Abstract
Forearm fractures represent one of the most common fractures in children aside from clavicle fractures, and the distal radius is the most common fracture site accounting for 20–30% of these fractures. Maintaining acceptable reduction is not always possible, and re-displacement or re-angulation is the most commonly reported complication. Factors leading to this complication can be broadly divided into three groups: fracture-, surgeon- and patient-related. The quality of casting has been historically measured subjectively. The description of several casting indices by different authors has been a major undertaking, attempting to address objective assessment of this factor. The following have been described: cast index, padding index, gap index, three point index and second metacarpal-radius angle. For distal radius fractures we think that the three point index is the most valuable measurement for predicting re-displacement among surgeon related factors; this index has not been used in forearm fractures in which the rest of the indices seem to be useful in predicting re-displacement. The casting indices should not be interpreted as a separate issue but in conjunction with fracture characteristics and patient factors.
Introduction
Forearm fractures represent one of the most common fractures in children aside from clavicle fractures [1–3], and the distal radius is the most common fracture site accounting for 20–30% of these fractures [4–8]. Metaphyseal fractures are more common than fractures of the diaphysis, followed by epiphyseal fractures [4, 9].
Eighty-one percent occur in children who are older than five years, with a peak incidence of distal forearm fractures occurring between ages 12–14 in boys and 10–12 in girls. The usual mechanism of injury is a direct fall in or around the house [3, 4].
Historically, most of these fractures in children have been treated by a good closed anatomical reduction [10] and immobilisation in a cast [3]. Conservative methods still play a major role in treatment [6] and 85% of these patients achieved satisfactory results with these methods [3].
Fracture healing is quick, and the fractures have an excellent capacity to spontaneously correct residual axial deformities during the growing years [1, 4]; nevertheless, several studies have shown that complete remodelling does not always occur, this is especially true in children who are older than eight to ten years [3].
Maintaining acceptable reduction is not always possible and re-displacement or re-angulation during cast treatment may occur; this is the most commonly reported complication in paediatric forearm fractures [2, 11–13]. Very high rates of unacceptable degrees of displacement after the initial fracture reduction have been reported. Some recent reports have indicated an increased trend for the routine use of percutaneous pin fixation for the initial treatment of high-risk fractures [6, 14, 15].
In this review article, we discuss risk factors and re-displacement, as well as the role of previously defined radiographic indices in predicting re-displacement of forearm and distal radius fractures in children treated with a plaster cast.
Risk factors
Loss of fracture reduction is the most commonly reported complication of manipulated distal forearm fractures; although earlier published series have reported loss of reduction rates between 10% and 91% of cases; in general, up to one third of cases will demonstrate late displacement [7]. Exact and repeated radiological checks are necessary [16] because early identification allows additional treatment, which will prevent further complications [7].
Factors leading to this complication can be broadly divided into three groups:
Fracture-related factors: Initial displacement, location of the fracture, distance from the physis, isolated distal radius fracture, associated ulna fracture at the same level, obliquity of the fracture [6, 7, 12]
Surgeon-related factors: Inadequate initial closed reduction, poor casting technique [6, 7]
Patient-related factors: Muscle atrophy, resolution of initial soft tissue swelling while in cast
Several studies have concentrated on the fracture/surgeon-related factors. Proctor et al. [10] identified two factors as the more important ones: an initial complete displacement and failure to achieve a perfect reduction. Haddad and Williams [11] reported that a perfect anatomical reduction was the most important favourable prognostic factor. Zamzam and Khoshhal [1] found that the initial displacement of the fracture was the most significant factor affecting outcome. Recently, Alemdaroglu et al. [6] introduced a new factor; they found that complete initial displacement of the fracture and increased obliquity of the fracture line were the most important risk factors for re-displacement.
However, we think that this complication is multi-factorial and all components should be taken into account. Fracture-related factors have been shown to be of great importance in the genesis of this problem, even though surgeon-related factors also play an important role.
The majority of factors mentioned above can be assessed through objective parameters; however, the quality of casting has been historically measured subjectively.
There has been a major effort in this field by different authors to describe several casting indices in order to address objective assessment of this factor. This is important because it can facilitate comparisons between these factors in future studies.
Acceptable reduction/re-displacement
To understand better the utility of these indices we must have clarity when talking about acceptable reduction/re-displacement. There are different parameters used to define this condition and they vary between authors.
