Abstract
Recent years have witnessed a paradigm shift in relation to the assessment of outcome in spine surgery: multidimensional patient-centred questionnaires have superseded traditional surgeon-based ratings of outcome, and surgical registries have been developed to capitalise on the principle of “strength in numbers.” However, the assessment of complications has not enjoyed this same enlightened patient-centred approach. The present study investigated post-surgical complications from the patient’s perspective. All German-speaking patients undergoing surgery within our Spine Center in 2005 were asked to complete the patient-orientated Core Measures Outcome Index of the SSE Spine Tango Spine Surgery Registry before and 12 months after surgery; the surgeon completed a Spine Tango surgery form. In the 12-month questionnaire, the patient was asked, “did any complications arise as a consequence of your operation 1 year ago (e.g. problems with wound healing, paralysis, sensory disturbances, etc.)? If so, give details.” Patients were also asked about their satisfaction with the operation and the global outcome of surgery. 1,035 patients were sent a 12-month questionnaire; 972 (94%) returned the completed questionnaire. 29% patients answered “yes” to the question about complications. The incidence of patient-rated complications was significantly associated with outcome/satisfaction (P < 0.05), suggesting these complications were not trivial to the patient. The results indicate that, just like outcome, “complications” should be assessed from both the patient’s and the surgeon’s perspectives, not least to better understand the reasons accounting for dissatisfaction and a poor patient-rated outcome.
Keywords: Spine surgery, Registry, Outcome, Self-assessment, Complications
Introduction
The occurrence of complications in connection with spine surgery is inevitable. The frequency of complications is dependent on the underlying pathology and the complexity of the procedure [1, 2, 10, 20]. Human error, technical failure, anatomical variations, unexpected biological responses, or any combination of these, can lead to unexpected outcomes. In the majority of cases, there are negative consequences for the patient of varying degrees of severity.
Whilst there is general consensus that a certain frequency of complications has to be accepted as an integral part of the therapeutic spectrum, the definition of what constitutes a complication is the subject of ongoing discussion [9]. Attempts to classify complications have been published [11] using various different criteria. The time of occurrence of the complications (preoperative, early, and late postoperative) is commonly used [9], and the incidence of specific parameters such as the accuracy of screw placement [8] or retrograde ejaculation [6] is sometimes reported.
Studies that include in the list of postoperative complications’ minor negative events such as superficial wound healing will have less favourable rates than those that list only “major” complications such as neurological deficits or complications such as haematomas, CSF fistulas, etc. that require re-intervention. General complications (internal medicine, systemic) occurring in the acute postoperative phase are often difficult to attribute directly to the surgery. Even if a deep vein thrombosis or pulmonary embolism would not have occurred without the surgical trauma, it is hardly possible to allocate this type of complication to a specific type of spine surgery. However, they must be classified as postoperative complications and will, in turn, have a major influence on the documented quality of a surgical procedure.
The variety of methodologies for assessing adverse events may be one of the reasons for the wide-ranging complication rates reported in the literature for spine surgery. Indeed, it is otherwise rather difficult to explain the variable incidence of 0–50% of complications for the same procedure in different papers [9]. Another factor to consider is that surgery-related complications are usually assessed and documented only by the medical staff directly involved in the treatment of the patient, and a certain bias cannot be completely excluded. Indeed, one study has shown that neither self-report by surgeons nor reliance on voluntary reports by the spine team conducting daily ward rounds was sufficient for identifying most adverse occurrences [17]. In the latter study, even rigorous daily medical record reviews (from all sources: surgical, medical, anaesthetic, and management lists) failed to document 8% adverse occurrences. It is hence questionable whether current methods of reporting constitute the most (or only) appropriate methodology for solving the problem of failure evaluation.
Notably, the input of the patient is seldom considered in connection with complications. In most other areas of outcome, we have come to realise that, for elective surgical procedures that aim to improve the patient’s quality of life by decreasing pain and disability, the patient is the best judge of success [7]. Applying the same principle to complications arising after surgery, the patient is perhaps also in the best position to deliver information on the occurrence of any new, untoward, and undesirable consequences of their operation, i.e. complications.
