Abstract
Although there are several accepted methods of surgical treatment for single-level cervical radiculopathy, the choice depend on the surgeon’s preference. The techniques may vary in peri-operative morbidity, short- and long-term outcome, but no study so far has analyzed their cost-effectiveness. This study might give some insight in balancing cost and effectiveness and deciding the right technique. Sixty consecutive patients (15 each group), mean age 36 (range 24–76 years) with single-level cervical disc disease underwent surgical treatment with four different techniques in two centers over the period of 1999–2005. The four groups were—(1) plate and tricortical autograft, (2) plate, cage, and bone substitute, (3) cage only, and (4) disc arthroplasty. The data was collected prospectively according to our protocol and subsequently analyzed. The clinical outcome was assessed comparing visual analog scale (VAS) of neck pain and, short form 12 (SF12) questionnaire both pre- and postoperatively. The radiological assessment was done for fusion rate and postoperative related possible complications at 3 months, 6 months, 1 year, and final follow-up. The cost analysis was done calculating the operative time, hospital stay, implant cost together. The mean follow-up period was 31 months (range 28–43 months). The clinical outcome in terms of VAS of neck and arm pain and SF12 physical and mental score improvement (P = 0.001) were comparable with all four techniques. The radiological fusion rate was comparable to current available data. As the hospital stay was longer (average 5 days) with plate and autograft group, the total cost was maximum (average £2,920) with this group. There was satisfactory clinical and radiological outcome with all four techniques. Using the cage alone was the most cost-effective technique, but the disc arthroplasty was comparable to the use of cage and plate. Anterior cervical discectomy and fusion is an established surgical treatment for cervical radiculopathy. Single-level cervical radiculopathy was treated with four different techniques. The clinical outcome and cost-effectiveness were compared in this study.
Keywords: Cervical radiculopathy, ACDF, Disc arthroplasty, Clinical outcome, Cost-effectiveness
Introduction
Anterior cervical discectomy and fusion (ACDF) is an established procedure for surgical treatment of cervical radiculopathy and myelopathy secondary to anterior compression due to osteophyte or soft disc prolapse [29]. Cervical disc arthroplasty is a promising nonfusion alternative for the treatment of degenerative disc disease for cases of predominantly anterior compression of the cervical spinal cord and/or nerve roots [30].
A half-century has transpired since the initial descriptions of anterior cervical discectomy by Bailey and Badgley [4]. Cloward [7] modified the technique of Bailey and Badgley in 1953. Robinson and Smith [21] and Robinson et al. [22] described their experience with cervical disease in 1955. Although single-level ACDF has a high fusion rate by any technique, there is debate about the added advantage of plating for one-level treatment [1, 23]. On the other hand, recent papers have reported increased fusion rates with plating, even at one level, compared with autologous and allogeneic grafts without plating [15, 25]. Despite the differences in the reported fusion rates of these procedures, they seem to be similar in their effectiveness of symptomatic relief [15, 23]. Differences in their complication profile, fusion rate, and cost are the main distinguishing factors [31]. Cooper [9] and Sonntag [27] have advocated for cost-effectiveness analysis to help determine the appropriate procedure when a one-level ACDF is indicated. Based on the reported concerns of progressive adjacent segment degeneration and motion loss after ACDF, the option of disc arthroplasty is in practice with early promising results. Decision analysis and cost-effectiveness analysis are useful techniques for formalizing the decision-making process and combining cost and outcome data into a single model. These techniques are particularly useful when there are real choices among which a clearly superior option does not exist.
Our study describes the clinical outcome and cost-effectiveness of four techniques for single-level cervical radiculopathy—(1) plate and tricortical autograft, (2) cage, plate, and bone substitute, (3) cage only, and (4) disc arthroplasty.
Method and patients
Sixty consecutively treated patients (15 in each group) with cervical radiculopathy owing to single-level degenerative disease were recruited to the study over a 5-year period. They were identified as potential study candidates at the time of initial consultation with their surgeon and were considered eligible for the study if they (1) had symptomatic single-level cervical degenerative disc disease presenting with radiculopathy, (2) were at least 18 years old, and (3) after failure of an adequate trial of nonoperative treatment that consisted of rest, anti-inflammatory medication, traction, and physical therapy. All patients presented with preoperative plain anteroposterior and lateral X-rays, as well as magnetic resonance imaging to confirm their clinical diagnosis. Exclusion criteria consisted of: (1) symptomatic multi-level cervical degenerative disc disease, (2) extensive compressive pathology requiring substantial resection of adjacent vertebral bodies, thereby necessitating fusion with or without instrumentation, (3) primarily posterior degenerative changes and neural compromise, and (4) unrelated comorbidity requiring regular narcotic analgesic and/or nonsteroidal anti-inflammatory treatment.