Bae et al. [7] defined distal radius fractures as “acceptable” in a bayonet apposition; specifically, in the sagittal plane up to 30° if more than five years of growth is remaining and 5° less for each year less than five, and in the frontal plane 10–15° if more than five years of growth is remaining. Flynn defined forearm fractures as “acceptable” at up to 10–20° angulation in children less than ten years old and no more than 10° angulation in those above ten years old and 30° malrotation. Noonan and Price [17] defined two groups of patients: under nine years old in which a complete displacement and 15° of angulation was accepted and over nine years old in which no more than 10° of angulation was accepted, and for distal radius fractures a complete bayonet apposition with no more than 20° and two years of growth remaining were accepted.
As a general rule, the more proximal to the physis the fracture is, the better the prognosis will be.
We believe that, of the parameters mentioned above we need to have in mind the age of the patient, the remaining years of growth and the proximity to the physis of the fracture involved in order to make the final decision.
Casting indices
To achieve a high quality casting (decreasing surgeon related factors), an adequate reduction is required as well as a good plaster application technique.
Obtaining the first point is possible if an appropriate technique is used; reduction manoeuvres must first exaggerate or recreate the deformity to relax the intact periosteum before longitudinal traction is applied [7].
The second point is obtained by application of a well-moulded cast with three-point bending or appropriate interosseous mould; this is critical in maintaining reduction and minimising the risk of subsequent late displacement [7] within an adequate immobilisation time of usually six weeks [17].
The casting indices are based on formulas that use different measurements done in both frontal and sagittal views, to enable identification of the quality of plaster application.
The first defined radiographic indices were based on measurements only at the fracture site without regard to the proximal and distal points of cast fixation [6].
The cast index was proposed by Chess et al. [6, 13] and is calculated on the basis of the cast geometry at the fracture site, such that:
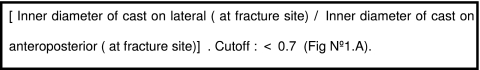
See Fig. 1a.
Fig. 1.
Radiographic indices used to assess quality of cast application following closed reduction. a Cast index: X/Y. b Gap index:  . c Three point index:
. c Three point index: 
(Reprinted from [7] with permission from Elsevier)
The Padding index and Canterbury index were designed by Bathia and Housden [6, 12] to help in the assessment of the cast technique for treatment of both diaphyseal and distal metaphyseal forearm fractures in children.
To calculate the Padding index:
To calculate the Canterbury index:
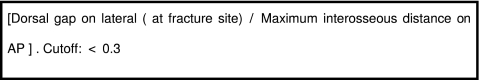
The Gap index is a recently defined radiographic measurement by Malviya et al. [18] based on ratios of the gaps in the cast at the level of the fracture to the entire inside width of the cast in two planes such that:
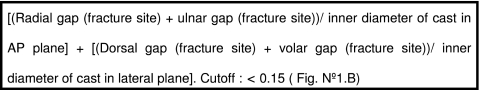
See Fig. 1b.
The three point index was recently defined by Alemdaroglu et al. [6] and differs from the other indices because it not only takes into account the gaps at the fracture site, it also uses the gaps proximal and distal to the fracture sites, which are important points to maintain reduction against common displacement forces [6]. It is determined by:
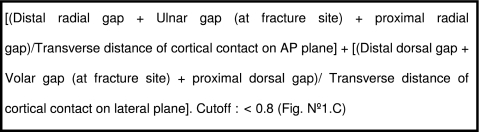
See Fig. 1c.
We think that it is important to mention another measurement that is not a formal casting index but is related to an appropriate fracture reduction and has been recently described by Edmonds et al. [19], namely, the second metacarpal-radius angle. This is the angle between the second metacarpal and the long axis of the radius in the anterioposterior (AP) plane and represents the deviation (radial/ulnar) of a moulded cast. They reported an ideal outcome in up to 86.7% of patients with angles >0° (ulnar moulded); this is important for most dorsally displaced fractures [19].
What’s in the literature?
Although, several studies have been done in recent years, overall the literature is sparse. Initial articles focussed on fracture/surgeon related factors of re-displacement [1, 10, 11]. A high quality cast application in children’s forearm and distal radius fractures has always been a goal; however, an objective assessment was not directly done until Chess et al. [13] defined the “cast index”. After this, other “casting indices” appeared with the aim to provide the best measurement for this issue (Table 1).