The primary intention of the present paper is to analyse the occurrence of complications from the patient’s perspective.
Methods
All German-speaking patients who underwent spine surgery (both lumbar and cervical) in the Spine Center of a specialised orthopaedic hospital during the period January 2005 to December 2005 were included in the study.
The SSE Spine Tango registry was used to assist with documentation of the relevant data. The surgical form enquired about pathology, previous treatment, patient morbidity status, surgeon credentials, surgical procedures applied, and duration of operation. At discharge, the occurrence, time of occurrence, and type of both general and surgical complications were documented. At follow-up visits, further data regarding the outcome, including the occurrence of complications, were registered.
Parallel to these medical data, the patients were requested to complete the Core Measures Outcome Index (COMI) questionnaire [16] both preoperatively and at 12 months following surgery. The questionnaires were sent to the patients to complete at home, to guarantee information free of external (care-provider) influence. The COMI is a multidimensional index consisting of validated questions covering the domains of pain, function, symptom specific well-being, general quality of life, and social and work disability. In addition to these questions answered both before and 12 months after surgery, at the 12-month follow-up, there were three questions enquiring about overall satisfaction with treatment of the back/neck problem in the hospital (five categories from “very satisfied” to “very dissatisfied”), the global outcome of surgery (five categories from “helped a lot” to “made things worse”), and the occurrence and nature of any complications that had arisen. The latter was addressed using the question “did any complications arise as a consequence of your operation 1 year ago (e.g. problems with wound healing, paralysis, sensory disturbances, etc.)? If so, give details.” The patients were hence free to describe, in their own words, any problems that they perceived as being an unwanted consequence of the surgery. Since the patients’ descriptions of complications did not necessarily correspond with those reported in the literature, and were not always worded using conventional medical terms, several categories were established, to which the different complications could then be assigned. Two surgeons independently examined a series of approximately 170 patient-centred complications, totally blind to patient identity, surgeon identity, and any other patient/operation details, and then chose complication categories similar to those used in the SSE Spine Tango surgical registry or created additional ones where needed. The categorisation was cross-checked and confirmed by a third investigator and any discrepancies (approximately 18%) were highlighted for discussion, in order to decide on a single set of categories and a decision rule for future cases. Consensus was reached easily in each case. A scientific assistant was also involved in this whole process, and, after examining the individual descriptions and the rules for assignment, was from thereon in responsible for categorising the complications.
Results
In the year of study, 1,074 patients underwent spine surgery for therapeutic (i.e. non-diagnostic) purposes. Their mean age was 58.2 (SD 17.1) years and there were 562 women and 512 men. An SSE Spine Tango surgery form was completed by the surgeon for 938 (87%) of these cases. Overall 11 spine surgeons contributed data, although 690/1,074 (64%) of the patients were operated on by the three senior consultants/departmental heads (one neurosurgeon and two orthopaedic surgeons) and a further 27%, by more junior consultant spine surgeons.
The distribution of main pathologies is shown in Table 1.
Table 1.
Distribution of main pathologies for patients operated on in 2005 and registered in the Spine Tango system
| Number of patients | Percentage of patients | Main pathology |
|---|---|---|
| 736 | 78.5 | Degenerative disease |
| 56 | 6.0 | Deformity |
| 54 | 5.8 | Spondylolisthesis |
| 29 | 3.1 | Failed surgery |
| 20 | 2.1 | Tumour |
| 17 | 1.8 | Fracture |
| 10 | 1.1 | Inflammation |
| 6 | 0.7 | Other |
| 5 | 0.5 | Pathological fracture |
| 5 | 0.5 | Infection |
| 938 | 100 |
Categories from the SSE Spine Tango surgery form
The level of the surgical procedure was as follows: 16.0% cervical/cervicothoracic, 7.4% thoracic/thoracolumbar/thoraco-lumbo-sacral, 53.7% lumbar, 22.2% lumbosacral, 0.7% sacral/coccygeal.