They were operated in two centers and by two surgeons over the period 1999–2005. The data was collected prospectively. The patients were systemically allocated to one of the four techniques. Allocation was based on surgeon’s preference. Although four groups were not randomized, there was no significant difference in age, sex (M:F) distribution and level of involvement between the groups (Table 1). There were 36 males and 24 females with mean age of 36 years (range 24–76 years). Standard right-sided anterior approach through a transverse incision was used for discectomy and fusion or disc arthroplasty in all the patients. We used Brantigan cage (DePuy) in the cage only group, standard AO plate, poly-ether-ether-ketone cage and fine particles allograft mixed with blood and marrow aspirated from the iliac crest in the cage and plate group and Bryan disc in the disc arthroplasty group. In Group 1 (plate and autograft) tricortical bone graft was harvested from the iliac crest of the same side of the operation in neck. The most common operated disc level was C5/6 (60%) and C6/7 (30%) of the enrolled patients with one-level procedure. Postoperative follow-up visits were scheduled for 6 weeks, 3 months, 6 months, 1 year, and 2 years after the index procedure. Detailed motor and sensory examination was done by the operating surgeons both pre- and postoperatively in every follow-up visit. Patients underwent routine radiographic investigations of their cervical spine, including plain lateral, anteroposterior, and flexion/extension X-rays at months 3 and 6 and years 1 and 2 postoperatively to determine fusion status and alignment or other information related with the graft or implant. The clinical outcome was assessed using the short form 12 (SF12) and visual analog score of pain in neck and arm pre- and postoperatively. The average prospective follow-up period was 31 months (range 28–43 months).
Table 1.
Demography of patients in different groups and level of cervical pathology
| M:F | Age (years) | Levels involved | |
|---|---|---|---|
| Group 1 (plate + autograft) | 10:5 | 35 (range 30–75) | C5/6 (9) |
| C6/7 (4) | |||
| C4/5 (2) | |||
| Group 2 (cage + plate + bone graft) | 9:6 | 37 (range 24–72) | C5/6 (10) |
| C6/7 (3) | |||
| C4/5 (2) | |||
| Group 3 (cage) | 8:7 | 38 (range 34–76) | C5/6 (8) |
| C6/7 (6) | |||
| C3/4 (1) | |||
| Group 4 (disc arthroplasty) | 9:6 | 34 (range 30–68) | C5/6 (9) |
| C6/7 (5) | |||
| C4/5 (1) |
The cost analysis was based on operating time, hospital stay, and prosthesis cost. We used data published in the website of the Department of Health, UK, Cost Manual 2005. The costs include implant cost (cage, plate, bone substitute, artificial disc), theater time (£420 per hour; Cost Manual DoH 2005), hospital bed cost (£300 per day). The cost of the inpatient and out patient physiotherapy was excluded as all the patients received the similar treatment. As none of our patients needed reoperation during the follow-up period, any possible hardware complication was not assigned to the cost. As the patients were from different socioeconomic background, the accurate estimation of work loss related cost was not possible. Hence this was excluded from the cost analysis.
We compared the blood loss, complications (including donor site morbidity in Group 2), clinical and radiological outcome with all four techniques.
All data were analyzed using SPSS version 11.5 for Windows (SPSS, Inc, Chicago, IL, USA). Two-tailed testing was performed with statistical significance accepted at a P-value of <0.05.
Results
The average operative time for plating and tricortical autograft was 160 min (120–190 min), for plate, cage, and bone substitute was 100 min (range 90–110 min), for cage only was 90 min (range 75–110 min), and for disc arthroplasty 105 min (range 90–120 min). The operative time is calculated from the point of positioning of the patient to the final wound closure. There was minimum blood loss (<50 ml) in all the groups except plate and autograft group (mean blood loss 100 ml). The average length of stay in the hospital was 5 days (3–10 days) in Group 1, 2.7 days (2–4 days) in Group 2, 2.5 days (2–4 days) in Group 3, and 2 days (1.5–4 days) in Group 4.
