Abstract
The role of the patient as an active partner in health care, and not just a passive object of diagnostic testing and medical treatment, is widely accepted. Providing information to patients is considered a crucial issue and the central focus in patient educational activities. It is necessary to educate patients on the nature of the outcomes and the benefits and risks of the procedures to involve them in the decision-making process and enable them to achieve fully informed consent. Information materials must contain scientifically reliable information and be presented in a form that is acceptable and useful to patients. Given the mismatch between public beliefs and current evidence, strategies for changing the public perceptions are required. Traditional patient education programmes have to face the potential barriers of storage, access problems and the need to keep content materials up to date. A computer-based resource provides many advantages, including “just-in-time” availability and a private learning environment. The use of the Internet for patient information needs will continue to expand as Internet access becomes readily available. However, the problem is no longer in finding information, but in assessing the credibility and validity of it. Health Web sites should provide health information that is secure and trustworthy. The large majority of the Web sites providing information related to spinal disorders are of limited and poor quality. Patient Line (PL), a patient information section in the Web site of Eurospine, was born in 2005 to offer patients and the general population the accumulated expertise represented by the members of the society and provide up-to-date information related to spinal disorders. In areas where evidence is scarce, Patient Line provides a real-time opinion of the EuroSpine membership. The published data reflect the pragmatic and the common sense range of treatments offered by the Eurospine membership. The first chapters have been dedicated to sciatica, scoliosis, cervical pain syndromes, low back pain and motion preservation surgery. Since 2008, the information has been available in English, German, French and Spanish. The goal is for Patient Line to become THE European patient information Web site on spinal disorders, providing reliable and updated best practice and evidence-based information where the evidence exists.
Keywords: Spine surgery, Patient information, Patient Line
Introduction
For decades, physicians used to dominate the patient–doctor relationship. They tended to see the process of decision making as the sole responsibility of the doctor. A growing number of publications on patient-centred care, patient participation, patient involvement and shared decision making reflect that these traditional roles of physicians and patients in decision making are changing [22]. Nowadays, the role of the patient as an active partner in health care, and not just a passive object of diagnostic testing and medical treatment, is widely accepted [9]. Patients have become more conscious consumers of health care. They expect to be given more information, and many express a desire to participate in medical decision making. Information and participation needs of patients, combined with a broader awareness in society of the ethics in health care, including respect for patient’s autonomy have become important elements of modern health care [22].
Patient-centred medicine has often been contrasted to a biomedical model of medicine. The biomedical approach does not sit easily with the more inclusive patient involvement and is a model that shows its age in today’s information-hungry society [9]. Providing information to patients is considered a crucial issue [13], yet many patients report considerable difficulties in obtaining relevant information [7]. There are numerous reasons for this. Health professionals frequently underestimate patients’ desire for, and ability to cope with, information. Consultation times are limited. There is often insufficient time to explain fully the condition and the treatment choices [7]. Doctors’ traditional methods may not be adequate for informing some patients. However, patients need to comprehend the options and outcomes in order to consider and communicate the personal values by which they assess the benefits versus potential risk of interventions. In certain areas of medicine, information can be as therapeutic for patients as medications, exercises or surgery. The better educated patients are, the better their treatment outcomes may be because of realistic behavioural modifications and expectations [28].
Patient education: definition, educational interventions and goals
Patient education has been defined as a systematic experience in which a combination or a variety of methods are used. These might include the provision of information and advice and behaviour modification techniques, which influence the way the patient experiences his illness and/or his knowledge and health behaviour, aimed at improving or maintaining or learning to cope with a condition, usually a chronic one [8].
Three types of patient education may be considered: information only, counselling and behavioural treatment [24, 25]. In daily practice, patient education will often be part of a treatment programme and seldom be used as single intervention [8].