The rates of surgical and general complications arising during the hospital stay itself, as reported in the SSE Spine Tango system, were 24/938 (2.6%) and 27/938 (2.9%), respectively. The surgical complications comprised nerve root damage (N = 2), cauda equina damage (N = 1), bleeding in spinal canal (N = 5), dura lesion (N = 3), wound infection (N = 2), and other complications (N = 11). The general complications comprised anaesthesiological (N = 1), cardiovascular (N = 7), pulmonary (N = 8), cerebral (N = 2), kidney/urinary (N = 2), liver/GI (N = 2), and other complications (N = 7).
1,035/1,074 (94%) patients were sent a 12-month follow-up questionnaire (39 were not sent a questionnaire for various reasons: too severely handicapped, language problems, express wish of the patient not to participate, young children, died since operation, etc.). Of these, 972 (94%) returned a questionnaire and 968 answered the questionnaire about complications. 285/968 (29%) reported various forms of complications. The incidence of complications varied between the surgeons from 23 to 42% (including only those surgeons that had done ≥ 10 operations).
From the patients’ descriptions, the complications were categorised as shown in Table 2.
Table 2.
Distribution of patient-orientated “complications” reported by the patients at 12-months post-surgery
| Number of patients | Percentage of patients | Complication |
|---|---|---|
| 110 | 38.6 | Sensory (± other complaints) |
| 73 | 25.6 | Pain (± other complaints) |
| 36 | 12.6 | Motor/weakness (± other complaints) |
| 18 | 6.3 | Wound healing |
| 14 | 4.9 | Other |
| 13 | 4.6 | General neurological |
| 4 | 1.4 | Swallowing difficulties |
| 4 | 1.4 | GU |
| 4 | 1.4 | Infection |
| 3 | 1.1 | Implant |
| 2 | 0.7 | Problems at graft site |
| 2 | 0.7 | Internal medicine |
| 1 | 0.4 | Instability |
| 1 | 0.4 | Psychological problems |
| 285 | 100 |
N = 285/968 reported a complication
There was no statistically significant difference between the sexes in the proportion of patient-centred complications (men 30.0%, women 27.0%; P = 0.31). Similarly, the type of health insurance cover did not influence the percent complications reported (private 30.0%, semi-private 28.0%, basic obligatory 27.9%; P = 0.82). There was a difference, however, in relation to the number of previous surgeries: those undergoing first-time ever spinal surgery 24.3%, first-time surgery at the given level 32.7%, repeat surgery at the given level 35.8% (P = 0.004). The incidence of patient-centred complications varied somewhat for the different main pathologies listed in Table 1, ranging from (for those with more than 20 patients in the category) 23.0% for spondylolisthesis to 38.5% for failed surgery.
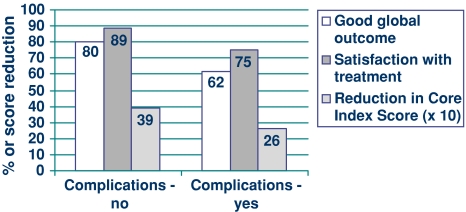
The incidence of patient-rated “complications” was significantly associated with global outcome and satisfaction (Fig. 1): a “good” global outcome (operation helped or helped a lot) was found in 79.8% of patients who had no such complications but only 62.4% of those with complications (P = 0.0001); the corresponding figures for “satisfaction with treatment received” were 89.1% (if no patient-rated complications) and 74.6% (complications), respectively (P = 0.0001). There was also a significant difference between the groups for the reduction in multidimensional Core Measures score (0–10 scale) from pre-surgery to 12 months follow-up: a reduction of 3.9 (SD 3.0) points was seen in the “no complications” group compared with 2.6 (SD 2.9) points in the group reporting complications (P = 0.0001).
Fig. 1.
Changes in various other outcome measures for patients with and without patient-orientated complications at 12-month follow-up
Discussion
For obvious reasons, the reporting of successful outcomes is more satisfying than listing complications. Complications are by definition something that should not occur and that generally provoke a search for the guilty agent or person. The personalisation of failure, in relation to the involved medical personnel, and adverse legal consequences [3, 14, 15, 19] prevent a neutral approach to the problem of assessing complications. This may explain the finding that relatively few articles are to be found when searching databases such as Pubmed using the key words “complications” and “spine surgery.” In the majority of surgical papers, if complications are listed at all, there is rarely any detailed information given about their severity, exact nature, and consequences. Instead, the focus of the paper is generally the (positive) surgical outcome of the described procedure, with complications being mentioned in a subordinate paragraph, in the knowledge that “no complications” would raise suspicion of biased reporting. The complications listed are usually directly associated with a specific treatment or technique, such as incidental dural tears in decompressive surgery [5, 13].