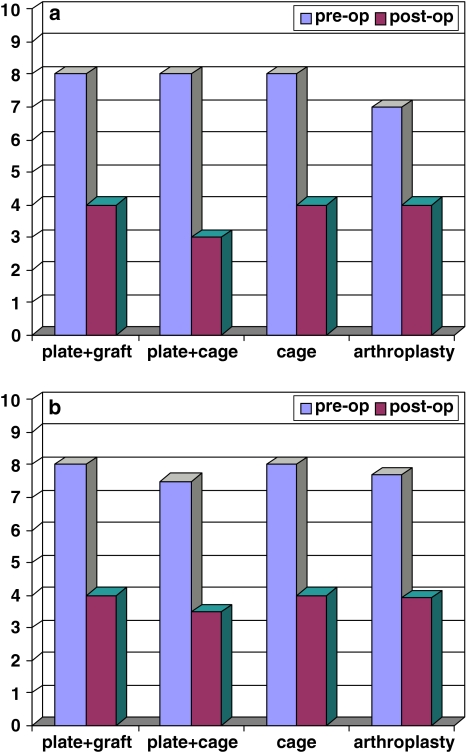
All four surgical techniques resulted in reduction of overall neck as well as arm pain (Fig. 1a, b). The level of reduction in pain intensity was comparable in all four groups and remained significant (P < 0.04) even at the final follow-up.
Fig. 1.
a Mean VAS neck pain before and after surgery in four different group. b Mean VAS arm pain before and after surgery in four different groups
Comparison of pre- and postoperative SF12 scores demonstrated a dramatic and comparable improvement in physical and mental subscores in all the groups. The results are summarized in the Table 2.
Table 2.
The pre- and postoperative SF12 physical and mental scores in four groups
| SF12 physical score | SF12 mental score | |||
|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | |
| Group 1 (plate + autograft) | 10 (8–14) | 16 (14–20), P < 0.003 | 15 (13–16) | 24 (21–27), P = 0.002 |
| Group 2 (cage + plate + bone graft) | 12 (10–15) | 18 (17–20), P < 0.005 | 13 (11–15) | 25 (23–27), P < 0.001 |
| Group 3 (cage) | 8 (6–10) | 14.5 (11–20), P < 0.003 | 14 (12–15) | 23 (21–26), P < 0.003 |
| Group 4 (disc arthroplasty) | 10 (7–12) | 16 (15–20), P < 0.002 | 15 (12–17) | 24 (22–26), P < 0.002 |
In the fusion groups based on the plane X-ray including flexion and extension views there was no evidence of pseudoarthrosis or movement at the operated levels. At 6 months, the fusion rate demonstrated on X-ray was 80% in the plate and autograft group, 84% in plate and cage group, and 78% in cage only group. At 1 year, the fusion rate was 100% in all three fusion groups. None of them required any revision surgery. None had any neurological complication.
Complication
In plate and autograft group 3 out of 15 patients (20%) had donor site morbidity—one persistent pain, one developed numbness around the site, and one superficial infection which resulted their longer hospital stay (longest stay—22 days).
In cage only group, one patient (6.6%) had asymptomatic cage subsidence which was found on X-ray at 18 months, and it did not progress further at the final follow-up at 30 months.
In the disc arthroplasty group, two patients (13%) had Grade II heterotopic ossification (HO) according to the McAfee et al. [20] modification of HO grading.
Cost analysis
In the plate and autograft group (Group 1) the average total cost incurred was £2,920 (theater—£1,120, hospital stay—£1,599, plate—£300).
In the plate, cage, and bone substitute group (Group 2) the average total cost incurred was £2,520 (theater—£700, hospital stay—£810, plate—£300, cage—£450, bone substitute—£210).
In the cage only group (Group 3) the average total cost was £1,930 (theater—£630, hospital stay—£750, cage—£550).
In the disc arthroplasty group (Group 4) the average total cost was £2,435 (theater—£735, hospital stay—£600, and disc—£1,100).
The cost of the implants and hardware was calculated as an average of three commonly used implants in the National Health Service in England. The cost of work loss was not included as patients were from different socioeconomic background which made it impossible to do accurate estimation (Table 3).
Table 3.
