Abstract
The ankylosed spine is prone to fracture after minor trauma due to its changed biomechanical properties. Although many case reports and small series have been published on patients with ankylosing spondylitis (AS) suffering spine fractures, solid data on clinical outcome are rare. In advanced diffuse idiopathic skeletal hyperostosis (DISH), ossification of spinal ligaments also leads to ankylosis. The prevalence of AS is stable, but since DISH may become more widespread due to its association with age, obesity and type 2 diabetes mellitus, a systematic review of the literature was conducted to increase the current knowledge on treatment, neurological status and complications of patients with preexisting ankylosed spines sustaining spinal trauma. A literature search was performed to obtain all relevant articles concerning the outcome of patients with AS or DISH admitted with spinal fractures. Predefined parameters were extracted from the papers and pooled to study the effect of treatment on neurological status and complications. Ninety-three articles were included, representing 345 AS patients and 55 DISH patients. Most fractures were localized in the cervical spine and resulted from low energy impact. Delayed diagnosis often occurred due to patient and doctor related factors. On admission 67.2% of the AS patients and 40.0% of the DISH patients demonstrated neurologic deficits, while secondary neurological deterioration occurred frequently. Surgical or nonoperative treatment did not alter the neurological prospective for most patients. The complication rate was 51.1% in AS patients and 32.7% in DISH patients. The overall mortality within 3 months after injury was 17.7% in AS and 20.0% in DISH. This review suggests that the clinical outcome of patients with fractures in previously ankylosed spines, due to AS or DISH, is considerably worse compared to the general trauma population. Considering the potential increase in prevalence of DISH cases, this condition may render a new challenge for physicians treating spinal injuries.
Keywords: Ankylosing spondylitis, Diffuse idiopathic skeletal hyperostosis, Spine fracture, Ankylosis, Treatment
Introduction
The ankylosed spine is prone to fracture even after trivial trauma [51]. Several authors have shown patients with ankylosing spondylitis (AS) to have a fourfold fracture risk during their lifetime compared to unaffected individuals [27, 133]. In AS spontaneous fusion of the sacroiliac joints and spine occurs due to chronic inflammation leading to initial back pain followed by generalized stiffness of the spine. The disease has a prevalence of 0.1–1.4%; typically affects males and usually becomes apparent between 20 and 30 years of age [10]. Due to multilevel bony fusion, long lever arms develop in the spinal column on which forces can act during trauma [21]. During progression of the disease the spine becomes increasingly susceptible to injury, eventually even after low energy impacts [11, 50, 113]. Fractures in the ankylosed spine are often unstable due to the ossification of supportive and elastic soft tissues and may cause neurologic deficit as a result of dislocation [65, 112]. Moreover, because of unstable fracture configurations, initially intact patients may sustain secondary neurologic deterioration after unprotected transfers and manipulation [20]. Neurological deficit after fracture is a well known and feared complication in AS, therefore these patients should be handled with great care when a fracture is suspected [83, 94].
Diffuse idiopathic skeletal hyperostosis (DISH) is a supposedly non-inflammatory disease in which spinal longitudinal ligaments and entheses slowly become ossified leading to decreased mobility of the affected region until complete ankylosis follows [6]. DISH is diagnosed when flowing ossification of the anterior longitudinal ligament is present on spine radiographs over at least four consecutive levels [96]. Its etiology is unknown, but the associations with obesity, type 2 diabetes mellitus and advanced age have been demonstrated by several authors [18, 61]. Studies investigating the demographic characteristics of DISH have found a prevalence ranging from 2.9% in a Korean population to 25% in a selected population of Caucasian males in the United States of America [60, 127]. Acknowledging that DISH is associated with traits typical of modern affluent societies such as increasing life expectancy, obesity and type 2 diabetes, its prevalence and degree of expression can be expected to increase during the coming decades [107, 130]. Most symptoms of DISH are mild and develop slowly but an increasing amount of evidence suggests that DISH is a less innocent condition than previously assumed [104]. Serious complications of DISH in the cervical region for example, are dysphagia; difficult endotracheal intubation, myelopathy and spinal canal stenosis [70, 90, 109]. Some authors have speculated that patients with DISH are also at risk for spinal fractures after minor impacts, comparable to the fracture mechanism of AS patients [6, 88].
This systematic review aims to increase the knowledge on treatment, neurological status and complications of trauma patients with ankylosed spines (due to AS or DISH) and admitted with spine fractures, by pooling data previously published in the literature.
Materials and methods
To identify the relevant publications on this subject, a Medline and EMBASE search was performed. References were obtained from the search parameters ‘ankylosing spondylitis’ and ‘trauma’ and ‘diffuse idiopathic skeletal hyperostosis’ and ‘trauma’ (and their respective synonyms). Articles in languages other than English, French or German and articles without abstract were excluded. All articles were initially screened for relevance by title and abstract. Inclusion criteria were: publication date between 1st January 1980 and 31st December 2007, the presence of AS or DISH and a spinal fracture, a sufficiently detailed description of fracture type and trauma mechanism; an adequate description of neurological status, complications and period of follow-up [4]. The first 3 months after admission were (arbitrarily) defined as the post-treatment phase; thereafter it was defined as the follow-up phase. Consequently, patient’s data were only included in the follow-up group if this period (≥ 3 months) was specifically described in the article. If not, data were only included for the post-treatment phase. Sufficiently described case reports were included to obtain as much information as possible on this subject, simultaneously acknowledging the limited number of large-scale case series expected to be available in the literature. A cross-reference search was performed to obtain the remaining articles. Two authors performed the close reading of all papers and extracted data independently to minimize selection bias and errors. The parameters obtained from the papers and their definitions are listed in Table 1. The data from both readers were compared and where they differed, the pertaining paper was reread until consensus was reached. If overlap was present in two papers from the same author or institution, the least informative paper was excluded. The level of evidence of the included articles was determined according to the guidelines proposed by the Center for Evidence Based Medicine (CEBM) [86]. The independent-samples t test was used to determine statistical significance between the AS and DISH group (SPSS version 12.0.2; SPSS Inc., Chicago, USA).
Table 1.
Parameters extracted from the papers
| Parameter | Definition |
|---|---|
| Name and affiliation of the authors | |
| Year of publication and name of journal | |
| Study design | Prospective, retrospective, case report (n = 1 or n = 2), case study (n ≥ 3 individuals) |
| Follow-up | Months |
| Quality of paper | Oxford Center for Evidence-based Medicine, Levels of Evidence [86] |
| Mean age of patients | Years |
| Male/total ratio | Number of males divided by the total number of patients |
| Traumatic impact | High: motor vehicle accident; fall >15 feet [3] |
| Low: fall from standing or sitting position | |
| Polytrauma patients (%) | Number of polytrauma patients reported divided by the total number of patients reported |
| Fracture level | Cervical, thoracic, lumbar, sacral |
| Fracture type | Hyperextension, flexion, compression, rotation |
| Type of treatment | Surgical: posterior fixation, anterior fixation, combined anterior-posterior fixation, laminectomy |
| Conservative: traction, halo, collar, brace, plaster jacket, bed rest | |
| Immobilization type | Traction, halo, collar, brace, plaster jacket, bed rest or none |
| Immobilization duration | Weeks |
| Neurological outcome | ASIA impairment scale [4] |
| Complications | Neurologic deterioration, deep venous thrombosis, pulmonary embolism, wound infection, cystitis, pneumonia, pseudoarthrosis, decubitus and miscellaneous complications |
| Delayed diagnosis | Diagnosis established >24 h after trauma |
| Mortality | Number of deceased patients |
Results
The literature search and cross-referencing resulted in a total of 1,035 references (951 on AS and 84 on DISH) of which 894 were rejected due to off topic abstract content and/or failure to meet the inclusion criteria. After reading the remaining 141 full text papers (109 on AS and 32 on DISH), another 48 were excluded because of insufficient detail, overlap of same author/institution or uncertain history of trauma. The remaining 93 articles were included:
Ankylosing spondylitis: 76 articles, describing a total of 345 patients [1, 2, 5, 9, 11, 15, 17, 19, 21–25, 27–29, 31–34, 36, 37, 39–41, 43–45, 50, 52, 55, 57–59, 62, 64, 65, 67, 68, 73, 75–77, 80, 82, 83, 85, 87, 89, 91–94, 97–102, 105, 106, 110, 112–114, 116–122, 125, 126, 128, 132].