In general, complications are assessed and documented by medical professionals. The selection and definition of what constitutes a complication is made by the investigator. Review of the hospital charts after a defined procedure is the methodology most commonly used [5, 12, 18] and, hence, incidents that can be measured or visualised are usually preferred. The accuracy of placement of pedicle screws [8], dural tears [4, 5], and neurological deficit [12] are just a few examples in this category. However, these complications are not necessarily the only ones that concern the patients or influence their satisfaction with treatment/global outcome. For example, incidental durotomy—an objective complication—is without relevant influence on the overall result if treated properly [13], and will not bother the patient. Using a patient questionnaire, Christensen et al. [6] enquired about the development of retrograde ejaculation in patients operated on with an anterior approach to the lumbosacral spine, 6–13 years previously. The authors reported an 8% male genital dysfunction but without negative effect on the general functional status evaluated with the Dallas pain questionnaire. These studies may indicate that the occurrence of a complication does not always compromise the subjective result. However, it is also possible that the instruments currently used for monitoring complications are not appropriate for detecting the type of complications that do have an impact on the overall result.
The scenario is rather reminiscent of the assessment of surgical success, some 30 years ago. Then, the main means of judging outcome was based on the clinician’s own simple rating scale, using categories such as “excellent, good, moderate, and poor”, and viewed predominantly from a surgical or clinical perspective. The technical success of the operation lent itself to evaluation in terms of, e.g., the degree of fusion or extent of decompression achieved, as monitored by appropriate imaging. In an effort to achieve further objectivity, these measures were sometimes supplemented with physiologic measures such as range of motion or muscle strength [7]. However, in many cases, these objective measures proved to be only weakly associated with outcomes of relevance to the patients and to society. As a result of this, recent years have witnessed a paradigm shift in relation to the assessment of outcome in spine surgery: multidimensional patient-centred questionnaires and independent-observer assessments have superseded the traditional surgeon-orientated ratings of success or failure.
In the present study, we made an attempt to assess complications from a patient-orientated approach, allowing them to describe in their own words the new or unexpected problems arising as a result of surgery. At the outset, we hypothesised that, in this domain too, the view of the patient may differ from that of the surgeon, and may be an important determinant of the global patient-rated outcome. And, indeed, our suspicions were confirmed by the almost 30% rate of incidents reported, and the significant correlation between these and the overall outcome and satisfaction with the procedure. As such, we believe that the concept of reporting complications should be revised. A process similar to the shift of paradigm in assessing the clinical results after spine surgery should be adopted for reporting the impact of complications. The “objective” view of complications based on radiographs and clinical findings in hospital charts may be important for improving operative techniques and strategies, but it is only partially relevant in terms of outcome. There is a certain correlation between “objective” complications and the patient’s satisfaction but only if the investigated complication is obvious for the patient and the doctor such as increasing kyphotic deformity [12]; in many other cases, there is no significant relationship [6].
As shown in our study, there is a considerable difference between the patient-rated complication rates and the complication rates typically reported in literature. It seems clear that patients perceive many events occurring after their spine surgery to be complications, and to be worthy of mention when formally enquired about. In theory, one might imagine that the same question would be asked of the patient by the surgeon at clinical follow-ups; however, the rates reported there were <10% up to 1 year postoperative (detailed data not shown). Hence, either these concerns are not being voiced at the clinical follow-up interview or they are being interpreted as too trivial to document by the surgeon. At present, since the patient-centred complications question enquires only about the occurrence of complications, nothing can be said about their severity and/or the long-term impact. This will be investigated in greater detail in our future analyses. We have modified our questionnaire to add a question concerning the bothersomeness of the complications (five categories), based on the pain bothersomeness question reported in Deyo et al [7]. Nonetheless, we should not lose sight of the fact that, even if there are minor negative events without severe consequences, these are still considered as complications from the viewpoint of the patient and may have an impact on the overall outcome.