Information only includes interventions aimed primarily at the exchange of information, by means of persuasive communication or information brochures [22]. Patients need information to [7]:
understand what is wrong;
gain a realistic idea of prognosis;
make the most of consultations;
understand the processes and likely outcomes of possible tests and treatments;
assist in self-care;
learn about available services and sources of help;
provide reassurance and help to cope;
help others understand;
legitimize seeking help and voicing their concerns;
learn how to prevent further illness;
identify further information and self-help groups;
identify the “best” health-care providers.
Counselling includes interventions mainly aimed at social support and giving patients the opportunity to discuss their health-related problems [24]. The emphasis should be on counselling patients to promote their health to cope better with their illnesses. This involves educating patients to better understand their medical condition or the choice between two treatments. Facilitating communication between patients and health-care providers so as to respond to patients’ concerns, help patients to make informed decisions on treatment and promote their ability to cope with health problems [9]. Behavioural treatment refers to interventions that include techniques aiming at behavioural change, such as behavioural instruction, skills training and biofeedback [24]. An example of this would be cognitive behavioural therapy, an evidenced-based and empirical way of using education to change behaviour.
Providing information is in fact the central focus in educational activities. Such an exchange of information is an essential element of a process of shared decision making between patients and their doctors [22]. It is necessary to educate patients on the nature of the outcomes and the benefits and risks of the procedures to involve them in the decision-making process and enable them to achieve fully informed consent [10]. Educational programmes should give people the strategies and tools necessary to make daily decisions to cope with the disease [24, 25]. Due to poor or outdated information available, patients and the general public hold many misconceptions [10]. Patient’s understanding of his or her health problem may modify treatment success. Fears and beliefs can have a major negative impact on recovery from spinal disorders. There are good grounds for optimism to assume that active involvement in decision making may increase the effectiveness of the treatment. Patients with hypertension benefit if they are allowed to adopt an active rather than a passive role in treatment. Patients with breast cancer suffer less depression and anxiety if they are treated by doctors who adopt a participative consultation style. Patients who are more actively involved in the discussions on the management of their diabetes achieve better sugar control. On the other hand, patients whose doctors are ignorant about their values and preferences may receive treatment that is inappropriate to their needs [7].
Patients often complain about the difficulty of obtaining enough and reliable information [7]. However they may not be receptive to the information communicated to them. Some may not be able to understand or recall given information at a later time even when this has been conveyed explicitly and in great detail [22]. Being able to reproduce information is not the same as understanding and being able to apply new knowledge. It is important to comprehend how the patient is processing the information and translating this understanding into action [18]. On average, patients forget half of what they were told by a doctor within 5 min of leaving the consultation room. In addition, health professionals can easily forget to pass on important information to the patient. There is always scope for improvement in communication between professionals and patients [27]. Contradictory messages coming from a variety of sources, due to a lack of coordination, can add to the uncertainty, which exacerbates anxiety [11]. We should ensure that patients have access to written or audiovisual material to inform themselves and to use in discussion with health professionals.
Patient education may include video, audio, computer-based or printed materials. Even the mass media may play a role in patient education [2–4]. No clear preferences are identified amongst patients. In fact, they are more concerned with the information content than with the media. Patients want to know the full picture as long as it is presented in a non-alarmist fashion [7]. We have to be honest. Patient information is often based on physician’s assumptions of what patients may want or need to know. Patient information materials, such as leaflets, booklets, books, videos, computer and Internet-based information, have notably increased over the recent years. Most are based on theoretical considerations rather than evidence [13]. Information materials must contain scientifically reliable information and be presented in a form that is acceptable and useful to patients. It is very important that patient information is based on the best and most up-to-date information available [7].
Some medical decisions may be complex because the evidence regarding outcomes is uncertain or the options have variable risk–benefit profiles that patients value differently [23]. Practice guidelines for these difficult decisions recommend that patients understand the probable range of outcomes of options; consider the personal value they place on benefits versus risks and participate with their practitioners in deciding about treatment [23]. Patient education should take into account the needs of patients and apply appropriate communication methodologies [15].
