Abstract
Most quality improvement efforts in surgery have focused on the technical quality of care provided, rather than whether the care was indicated, or could have been provided with a safer procedure. Because risk is inherent in any procedure, reducing the number of unnecessary operations is an important issue in patient safety. In the case of lumbar spine surgery, several lines of evidence suggest that, in at least some locations, there may be excessively high surgery rates. This evidence comes from international comparisons of surgical rates; study of small area variations within countries; increasing surgical rates in the absence of new indications; comparisons of surgical outcomes between geographic areas with high or low surgical rates; expert opinion; the preferences of well-informed patients; and increasing rates of repeat surgery. From a population perspective, reducing unnecessary surgery may have a greater impact on complication rates than improving the technical quality of surgery that is performed. Evidence suggests this may be true for coronary bypass surgery in the US and hysterectomy rates in Canada. Though similar studies have not been done for spine surgery, wide geographic variations in surgical rates suggest that this could be the case for spine surgery as well. We suggest that monitoring geographic variations in surgery rates may become an important aspect of quality improvement, and that rates of repeat surgery may bear special attention. Patient registries can help in this regard, if they are very complete and rigorously maintained. They can provide data on surgical rates; offer post-marketing surveillance for new surgical devices and techniques; and help to identify patient subgroups that may benefit most from certain procedures.
Keywords: Spine surgery, Quality management
Introduction
The traditional purview of quality improvement efforts in surgery has been the technical quality of care. As others have noted, traditional quality review efforts typically start and stop at the hospital door and focus strictly on the process or outcomes of care delivered [1]. The process of reviewing individual cases is often triggered by an adverse event.
In this traditional paradigm, it is unusual to ask whether this care should have been delivered in the first place. Such quality review efforts never ask questions such as the following: should the procedure have been performed at all? Did the potential benefit to the patient outweigh the risks? Are there other patients not operated on who might have benefited more [1]? Could a less invasive form of surgery have offered greater or equal benefit with less risk?
An exception to this generalization occurs in some surgical departments where there is an “Indications Conference” that focuses on just such questions. However, such efforts are only likely to be effective if all cases are reviewed, and not selected, “interesting”, or “available” cases.
An important reason to examine such questions is that many adverse events following surgery are unavoidable consequences of the physiologic insult to patients. Indeed, some studies have suggested that only a minority of adverse events are a result of physician negligence. A familiar example occurs in drug prescribing, where a negative drug reaction may occur in a patient for whom a drug has been appropriately prescribed for the first time. This is an adverse event, but not one that is due to negligence. However, if a drug reaction occurs in a patient with a known sensitivity to the drug, this adverse event would be properly judged to be caused by negligence [1]. In a review of 30,000 patient records from 50 hospitals, adverse events were identified in 3.7% of hospital stays, but adverse events caused by negligence occurred in only 1% [2]. Thus, a majority of adverse events may be an unavoidable feature of care, making the question of whether the care was necessary an important quality concern.
In the field of spine surgery, there is persistent controversy about the indications for certain types of elective surgery, whether or not a fusion is required in addition to a decompression procedure, and when surgical implants are necessary [3]. Furthermore, one can make a case that at least in some regions, spine surgery, fusion procedures, and surgical implants may be overused. If this is true, then assessing the need for surgery in the first place, or the choice of a procedure, becomes prominently important in quality assurance.
Is there evidence of excessive spine surgery?
There is probably no definitive way to determine whether there is excessive spine surgery. As yet, we have no gold standard for determining the need for what are usually elective procedures, involving major components of physician judgment and patient preference. Patients may not fully understand the options available to them, including the choice of nonsurgical care. Yet randomized trials suggest that for the example of patients with sciatica, surgical and non-surgical care may have similar long term outcomes, though with a short-term advantage for surgery.
Several lines of evidence suggest that, at least in some countries and regions, spine surgery may be performed more often than necessary. These can be briefly summarized as follows.