Diffuse idiopathic skeletal hyperostosis: 17 articles, describing a total of 55 patients [7, 12, 14, 16, 26, 30, 49, 54, 66, 74, 79, 81, 88, 108, 111, 128, 131].
All papers described retrospective case series or case reports, therefore all were assigned grade 4 level of evidence.
General information on the study population
The mean patient age was 59.1 years for AS and 68.2 years for DISH; the difference between the mean age of both groups was statistically significant (P = 0.004). Both groups consisted predominantly of males (male/total ratio was 0.90 in AS; 0.84 in DISH). The mean duration of follow-up was 11.2 months for AS and 12.0 months for DISH. Male/total ratio and follow-up duration were comparable in the AS and DISH groups (P > 0.05). The percentage of DISH patients with multiple trauma significantly exceeded AS patients; 10.9% in DISH versus 1.4% in AS (P = 0.034). In Table 2 details on the characteristics of the study population are presented.
Table 2.
Patient characteristics
| AS | DISH | P value | |
|---|---|---|---|
| Number of articles | 76 | 17 | |
| Mean follow-up (range) | 11.2 (1–65) | 12.0 (1–32) | 0.851 |
| Number of patients | 345 | 55 | |
| Mean age (SD–range) | 59.1 (12.6–32 to 82) | 68.2 (10.2–44 to 82) | 0.004 |
| Gender ratio | 0.90 | 0.84 | 0.538 |
| Polytrauma patients | 1.4% | 10.9% | 0.034 |
Bold entries are the P values for the parameters mean age and polytrauma patients
Trauma mechanism, fracture location and diagnosis
The majority of patients sustained low energy trauma causing their fracture; 227 patients with AS (65.8%) and 38 patients (69.1%) with DISH had low energy impacts. In most cases the trauma mechanism consisted of a fall from standing/sitting position. High energy impacts caused a fracture in 107 patients with AS (31.0%) and 13 patients with DISH (23.6%). In 11 patients with AS and four patients with DISH there was no recollection of trauma at all.
Most fractures were localized in the cervical spine; this was the case for 280 AS patients (81.2%) and 33 DISH patients (60.0%). Fractures of the thoracic spine were described more often in patients with DISH (34.5%) than in AS (10.7%). Fractures of the lumbar spine occurred in 27 AS patients (7.8%) and three DISH patients (5.5%). One sacral fracture occurred in a patient with AS. Hyperextension was the most frequent cause of fracture, representing the trauma mechanism for 96 patients with AS (74.4% of 129 reported cases) and 22 patients with DISH (51.2% of 43 reported cases). Flexion-type fractures occurred in 20 AS patients (15.5%) and in none of the DISH patients. Compression fractures were described in six AS patients and in six DISH patients. Rotation-type fractures were reported in seven patients with AS versus 15 patients with DISH. Details of the fracture type in relation to fracture level are listed in Tables 3 and 4.
Table 3.
Fracture type versus fracture level in patients with AS (based on n = 129)
| Cervical | Thoracic | Lumbar | Sacral | Total | |
|---|---|---|---|---|---|
| Extension | 68 (68.0%) | 15 (93.7%) | 12 (100%) | 1 (100%) | 96 (74.4%) |
| Flexion | 20 (20.0%) | 0 | 0 | 0 | 20 (15.5%) |
| Compression | 5 (5.0%) | 1 (6.3%) | 0 | 0 | 6 (4.7%) |
| Rotation | 7 (7.0%) | 0 | 0 | 0 | 7 (5.4%) |
| Total | 100 | 16 | 12 | 1 | 129 (100%) |
Table 4.
Fracture type versus fracture level in patients with DISH (based on n = 43)
| Cervical | Thoracic | Lumbar | Total | |
|---|---|---|---|---|
| Extension | 12 (44.4%) | 10 (71.4%) | 0 | 22 (51.2%) |
| Flexion | 0 | 0 | 0 | 0 |
| Compression | 3 (11.1%) | 2 (14.3%) | 1 (50%) | 6 (14.0%) |
| Rotation | 12 (44.4%) | 2 (14.3%) | 1 (50%) | 15 (34.9%) |
| Total | 27 | 14 | 2 | 43 (100%) |
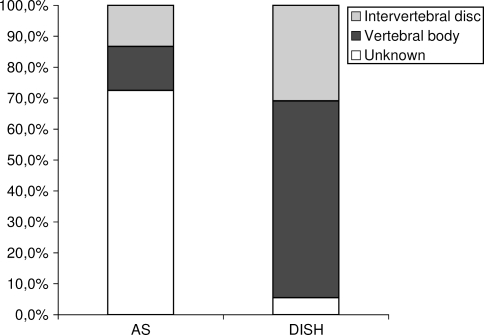
In patients with DISH the majority of fractures observed were through the vertebral body (63.6% of the total number of fractures), whereas in AS patients, the number of fractures through the vertebral body equaled the number of fractures through the intervertebral disc (see also Fig. 1). The large difference in number of fracture patterns reported for AS and DISH unfortunately prevents any quantitative comparison. A delay in diagnosis often occurred; in 59 patients with AS (17.1% of the total AS population) the fracture was not diagnosed within 24 h following trauma. In 31 patients (52.5% of these 59 patients) the fracture was not timely recognized by the physician (‘doctor’s delay’), while 28 patients (47.6%) delayed their decision to seek medical attention (‘patient’s delay’). In five patients with DISH (9.1%) the diagnosis was delayed by failure to identify the fracture, thus representing 100% doctor’s delay.
Fig 1.
Fracture localization in vertebral body or intervertebral disc (based on n = 345 in AS and n = 55 in DISH)
Treatment
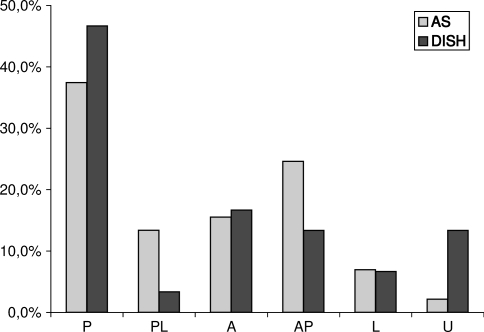
Surgical treatment was performed in 187 AS patients (54.2%) and in 30 DISH patients (54.5%) and consisted mainly of posterior fixation. In AS patients posterior procedures were more often combined with decompression of the spinal cord than in patients with DISH. In most articles the rationale behind the treatment strategy was not described, but reasons reported often were: (secondary) deterioration of neurological status, unstable fracture configuration and the presence of an epidural hematoma.
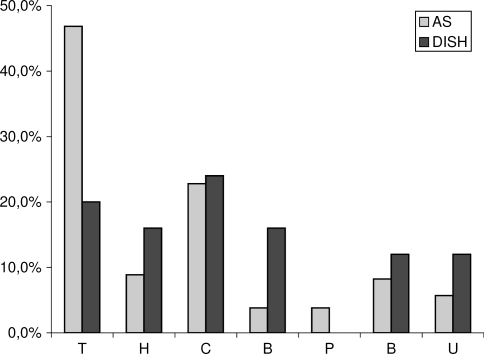
Conservative treatment was performed in 158 AS patients (45.8%) and 25 DISH patients (45.5%), respectively. The main reason to refrain from surgery was high surgical risk or patient refusal. In conservative treatment patients with DISH were most frequently treated with a collar whereas patients with AS were predominantly treated with cervical traction or collar. Immobilization by braces was applied in 16.0% of the DISH patients versus 3.8% of the AS patients, possibly reflecting the larger number of thoracic fractures for DISH patients. For details see Figs. 2 and 3.
Fig 2.
Surgical treatment in AS and DISH patients (based on n = 345 in AS and n = 55 in DISH). P posterior fixation, PL posterior fixation combined with laminectomy, A anterior fixation, AP anterior and posterior fixation, L laminectomy, U unknown
Fig 3.
Conservative treatment in AS and DISH patients (based on n = 345 in AS and n = 55 in DISH). T traction, H halo frame, C collar, B brace, P plaster jacket, B bedrest, U unknown
Neurological status
At the time of admission 232 AS patients (67.2%) had a neurologic deficit (ASIA A-D) versus 22 DISH patients (40.0%). Secondary deterioration of neurological status was observed in 48 patients AS patients (13.9%) and in eight DISH patients (14.5%) in the post-treatment phase (<3 months). In the follow-up phase (≥3 months) three AS patients and one DISH patient showed neurological deterioration. In the majority of cases the definitive treatment (whether surgical or nonoperative) did not influence the outcome of neurological status.