Patient education: effectiveness and clinical relevance
From the available literature, the effectiveness of educational interventions and the clinical relevance of the benefits are still unclear [20, 24, 25]. Patient education has two major drawbacks: Firstly, its statistically significant benefits are modest. Secondly, the benefits of patient education are short lived [24]. Inadequate attention to health education principles and educational programme design are often more problematic than the issues of content [29]. The quality of the analysis prior to designing an educational intervention will certainly determine its subsequent effectiveness [17]. Some recognize that important omissions could have been avoided if patients had been consulted about their information needs before the materials were developed [7].
The effect of patient education material should be assessed with the same rigour as other interventions [27]. Patient education is entering a new era where accountability in educational outcomes, interest in literacy/language barriers and the importance of cost-effectiveness will influence the process of patient education and inevitably patient choice. Prioritizing educational content and using validated instruments for measuring the outcomes of patient education will be necessary steps in improving patient outcomes [29].
There has been an assumption that all benefits of patient education would be generic. However, more recent studies raise doubts on the achievement of meaningful benefits in certain areas of medicine and suggest that future research should be disease specific [25]. The effectiveness of the interventions depends upon the context in which treatment decisions are made and the nature of available options. A recent meta-analysis shows that good-quality information has a positive effect in cancer patients [11]. A systematic review of rheumatoid arthritis patient education found a small beneficial effect of patient education at the first follow-up, but failed to show long-term benefit from patient education interventions [25]. In cardiovascular disease, participation in education programmes has been shown to result in improved clinical outcomes, including statistically significant reduction in the 10-year cardiovascular disease risk as well as actual cardiovascular disease events in the long term [17]. While past studies suggest that patient education may be associated with better clinical outcomes, doubts remain on the effectiveness of patient education strategies in anticoagulation therapy [29].
The vast majority of studies analysing patient education in spinal disorders focuses on back pain. The educational material available related to patient education in spinal deformities is much less by comparison.
Back pain
Consistently, patient’s beliefs and attitudes about back pain have been important predictors of outcome [10]. Contrary to recent evidence-based clinical practice guidelines, most subjects have pessimistic beliefs. Given the mismatch between public beliefs on back pain and current evidence, strategies for changing the public perceptions are required. The population exposed to a social marketing intervention (education campaign within the Australian state of Victoria) showed sustained improvements in back pain beliefs, as well as dramatic reductions in health-care use and work-related disability. The end result was a reduction in the number of individuals with long-term, disabling back conditions and a substantial cost saving [10]. Significant sustained improvements in population beliefs on back pain were observed 3 years after cessation of the media campaign [2] and these continued in primary care physcians for even longer [3].
Written information has been shown to improve patient satisfaction and disease knowledge. However, knowledge alone is rarely sufficient for behaviour change [17]. Recent data show that there is conflicting evidence that information positively modifies beliefs on back pain or is efficient in preventing LBP occurrences, recurrences and consequences such as health-care use [13]. Earlier investigations suggested that the Back book, an evidence-based patient educational booklet, improves back beliefs significantly, both fear-avoidance beliefs about physical activity and beliefs about the consequences of back trouble [5]. A recent systematic review concludes that there is strong evidence that the booklet increases knowledge, compared with no intervention or usual care alone, associated with a healthcare provider-related cue or videodisc [13]. Cultural aspects and the clinical setting where the booklet is provided play a role. Physician-related cues may increase in the short-term the confidence in booklet use or and adherence to exercises as compared with providing the booklet without those cues [13]. In French and British adults of working age seeking medical care for low back pain, adding the back book or postural hygiene pamphlet improves disability, reduces reattendances and improves positive beliefs when compared with not giving it. However in Dutch patients, there was no advantage over usual care [12, 16]. Improving back beliefs may not modify every clinical outcome or have only a small treatment effect. There is strong evidence that the booklet is not effective with regard to absenteeism. Information based on a biopsychosocial model is an efficient strategy to modify patients’ fears and beliefs on back pain and increase the adherence to exercises [13]. There is moderate evidence that back schools, consisting of information and back exercises, conducted in occupational settings are more effective for patients with recurrent and chronic low back pain than other treatments, placebo or waiting list controls for pain during short- and intermediate-term follow-up [14].
