tourniquet in the internal fixation of fractures of the distal part of the fibula: a prospective, randomized trial. J Bone Joint Surg Am. 1993;75:700–703. doi: 10.2106/00004623-199305000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Massey KA, Blakeslee C, Martin W, Pitkow HS. Pneumatic ankle tourniquets: physiological factors related to minimal arterial occlusion pressure. J Foot Ankle Surg. 1999;38:306–307. doi: 10.1016/S1067-2516(99)80067-2. [DOI] [PubMed] [Google Scholar]
- 8.Moore MR, Grafin SR, Hargens AR. Wide tourniquets eliminate blood flow at low inflation pressures. J Hand Surg Am. 1987;12:1006–1011. doi: 10.1016/s0363-5023(87)80098-9. [DOI] [PubMed] [Google Scholar]
- 9.Muirhead A, Newman RJ. A low-pressure tourniquet system for the lower limb. Injury. 1986;17:53–54. doi: 10.1016/0020-1383(86)90020-3. [DOI] [PubMed] [Google Scholar]
- 10.Neimkin RJ, Smith RJ. Double tourniquet with linked mercury manometers for hand surgery. J Hand Surg Am. 1983;8:938–941. doi: 10.1016/s0363-5023(83)80101-4. [DOI] [PubMed] [Google Scholar]
- 11.Newman RJ, Muirhead A. A safe and effective low-pressure tourniquet: a prospective evaluation. J Bone Joint Surg Br. 1986;68:625–628. doi: 10.1302/0301-620X.68B4.3525572. [DOI] [PubMed] [Google Scholar]
- 12.Omeroğlu H, Günel U, Biçimoğlu A, Tabak AY, Uçaner A, Güney O. The relationship between the use of tourniquet and the intensity of postoperative pain in surgically treated malleolar fractures. Foot Ankle Int. 1997;18:798–802. doi: 10.1177/107110079701801208. [DOI] [PubMed] [Google Scholar]
- 13.Pauers RS, Carocci MA. Low pressure pneumatic tourniquets: effectiveness at minimum recommended inflation pressures. J Foot Ankle Surg. 1994;33:605–609. [PubMed] [Google Scholar]
- 14.Reid HS, Camp RA, Jacob WH. Tourniquet hemostasis. A clinical study. Clin Orthop. 1983;177:230–234. [PubMed] [Google Scholar]
- 15.Tejwani NC, Immerman I, Achan P, Egol KA, McLaurin T. Tourniquet cuff pressure: the gulf between science and practice. J Trauma. 2006;61:1415–1418. doi: 10.1097/01.ta.0000226159.84194.34. [DOI] [PubMed] [Google Scholar]
- 16.Tuncali B, Karci A, Bacakoglu AK, Tuncali BE, Ekin A. Controlled hypotension and minimal inflation pressure: a new approach for pneumatic tourniquet application in upper limb surgery. Anesth Analg. 2003;97:1529–1532. doi: 10.1213/01.ANE.0000081660.97731.91. [DOI] [PubMed] [Google Scholar]
- 17.Younger AS, Kalla TP, McEwen JA, Inkpen K. Survey of tourniquet use in orthopaedic foot and ankle surgery. Foot Ankle Int. 2005;26:208–217. doi: 10.1177/107110070502600305. [DOI] [PubMed] [Google Scholar]
- 18.Younger AS, McEwen JA, Inkpen K. Wide countered thigh cuffs and automated limb occlusion measurement allow lower tourniquet pressures. Clin Orthop. 2004;428:286–293. doi: 10.1097/01.blo.0000142625.82654.b3. [DOI] [PubMed] [Google Scholar]