In the surgical group 111 AS patients (59.4%) showed no change in neurological function within the first 3 months, versus 23 DISH patients (76.7%). At follow-up the majority of patients had the same degree of neurological deficit they had in the post-treatment phase; 77 AS patients (73.3%) and 20 DISH patients (90.9%), respectively. Improvement of neurological status was described in 51 AS patients (27.3%) and two DISH patients (6.7%) in the post-treatment phase and in 28 AS patients (26.7%) and in two DISH patients (9.1%) at follow-up. In the conservatively treated patients 126 AS patients (79.7%) and 21 DISH patients (84.0%) demonstrated no change in neurological function during the post-treatment phase, at follow-up this was the case in 79 AS patients (74.5%) and 15 DISH patients (88.2%). In nine AS patients (5.7%) and one DISH (4.0%) patient neurological status improved in the post-treatment phase; at follow up 24 AS patients (22.6%) and one DISH patient (5.9%) showed improvement of neurological function. Overall, surgical treatment seemed to lead to neurological improvement in more AS and DISH patients than conservative treatment; both in the post-treatment phase and at follow-up.
Most patients improved one ASIA scale; this was the case in 36 patients with AS and three patients with DISH. A total of 13 AS patients improved two scales, nine patients improved three scales and in two patients an improvement of four ASIA scales was reported. In DISH patients improvements of only one ASIA scale were observed (see also Tables 5 and 6).
Table 5.
Neurological status in patients with AS (based on n = 345)
| Surgical treatment | ||||||
|---|---|---|---|---|---|---|
| N/K | A | B | C | D | E | |
| Post-treatment (<3 months) | ||||||
| N/K | 1 | |||||
| A | 28 | 3 | 1 | 5 | 2 | |
| B | 6 | 4 | 7 | 4 | ||
| C | 1 | 8 | 5 | 5 | ||
| D | 1 | 2 | 3 | 23 | 15 | |
| E | 7 | 1 | 7 | 3 | 45 | |
| Follow-up (>3 months) | ||||||
| A | 17 | 1 | ||||
| B | 2 | 5 | ||||
| C | 5 | 8 | 2 | |||
| D | 16 | 12 | ||||
| E | 37 | |||||
| Conservative treatment | ||||||
|---|---|---|---|---|---|---|
| N/K | A | B | C | D | E | |
| Post-treatment (< 3 months) | ||||||
| N/K | 1 | |||||
| A | 47 | |||||
| B | 8 | |||||
| C | 4 | 10 | 1 | |||
| D | 2 | 2 | 27 | 8 | ||
| E | 9 | 1 | 2 | 3 | 33 | |
| Follow-up (>3 months) | ||||||
| A | 26 | 1 | 2 | 1 | 1 | |
| B | 1 | 1 | 3 | |||
| C | 1 | 8 | ||||
| D | 1 | 18 | 7 | |||
| E | 1 | 33 | ||||
Bold values stand for the number of patients in which neurological status was unchanged after treatment, resulting in an ASIA classification that did not alter (so A–A, B–B, C–C etc)
Patients admitted with EMV = 3; therefore ASIA classification could not be assessed
N/K not known
Table 6.
Neurological status in patients with DISH (based on n = 55)
| Surgical treatment | |||||
|---|---|---|---|---|---|
| A | B | C | D | E | |
| Post-treatment (<3 months) | |||||
| A | 5 | 1 | |||
| B | |||||
| C | 3 | 1 | |||
| D | 1 | 4 | |||
| E | 1 | 3 | 11 | ||
| Follow-up (>3 months) | |||||
| A | 6 | ||||
| B | 1 | ||||
| C | 2 | 1 | |||
| D | 3 | 1 | |||
| E | 8 | ||||
| Conservative treatment | |||||
|---|---|---|---|---|---|
| A | B | C | D | E | |
| Post-treatment (<3 months) | |||||
| A | 5 | ||||
| B | |||||
| C | 1 | ||||
| D | 1 | ||||
| E | 2 | 1 | 15 | ||
| Follow-up (>3 months) | |||||
| A | 1 | ||||
| B | |||||
| C | |||||
| D | 1 | 1 | |||
| E | 1 | 13 | |||
Bold values stand for the number of patients in which neurological status was unchanged after treatment, resulting in an ASIA classification that did not alter (so A–A, B–B, C–C etc)
Complications
In seven patients with AS, uncommon complications of spinal fractures were described, such as aortic dissection (n = 4) [25, 100, 101, 120], aortic pseudoaneurysm (n = 1) [68] and tracheal rupture (n = 1) [59]. Most of these complications were lethal (n = 4). Besides these uncommon findings, general complications such as postoperative wound infections, deep venous thrombosis, pneumonia and respiratory insufficiency were frequently reported complications in both AS and DISH patients; the latter two complications were common and led to fatal outcome in many cases. In some articles complications (whether fatal or not) may not have been fully reported. Based on the data provided, however, the complication and mortality rate seemed to be higher in conservatively treated patients than in surgically treated patients (see Table 7 for details).
Table 7.
Complications in patients with AS and DISH: number of patients reported (fatal outcome)
| Complication | AS | DISH | ||
|---|---|---|---|---|
| Surgical | Conservative | Surgical | Conservative | |
| Aortic dissection | 3 (2) | 1 (1) | ||
| Aortic pseudoaneurysm | 1 | |||
| Cervical myelopathy | 1 (1) | |||
| Cardiac arrest | 1 (1) | 4 (4) | 1 (1) | |
| Cerebrovascular accident | 4 (3) | |||
| Decubitus | 1 | 2 | ||
| Deep venous thrombosis | 2 | 1 | ||
| Epidural hematoma | 7 | 4 | 1 | |
| Epilepsy | 1 (1) | |||
| Esophago-cutaneus fistula from tracheotomy | 1 | |||
| Gastrointestinal tract bleeding | 1 | 6 | ||
| Hemothorax | 1 | 1 | 1 | 1 |
| Heterotopic ossification | 1 | |||
| Instrumentation failure | 33 | 3 | 1 | |
| Massive hemorrhage during surgery | 3 | |||
| Multiple organ failure | 1 (1) | |||
| Nonunion/pseudoarthrosis | 6 | |||
| Pneumonia | 12 (10) | 22 (18) | 2 | 3 (2) |
| Pulmonary embolus | 3 (3) | 2 (2) | ||
| Respiratory insufficiency | 10 (6) | 24 (10) | 5 (4) | |
| Septicaemia | 2 (1) | 2 (2) | ||
| Tracheal rupture | 1 (1) | |||
| Wound infection | 9 | 1 | 1 | |
| Total number reported (fatal outcome) | 93 (26) | 83 (40) | 6 | 12 (8) |
| % of total reported patients (% fatal outcome) | 27.0 (7.5) | 24.1 (11.6) | 10.9 | 21.8 (14.5) |
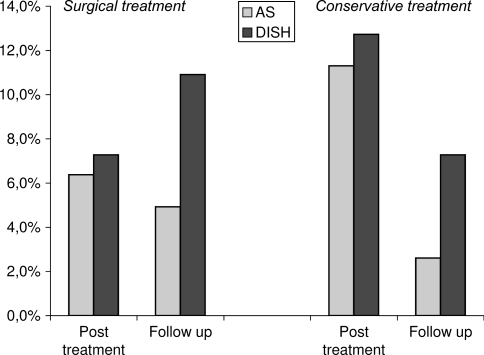
Mortality
The overall mortality in the post-treatment phase was comparable in both study groups; 6.4% in AS versus 7.3% in DISH in the surgically treated patients and 11.3% in AS versus 12.7% in DISH in the nonoperatively treated group. At follow-up the mortality in the surgically treated group was 4.9% for patients with AS and 10.9% for patients with DISH. The mortality in nonoperatively treated patients with DISH was also higher than in AS at follow-up; 7.3 versus 2.6%, respectively. These differences were not statistically significant (see also Fig. 4).
Fig 4.
Mortality in AS and DISH patients (based on n = 345 in AS and n = 55 in DISH)
A small number of AS patients died in the acute phase after trauma or intraoperatively as a result of severe complications such as lacerations of the aorta or trachea (see complications). The most frequent cause of death for both study groups, however, was pneumonia and/or respiratory failure; both in the post-treatment phase and at follow-up. The cause of death was not reported in 21 AS patients and in 13 patients with DISH.