The operative time, blood loss, length of inpatient stay and the cost incurred in different techniques
| Groups | Operative time (min) | Blood loss (ml) | Length of inpatient stay (days) | Cost without implants | Total cost |
|---|---|---|---|---|---|
| Plate + graft | 160 (120–190) | 100 | 5 (3–10) | £2,620 | £2,920 |
| Plate + cage + bone substitute | 100 (90–110) | <50 | 2.7 (2–4) | £1,510 | £2,520 |
| Cage | 90 (75–110) | <50 | 2.5 (2–4) | £1,380 | £1,930 |
| Disc arthroplasty | 105 (90–120) | <50 | 2 (1.5–4) | £1,335 | £2,435 |
Discussion
The ACDF is an effective procedure for treating cervical degenerative disease. There is no compelling evidence in the literature that one procedure is significantly superior to another in term of fusion rate or clinical outcome.
In most studies published in the literature the fusion rate with autograft (74–97%), allograft (54–90%), cage (93–100%), and plating (94–100%) is comparable [2, 5, 6, 10, 12, 14, 16, 19, 25]. Although the clinical results have been described as similar there are certain advantages and disadvantages of one procedure over another. The fusion time is significantly shorter in the autograft group [16]. The donor site morbidity (5.8–37%) including hematoma, infection, numbness, pain resulting in prolonged hospital stay could be a disadvantage for autograft [3, 11, 26]. Cho et al. [6] and Vavruch et al. [28] reported that cage could provide solid fusion, increased cervical lordosis, increased disc height with few complications. With plating the rate of solid fusion increases, graft complications such as collapse, subsidence, extrusion decreases, cervical spinal sagittal alignment is well maintained and also the need for external immobilization after the surgery is minimized [8, 13]. Cervical disc arthroplasty is emerging as a viable alternative to fusion in the treatment of cervical disc disease. Disc arthroplasty also restores/maintains segmental cervical motion and thus may decrease the incidence of adjacent segment degeneration that plagues spinal fusion surgery [22]. As reported in the literature [17] HO is one of the known complications of disc arthroplasty which affects the segmental motion of the operated level. Our rate of HO (13%) was comparable to the reported incidence (17.8%) in the literature [17].
There is no large published study on comparing the clinical outcome and cost-effectiveness of these four techniques for single-level cervical radiculopathy. Our study showed comparable good radiological and clinical outcome in terms of improvement of neck and arm pain and physical and mental health score with SF12 questionnaire in all the groups. The complication rate was minimal and comparable with the published data.
Although previously published analysis of the costs and effectiveness of ACDF included lost wages in the costs of surgery, there is no common consensus among cost-effectiveness experts whether lost productivity should be included in formal cost analysis. The recommendation of the Panel on Cost-Effectiveness in Health and Medicine is not to include these costs in the numerator in the base case analysis [18]. Cost-effectiveness analysis is not a tool to determine the “best” treatment for any particular disease or pathologic entity. It is an analytical technique of combining many variables in a single model that allows systematic testing of the effect of each variable on outcome. In all four groups with single-level cervical radiculopathy, fusion factors, short-term risks, costs, graft and hardware complications, outcome, and long-term reoperation rates must be considered in trying to determine the relative cost-effectiveness of the alternative procedures.
If we exclude the cost of implants and hardware the total cost in all the groups except plate and autograft group is comparable. Excluding implants, the average cost was £1,510 in plate and cage group, £1,380 in cage only, and £1,335 in disc arthroplasty group. On the other hand same cost was much higher (£2,620) in the plate and autograft group owing to the local donor site complications, more pain and longer inpatient hospital stay. The documented donor site complications like pain, infection, hematoma formation, and reoperation rate varies from 3 to 26% [24, 26]. Although clinical outcome with plating and tricortical iliac crest graft is good, donor site complications should be taken into consideration.
The cost analysis was based on data from two centers only and may therefore not be the representative of costs at other hospitals. Post-discharge costs, outpatient physiotherapy, and home health aides were not included in the total cost for any particular procedure. Even if the care was provided by the family member the resource utilization ideally should be estimated and included to the total cost of the procedure. If all these are taken into consideration the total cost of the procedures would be expected to increase. This study provides evidence on degree of clinical improvement and analysis of short-term costs only.
Conclusion
In this observational study we found that clinical outcome was satisfactory and comparable with all the techniques. Using cage alone for single-level ACDF was the cheapest and therefore most cost-effective. The cost of disc arthroplasty was comparable to cage and plate. The benefit with cage only group was largely driven by shorter operative time and shorter hospital stay whereas harvesting tricortical bone graft lengthened the operative time and the donor site morbidity resulted in longer hospital stay in plate and autograft group and hence the total cost incurred was higher.