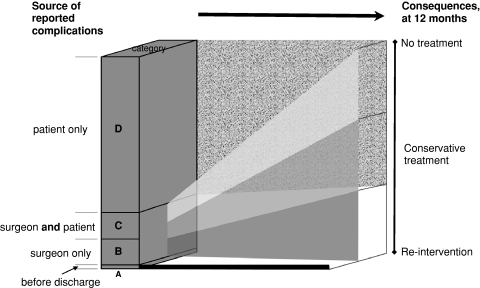
For improved understanding, we propose a different classification system for post-surgical complications. The differentiation can be made between complications perceived by the doctor, the patient or both (Fig. 2). Depending on the severity, different consequences arise. Apart from a minority of severe and obvious pathologies whose medical indications necessitate aggressive treatment, the subjective evaluation by the patient should determine the therapeutic consequences.
Fig. 2.
Source of the reported complications and their consequences after 12 months. (A) Complication arises before discharge and requires re-intervention, but the patient is unaware of a problem (e.g. a screw is too long and carries the risk of erosion of a vessel, or a screw is malpositioned, increasing the risk of instability). These complications carry a risk for the future and must be acted on early. They arise in approximately 1.4% of all operations (and constitute one-third of all the complications reported at discharge). (B) Complication recorded within 12 months by the surgeon but not by the patient may concern something like a screw penetrating the pedicle. This type of complication may or may not lead to an action (often very surgeon-dependent). Occurs in about 4–5% of all patients and comprises approximately half of all the surgeon-rated complications. (C) Complication reported within 12 months by both the patient [= 14% of all patient-reported complications (C/C + D)] and the doctor (= 50% of all surgeon-reported complications (C/C + B) may or may not need treatment. This type arises in 4–5% of all cases. From groups B and C together (i.e. all surgeon-reported complications), about one-third of patients are re-operated, one-third treated conservatively, and one-third not treated at all. (D) Complication reported (up to 12 months) by the patient but not the surgeon. Sometimes treatable and treated conservatively, sometimes not. Such complications are reported by approximately 25% patients
The unexpectedly high rate of complications from the patients’ perspective necessitates a reorientation in assessing the results of surgery. A modification of the assessment criteria to include consideration of the patient’s subjective impression might be an important step forward in understanding the poor results and dissatisfaction in certain areas of spine surgery.
In conclusion, whilst it is conceivable that the concept of a “complication” differs between the patient and the surgeon, the results suggest that, just like outcome, “complications” should be assessed from both the patient’s and the surgeon’s perspective—not least to better understand the reasons accounting for dissatisfaction with surgery and a poor patient-rated outcome.
Acknowledgments
Conflict of interest statement None of the authors has any potential conflict of interest.