Discussion
In the present study a systematic review of the literature was performed to increase the knowledge of treatment, neurological status and complications of patients with an ankylosed spine, due to AS or DISH, sustaining spinal fracture. The study groups were comparable with respect to gender ratio and follow-up duration. The mean age and the number of polytrauma patients were significantly higher in the DISH group than in the AS group. This renders in the authors’ opinion direct quantitative comparison of the treatment strategies, neurological outcome and complications of both groups impossible. Regarding the limited number of papers available; the weak study designs and low level of evidence of all articles, it follows that evidence is rather limited (immediately uncovering a weakness of the present study since it is based on these papers). The absence of adequate follow-up data can be considered the most significant weakness of the majority of papers included and may reflect the remarkably high morbidity/mortality rates of trauma patients with ankylosed spines compared to a ‘regular’ trauma population. From studies conducted previously to establish the outcome of traumatic spine fracture treatment, it was concluded that sufficient long-term follow-up has invariably been difficult to establish in these cohorts of patients [35, 63]. Some findings of the present study, however, deserve special attention.
The majority of fractures was caused by low energy impacts and was localized in the cervical spine. The cervical region is the most vulnerable part of the spinal column because of increased mobility, small vertebral bodies, oblique articular facets and the mobility of the heavy skull on the cervical spine [103, 129]. Mac Millan et al. [69] stated that traumatic fractures in patients with a partially fused spine tend to occur adjacent to the fused segments, rather than through the fused region itself. Paley et al. [88] also reported fractures to occur at the junction of the mobile and the fused spine. Hendrix et al. [42] found an association between the number of contiguously ankylosed segments of the spine and increased fracture instability. It can be hypothesized that the biomechanically vulnerable cervicothoracic junction becomes even more susceptible to injury in case of ankylosis since forces can act on longer lever arms.
In patients with AS, both doctor’s delay and patient’s delay in diagnosis occurred. Patient’s delay may have been caused by preexisting back pain not instantly distinguishable from fracture pain. Indeed, in some cases AS patients did not notice any symptoms as a result of fracture until abrupt neurological deterioration occurred [102, 122]. This phenomenon is referred to as ‘the fatal pause’ because of the delayed development of neurological deficits [20]. The absence of major trauma in the patient’s history may also lead to doctor’s delay, since spinal fractures will be suspected less after a trivial fall. Furthermore, radiographs of patients with ankylosing spine disorders may be difficult to interpret, due to preexisting pathologic osseous changes [42]. In DISH patients all delayed diagnoses were caused by doctor’s delay, possibly because of low awareness for this condition. This low awareness may also be responsible for the limited number of cases reported in the literature.
In patients with DISH the fracture was more often through the vertebral body than through the intervertebral disc (IVD). Some authors have previously suggested that the fracture mechanism may be different for AS and DISH, since AS fractures tend to occur more often at the level of the IVD while DISH fractures tend to occur at the level of the vertebral body [37]. A functional degradation of the IVD because of chondroid metaplasia and loss of elasticity due to calcification of the annulus fibrosis and nucleus pulposus making the IVD the weakest link in the AS affected spine, may contribute to this level dependent fracture configuration [88]. In advanced stages of DISH exuberant bone/calcifications are formed in the anterior longitudinal ligament, especially at the level of the IVD. It is suggested that at this level fractures may develop less easily than through the vertebral body where ligament ossification is minimal. Stress shielding as a result of load transfer through ossified ligaments leading to weakening of the vertebral body may also play a role in DISH fracture initiation and propagation [8]. Unfortunately, fracture patterns were only described in 95 AS patients (27.5% of the total AS group) so no solid conclusions could be drawn on this interesting subject.
The number of patients suffering from a neurological deficit was high in both groups; many patients with AS and DISH were admitted with a degree of neurological deficit. Worsening of neurological function due to inadequate immobilization, inconsiderate transfers or application of a hard collar on the cervical spine with pre-existing kyphotic deformity was reported in several articles [68, 74, 89, 122]. Compared to studies describing (healthy and considerably younger) individuals sustaining traumatic spine fractures where only 0.08% of the patients deteriorated in neurological function, these numbers are of major concern [124]. It is suggested that patients with traumatic fractures of the ankylosed spine are not only susceptible to initial neurological deficit but also to secondary neurological deterioration due to highly unstable fracture configurations between the fused segments [11]. In the absence of a definite stabilization method, transfer and manipulation of these patients should proceed with utmost care.
Different types of complications were reported for patients with AS and DISH. In some articles concerning AS patients, rare complications such as aorta laceration and rupture of the trachea were described. Aortitis is a known complication of AS, in which adventitial scarring, intimal proliferation and fibrous thickening of the aortic wall are commonly seen [25, 123]. Thoracic and lumbar injuries in AS patients may be associated with injury to the aorta either due to direct mechanical trauma or to blunt forces associated with the spinal fracture [100]. However, laceration may be most likely the result of pathophysiological changes that cause the aorta to become firmly adherent to the anterior longitudinal ligament and subject this structure to shearing forces during fracture dislocation [25, 101].
The mortality of surgically treated trauma patients with an ankylosing spinal disorder was high compared to previously healthy individuals with traumatic spine fractures. A total of 17.7% from the cohort of patients with AS and 20.0% from the patients with DISH deceased within 3 months after injury whereas the previously reported mortality in individuals treated surgically for traumatic spinal fractures was only 0.4% [124]. The mortality in the follow-up phase was higher in DISH patients than in AS patients, regardless of type of treatment received. Several authors have stated that advancing age, obesity and diabetes mellitus are associated with higher mortality rates in trauma patients [13, 46, 53, 56, 72, 78, 84]. In addition, some authors have reported the treatment with a halo frame or other immobilization device in elderly patients with cervical fractures to be associated with higher morbidity and mortality rates [47, 71, 115]. Finally, it is also known from the literature that surgery in elderly people is associated with higher rates of morbidity and mortality probably due to preexisting medical conditions [38, 48, 95]. Since DISH has been associated with obesity, type 2 diabetes and advancing age, this could explain the higher mortality [18, 61].
The prevalence of AS is stable and is estimated to be 0.05–1.4% [10]. Studies investigating DISH have found a prevalence ranging from 2.9 to 25% in selected populations [60, 127]. Acknowledging the association of DISH with typical traits of modern affluent societies (obesity and diabetes for example) its prevalence and degree of expression can be expected to increase during the coming decades, therefore clinicians should be prepared to admit more trauma patients with DISH [18, 61].
Recognizing the limitations of the current study, we suggest the following conclusions can be drawn (Level of Evidence 4; Grade of Recommendation C) [86].
Patients with an ankylosed spine have an increased fracture risk even after minor trauma.
Delayed diagnosis of fractures in patients with ankylosing spinal disorders often occur due to both doctor and patient related factors.
Fractures of the ankylosed spine tend to be unstable, because ossified ligaments and surrounding tissue also fracture.
An intrinsic unstable fracture configuration may lead to primary and secondary neurological deficit.
The clinical outcome of patients fracturing their ankylosed spine is worse compared to the general spine trauma population.
Surgical treatment may be favorable for patients with an ankylosed spine and spinal fracture, as this treatment option may be associated with lower complication and mortality rates and may lead to neurological improvement more frequently.
The presence of ankylosed spine segments should alert the treating physician for unstable spine fractures in every trauma patient.
In trauma registries ankylotic conditions of the spine should be registered separately, in order to acquire more knowledge on the patterns and prognosis of these injuries.
As DISH may be a rapidly increasing condition in affluent societies, awareness of this condition should be raised among physicians assessing trauma patients and treating spinal injuries.
Acknowledgments
Project no. S-07-20V was supported by the AO Research Fund of the AO Foundation.