International comparisons
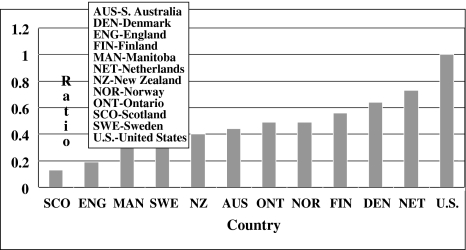
Rates of spine surgery vary dramatically from one country to the next, even among highly developed countries. The United States performs spine surgery at roughly twice the rate of most developed countries. The most recent formal comparisons suggest that the US rate is roughly twice that in New Zealand, Australia, Canada, Norway and Finland (Fig. 1). Spine surgery rates in the United Kingdom are about one-fifth of the US rate [4]. We have little reason to believe that there are biological differences from country to country, and epidemiologic studies suggest that rates of back pain are similar among geographic areas. Differences in health care organization and financing, surgical queues, patient expectations, surgical training, and professional uncertainty may explain some of these variations, but biological explanations seem unlikely. Although it may be that every other nation is underperforming spine surgery and that the US rate is optimal, it seems equally likely that lower rates may be optimal, and the US and other high rate countries may be performing excessive surgery.
Fig. 1.
Ratio of back surgery rate in selected countries to back surgery rate in the US (1988). (Adapted with permission from Spine, 1994, Lippincott Williams and Wilkins [4])
Other geographic variations
Even within countries, there are typically wide geographic variations in rates of spine surgery [5]. For example, one US study of the Medicare population showed 8-fold regional variation in rates of spinal decompression, and 20-fold variation in rates of spinal fusion [6]. To many observers, this suggests a poor consensus regarding indications for spine surgery and again raises the likelihood that rates may be excessive in some areas.
Trends in surgery rates
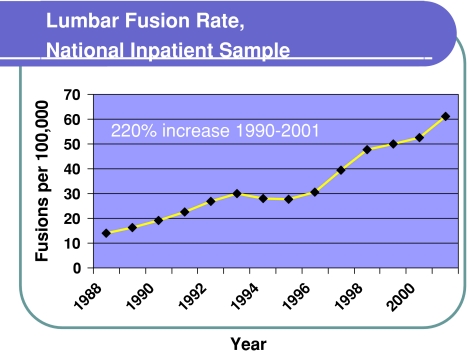
There is little reason to believe that anatomic abnormalities of the spine are becoming more common, and yet surgery rates, at least in the US, are steadily increasing [7]. This is not simply due to aging of the population, because most studies report age-adjusted rates. One study demonstrated a 220% increase in spinal fusion surgery in particular, between 1990 and 2000 (Fig. 2) [8]. This occurred in the absence of clarified indications or new demonstrations of efficacy for spine fusion. In fact, the increase preceded publication of the first randomized trial of fusion versus nonsurgical therapy for discogenic back pain. Although causal inferences cannot be made, there was a sharp acceleration in fusion rates after 1996, coinciding with the introduction of intervertebral interbody fusion cages [8].
Fig. 2.
Lumbar spine fusion rates, US National inpatient sample. (Adapted with permission from Spine, 2005, Lippincott Williams and Wilkins [8])
Other studies demonstrated that during the last 5 years of the 1990s, spine surgery rates in the Medicare population increased 40%; spine fusion rates increased 70%; and instrumented spinal fusions increased 100% [9]. A review of published literature similarly demonstrated a substantial increase in the use of fusion surgery and instrumentation from the 1980s to the 1990s, but with little change in reported solid fusion rates or in clinical outcomes [10].
Surgical outcomes
A study in the state of Maine identified regions that had low, intermediate, or high rates of lumbar spine surgery. In a prospective cohort study that involved most of the spine surgeons in the state, preoperative data were collected and post-operative follow-up was obtained over 2–4 years. By each of the outcomes measured (Roland Disability Score, satisfaction with surgical outcome, and rates of disability compensation) the best results occurred in areas with the lowest surgery rates and the worse outcomes occurred in areas with the highest surgical rates. The region with intermediate surgical rates had intermediate outcomes on each measure (Table 1) [11]. Although we cannot comment on outcomes for the patients who did not undergo surgery, these results suggest that higher rates of surgery did not necessarily lead to better outcomes. This seems consistent with randomized trial results for sciatica that show substantial improvement even with nonoperative care.
Table 1.