The limitation of our study was lack of randomization and small number (n = 15) of patients in each group. Nevertheless this study will give some insight to the surgeons to help them choose the most appropriate technique for single-level ACDF. Further prospective randomized study involving a bigger number of patients with particular attention to the long-term outcome and cost, is needed to determine more accurately their relative cost-effectiveness.
Contributor Information
Arup K. Bhadra, Email: arupbhadra@yahoo.com
A. S. Raman, Email: Siva.raman@nhs.net
Adrian T. H. Casey, Email: athcasey@doctors.org.uk
R. J. Crawford, Email: rwjcrawford@doctors.org.uk
References
- 1.Abraham DJ, Herkowitz HN. Indications and trends in use of cervical spine fusions. Orthop Clin North Am. 1998;29:731–744. doi: 10.1016/S0030-5898(05)70044-4. [DOI] [PubMed] [Google Scholar]
- 2.An HS, Simpson JM, Glover JM, Stephany J. Comparison between allograft plus demineralised bone matrix versus auto graft in anterior cervical fusion. Spine. 1995;20:2211–2216. [PubMed] [Google Scholar]
- 3.Arrington ED, Smith WJ, Chambers HG, et al. Complications of iliac crest bone graft harvesting. Clin Orthop Relat Res. 1996;329:300–309. doi: 10.1097/00003086-199608000-00037. [DOI] [PubMed] [Google Scholar]
- 4.Bailey RW, Badgley CE. Stabilisation of cervical spine by anterior fusion. Am J Orthop. 1960;42:565–594. [PubMed] [Google Scholar]
- 5.Bishop RC, Moore KA, Hadley MN. Anterior cervical interbody fusion using autogenic and allogenic bone graft substrate: a prospective comparative analysis. J Neurosurg. 1996;85:206–210. doi: 10.3171/jns.1996.85.2.0206. [DOI] [PubMed] [Google Scholar]
- 6.Cho DY, Liau WR, Lee WY et al (2002) Preliminary experience using polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgery 51:1343–1350 Erratum in Neurosurgery 52:693, 2003. doi:10.1097/00006123-200212000-00003 [PubMed]
- 7.Cloward RB. The anterior approach for the removal of ruptured cervical disks. J Neurosurg. 1958;15:602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 8.Connolly PJ, Esses SI, Kostuik JP. Anterior cervical fusion: outcome analysis of patients fused with and without anterior cervical plate. J Spinal Disord. 1996;9:202–206. [PubMed] [Google Scholar]
- 9.Cooper PR. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery. 2002;50:237–238. doi: 10.1097/00006123-200202000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Emery SE, Bolesta MJ, Banks MA, Jones PK. Robinson anterior cervical fusion. Spine. 1994;19:660–663. doi: 10.1097/00007632-199403001-00004. [DOI] [PubMed] [Google Scholar]
- 11.Goulet JA, Senunas LE, DeSilva GL, et al. Autogenous iliac crest bone graft. Clin Orthop Relat Res. 1997;339:76–81. doi: 10.1097/00003086-199706000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Hacker RJ, Cauthen JC, Gilbert TJ, Griffith SL. A prospective randomized multicenter clinical evaluation of an anterior cervical fusion cage. Spine. 2000;25:2646–2655. doi: 10.1097/00007632-200010150-00017. [DOI] [PubMed] [Google Scholar]
- 13.Heidecke V, Rainov NG, Berkert W. Anterior cervical fusion with the Orion locking plate system. Spine. 1998;23:1796–1802. doi: 10.1097/00007632-199808150-00014. [DOI] [PubMed] [Google Scholar]
- 14.Heidecke V, Rainov NG, Marx T, et al. Outcome in Cloward anterior fusion for degenerative cervical spine disease. Acta Neurochir (Wien) 2000;142:283–291. doi: 10.1007/s007010050037. [DOI] [PubMed] [Google Scholar]
- 15.Kaiser MG, Haid RWJ, Subach BR, et al. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery. 2002;50:229–238. doi: 10.1097/00006123-200202000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Kao FC, Niu CC, Chen LH, et al. Maintenance of interbody space in one and two level anterior cervical interbody fusion: comparison of effectiveness of autograft, allograft and cage. Clin Orthop Relat Res. 2005;430:108–116. doi: 10.1097/01.blo.0000142626.90278.9e. [DOI] [PubMed] [Google Scholar]