Contributor Information
L. A. Westerveld, Phone: +31-88-7559001, FAX: +31-30-2510638, Email: l.a.westerveld@umcutrecht.nl
J. J. Verlaan, Email: jj.verlaan@wxs.nl
F. C. Oner, Email: f.c.oner@umcutrecht.nl
References
- 1.Akman MN, Karatas M, Kilinc S, et al. Double spinal cord injury in a patient with ankylosing spondylitis. Spinal Cord. 1999;37:305–307. doi: 10.1038/sj.sc.3100754. [DOI] [PubMed] [Google Scholar]
- 2.Amamilo SC. Fractures of the cervical spine in patients with ankylosing spondylitis. Orthop Rev. 1989;18:339–344. [PubMed] [Google Scholar]
- 3.American College of Surgeons Advanced Trauma Life Support for Doctors, Student Course Manual (1997). American College of Surgeons, Chicago
- 4.American Spinal Injury Association IMSoP International standards for neurologic and functional classification of spinal cord injury (1992). ASIA/IMSOP, Chicago
- 5.Baron M, Tator CH, Little H. Hangman’s fracture in ankylosing spondylitis preceded by vertical subluxation of the axis. Arthritis Rheum. 1980;23:850–855. doi: 10.1002/art.1780230712. [DOI] [PubMed] [Google Scholar]
- 6.Belanger TA, Rowe DE. Diffuse idiopathic skeletal hyperostosis: musculoskeletal manifestations. J Am Acad Orthop Surg. 2001;9:258–267. doi: 10.5435/00124635-200107000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Bernini PM, Floman Y, Marvel J, et al. Multiple thoracic spine fractures complicating ankylosing hyperostosis of the spine. J Trauma. 1981;21:811–814. doi: 10.1097/00005373-198109000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Bobyn JD, Mortimer ES, Glassman AH, et al. Producing and avoiding stress shielding. Laboratory and clinical observations of noncemented total hip arthroplasty. Clin Orthop Relat Res. 1992;274:79–96. [PubMed] [Google Scholar]
- 9.Boriani S, Romano B. Spinal lesions due to hyperextension in ankylosing spondylitis. Ital J Orthop Traumatol. 1983;9:365–368. [PubMed] [Google Scholar]
- 10.Braun J, Sieper J. Ankylosing spondylitis. Lancet. 2007;369:1379–1390. doi: 10.1016/S0140-6736(07)60635-7. [DOI] [PubMed] [Google Scholar]
- 11.Broom MJ, Raycroft JF. Complications of fractures of the cervical spine in ankylosing spondylitis. Spine. 1988;13:763–766. doi: 10.1097/00007632-198807000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Burkus JK, Denis F. Hyperextension injuries of the thoracic spine in diffuse idiopathic skeletal hyperostosis. Report of four cases. J Bone Joint Surg Am. 1994;76:237–243. doi: 10.2106/00004623-199402000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Byrnes MC, McDaniel MD, Moore MB, et al. The effect of obesity on outcomes among injured patients. J Trauma. 2005;58:232–237. doi: 10.1097/01.ta.0000152081.67588.10. [DOI] [PubMed] [Google Scholar]
- 14.Callahan EP, Aguillera H. Complications following minor trauma in a patient with diffuse idiopathic skeletal hyperostosis. Ann Emerg Med. 1993;22:1067–1070. doi: 10.1016/s0196-0644(05)82754-4. [DOI] [PubMed] [Google Scholar]
- 15.Chong CF. Fracture of the delicate bamboo: a diagnostic pitfall. Ann Emerg Med. 2004;44:88–89. doi: 10.1016/j.annemergmed.2004.01.030. [DOI] [PubMed] [Google Scholar]
- 16.Corke CF. Spinal fracture and paraplegia after minimal trauma in a patient with ankylosing vertebral hyperostosis. Br Med J (Clin Res Ed) 1981;282:2035. doi: 10.1136/bmj.282.6281.2035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cornefjord M, Alemany M, Olerud C. Posterior fixation of subaxial cervical spine fractures in patients with ankylosing spondylitis. Eur Spine J. 2005;14:401–408. doi: 10.1007/s00586-004-0733-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Denko CW, Malemud CJ. Body mass index and blood glucose: correlations with serum insulin, growth hormone, and insulin-like growth factor-1 levels in patients with diffuse idiopathic skeletal hyperostosis (DISH) Rheumatol Int. 2006;26:292–297. doi: 10.1007/s00296-005-0588-8. [DOI] [PubMed] [Google Scholar]
- 19.Detwiler KN, Loftus CM, Godersky JC, et al. Management of cervical spine injuries in patients with ankylosing spondylitis. J Neurosurg. 1990;72:210–215. doi: 10.3171/jns.1990.72.2.0210. [DOI] [PubMed] [Google Scholar]
- 20.Einsiedel T, Kleimann M, Nothofer W, et al. Special problems and management in lesions of cervical spine affected by Bechterew’s disease. Unfallchirurg. 2001;104:1129–1133. doi: 10.1007/s001130170003. [DOI] [PubMed] [Google Scholar]
- 21.Einsiedel T, Schmelz A, Arand M, et al. Injuries of the cervical spine in patients with ankylosing spondylitis: experience at two trauma centers. J Neurosurg Spine. 2006;5:33–45. doi: 10.3171/spi.2006.5.1.33. [DOI] [PubMed] [Google Scholar]
- 22.El Masry MA, Badawy WS, Chan D. Combined anterior and posterior stabilisation for treating an unstable cervical spine fracture in a patient with long standing ankylosing spondylitis. Injury. 2004;35:1064–1067. doi: 10.1016/j.injury.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 23.Exner G, Botel U, Kluger P, et al. Treatment of fracture and complication of cervical spine with ankylosing spondylitis. Spinal Cord. 1998;36:377–379. doi: 10.1038/sj.sc.3100673. [DOI] [PubMed] [Google Scholar]
- 24.Fast A, Parikh S, Marin EL. Spine fractures in ankylosing spondylitis. Arch Phys Med Rehabil. 1986;67:595–597. [PubMed] [Google Scholar]
- 25.Fazl M, Bilbao JM, Hudson AR. Laceration of the aorta complicating spinal fracture in ankylosing spondylitis. Neurosurgery. 1981;8:732–734. doi: 10.1227/00006123-198106000-00019. [DOI] [PubMed] [Google Scholar]
- 26.Ferree BA, Wieser M, Clarke RP. Hyperextension spinal fracture. Orthop Rev. 1989;18:1061–1064. [PubMed] [Google Scholar]
- 27.Finkelstein JA, Chapman JR, Mirza S. Occult vertebral fractures in ankylosing spondylitis. Spinal Cord. 1999;37:444–447. doi: 10.1038/sj.sc.3100837. [DOI] [PubMed] [Google Scholar]
- 28.Fishman EK, Magid D. Cervical fracture in ankylosing spondylitis: value of multidimensional imaging. Clin Imaging. 1992;16:31–33. doi: 10.1016/0899-7071(92)90086-o. [DOI] [PubMed] [Google Scholar]
- 29.Foo D, Bignami A, Rossier AB. Two spinal cord lesions in a patient with ankylosing spondylitis and cervical spine injury. Neurology. 1983;33:245–249. doi: 10.1212/wnl.33.2.245. [DOI] [PubMed] [Google Scholar]
- 30.Foo D, Rossier AB. Post-traumatic spinal epidural hematoma. Neurosurgery. 1982;11:25–32. doi: 10.1227/00006123-198207010-00006. [DOI] [PubMed] [Google Scholar]
- 31.Foo D, Sarkarati M, Marcelino V. Cervical spinal cord injury complicating ankylosing spondylitis. Paraplegia. 1985;23:358–363. doi: 10.1038/sc.1985.57. [DOI] [PubMed] [Google Scholar]
- 32.Gartman J, Bullitt E, Baker ML. Axis fracture in ankylosing spondylitis: case report. Neurosurgery. 1991;29:590–594. doi: 10.1097/00006123-199110000-00018. [DOI] [PubMed] [Google Scholar]
- 33.Garza-Mercado R. Traumatic extradural hematoma of the cervical spine. Neurosurgery. 1989;24:410–414. doi: 10.1227/00006123-198903000-00018. [DOI] [PubMed] [Google Scholar]