Lumbar surgical outcomes in 3 regions of Maine, according to surgical rates in each area
| Low rate area | Middle rate area | High rate area | |
|---|---|---|---|
| Improvement in Roland score* | 13 | 11 | 8 |
| Disability compensation | 8% | 10% | 18% |
| Satisfied with outcome* | 72% | 63% | 49% |
Follow-up was 2–4 years for all patients
*p < 0.05
Ref. [11]
Expert opinion
In the US, several prominent surgeons have voiced the opinion that excessive spinal fusion surgery is being performed. One neurosurgeon estimated that fewer than half of fusions are appropriate [12] and an orthopaedic surgeon was described as being worried by what he views as a proliferation of spinal fusions [13]. In a presidential address for the Scoliosis Research Society, Dr. Harry Shufflebarger described “a fusion cage explosion” after the 1996 approval of these devices, but went on to suggest that “4 years later, the efficacy of these stand-alone devices is very questionable” [14]. Although opinions certainly vary, these reports suggest that there is substantial expert opinion that too much spine fusion surgery is done in the US.
Preferences of well-informed patients
Formal decision aids have been developed for patients considering back surgery. These attempt to summarize as accurately as possible the available literature on outcomes of surgical and nonsurgical treatment for herniated disc, spinal stenosis, and axial low back pain. They also include video interviews of patients with good and bad outcomes from both surgical and nonsurgical treatments, to give the patient a vicarious sense of having good or bad outcomes. These decision aids have been shown to improve patient knowledge about back pain and treatment outcomes. In a randomized trial, patients who viewed the video decision aid had a 22% lower rate of spine surgery than the comparison group that received only briefer written materials. Despite a lower surgery rate, the pain and functional outcomes at 1 year were equivalent [15]. Thus, the rate of surgery chosen by well-informed patients along with their surgeons may be lower than that which occurs with usual care, with no decline in patient outcomes [15, 16]. Again, this suggests that surgical rates may be higher than necessary to optimize patient outcomes.
Repeat surgery
Second operations on the lumbar spine account for a substantial portion of all spine operations. Repeat surgery is usually viewed as undesirable, and is sometimes used as evidence of failure of the initial operation. Most repeat operations are a result of new or recurrent pain, device failures, or complications following an initial operation. Unfortunately, the results of second or subsequent operations are generally less favorable than those of the first operations.
Although it studied a worker’s compensation population, one study found that the success rate after a second lumbar surgical procedure was only 53%, after a third operation it was 35% and after a fourth or fifth operation it was even lower. After a fourth or fifth operation, patients were more likely to report being worse than being improved. Physician ratings of success were similarly disappointing [17]. These data suggest that repeat back surgery often does not have a successful result.
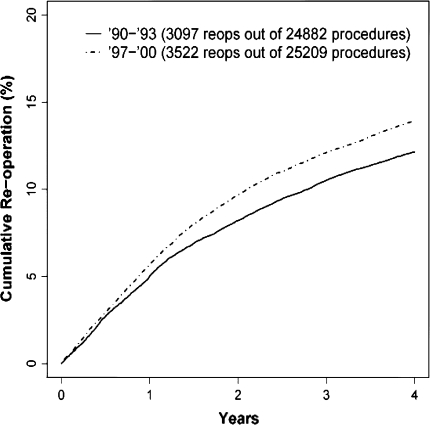
Studies in Washington State report that most repeat operations after fusion surgery are for problems with internal fixation devices or for pseudarthrosis [18]. This suggests that only a minority are for new disease at other spine levels. Furthermore, these studies found that, despite greater use of fusion surgery and surgical implants, the rate of repeat surgery was greater in the late 1990s than in the early 1990s (Fig. 3) [19]. Finally, these studies suggested that patients who underwent spinal fusion procedures were more likely to have repeat surgery than those who had decompression surgery alone, after the first year of follow-up [18]. These findings challenge the wisdom of the rising surgical rate during the 1990s, and also raise questions about the wisdom of more fusion surgery and surgical implants in particular.
Fig. 3.
Four-year cumulative probability of a second operation following a lumbar spine operation, Washington State, comparing patients operated in 1990–93 with those operated in 1997–2000. (Reproduced with permission from Spine, 2007, Lippincott Williams and Wilkins [19])
The reasons for possibly excessive spine surgery may be many. Excessive use of spine imaging may contribute to the problem [20, 21], along with unrealistic patient expectations, a desire to validate disability claims, or wishful thinking on the part of both doctors and patients. In some health care systems, financial incentives for hospitals, surgeons, and device manufacturers may play a role. Whatever the reasons may be, improved surveillance of surgical indications and the choice of surgical procedure could have an important impact in reducing rates of surgical complications.