- 17.Leung C, Casey AT, Goffin J, et al. Clinical significance of heterotopic ossification in cervical disc replacement: a prospective multicenter clinical trial. Neurosurgery. 2005;57(4):759–763. doi: 10.1227/01.NEU.0000175856.31210.58. [DOI] [PubMed] [Google Scholar]
- 18.Luce BR, Manning WG, Siegel JE, et al. et al. Estimating costs in cost-effectiveness analysis. In: Gold MR, Russell LB, Seigel JE, et al.et al., editors. Cost-effectiveness in health and medicine. New York: Oxford University Press; 1996. pp. 176–213. [Google Scholar]
- 19.Majd ME, Vadhva M, Holt RT. Anterior cervical reconstruction using titanium cages with anterior plating. Spine. 1999;24:852–859. doi: 10.1097/00007632-199908010-00016. [DOI] [PubMed] [Google Scholar]
- 20.McAfee PC, Cunningham BW, Devine J, et al. Classification of heterotopic ossification (HO) in artificial disk replacement. J Spinal Disord Tech. 2003;16:384–389. doi: 10.1097/00024720-200308000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Robinson RA, Smith GW. Anterior lateral disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp. 1955;96:223–224. [Google Scholar]
- 22.Robinson RA, Walker AE, Ferlic DC, et al. The results of interbody fusion of the cervical spine. J Bone Joint Surg. 1962;44A:1569–1587. [Google Scholar]
- 23.Savolainen S, Rinne J, Hernesniemi J. A prospective randomized study of anterior single-level cervical disc operations with long-term follow-up: surgical fusion is unnecessary. Neurosurgery. 1998;43:51–55. doi: 10.1097/00006123-199807000-00032. [DOI] [PubMed] [Google Scholar]
- 24.Schnee CL, Freese A, Weil RJ, et al. Analysis of harvest morbidity and radiographic outcome using autograft for anterior cervical fusion. Spine. 1997;22:2222–2227. doi: 10.1097/00007632-199710010-00005. [DOI] [PubMed] [Google Scholar]
- 25.Shapiro S, Connolly P, Donaldson J, et al. Cadaveric fibula, locking plate and allogenic bone matrix for anterior cervical fusion after cervical discectomy for radiculopathy or myelopathy. J Neurosurg. 2001;95(1 Suppl):43–50. doi: 10.3171/spi.2001.95.1.0043. [DOI] [PubMed] [Google Scholar]
- 26.Silber JS, Anderson DG, Daffner SD, et al. Donor site morbidity after anterior iliac crest bone harvest for single level anterior cervical discectomy and fusion. Spine. 2003;28(2):134–139. doi: 10.1097/00007632-200301150-00008. [DOI] [PubMed] [Google Scholar]
- 27.Sonntag VKH. A prospective randomized study of anterior single-level cervical disc operations with long-term follow-up: surgical fusion is unnecessary. Neurosurgery. 1998;43:55. doi: 10.1097/00006123-199807000-00033. [DOI] [PubMed] [Google Scholar]
- 28.Vavruch L, Hedlund R, Javdi D, et al. A prospective randomized comparison between the Cloward procedure and a carbon fibre cage in the cervical spine. A clinical and radiologic study. Spine. 2002;27:1694–1701. doi: 10.1097/00007632-200208150-00003. [DOI] [PubMed] [Google Scholar]
- 29.Wang M, Leung C, Casey ATH. Cervical arthroplasty with the Bryan disc. Neurosurgery. 2005;56(Suppl 1):58–65. doi: 10.1227/01.NEU.0000153216.68321.C2. [DOI] [PubMed] [Google Scholar]
- 30.Yue WM, Bronder W, Highland TR. Long term results after anterior cervical discectomy and fusion with allograft and plating: 5–11 year radiologic and clinical follow up study. Spine. 2005;30(19):2138–2144. doi: 10.1097/01.brs.0000180479.63092.17. [DOI] [PubMed] [Google Scholar]
- 31.Zdeblick TA, Ducker TB. The use of freeze-dried allograft bone for anterior cervical fusions. Spine. 1991;16:726–729. doi: 10.1097/00007632-199107000-00006. [DOI] [PubMed] [Google Scholar]