Table 1.
Summary of findings from the study articles retrieved and reviewed
| Author | Journal | Year | Indices | Patients | Results | Conclusion |
|---|---|---|---|---|---|---|
| Edmonds et al. | J Child Orthop | 2009 | Second metacarpal-radius angle/cast index | 253 children with distal third forearm fractures | Success of reduction (determined by angle) significant predictor of treatment success (OR:1.6; p < 0.001) No association between treatment “failure” and cast index |
Emphasise the importance of the ulnar deviation mould as measured by the second metacarpal-radius angle |
| Alemdaroglu et al. | J Bone Joint Surg Am | 2008 | Cast index Padding index Canterbury index Gap index Three point index |
75 bicortical displaced distal radius fractures in 74 patients <15 years old | Three point index superior to other indices | Three point index should be used to predict re-displacement and assess the quality of casting |
| S:94.7%; E:95.2%; NPV:98.4%; PPV:85.7% | ||||||
| Singh et al. | Acta Orthop | 2008 | Cast index Padding index |
Five randomly selected cases—20 consultants and 20 registrars-prediction of re-displacement | The accuracy of predicting re-displacement was increased in consultants from 33% to 72% and in registrars from 28% to 81%; P<0.05 | These indices are simple, reliable and reproducible and can be used in clinics and wards to predict re-displacement |
| Malviya et al. | J Pediatr Orthop B | 2007 | Gap index Cast index |
20 cases vs 80 controls, distal third radius fractures | The gap index was more sensitive than the cast index in predicting failure; p < 0.001. RR:6.8 (cast index);RR:35 (gap index) |
The gap index is a better predictor of failure than the cast index |
| Webb et al. | J Bone Joint Surg | 2006 | Cast index | 113 children >4 years old in short vs. long-arm cast (distal forearm fractures) | Cast index >0.7 greater risk for loss of fracture reduction | A well moulded cast in a short-arm cast is as effective as a long-arm cast in treatment of these fractures |
| Bathia et al. | Injury | 2006 | Cast index Padding index Canterbury index |
142 children w/ displaced fracture of forearm or wrist | Cast index, padding index and Canterbury index were greater in the re-displacement group p < 0.005. Improvement in plaster application monitored by these indices reduced re-displacement by 50% |
High cast index, padding index and Canterbury index are important risk factors for re-displacement |
| Chess et al. | J Pediatr Orthop | 1994 | Cast index | 761 distal third forearm fractures | Average angulation change was 4.5°. If change >5° it was a high cast index, p < 0.01 | Excellent results are obtained in all distal pediatric forearm fractures if proper cast moulding is used |
The first indices used were the cast index and the padding index. Chess et al. [13] conducted a study in which all distal one third fractures requiring reduction were included if the distal radial physis was open, a short-arm cast was used and prereduction, postreduction and three week follow-up radiographs were available for review. Subsequently, up to 761 cases were included; however, only 558 cases were left for analysis. They included pronation-flexion and supination-extension injuries. Cast index values averaged 0.72 and the change in angulation was less than 5° in 90% of cases. For all supination-extension injuries, re-angulation was related to poor cast moulding, reflected by a high cast index (p < 0.01). In this study the cast index was applied to distal forearm fractures and the re-displacement in supination–extension type injuries were most related to an abnormal cast index value.
Webb et al. [20] included a total of 113 cases of distal third forearm fractures, which were randomised to be treated with either a short- or long-arm cast. Also, the cast index was measured. The follow-up was done according to the standard protocol of his institution. Between both groups there was no significant difference in terms of cast index; however, the group of long-arm cast patients who lost reduction showed a high cast index (p = 0.001). Also in this study, distal third forearm fractures were included and there was a significant relationship between cast index and loss of reduction.
Bathia et al. [12] conducted a retrospective/prospective study in which the review of case records and radiographs of forearm and distal radius/ulna fractures were included. He described the padding index/Canterbury index. A total of 142 cases were left which included 49 distal radius fractures, 41 distal radius + ulna fractures, and 52 shaft radius + ulna fractures. Re-displacement was observed in 32% of cases. When the non-displacement/displacement groups were compared, all three indexes measured were significantly higher in the displaced group. In this study distal radius fractures were included for the first time and even though all indices were higher in the group that showed displacement, there was no subgroup analysis, meaning that the forearm fractures were not differentiated from the distal radius fractures, thus acting as a possible confounder.