A population prospective
The literature on quality improvement and the literature on geographic variations in care have developed quite independently of each other. However, as noted above, the observation of wide geographic variations in the use of surgical procedures raises the question of excessive rates in some areas and the consequent possibility that adverse events might be reduced by reducing excessive surgery. Thus, although adverse events caused by poor technique have been the traditional targets for quality improvement, adverse outcomes produced by high rates of surgery rarely undergo similar investigation. Failure to examine the potential for reducing adverse events by reducing high rates of intervention may have occurred because of the common assumption that more care is always better [1].
Thus, one might argue that more adverse outcomes in areas of high intervention rates are an acceptable trade-off, given the expected health benefits from high rates of intervention. However, the studies of regional outcomes in Maine, and the studies of shared decision making cited above suggest that high rates of surgery are not necessarily associated with health benefits.
Furthermore, no one suggests that negligent events discovered by traditional quality review efforts be ignored just because many patients who received the treatment also received benefits. This new population perspective asks not just whether there is an unnecessarily high rate of adverse events among people who got operations, but whether there is an unnecessarily high rate of adverse events among the population of a geographic region. If surgical rates vary independently of underlying disease rates, then the area’s population is a meaningful denominator for comparing the care delivered to residents of different areas [1].
This population-level perspective suggests that quality review efforts need not start and stop at the hospital door. They suggest that the negative consequences of high surgical rates on quality of care can be explored, but also that questions of poor access in low-rate areas can be explored. The traditional approach to quality improvement may identify practitioners who need improvement in technical skills; the population-based approach might identify surgical enthusiasts with excellent technical skills but who nonetheless produce poor outcomes for the population of the area they serve [1].
The population-based approach acknowledges that simply by virtue of where they live, residents of areas with high surgical rates are more likely than those in areas with low surgical rates to experience an adverse outcome from surgery. If the rate of surgical complications per operation is the same everywhere, then an area with 20 times more fusion surgery will produce 20 times more surgical complications than an area with a lower rate. Although technical quality of care for surgical patients may be greater in the region with high surgical rates, it would have to be markedly superior to cancel the increase in adverse outcomes related to the higher surgical rate.
Examples from other types of surgery
Canadian investigators have examined US data for coronary bypass surgery among 150 geographic areas of the US. They examined mortality within 30 days of admission to the hospital, during the hospital stay, and after discharge from the hospital. They found that the rate of death from bypass surgery per thousand Medicare enrollees varied 14-fold. The technical quality of care (judged by the mortality rate per thousand operations) was strongly related to the population’s overall rate of adverse outcomes. However, the overall surgical rate was also strongly associated with death rates among the geographic areas. In areas with high rates of surgery, reducing the surgical rate to the national average would have saved substantially more lives than simply reducing the mortality rate among surgical patients (the improvement in technical quality). However, in one city, with a bypass surgery rate lower than the US average, outcomes might have been more easily improved by focusing on technical quality than on surgical rates [1].
The same authors examined hysterectomy as a procedure that is less likely to result in surgical mortality. In this case, the researchers used rates of readmission to the hospital within 30 days of surgery as a marker of surgical complications. Previous medical record reviews by a physician panel had demonstrated that almost 80% of such readmissions were caused by complications of treatment. This study made use of Canadian data and demonstrated that three times more complications could be prevented by reducing an area’s surgical rate to the national average rate as by improving technical quality of care [1].
We are unaware of similar studies for spine surgery. However, spine surgery shows some of the widest geographic rate variations of all surgical procedures. Therefore, studies of this approach may be useful, and this may become an important aspect of quality improvement within a health system.
The choice of surgical procedure
Even among patients where a surgical benefit is highly likely, the choice of surgical procedure may be an important target for quality improvement. Certain types of spine surgery are associated with greater rates of complication than others. Unlike decompression alone, spine fusion requires decortication of bone and often the placement of implants. It requires more extensive dissection and longer operative time than decompression. Thus, it is not surprising that fusion surgery is associated with higher complication rates than decompression alone.