- 34.Gelineck J, Carvalho A. Fractures of the spine in ankylosing spondylitis. RoFo. 1990;152:307–310. doi: 10.1055/s-2008-1046873. [DOI] [PubMed] [Google Scholar]
- 35.Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine. 1992;17:528–540. doi: 10.1097/00007632-199205000-00010. [DOI] [PubMed] [Google Scholar]
- 36.Govender S, Charles RW. Fracture of the dens in ankylosing spondylitis. Injury. 1987;18:213–214. doi: 10.1016/0020-1383(87)90141-0. [DOI] [PubMed] [Google Scholar]
- 37.Graham B, Peteghem PK. Fractures of the spine in ankylosing spondylitis. Diagnosis, treatment and complications. Spine. 1989;14:803–807. doi: 10.1097/00007632-198908000-00005. [DOI] [PubMed] [Google Scholar]
- 38.Gretschel S, Estevez-Schwarz L, Hunerbein M, et al. Gastric cancer surgery in elderly patients. World J Surg. 2006;30:1468–1474. doi: 10.1007/s00268-005-0633-5. [DOI] [PubMed] [Google Scholar]
- 39.Grisolia A, Bell RL, Peltier LF. Fractures and dislocations of the spine complicating ankylosing spondylitis: a report of six cases 1967. Clin Orthop Relat Res. 2004;422:129–134. doi: 10.1097/01.blo.0000131643.61246.0a. [DOI] [PubMed] [Google Scholar]
- 40.Hanson JA, Mirza S. Predisposition for spinal fracture in ankylosing spondylitis. AJR Am J Roentgenol. 2000;174:150. doi: 10.2214/ajr.174.1.1740150. [DOI] [PubMed] [Google Scholar]
- 41.Harrop JS, Sharan A, Anderson G, et al. Failure of standard imaging to detect a cervical fracture in a patient with ankylosing spondylitis. Spine. 2005;30:E417–E419. doi: 10.1097/01.brs.0000170594.45021.67. [DOI] [PubMed] [Google Scholar]
- 42.Hendrix RW, Melany M, Miller F, et al. Fracture of the spine in patients with ankylosis due to diffuse skeletal hyperostosis: clinical and imaging findings. AJR Am J Roentgenol. 1994;162:899–904. doi: 10.2214/ajr.162.4.8141015. [DOI] [PubMed] [Google Scholar]
- 43.Hertlein H, Schams S, Lob G. Extension-distraction injury of the lumbar spine in spondylarthrosis ankylopoetica. Unfallchirurgie. 1991;17:259–263. doi: 10.1007/BF02588404. [DOI] [PubMed] [Google Scholar]
- 44.Heyde CE, Robinson Y, Kayser R, et al. Fatal complex fracture of the cervical spine in a patient with ankylosing spondylitis after a fall from a racing bicycle. Sportverletz Sportschaden. 2007;21:148–151. doi: 10.1055/s-2007-963315. [DOI] [PubMed] [Google Scholar]
- 45.Hitchon PW, From AM, Brenton MD, et al. Fractures of the thoracolumbar spine complicating ankylosing spondylitis. J Neurosurg. 2002;97:218–222. doi: 10.3171/spi.2002.97.2.0218. [DOI] [PubMed] [Google Scholar]
- 46.Hollis S, Lecky F, Yates DW, et al. The effect of pre-existing medical conditions and age on mortality after injury. J Trauma. 2006;61:1255–1260. doi: 10.1097/01.ta.0000243889.07090.da. [DOI] [PubMed] [Google Scholar]
- 47.Horn EM, Theodore N, Feiz-Erfan I, et al. Complications of halo fixation in the elderly. J Neurosurg Spine. 2006;5:46–49. doi: 10.3171/spi.2006.5.1.46. [DOI] [PubMed] [Google Scholar]
- 48.Hornick TR. Surgical innovations: impact on the quality of life of the older patient. Clin Geriatr Med. 2006;22:499–513. doi: 10.1016/j.cger.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 49.Houk RW, Hendrix RW, Lee C, et al. Cervical fracture and paraplegia complicating diffuse idiopathic skeletal hyperostosis. Arthritis Rheum. 1984;27:472–475. doi: 10.1002/art.1780270418. [DOI] [PubMed] [Google Scholar]
- 50.Hunter T, Dubo HIC. Spinal fractures complicating ankylosing spondylitis. A long-term followup study. Arthritis Rheum. 1983;26:751–759. doi: 10.1002/art.1780260608. [DOI] [PubMed] [Google Scholar]
- 51.Hunter T, Forster B, Dvorak M. Ankylosed spines are prone to fracture. Can Fam Physician. 1995;41:1213–1216. [PMC free article] [PubMed] [Google Scholar]
- 52.Iplikcioglu AC, Bayar MA, Kokes F, et al. Magnetic resonance imaging in cervical trauma associated with ankylosing spondylitis: report of two cases. J Trauma. 1994;36:412–413. doi: 10.1097/00005373-199403000-00026. [DOI] [PubMed] [Google Scholar]
- 53.Irwin ZN, Arthur M, Mullins RJ, et al. Variations in injury patterns, treatment, and outcome for spinal fracture and paralysis in adult versus geriatric patients. Spine. 2004;29:796–802. doi: 10.1097/01.brs.0000119400.92204.b5. [DOI] [PubMed] [Google Scholar]
- 54.Israel Z, Mosheiff R, Gross E, et al. Hyperextension fracture-dislocation of the thoracic spine with paraplegia in a patient with diffuse idiopathic skeletal hyperostosis. J Spinal Disord. 1994;7:455–457. [PubMed] [Google Scholar]
- 55.Juric G, Coumas JM, Giansiracusa DF, et al. Hemothorax—An unusual presentation of spinal fracture in ankylosing spondylitis. J Rheumatol. 1990;17:263–266. [PubMed] [Google Scholar]
- 56.Kao LS, Todd SR, Moore FA. The impact of diabetes on outcome in traumatically injured patients: an analysis of the National Trauma Data Bank. Am J Surg. 2006;192:710–714. doi: 10.1016/j.amjsurg.2006.08.031. [DOI] [PubMed] [Google Scholar]
- 57.Kaplan SL, Tun CG, Sarkarati M. Odontoid fracture complicating ankylosing spondylitis: a case report and review of the literature. Spine. 1990;15:607–610. doi: 10.1097/00007632-199006000-00037. [DOI] [PubMed] [Google Scholar]
- 58.Kauppi M, Belt EA, Soini I. ‘Bamboo spine’ starts to bend—Something is wrong. Clin Exp Rheumatol. 2000;18:513–514. [PubMed] [Google Scholar]
- 59.Kessler T, Quintel M, Winkler H, et al. Lethal transverse fracture through the body of C6 with tracheal lesion in ankylosing spondylitis: case report. Unfallchirurg. 1996;99:525–529. [PubMed] [Google Scholar]
- 60.Kim SK, Choi BR, Kim CG, et al. The prevalence of diffuse idiopathic skeletal hyperostosis in Korea. J Rheumatol. 2004;31:2032–2035. [PubMed] [Google Scholar]
- 61.Kiss C, Szilagyi M, Paksy A, et al. Risk factors for diffuse idiopathic skeletal hyperostosis: a case-control study. Rheumatology (Oxford) 2002;41:27–30. doi: 10.1093/rheumatology/41.1.27. [DOI] [PubMed] [Google Scholar]
- 62.Kiwerski J, Wieclawek H, Garwacka I. Fractures of the cervical spine in ankylosing spondylitis. Int Orthop. 1985;8:243–246. doi: 10.1007/BF00266867. [DOI] [PubMed] [Google Scholar]
- 63.Knop C, Blauth M, Buhren V, et al. Surgical treatment of injuries of the thoracolumbar transition-3: Follow-up examination. Results of a prospective multi-center study by the “Spinal” Study Group of the German Society of Trauma Surgery. Unfallchirurg. 2001;104:583–600. doi: 10.1007/s001130170089. [DOI] [PubMed] [Google Scholar]
- 64.Lahoti OP, Callanan I, Reidy DP, et al. Hidden flexion injury of the cervical spine in ankylosing spondylitis. Injury. 1995;26:67–69. doi: 10.1016/0020-1383(95)90560-k. [DOI] [PubMed] [Google Scholar]
- 65.Lange U, Pape HC, Bastian L, et al. Operative management of cervical spine injuries in patients with Bechterew’s disease. Unfallchirurg. 2005;108:63–68. doi: 10.1007/s00113-004-0793-z. [DOI] [PubMed] [Google Scholar]