The most recent systematic review on patient education in back related problems shows that there is no difference between the effects of various types of individual patient education [8]. The way the educational material has been developed and presented and the time spent by patients in reading the material may all influence its effectiveness [8]. An individual oral educational intervention of 2.5 h is useful to speed up return to work in workers with acute or subacute LBP. Simple patient education sessions of shorter duration or written information do not seem to be effective as a sole treatment. However, as the authors point out, they may be considered harmless if they are evidence based and up to date. Thus, there is no reason for not using oral and written education to support treatment [8]. Henrotin et al. [13] reached a similar conclusion. Information packages including e-mail, videotape and an educational booklet are more effective than written information alone.
Computer-based patient education: EuroSpine Patient Line
Traditional patient education programmes have to face the potential barriers of storage, access problems and the need to keep content materials up to date. Computer-generated and archived resources might be a solution [27]. Prior to the Internet, specialist knowledge of health care was required to access medical information, and physicians were almost the sole holders of medical information. Whereas only 20% of Internet users will buy goods online, 84% would use the Internet for medical information [28]. Undoubtedly, the use of the Internet for patient information needs will continue to expand as Internet access becomes readily available. The World Wide Web will probably change the way physicians interact with patients, just as the printing press changed the paradigm for who had access to and possession of information [28]. Patients use the Web to research their conditions and treatment options, to share more effectively in the decision-making process.
Vulnerable or seriously ill patients may be given false hope by Web sites making misleading or inaccurate claims regarding treatment options. Unscrupulous marketing by licensed or unregulated industry may target patient chat rooms. Ethical sites exist to inform, but awareness and access is low. Some sites provide excellent PDF downloads to assist patients such as the “I’ve got nothing to lose by trying it”, available at http://www.senseaboutscience.org.uk, which helps patients to weigh up claims of cures and treatments for long-term conditions.
A computer-based resource provides a number of advantages, including “just-in-time” availability, a private learning environment, and immediate reinforcement of the learning that has occurred [18]. Interactive technology is able to tailor the information to the individual, who can control the information flow [11]. To best meet individual learning needs, patients look for opportunities to learn in ways that work for them. At various points during the learning processes, patients need opportunities to reflect on what they have learnt and what they still need to know. Computer-based technologies that customize the assessment and education intervention processes may support this important educational concept [18]. Financial, administrative and attitudinal barriers may limit its progression. However, the final cost of computer-based patient education may be less than the cost of printed material [27].
Availability and training for computer-based learning programmes are more accessible in the developed world; access is not always equitable. They have been shown to be effective for persons across the age continuum. Rural patients and those from lower socioeconomic backgrounds respond well to computer-based interventions [18]. In fact, patients with low literacy skills may have greater benefit from the individualized pace of instruction and the non-threatening learning that occurs with a multimedia programme. The use of graphics and audio may make understanding easier for individuals with limited reading ability [18]. It is still difficult to generalize about the effects of computer-generated patient education material on professional practice, but some early studies suggest that repeated instruction by this media results in a greater change of behaviour than single-session traditional instruction [18]. Computer-based patient education can occur at their pace. It has a positive impact on knowledge acquisition and supports patients’ understanding of their personal disease and management plan. It increases involvement in learning and expands patients’ understanding of their medical conditions [18].