Studies of Medicare patients in the US, for example, suggest that any operation including a fusion is associated with higher rates of overall complications, blood transfusion, and post-operative mortality than decompression alone, even adjusting for patients’ age and comorbidity [3, 22]. Furthermore, rates of reoperation following spine fusion surgery may be greater than rates of reoperation following decompression alone [3, 18]. Paradoxically, reoperation rates may be the highest for fusions involving internal fixation devices as compared to bone grafting alone [23]. Complication rates are also greater when more levels are operated [24]. Thus, the choice of surgical procedure may have important implications for the likelihood of surgical complications.
In general, randomized trials comparing fusion with bone grafting alone to fusion with pedicle screws have shown no clinical advantage in terms of pain relief or function for those with instrumentation, although instrumentation does slightly increase the rate of solid fusion [3, 25–29]. Thus, it seems likely that any efficacy advantage of instrumentation in terms of clinical outcomes is small.
In contrast, with regard to complications, randomized trials show that patients with instrumentation have a substantially higher likelihood of repeat surgery, higher rates of nerve injury, greater blood loss, longer operative time, and a higher rate of overall complications [3, 23, 29]. Because implants also are expensive, their use may have the net effect of diverting resources from more highly effective clinical services to less effective clinical services.
Overall, the evidence suggests that choosing the least invasive procedure that can accomplish surgical goals may be the best procedure. This philosophy may conflict with a competing surgical theory, which is that the surgeon should try to correct every abnormality that appears on an imaging test in order to avoid future difficulties. The theory behind this “prophylactic” approach remains unproven, however, and the expectation of greater complications from more extensive surgery must be weighed against potential benefits.
Thus, surgeons may wish to carefully consider whether decompression alone would be sufficient; whether stabilizing structures such as the facet joints can be retained; whether a fusion procedure is really necessary; and if a fusion is performed, whether instrumentation is necessary. More research to inform this balance of risk and benefit, and the choice of surgical procedures in individual cases, would be extremely valuable.
Finally, one strategy for quality monitoring may be to scrutinize all cases of proposed repeat spine surgery. Such review might consider the evidence of diminishing returns with each successive operation, and also prompt examination of the indications for the initial operation.
Spine registries and post-marketing surveillance
The use of spine surgery registries will have limited value for understanding treatment efficacy. This is because of the known hazards of making non-randomized comparisons and the unmeasured confounding that often results. However, spine registries may be extremely valuable for studying the safety of alternative treatment approaches, and especially for identifying relatively uncommon complications. In an era of burgeoning innovations for spine surgery, including new bone substitutes, new biological substances, and new implants, registries may provide the best opportunity for post-marketing surveillance of unexpected complications and outcomes. Among other things, a well-designed registry provides the opportunity to record detailed information about patient symptoms, clinical findings, and imaging results: data that are not routinely available in most surveys, hospital discharge registries, or insurance claims databases.
To provide valid information, registries must be extremely complete and must succeed in obtaining follow-up results on virtually every patient. If patients are selectively included in the registry, the apparent results of surgery may appear better or worse than reality. The same error can occur if follow-up is not extremely complete. In many clinical studies, for example, patients with the worst baseline prognosis are the most likely to be lost to follow-up, creating an obvious potential for misleading results. However, if truly complete registries can be created, the potential for population-level monitoring of adverse events could be greatly enhanced. The ability to monitor safety in this fashion would add greatly to our ability to improve quality of care and to be more selective in the use of new treatments and technologies.
Another important advantage of treatment registries would be to help identify subgroups of patients who appear to benefit the most or the least from a particular treatment approaches. As just one example, some studies have noted a substantial improvement in outcomes following spine fusion for patients with spondylolisthesis, but a much smaller benefit for patients with degenerative disc and axial back pain alone [30]. Such information may help us to determine where restraint is the best clinical policy as well as situations where greater utilization may be of benefit.
Conclusions
In addition to monitoring the technical quality of care, an important agenda for quality improvement concerns restraint from performing unnecessary surgery or from performing unnecessarily invasive surgery. Cases of repeat surgery may bear particular scrutiny, examining the likelihood of success and the indications for the initial procedure. Taking a population prospective may be valuable in this regard, though it requires stepping outside the boundaries of a single hospital or clinical practice. Thus, it may be a role best filled by payers, government, or professional societies that would have access to data for an entire population.