- 66.Le Hir PX, Sautet A, Le GL, et al. Hyperextension vertebral body fractures in diffuse idiopathic skeletal hyperostosis: a cause of intravertebral fluidlike collections on MR imaging. AJR Am J Roentgenol. 1999;173:1679–1683. doi: 10.2214/ajr.173.6.10584819. [DOI] [PubMed] [Google Scholar]
- 67.Liang CL, Lu K, Lee TC, et al. Dissociation of atlantoaxial junction in ankylosing spondylitis: case report. J Trauma. 2002;53:1173–1175. doi: 10.1097/00005373-200212000-00024. [DOI] [PubMed] [Google Scholar]
- 68.Lifshutz J, Lidar Z, Maiman D. Thoracic aortic pseudoaneurysm after spine trauma in ankylosing spondylitis. Case report. J Neurosurg Spine. 2005;2:218–221. doi: 10.3171/spi.2005.2.2.0218. [DOI] [PubMed] [Google Scholar]
- 69.Mac Millan M, Stauffer ES. Traumatic instability in the previously fused cervical spine. J Spinal Disord. 1991;4:449–454. doi: 10.1097/00002517-199112000-00007. [DOI] [PubMed] [Google Scholar]
- 70.Mader R. Clinical manifestations of diffuse idiopathic skeletal hyperostosis of the cervical spine. Semin Arthritis Rheum. 2002;32:130–135. doi: 10.1053/sarh.2002.33726. [DOI] [PubMed] [Google Scholar]
- 71.Majercik S, Tashjian RZ, Biffl WL, et al. Halo vest immobilization in the elderly: a death sentence? J Trauma. 2005;59:350–356. doi: 10.1097/01.ta.0000174671.07664.7c. [DOI] [PubMed] [Google Scholar]
- 72.Malik SA, Murphy M, Connolly P, et al. Evaluation of morbidity, mortality and outcome following cervical spine injuries in elderly patients. Eur Spine J. 2008;17:585–591. doi: 10.1007/s00586-008-0603-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Markel DC, Graziano GP. Fracture of the S1 vertebral body in a patient with ankylosing spondylitis. J Spinal Disord. 1992;5:222–226. [PubMed] [Google Scholar]
- 74.Maskery NSS, Burrows N. Cervical spine control; Bending the rules. Emerg Med J. 2002;19:592–593. doi: 10.1136/emj.19.6.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Matejka J. Hyperextension injuries of the thoracolumbar spine. Zentralbl Chir. 2006;131:75–79. doi: 10.1055/s-2006-921391. [DOI] [PubMed] [Google Scholar]
- 76.May PJ, Raunest J, Herdmann J, et al. Management of vertebral fractures in ankylosing spondylitis. Unfallchirurg. 2002;105:165–169. doi: 10.1007/s001130100326. [DOI] [PubMed] [Google Scholar]
- 77.McCall I, El Masri W, Jaffray D. Hangman’s fracture in ankylosing spondylitis. Injury. 1985;16:483–484. doi: 10.1016/0020-1383(85)90174-3. [DOI] [PubMed] [Google Scholar]
- 78.McGwin G, Jr, Maclennan PA, Fife JB, et al. Preexisting conditions and mortality in older trauma patients. J Trauma. 2004;56:1291–1296. doi: 10.1097/01.ta.0000089354.02065.d0. [DOI] [PubMed] [Google Scholar]
- 79.McKenzie MK, Bartal E, Pay NT. A hyperextension injury of the thoracic spine in association with diffuse idiopathic skeletal hyperostosis. Orthopedics. 1991;14:895–898. doi: 10.3928/0147-7447-19910801-14. [DOI] [PubMed] [Google Scholar]
- 80.Miller FH, Rogers LF. Fractures of the dens complicating ankylosing spondylitis with atlantooccipital fusion. J Rheumatol. 1991;18:771–774. [PubMed] [Google Scholar]
- 81.Mody GM, Charles RW, Ranchod HA, et al. Cervical spine fracture in diffuse idiopathic skeletal hyperostosis. J Rheumatol. 1988;15:129–131. [PubMed] [Google Scholar]
- 82.Moreau APM, Willcox N, Brown MF. Immobilisation of spinal fractures in patients with ankylosing spondylitis: two case reports. Injury. 2003;34:372–373. doi: 10.1016/s0020-1383(01)00190-5. [DOI] [PubMed] [Google Scholar]
- 83.Murray GC, Persellin RH. Cervical fracture complicating ankylosing spondylitis. A report of eight cases and review of the literature. Am J Med. 1981;70:1033–1041. doi: 10.1016/0002-9343(81)90860-3. [DOI] [PubMed] [Google Scholar]
- 84.Neville AL, Brown CV, Weng J, et al. Obesity is an independent risk factor of mortality in severely injured blunt trauma patients. Arch Surg. 2004;139:983–987. doi: 10.1001/archsurg.139.9.983. [DOI] [PubMed] [Google Scholar]
- 85.Olerud C, Frost A, Bring J. Spinal fractures in patients with ankylosing spondylitis. Eur Spine J. 1996;5:51–55. doi: 10.1007/BF00307827. [DOI] [PubMed] [Google Scholar]
- 86.Oxford Centre for Evidence-based Medicine (2001). Levels of Evidence. [http://www.cebm.net/index.aspx?o=1025]
- 87.Ozgocmen S, Ardicoglu O. Odontoid fracture complicating ankylosing spondylitis. Spinal Cord. 2000;38:117–119. doi: 10.1038/sj.sc.3100926. [DOI] [PubMed] [Google Scholar]
- 88.Paley D, Schwartz M, Cooper P, et al. Fractures of the spine in diffuse idiopathic skeletal hyperostosis. Clin Orthop Relat Res. 1991;267:22–32. [PubMed] [Google Scholar]
- 89.Papadopoulos MC, Chakraborty A, Waldron G, et al. Lesson of the week: exacerbating cervical spine injury by applying a hard collar. BMJ. 1999;319:171–172. doi: 10.1136/bmj.319.7203.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pascal-Moussellard H, Drossard G, Cursolles JC, et al. Myelopathy by lesions of the craniocervical junction in a patient with forestier disease. Spine. 2006;31:E557–E560. doi: 10.1097/01.brs.0000225972.24608.be. [DOI] [PubMed] [Google Scholar]
- 91.Payer M. Surgical management of cervical fractures in ankylosing spondylitis using a combined posterior–anterior approach. J Clin Neurosci. 2006;13:73–77. doi: 10.1016/j.jocn.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 92.Peh WC. A 33-year-old man presented with progressive neck pain and a subjective sensation of neck instability. Diagnosis: type II dens fracture complicating ankylosing spondylitis. Australas Radiol. 2001;45:101–103. doi: 10.1046/j.1440-1673.2001.00884.x. [DOI] [PubMed] [Google Scholar]
- 93.Peh WCG, Ho EKW. Fracture of the odontoid peg in ankylosing spondylitis: case report. J Trauma. 1995;38:361–363. doi: 10.1097/00005373-199503000-00009. [DOI] [PubMed] [Google Scholar]
- 94.Podolsky SM, Hoffman JR, Pietrafesa CA. Neurologic complications following immobilization of cervical spine fracture in a patient with ankylosing spondylitis. Ann Emerg Med. 1983;12:578–580. doi: 10.1016/s0196-0644(83)80305-9. [DOI] [PubMed] [Google Scholar]
- 95.Pofahl WE, Pories WJ. Current status and future directions of geriatric general surgery. J Am Geriatr Soc. 2003;51:S351–S354. doi: 10.1046/j.1365-2389.2003.51347.x. [DOI] [PubMed] [Google Scholar]
- 96.Resnick D, Shaul SR, Robins JM. Diffuse idiopathic skeletal hyperostosis (DISH): Forestier’s disease with extraspinal manifestations. Radiology. 1975;115:513–524. doi: 10.1148/15.3.513. [DOI] [PubMed] [Google Scholar]
- 97.Roosen K, Wissing H, Grote W, et al. Operative stabilization of fractures in the cervical spine in Bechterew’s disease. Unfallchirurg. 1985;88:215–218. [PubMed] [Google Scholar]
- 98.Ruf M, Rehm S, Poeckler-Schoeniger C, et al. Iatrogenic fractures in ankylosing spondylitis - A report of two cases. Eur Spine J. 2006;15:100–104. doi: 10.1007/s00586-005-0973-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Samartzis D, Anderson DG, Shen FH. Multiple and simultaneous spine fractures in ankylosing spondylitis: case report. Spine. 2005;30:E711–E715. doi: 10.1097/01.brs.0000188272.19229.74. [DOI] [PubMed] [Google Scholar]