Almost 70% of patients would like their physician to recommend a Web site for information, but only 4% receive such information [28]. The availability of Web server software means anyone can set up a Web site and publish unrestricted data that is accessible to everyone. The problem is no longer in finding information, but in assessing the credibility and validity of it. This can be a challenge to trained researchers accessing peer-reviewed learned articles; the problems for the patients are multiple. Retrieving high-quality online information that may be of use can be problematic. Search engines do not assess the validity and quality of the information. Two papers evaluate the quality of information on low back pain that a “typical” patient user might access on the Internet [6, 19]. They both highlight the poor quality of Internet information. The great majority of evaluated Web sites (96%) scored less than half the maximum available quality scores. In general, Web sites failed to provide information conforming to evidence. Another paper evaluating the quality and accuracy of information on scoliosis on the Internet reached very similar conclusions [21]. The large majority of the Web sites are of limited and poor quality, with 90% scoring less than 16 of a possible 32 on a content quality score. The potential for dissemination of inadequate or misleading information has been recognized [21]. A standard of ethics for the dissemination of patient-specific health information has not been universally accepted or imposed on the myriad of Web portals available on the Internet, but some organizations have combined to develop an e-Health code of ethics and quality criteria for health-related Web sites [1]. Developments such as the creation of a “dot. health” domain to guide Internet users to reliable health sites also may be of help [6]. Health Web sites should provide health information that is secure and trustworthy. Online advertising and disclosure of sponsorship or other financial relations that could significantly affect the site’s content or services must be clearly identified. Personal information must be kept private and secure and employ special precautions such as encryption. Consumers need to be able to distinguish online health services that follow ethic principles from those that do not [26].
EuroSpine Patient Line (http://www.eurospine.org)
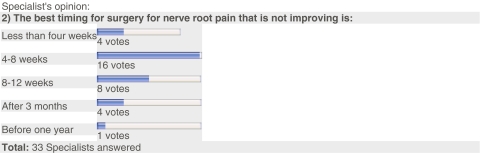
The requirement for a patient information section in the Web site of Eurospine, the Spine Society of Europe, was discussed and became the main message of Dieter Grob’s 2002 Presidential address. Patient Line (PL) was born in 2005 to offer patients and the general population the accumulated expertise represented by the members of the society. The Society decided to have a reliable open window to the external world to provide up-to-date information related to spinal disorders based on the best published evidence and expert opinion. In areas where evidence is scarce, Patient Line provides a real-time opinion of the EuroSpine membership, represented by the percentage of votes endorsing each treatment option (Fig. 1). Using the information available on PL, commonly accepted procedures can be evaluated by the patients themselves. In addition, patients should be able to evaluate the popularity or uncertainty amongst experts of specific treatments they have been offered. This information should result in a better understanding of their own treatment and involve them in the process of shared decision making. The published data is not meant to be the ultimate truth, but should reflect the pragmatic and the common sense range of treatments offered by the Eurospine membership. However, if patients find a significant difference between the answers shown in the graphs and their doctor’s opinion, they should be encouraged to ask what made him/her reach such a decision.
Fig. 1.
Graph expressing the real-time opinion of EuroSpine membership
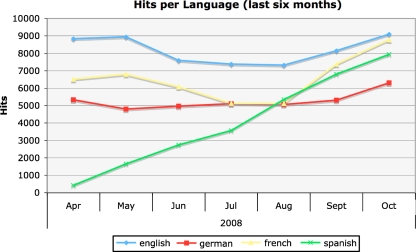
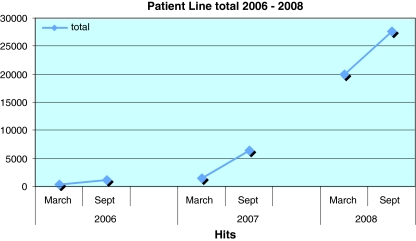
Patient Line intends to be a link between evidence, daily practice and patients. The first chapters have been dedicated to sciatica, scoliosis, cervical pain syndromes, low back pain and motion preservation surgery. Since 2008, the information has been available in English, German, French and Spanish. In 2007, Patient Line was the most visited area of EuroSpine Web site with 3,000–5,000 hits per month, which increased almost tenfold (21,000–23,000 hits per month) in 2008 (Figs. 2, 3). This original idea is growing quickly and has been very well received. It is time to improve its structure to reach as many patients as possible in a continent where English is still unknown to a large percentage of the population. National Web sites of spine societies provide similar information sources to patients and have a similar average “hit” rate, but are not so interactive (http://www.geeraquis.org, http://www.spinesurgeons.ac.uk). The goal should be for Patient Line to become THE European patient information Web site on spinal disorders, providing reliable and updated best practice and evidence-based information where the evidence exists. It needs to cover a wide range of topics and adhere to modern e-health code of ethics and quality criteria for health-related Web sites.