References
- 1.Abramovitz JN. Complications of surgery for discogenic disease of the spine. Neurosurg Clin N Am. 1993;4:167–176. [PubMed] [Google Scholar]
- 2.Ahlhelm F, Reith W, Naumann N, Schulte-Altedorneburg G, Papanagiotou P, Kelm J, Nabhan A. Postoperative syndrome after spine surgery. Radiologe. 2006;46:486–494. doi: 10.1007/s00117-006-1386-3. [DOI] [PubMed] [Google Scholar]
- 3.Berlinger N, Wu AW. Subtracting insult from injury: addressing cultural expectations in the disclosure of medical error. J Med Ethics. 2005;31:106–108. doi: 10.1136/jme.2003.005538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bosacco SJ, Gardner MJ, Guille JT (2001) Evaluation and treatment of dural tears in lumbar spine surgery: a review. Clin Orthop Relat Res 238–247. doi:10.1097/00003086-200108000-00033 [DOI] [PubMed]
- 5.Cammisa FP, Jr, Girardi FP, Sangani PK, Parvataneni HK, Cadag S, Sandhu HS. Incidental durotomy in spine surgery. Spine. 2000;25:2663–2667. doi: 10.1097/00007632-200010150-00019. [DOI] [PubMed] [Google Scholar]
- 6.Christensen FB. Lumbar spinal fusion. Outcome in relation to surgical methods, choice of implant and postoperative rehabilitation. Acta Orthop Scand Suppl. 2004;75:2–43. [PubMed] [Google Scholar]
- 7.Deyo RA, Battie M, Beurskens AJHM, Bombardier C, Croft P, Koes B, Malmivaara A, Roland M, Korff M, Waddell G. Outcome measures for low back pain research. A proposal for standardized use. Spine. 1998;23:2003–2013. doi: 10.1097/00007632-199809150-00018. [DOI] [PubMed] [Google Scholar]
- 8.Di Silvestre M, Parisini P, Lolli F, Bakaloudis G. Complications of thoracic pedicle screws in scoliosis treatment. Spine. 2007;32:1655–1661. doi: 10.1097/BRS.0b013e318074d604. [DOI] [PubMed] [Google Scholar]
- 9.Fritzell P, Hagg O, Nordwall A. Complications in lumbar fusion surgery for chronic low back pain: comparison of three surgical techniques used in a prospective randomized study. A report from the Swedish Lumbar Spine Study Group. Eur Spine J. 2003;12:178–189. doi: 10.1007/s00586-002-0493-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gibson JN, Waddell G (2005) Surgery for degenerative lumbar spondylosis. Cochrane Database Syst Rev CD001352 [DOI] [PubMed]
- 11.Grob D. Complications and pitfalls of spinal fusion. In: Spine: state of the art reviews—spinal fusion, vol 6. Philadelphia: Hanley and Belfus; 1992. pp. 615–627. [Google Scholar]
- 12.Ikenaga M, Shikata J, Takemoto M, Tanaka C. Clinical outcomes and complications after pedicle subtraction osteotomy for correction of thoracolumbar kyphosis. J Neurosurg Spine. 2007;6:330–336. doi: 10.3171/spi.2007.6.4.8. [DOI] [PubMed] [Google Scholar]
- 13.Jones AA, Stambough JL, Balderston RA, Rothman RH, Booth RE., Jr Long-term results of lumbar spine surgery complicated by unintended incidental durotomy. Spine. 1989;14:443–446. doi: 10.1097/00007632-198904000-00021. [DOI] [PubMed] [Google Scholar]
- 14.Krizek TJ. Surgical error: ethical issues of adverse events. Arch Surg. 2000;135:1359–1366. doi: 10.1001/archsurg.135.11.1359. [DOI] [PubMed] [Google Scholar]
- 15.Krizek TJ. Surgical error: reflections on adverse events. Bull Am Coll Surg. 2000;85:18–22. [PubMed] [Google Scholar]
- 16.Mannion AF, Elfering A, Staerkle R, Junge A, Grob D, Semmer NK, Jacobshagen N, Dvorak J, Boos N. Outcome assessment in low back pain: how low can you go? Eur Spine J. 2005;14:1014–1026. doi: 10.1007/s00586-005-0911-9. [DOI] [PubMed] [Google Scholar]
- 17.Mirza SK, Deyo RA, Heagerty PJ, Turner JA, Lee LA, Goodkin R. Towards standardized measurement of adverse events in spine surgery: conceptual model and pilot evaluation. BMC Musculoskelet Disord. 2006;7:53. doi: 10.1186/1471-2474-7-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mohamad F, Parent S, Pawelek J, Marks M, Bastrom T, Faro F, Newton P. Perioperative complications after surgical correction in neuromuscular scoliosis. J Pediatr Orthop. 2007;27:392–397. doi: 10.1097/01.bpb.0000271321.10869.98. [DOI] [PubMed] [Google Scholar]
- 19.Wu AW. Medical error: the second victim. The doctor who makes the mistake needs help too. BMJ. 2000;320:726–727. doi: 10.1136/bmj.320.7237.726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Young PM, Berquist TH, Bancroft LW, Peterson JJ. Complications of spinal instrumentation. Radiographics. 2007;27:775–789. doi: 10.1148/rg.273065055. [DOI] [PubMed] [Google Scholar]