Using data on geographic variations in care may be an important aspect of this approach, because reducing surgical rates in high rate areas to some average rate may have greater benefits in preventing adverse events than simply focusing on the technical quality of care. We have a growing body of knowledge about both efficacy and safety of many surgical treatments for spine disorders. However, the evidence-based, judicious use of these treatments, and patient selection, remain far from optimal. Though exceptional rigor will be necessary, spine registries may be one strategy for improving patient selection and the choice of procedures, and for identifying situations where restraint is the best clinical policy.
Acknowledgments
Conflict of interest statement None of the authors has any potential conflict of interest.
References
- 1.Roos NP, Black CD, Roos LL, Tate RB, Carriere KC. A population-based approach to monitoring adverse outcomes of medical care. Med Care. 1995;33:127–138. doi: 10.1097/00005650-199533020-00001. [DOI] [PubMed] [Google Scholar]
- 2.Brennan TA, Leape LL, Laird NM et al (1991) Incidence of adverse events and negligence in hospitalized patients: results of the Harvard Medical Practice Study I. N Engl J Med 324:370–376 [DOI] [PubMed]
- 3.Deyo RA, Nachemson A, Mirza SK. Spinal-fusion surgery: the case for restraint. N Engl J Med. 2004;350(7):722–726. doi: 10.1056/NEJMsb031771. [DOI] [PubMed] [Google Scholar]
- 4.Cherkin DC, Deyo RA, Loeser JD, Bush T, Waddell G. An international comparison of back surgery rates. Spine. 1994;19(11):1201–1206. doi: 10.1097/00007632-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Deyo RA, Mirza SK. Trends and variations in the use of spine surgery. Clin Orthop Relat Res. 2006;443:139–146. doi: 10.1097/01.blo.0000198726.62514.75. [DOI] [PubMed] [Google Scholar]
- 6.Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES. United States trends and regional variations in lumbar spine surgery: 1992–2003. Spine. 2006;31(23):2707–2714. doi: 10.1097/01.brs.0000248132.15231.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gray DT, Deyo RA, Kreuter W, Mirza SK, Heagerty PJ, Comstock BA, Chan L. Population-based trends in volumes and rates of ambulatory lumbar spine surgery. Spine. 2006;31:1957–1963. doi: 10.1097/01.brs.0000229148.63418.c1. [DOI] [PubMed] [Google Scholar]
- 8.Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BIUS. Trends in lumbar fusion surgery for degenerative conditions. Spine. 2005;30(12):1441–1445. doi: 10.1097/01.brs.0000166503.37969.8a. [DOI] [PubMed] [Google Scholar]
- 9.Lurie JD, Weinstein JN (2001) Shared decision-making and the orthopaedic workforce. Clin Orthop Relat Res 385:68–75. doi:10.1097/00003086-200104000-00012 [DOI] [PubMed]
- 10.Bono CM, Lee CK. Critical analysis of trends in fusion for degenerative disc disease over the past 20 years: influence of technique on fusion rate and clinical outcome. Spine. 2004;29(4):455–463. doi: 10.1097/01.BRS.0000090825.94611.28. [DOI] [PubMed] [Google Scholar]
- 11.Keller RB, Atlas SJ, Soule DN, Singer DE, Deyo RA. Relationship between rates and outcomes of operative treatment of lumbar disc herniation and spinal stenosis. J Bone Joint Surg Am. 1999;81(6):752–762. doi: 10.2106/00004623-199906000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Abelson R, Petersen M (2003) An operation to ease back pain bolsters the bottom line, too. The New York Times, December 31
- 13.Groopman J (2002) A knife in the back. New Yorker (April):8
- 14.Shufflebarger HL. Surgeons, societies, and companies: ethics and legalities. Spine. 2001;26:1947–1949. doi: 10.1097/00007632-200109150-00002. [DOI] [PubMed] [Google Scholar]