Malviya et al. [18] defined the gap index. They conducted a study which compared the gap index and the cast index; there were 20 cases and 80 controls, all patients sustained a distal third radius fracture. A significant difference (p < 0.001) was observed in the cast index and the gap index of both groups. The gap index was more sensitive than the cast index in predicting failure. At a level of cast index >0.8 the relative risk of failure was 6.8 as compared with 35 with a gap index >0.15. In this study distal third forearm fractures were also studied and both indices showed an association with risk of re-displacement; however, it seems that the gap index is a better predictor.
Singh et al. [21] assessed the reliability and practicality of the cast and padding index in plaster quality application for clinical decision making in forearm fractures. There were five randomly selected cases and 40 orthopaedic surgeons who were asked to predict the risk of re-displacement. After being taught these indices, the surgeons were requested to evaluate. All showed an increase in the number of correct responses—the consultants from 33% to 72% and the registrars from 28% to 81%. This is an interesting study because it attempted to reflect daily work and showed a practical method of applying the indices. All selected cases were forearm fractures and no distal radius fractures were included. It showed the utility of both indices.
Alemdaroglu et al. [6] introduced a new index which was designed according to the basic principles of cast treatment: three-point fixation and reduction accuracy. This study was specific for distal radius fractures and 74 patients were included presenting 75 bi-cortical displaced or severely angulated fractures. All indices were included. The three point index had the highest sensitivity, specificity, positive predictor value and negative predictor value. This is the first study in which all indices were compared in a specific type of fracture; besides the three point index, the gap index was found to be more promising than the other indices but its clinical application is still discouraging.
Edmonds et al. [19] recently defined a measurement on AP view that guides the reduction in that plane. It is important because the remodelling process in that plane is less effective. It was defined as the angle between the second metacarpal and the long axis of the radius. The cast index was also measured and 253 distal third forearm fractures were included. The mould seen on the AP view as determined by the second metacarpal-radius angle was a reproducible radiographic predictor of treatment success. The outcome was considered ideal in 86.7% of cases if moulded with ulnar deviation (angle >0°). There was no association between the treatment “failure” and cast index.
It is clear that there are not many studies about this topic and there is no homogeneity among them. For distal radius fractures we think that the three point index is the most valuable measurement among surgeon related factors for predicting re-displacement as demonstrated by Alemdaroglu et al. [6]. It contributes to the understanding of the intrinsic and extrinsic dynamics of stability of these fractures; however, we also think that more studies are needed to confirm this. This index has not been used in forearm fractures in which the rest of the indices seemed to be useful in predicting re-displacement even though more control trials are needed.
Conclusion
This is a very complex subject to be explained by a single factor; thus, we conclude that it is a multifactorial issue and should be considered on this basis. Complete initial displacement of the fracture, anatomical reduction and obliquity of the fracture line seem to be the most important risk factors for re-displacement. The casting indices should not be interpreted as a separate issue but in conjunction with fracture characteristics and patients factors. The three point index seems to be the more promising of all these indices in distal radius fractures; however, its accuracy has not been proven in forearm fractures.