Fig. 2.
EuroSpine Patient Line hits per language from April to October 2008
Fig. 3.
Patient Line, March to September, hits in the last 3 years
Acknowledgments
Conflict of interest statement None of the authors has any potential conflict of interest.
References
- 1.Boyer C, Gaudinat A, Baujard V, Geissbühler A. Health on the net foundation: assessing the quality of health pages all over the world. Stud Health Technol Inform. 2007;129(Pt 2):1017–1021. [PubMed] [Google Scholar]
- 2.Buchbinder R, Jolley D. Effects of a media campaign on back beliefs is sustained 3 years after its cessation. Spine. 2005;30:1323–1330. doi: 10.1097/01.brs.0000164121.77862.4b. [DOI] [PubMed] [Google Scholar]
- 3.Buchbinder R, Jolley D. Improvements in general practitioner beliefs and stated management of back pain persist 4.5 years after the cessation of a public health media campaign. Spine. 2007;32:E156–E162. doi: 10.1097/01.brs.0000256885.00681.00. [DOI] [PubMed] [Google Scholar]
- 4.Buchbinder R, Jolley D, Wyatt M. 2001 Volvo award winner in clinical studies: effects of media campaign on back pain beliefs and its potential influence on management of low back pain in general practice. Spine. 2001;26:2535–2542. doi: 10.1097/00007632-200112010-00005. [DOI] [PubMed] [Google Scholar]
- 5.Burton K, Waddell G, Burtt R. Patient educational material in the management of low back pain in primary care. Hosp Jt Dis. 1996;55:138–141. [PubMed] [Google Scholar]
- 6.Butler L, Foster NE. Back pain online. a cross-sectional survey of the quality of Web-based information on low back pain. Spine. 2003;28:395–401. doi: 10.1097/00007632-200302150-00017. [DOI] [PubMed] [Google Scholar]
- 7.Coulter A, Entwistle V, Gilbert D. Sharing decisions with patients: is the information good enough? BMJ. 1999;318:318–322. doi: 10.1136/bmj.318.7179.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engers A, Jellena P, Wensing M, van der Windt DA, Grol R, van Tulder MW (2008) Individual patient education for low back pain. Cochrane Database Syst Rev (1):CD004057(publ 3). doi:10.1002/14651858 [DOI] [PMC free article] [PubMed]
- 9.Finset A. Patient education and counselling in a changing era of health care. Patient Educ Couns. 2007;66:2–3. doi: 10.1016/j.pec.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 10.Gross DP, Ferrari R, Russell AS, Battié MC, Schopflocher D, Hu RW, Waddell G, Buchbinder R. A population-based survey of back pain beliefs in Canada. Spine. 2006;31:2142–2145. doi: 10.1097/01.brs.0000231771.14965.e4. [DOI] [PubMed] [Google Scholar]
- 11.Gysels M, Higginson IJ. Interactive technologies and videotapes for patient education in cancer care: systematic review and meta-analysis of randomised trials. Support Care Cancer. 2007;15:7–20. doi: 10.1007/s00520-006-0112-z. [DOI] [PubMed] [Google Scholar]
- 12.Haas M, Groupp E, Muench J. Chronic disease self-management program for low back pain in the elderly. J Manipulative Physiol Ther. 2005;28:228–237. doi: 10.1016/j.jmpt.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 13.Henrotin YE, Cedraschi C, Duplan B, Bazin T, Duquesnoy B. Information and low back pain management: a systematic review. Spine. 2006;31:E326–E334. doi: 10.1097/01.brs.0000217620.85893.32. [DOI] [PubMed] [Google Scholar]
- 14.Heymans MW, Tulder MW, Bombardier C, Koes BW. Back schools for non-specific low back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine. 2005;30:2153–2163. doi: 10.1097/01.brs.0000182227.33627.15. [DOI] [PubMed] [Google Scholar]