- 100.Savolaine ER, Ebraheim NA, Stitgen S, et al. Aortic rupture complicating a fracture of an ankylosed thoracic spine: a case report. Clin Orthop Relat Res. 1991;272:136–140. [PubMed] [Google Scholar]
- 101.Schaberg J. Aortic injury occurring after minor trauma in ankylosing spondylitis. J Vasc Surg. 1986;4:410–411. [PubMed] [Google Scholar]
- 102.Schroder J, Liljenqvist U, Greiner C, et al. Complications of halo treatment for cervical spine injuries in patients with ankylosing spondylitis—report of three cases. Arch Orthop Trauma Surg. 2003;123:112–114. doi: 10.1007/s00402-003-0488-x. [DOI] [PubMed] [Google Scholar]
- 103.Secin FP, Poggi EJ, Luzuriaga F, et al. Disabling injuries of the cervical spine in Argentine rugby over the last 20 years. Br J Sports Med. 1999;33:33–36. doi: 10.1136/bjsm.33.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sharma RR, Mahapatra A, Pawar SJ, et al. Spinal cord and cauda equina compression in ‘DISH’. Neurol India. 2001;49:148–152. [PubMed] [Google Scholar]
- 105.Shen FH, Samartzis D. Cervical spine fracture in the ankylosing spondylitis patient. J Am Coll Surg. 2005;200:632–633. doi: 10.1016/j.jamcollsurg.2004.07.036. [DOI] [PubMed] [Google Scholar]
- 106.Shen FH, Samartzis D. Successful nonoperative treatment of a three-column thoracic fracture in a patient with ankylosing spondylitis: existence and clinical significance of the fourth column of the spine. Spine. 2007;32:E423–E427. doi: 10.1097/BRS.0b013e318074d59f. [DOI] [PubMed] [Google Scholar]
- 107.Smyth S, Heron A. Diabetes and obesity: the twin epidemics. Nat Med. 2006;12:75–80. doi: 10.1038/nm0106-75. [DOI] [PubMed] [Google Scholar]
- 108.Sreedharan S, Li YH. Diffuse idiopathic skeletal hyperostosis with cervical spinal cord injury— a report of 3 cases and a literature review. Ann Acad Med Singapore. 2005;34:257–261. [PubMed] [Google Scholar]
- 109.Stechison MT, Tator CH. Cervical myelopathy in diffuse idiopathic skeletal hyperostosis. Case report. J Neurosurg. 1990;73:279–282. doi: 10.3171/jns.1990.73.2.0279. [DOI] [PubMed] [Google Scholar]
- 110.Straiton N. Fractures of the lower vertebral column in ankylosing spondylitis. Br J Clin Pract. 1987;41:933–934. [PubMed] [Google Scholar]
- 111.Strohm PC, Zwingmann J, Bley TA, et al. Injuries of the cervical spine with Forestier’s disease: problems in the diagnostic and surgical management. Unfallchirurg. 2006;109:905–909. doi: 10.1007/s00113-006-1114-5. [DOI] [PubMed] [Google Scholar]
- 112.Surin VV. Fractures of the cervical spine in patients with ankylosing spondylitis. Acta Orthop Scand. 1980;51:79–84. doi: 10.3109/17453678008990772. [DOI] [PubMed] [Google Scholar]
- 113.Taggard DA, Traynelis VC. Management of cervical spinal fractures in ankylosing spondylitis with posterior fixation. Spine. 2000;25:2035–2039. doi: 10.1097/00007632-200008150-00006. [DOI] [PubMed] [Google Scholar]
- 114.Tait TJ, Barlow G, Iveson JMI. Cervical spine fracture in ankylosing spondylitis: a case of ‘auto-fracture’. Br J Rheumatol. 1998;37:467–468. doi: 10.1093/rheumatology/37.4.467. [DOI] [PubMed] [Google Scholar]
- 115.Tashjian RZ, Majercik S, Biffl WL, et al. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma. 2006;60:199–203. doi: 10.1097/01.ta.0000197426.72261.17. [DOI] [PubMed] [Google Scholar]
- 116.Tetzlaff JE, Yoon HJ, Bell G. Massive bleeding during spine surgery in a patient with ankylosing spondylitis. Can J Anaesth. 1998;45:903–906. doi: 10.1007/BF03012228. [DOI] [PubMed] [Google Scholar]
- 117.Thorngren KG, Liedberg E, Aspelin P. Fractures of the thoracic and lumbar spine in ankylosing spondylitis. Arch Orthop Trauma Surg. 1981;98:101–107. doi: 10.1007/BF00460796. [DOI] [PubMed] [Google Scholar]
- 118.Thumbikat P, Hariharan RP, Ravichandran G, et al. Spinal cord injury in patients with ankylosing spondylitis: a 10-year review. Spine. 2007;32:2989–2995. doi: 10.1097/BRS.0b013e31815cddfc. [DOI] [PubMed] [Google Scholar]
- 119.Tico N, Ramon S, Garcia-Ortun F, et al. Traumatic spinal cord injury complicating ankylosing spondylitis. Spinal Cord. 1998;36:349–352. doi: 10.1038/sj.sc.3100619. [DOI] [PubMed] [Google Scholar]
- 120.Tiesenhausen K, Thalhammer M, Koch G, et al. Traumatic aortic rupture in ankylosing spondylitis—a lethal complication. Unfallchirurg. 2001;104:1101–1103. doi: 10.1007/s001130170025. [DOI] [PubMed] [Google Scholar]
- 121.Trent G, Armstrong GWD, O’Neil J. Thoracolumbar fractures in ankylosing spondylitis: high-risk injuries. Clin Orthop Relat Res. 1988;227:61–66. [PubMed] [Google Scholar]
- 122.Upadhyay SS, Ho EK, Hsu LC. Positioning for plain spinal radiography producing paraplegia in a patient with ankylosing spondylitis. Br J Radiol. 1991;64:549–551. doi: 10.1259/0007-1285-64-762-549. [DOI] [PubMed] [Google Scholar]
- 123.van der Linden S (1997) Ankylosing spondylitis. In: Kelley WN, Harris S, Ruddy S et al Textbook of Rheumatology, 5th edn. WB Saunders, Philadelphia, 2:969–982
- 124.Verlaan JJ, Diekerhof CH, Buskens E, et al. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine. 2004;29:803–814. doi: 10.1097/01.brs.0000116990.31984.a9. [DOI] [PubMed] [Google Scholar]
- 125.Vives MJ, Harris C, Reiter MF et al (2007) Use of stand-up magnetic resonance imaging for evaluation of a cervicothoracic injury in a patient with ankylosing spondylitis. Spine J [Epub ahead of print] [DOI] [PubMed]
- 126.Wade W, Saltzstein R, Maiman D. Spinal fractures complicating ankylosing spondylitis. Arch Phys Med Rehabil. 1989;70:398–401. [PubMed] [Google Scholar]
- 127.Weinfeld RM, Olson PN, Maki DD, et al. The prevalence of diffuse idiopathic skeletal hyperostosis (DISH) in two large American Midwest metropolitan hospital populations. Skeletal Radiol. 1997;26:222–225. doi: 10.1007/s002560050225. [DOI] [PubMed] [Google Scholar]
- 128.Whang PG, Goldberg G, Lawrence JP et al (2008) The management of spinal fractures in patients with ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis: a comparison of treatment methods and clinical outcomes. J Spinal Disord Tech (in press) [DOI] [PubMed]
- 129.Winkelstein BA, Myers BS. The biomechanics of cervical spine injury and implications for injury prevention. Med Sci Sports Exerc. 1997;29:S246–S255. doi: 10.1097/00005768-199707001-00007. [DOI] [PubMed] [Google Scholar]
- 130.Organization World Health. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. Tech Rep Ser. 2000;894:1–253. [PubMed] [Google Scholar]
- 131.Wrobel CJ, Meyer W. Diffuse idiopathic skeletal hyperostosis. J Neurosurg. 2000;93:341–342. doi: 10.3171/spi.2000.93.2.0341. [DOI] [PubMed] [Google Scholar]
- 132.Wu CT, Lee ST. Spinal epidural hematoma and ankylosing spondylitis: case report and review of the literature. J Trauma. 1998;44:558–561. doi: 10.1097/00005373-199803000-00029. [DOI] [PubMed] [Google Scholar]
- 133.Young JS, Cheshire JE, Pierce JA, et al. Cervical ankylosis with acute spinal cord injury. Paraplegia. 1977;15:133–146. doi: 10.1038/sc.1977.19. [DOI] [PubMed] [Google Scholar]