References
- 1.Zamzam MM, Khoshhal KI. Displaced fracture of the distal radius in children: factors responsible for re-displacement after closed reduction. J Bone Joint Surg. 2005;87(6):841–843. doi: 10.1302/0301-620X.87B6.15648. [DOI] [PubMed] [Google Scholar]
- 2.Bochang C, Jie Y, Zhigang W, Weigl D, Bar-On KK. Immobilisation of forearm fractures in children: extended versus flexed elbow. J Bone Joint Surg Br. 2005;87-B:994–996. doi: 10.1302/0301-620X.87B7.15774. [DOI] [PubMed] [Google Scholar]
- 3.Hove LM, Brudvik C. Displaced paediatric fractures of the distal radius. Arch Orthop Trauma Surg. 2008;128:55–60. doi: 10.1007/s00402-007-0473-x. [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez-Merchán EC. Pediatric fractures of the forearm. Clin Orthop Relat Res. 2005;432:65–72. doi: 10.1097/01.blo.0000156480.76450.04. [DOI] [PubMed] [Google Scholar]
- 5.Schmittenbecher PP. State-of-the-art treatment of forearm shaft fractures. Injury. 2005;36:S-A25–S-A34. doi: 10.1016/j.injury.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 6.Alemdaroglu KB, Iltar S, Çimen O, Uysal M. Risk factors in redisplacement of distal radial fractures in children. J Bone Joint Surg. 2008;90:1224–1230. doi: 10.2106/JBJS.G.00624. [DOI] [PubMed] [Google Scholar]
- 7.Bae DS. Pediatric distal radius and forearm fractures. J Hand Surg. 2008;33A:1911–1923. doi: 10.1016/j.jhsa.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 8.Zimmermann R, Gschwenter M, Kralinger F, Arora R, Gabl M, Pechlaner S. Long-term results following pediatric forearm fracture. Arch Orthop Trauma Surg. 2004;124:179–186. doi: 10.1007/s00402-003-0619-4. [DOI] [PubMed] [Google Scholar]
- 9.Boyer BA, Overton B, Schrader W, Riley P, Fleissner P. Position of immobilization for pediatric forearm fractures. J Pediatr Orthop. 2002;22:185–187. doi: 10.1097/00004694-200203000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Proctor MT, Moore DJ, Paterson JMH. Re-displacement after manipulation of distal radial fractures in children. J Bone Joint Surg Br. 1993;75-b:453–454. doi: 10.1302/0301-620X.75B3.8496221. [DOI] [PubMed] [Google Scholar]
- 11.Haddad FS, Williams RL. Forearm fractures in children: avoiding re-displacement. Injury. 1995;26(10):691–692. doi: 10.1016/0020-1383(95)00136-0. [DOI] [PubMed] [Google Scholar]
- 12.Bhatia M, Housden PH. Re-displacement of paediatric forearm fractures: role of plaster molding and padding. Injury Int J Care Injured. 2006;37:259–268. doi: 10.1016/j.injury.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 13.Chess DG, Hyndman JC, Leahey JL, Brown DCS, Sinclair AM. Short arm plaster cast for distal pediatric forearm fractures. J Pediatr Orthop. 1994;14:211–213. doi: 10.1097/01241398-199403000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Celebi I, Muratli HH, Dogan O, Yagmurlu MF, Aksahin E, Bicimoglu A. The results of intramedullary nailing in children who developed re-displacement during cast treatment of both-bone forearm fractures. Acta Orthop Traumatol Turc. 2007;41(3):175–182. [PubMed] [Google Scholar]
- 15.Garg NK, Ballal MS, Malek IA, Webster RA, Bruce CE. Use of elastic stable intramedullary nailing for treating unstable forearm fractures in children. J Trauma. 2008;65:109–115. doi: 10.1097/TA.0b013e3181623309. [DOI] [PubMed] [Google Scholar]
- 16.Reichmann W. Distal radial fracture in childhood. Handchirurgie. 1978;10(4):179–181. [PubMed] [Google Scholar]
- 17.Noonan KJ, Price CT. Forearm and distal radius fractures in children. J Am Acad Orthop Surg. 1998;6(3):146–156. doi: 10.5435/00124635-199805000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Malviya A, Tsintzas D, Mahawar K, Bache CE, Glithero PR. Gap index: a good predictor of failure of plaster cast in distal third radius fractures. J Pediatr Orthop B. 2007;16(1):48–52. doi: 10.1097/01.bpb.0000236232.57269.ec. [DOI] [PubMed] [Google Scholar]
- 19.Edmonds EW, Capelo RM, Stearns P, Bastrom TP, Wallace CD, Newton PO (2009) Predicting initial treatment failure of fiberglass casts in pediatric distal radius fractures: utility of the second metacarpal–radius angle. J Child Orthop 3:375–381 [DOI] [PMC free article] [PubMed]
- 20.Webb GR, Galpin RD, Armstrong DG. Comparison of short and long plaster casts for displaced fractures in the distal third of the forearm in children. J Bone Joint Surg. 2006;88A:9–17. doi: 10.2106/JBJS.E.00131. [DOI] [PubMed] [Google Scholar]
- 21.Singh S, Bhatia M, Housden P. Cast and padding indices used for clinical decision making in forearm fractures in children. Acta Orthop. 2008;79(3):386–389. doi: 10.1080/17453670710015292. [DOI] [PubMed] [Google Scholar]