- 15.Deyo RA, Cherkin DC, Weinstein J, Howe J, Ciol M, Mulley AG., Jr Involving patients in clinical decisions: impact of an interactive video program on use of back surgery. Med Care. 2000;38(9):959–969. doi: 10.1097/00005650-200009000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Phelan EA, Deyo RA, Cherkin DC, et al. Helping patients decide about back surgery: a randomized trial of an interactive video program. Spine. 2001;26(2):206–211. doi: 10.1097/00007632-200101150-00016. [DOI] [PubMed] [Google Scholar]
- 17.Waddell G, Kummel EG, Lotto WN, Graham JD, Hall H, McCulloch JA. Failed lumbar disc surgery and repeat surgery following industrial injuries. J Bone Joint Surg Am. 1979;61(2):201–207. [PubMed] [Google Scholar]
- 18.Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA. Reoperation rates following lumbar spine surgery and the influence of spinal fusion procedures. Spine. 2007;32(3):382–387. doi: 10.1097/01.brs.0000254104.55716.46. [DOI] [PubMed] [Google Scholar]
- 19.Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA. Are lumbar spine reoperation rates falling with greater use of fusion surgery and new surgical technology? Spine. 2007;32(19):2119–2126. doi: 10.1097/BRS.0b013e318145a56a. [DOI] [PubMed] [Google Scholar]
- 20.Lurie JD, Birkmeyer NJ, Weinstein JN. Rates of advanced spinal imaging and spine surgery. Spine. 2003;28(6):616–620. doi: 10.1097/00007632-200303150-00018. [DOI] [PubMed] [Google Scholar]
- 21.Jarvik JG, Hollingworth W, Martin B, et al. Rapid magnetic resonance imaging vs radiographs for patients with low back pain: a randomized controlled trial. JAMA. 2003;289(21):2810–2818. doi: 10.1001/jama.289.21.2810. [DOI] [PubMed] [Google Scholar]
- 22.Deyo RA, Ciol MA, Cherkin DC, Loeser JD, Bigos SJ. Lumbar spinal fusion. A cohort study of complications, reoperations, and resource use in the Medicare population. Spine. 1993;18:1463–1470. doi: 10.1097/00007632-199318110-00010. [DOI] [PubMed] [Google Scholar]
- 23.Fritzell P, Hagg O, Nordwall A. Complications in lumbar fusion surgery for chronic low back pain: comparison of three surgical techniques used in a prospective randomized study. A report from the Swedish Lumbar Spine Study Group. Eur Spine J. 2003;12:178–189. doi: 10.1007/s00586-002-0493-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carreon LY, Puno RM, Dimar JR, 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85A:2089–2092. doi: 10.2106/00004623-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Fritzell P, Hagg O, Wessberg P, et al. Lumbar fusion versus nonsurgical treatment for chronic low back pain: a multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine. 2001;26:2521–2532. doi: 10.1097/00007632-200112010-00002. [DOI] [PubMed] [Google Scholar]
- 26.Fritzell P, Hagg O, Wessberg P, Nordwall A. Swedish lumbar spine study group. Chronic low back pain and fusion: a comparison of three surgical techniques. Spine. 2002;27:1131–1141. doi: 10.1097/00007632-200206010-00002. [DOI] [PubMed] [Google Scholar]
- 27.Gibson JNA, Waddell G. Surgery for degenerative lumbar spondylosis: updated Cochrane Review. Spine. 2005;30:2312–2320. doi: 10.1097/01.brs.0000182315.88558.9c. [DOI] [PubMed] [Google Scholar]
- 28.Moller H, Hedlund R. Instrumented and noninstrumented posterolateral fusion in adult spondylolisthesis—a prospective randomized study: part 2. Spine. 2000;25:1716–1721. doi: 10.1097/00007632-200007010-00017. [DOI] [PubMed] [Google Scholar]
- 29.Thomsen K, Christensen FB, Eiskjaer SP, Hansen ES, Fruensgaard S, Bunger CE. The effect of pedicle screw instrumentation on functional outcome and fusion rates in posterolateral lumbar spinal fusion: a prospective, randomized clinical study. Spine. 1997;22:2813–2822. doi: 10.1097/00007632-199712150-00004. [DOI] [PubMed] [Google Scholar]
- 30.Carragee EJ, Lincoln T, Parmar VS, Alamin T. A gold standard evaluation of the “discogenic pain: diagnosis as determined by provocative discography. Spine. 2006;31:2115–2123. doi: 10.1097/01.brs.0000231436.30262.dd. [DOI] [PubMed] [Google Scholar]