- 15.Hubley J. Patient education in the developing world: a discipline comes of age. Patient Educ Couns. 2006;61:161–164. doi: 10.1016/j.pec.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 16.Jellema P, Roer N, Windt DA, Tulder MW, Horst HE, Stalman WA, Bouter LM. Should treatment of (sub)acute low back pain be aimed at psychosocial prognostic factors? Cluster randomised clinical trial in general practice. BMJ. 2005;331:84. doi: 10.1136/bmj.38495.686736.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.John H, Hale ED, Treharne GJ, Kitas GD. Patient education on cardiovascular aspects of rheumatoid disease: an unmet need. Rheumatology. 2007;46:1513–1516. doi: 10.1093/rheumatology/kem176. [DOI] [PubMed] [Google Scholar]
- 18.Lewis D. Computer-based approaches to patient education: a review of the literature. J Am Med Inform Assoc. 1999;6:272–282. doi: 10.1136/jamia.1999.0060272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li L, Irvin E, Guzman J. Surfing for back pain patients: the nature and quality of back pain information on the Internet. Spine. 2001;26:545–557. doi: 10.1097/00007632-200103010-00020. [DOI] [PubMed] [Google Scholar]
- 20.Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N (2003) The clinical cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation. Health Technol Assess 7(22):iii, 1–190 [DOI] [PubMed]
- 21.Mathur S, Shanti N, Brkaric M, Sood V, Kubeck J, Paulino C, Merola AA. Surfing for scoliosis: the quality of information available on the Internet. Spine. 2005;30:2695–2700. doi: 10.1097/01.brs.0000188266.22041.c2. [DOI] [PubMed] [Google Scholar]
- 22.Molenaar S, Sprangers MAG, Postma-Schuit FCE, Rutgers EJT, Noorlander J, Hendriks J, Haes HCJM. Feasibility and effects of decision aids. Med Decis Making. 2000;20:112–127. doi: 10.1177/0272989X0002000114. [DOI] [PubMed] [Google Scholar]
- 23.O’Connor AM, Rostom A, Fiset V, Tetroe J, Entwistle V, Llewellyn-Thomas H, Holmes-Rovner M, Barry M, Jones J. BMJ. 1999;319:731–734. doi: 10.1136/bmj.319.7212.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Riemsma RP, Taal E, Kirwan JR, Rasker JJ. Patient education programmes for adults with rheumatoid arthritis: benefits are small and short-lived. BMJ. 2002;325:558–559. doi: 10.1136/bmj.325.7364.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Riemsma RP, Taal E, Kirwan JR, Rasker JJ. Systematic review of rheumatoid arthritis patient education. Arthritis Care Res. 2004;15:1045–1059. doi: 10.1002/art.20823. [DOI] [PubMed] [Google Scholar]
- 26.Shepperd S, Charnock D, Gann B. Helping patients access high-quality health information. BMJ. 1999;319:764–766. doi: 10.1136/bmj.319.7212.764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Treweek SP, Glenton C, Oxman AD, Penrose A. Computer-generated patient education materials: do they affect professional practice? A systematic review. J Am Med Inform Assoc. 2002;9:346–358. doi: 10.1197/jamia.M1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ullrich PF, Vaccaro AR. Patient education on the Internet: opportunities and pitfalls. Spine. 2002;27:E185–E188. doi: 10.1097/00007632-200204010-00019. [DOI] [PubMed] [Google Scholar]
- 29.Wofford JL, Wells MD, Singh S. Best strategies for patient education about anticoagulation with warfarin: a systematic review. BMC Health Serv Res. 2008;8:40. doi: 10.1186/1472-6963-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]