Abstract
Although recognized as an important aspect in the management of spondylolisthesis, there is no consensus on the most reliable and optimal measure of lumbosacral kyphosis (LSK). Using a custom computer software, four raters evaluated 60 standing lateral radiographs of the lumbosacral spine during two sessions at a 1-week interval. The sample size consisted of 20 normal, 20 low and 20 high grade spondylolisthetic subjects. Six parameters were included for analysis: Boxall’s slip angle, Dubousset’s lumbosacral angle (LSA), the Spinal Deformity Study Group’s (SDSG) LSA, dysplastic SDSG LSA, sagittal rotation (SR), kyphotic Cobb angle (k-Cobb). Intra- and inter-rater reliability for all parameters was assessed using intra-class correlation coefficients (ICC). Correlations between parameters and slip percentage were evaluated with Pearson coefficients. The intra-rater ICC’s for all the parameters ranged between 0.81 and 0.97 and the inter-rater ICC’s were between 0.74 and 0.98. All parameters except sagittal rotation showed a medium to large correlation with slip percentage. Dubousset’s LSA and the k-Cobb showed the largest correlations (r = −0.78 and r = −0.50, respectively). SR was associated with the weakest correlation (r = −0.10). All other parameters had medium correlations with percent slip (r = 0.31–0.43). All measurement techniques provided excellent inter- and intra-rater reliability. Dubousset’s LSA showed the strongest correlation with slip grade. This parameter can be used in the clinical setting with PACS software capabilities to assess LSK. A computer-assisted technique is recommended in order to increase the reliability of the measurement of LSK in spondylolisthesis.
Keywords: Lumbosacral kyphosis, Reliability, Radiographic measurements, Spine, Spondylolisthesis
Introduction
In spondylolisthesis, there are two components involved in the underlying deformity: translational and angular [1, 4, 5, 13, 23, 26]. In translational deformity, the degree of slip can be expressed as grades as described by Meyerding [22], where the superior endplate of S1 is divided into quarters, or as a percentage as described by the modified Taillard [4] method, where a ratio is measured between the distance from two tangent lines to the posterior borders of S1 and L5 and the anteroposterior diameter of L5. In contrast, there are many more parameters to assess the angular deformity or lumbosacral kyphosis (LSK) [2, 4, 8, 13, 23, 26, 29, 30].
Normally, the junction between the fifth lumbar and the first sacral vertebra is lordotic [16]. However, as the degree of slip progresses to higher grades, this relationship tends to become kyphotic in nature [23]. Some authors suggest that measuring the lumbosacral kyphosis is important in determining risk of progression [1, 4, 8, 13, 19, 23, 26]. However, there is no strong data in the literature supporting this assumption. In addition, other authors suggest that correction of LSK is the most important aspect in the surgical management of spondylolisthesis, rather than the correction of the translational component of the deformity, as this restores global spinal balance, enhances the biomechanics of fusion, and can be protective against L5 nerve root stretch [4, 6, 8, 14, 16, 17, 19, 21, 25]. However, other authors have failed to show a correlation neither between LSK parameters and surgical outcome [11, 24] nor between LSK and risk of progression or need for future surgery [10]. In addition, despite the multitude of LSK parameters, there is no wide acceptance of a single measure, mainly because little is known about the reliability of these measures.
Therefore, before one can make conclusions on the predictive value of these parameters, it is important that their intra- and inter-rater reliability be determined. The objective of this study was to determine the intra- and inter-rater reliability of six of the most commonly employed parameters of LSK. In addition, their correlation to slip percentage was also evaluated.
Materials and methods
The study design is based on the recommendations made by Harrison [12]. These recommendations are aimed at standardizing reliability assessment of radiographic measurements.
The database of all patients with developmental isthmic spondylolisthesis seen at the spine clinic of a pediatric hospital from 1993 to December 2005 was searched. To be considered in the study, a standard lateral standing radiograph of the spine had to be available. Radiology technicians followed standard protocol to obtain this radiograph. This included a 30 × 90-cm left-to-right cassette of the spine and pelvis with the subject in a comfortable standing position, the knees fully extended, and the upper extremities flexed at the elbow with the fists resting on the clavicles [9, 15].
If a subject was operated for spondylolisthesis, the preoperative film was chosen. The films were assessed by a single observer to determine percent slip using the modified Taillard method [4]. Slips less than 50% were considered low grade and slips of 50% or more were considered high grade. Twenty subjects in each of these two groups were selected randomly from the database. Similarly, a group of 20 control subjects with available standing lateral spine radiographs were selected randomly from the hospital’s main radiograph database of normal subjects. These subjects consulted at the spine clinic for screening of spinal deformity, but the clinical and radiological examination failed to demonstrate any evidence of spinal deformity. Thus, the final study sample consisted of radiographic images from 20 normal, 20 low and 20 high grade spondylolisthetic subjects. All films were saved in digital format.
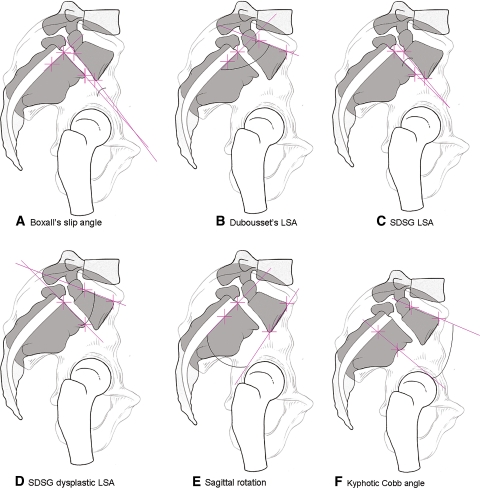
Four raters consisting of two orthopedic residents and two spine surgeons evaluated all the images at two different sessions at a 1-week interval using a custom computer software. This software was designed by an independent programmer to generate six LSK parameters from a series of landmarks identified by the raters on a computer monitor. The eight landmarks identified by the four raters on the lateral radiographs were the four corners of the fifth lumbar and first sacral vertebral bodies. From these points, the software was able to automatically compute the following six parameters (Fig. 1):
Boxall’s slip angle (BSA): the angle subtended by the inferior end plate of L5 with a line perpendicular to the posterior aspect of S1 [4].
Dubousset’s lumbosacral angle (Dub-LSA): the angle subtended by the superior end plate of L5 with the posterior aspect of S1 [8].
The Spinal Deformity Study Group’s lumbosacral angle (SDSG LSA): the angle subtended by the inferior end plate of L5 with the superior end plate of S1 [3].
SDSG dysplastic angle (dys-SDSG): the angle subtended by the superior end plate of L5 with the superior end plate of S1 [3].
Sagittal rotation (SR): the angle subtended by the anterior border of L5 with the posterior border of S1 [29].
Kyphotic Cobb angle (k-Cobb): the angle subtended by the superior end plate of L5 and the inferior end plate S1 [2].
Fig. 1.
The six radiographic parameters of LSK that were evaluated (see text for details.) a Boxall’s slip angle; b Dubousset’s lumbosacral angle, LSA; c Spinal Deformity Study Group’s, SDSG LSA; d SDSG dysplastic LSA; e Sagittal rotation; f kyphotic Cobb angle
Statistical analysis was performed by a biostatistician (PhDx Inc., Albuquerque, NM). Descriptive statistics were performed for all data. Intra-class correlation coefficients (ICC’s) with the associated 95 percent confidence intervals were employed to assess the inter- and intra-rater reliability. The inter-rater ICC was calculated from the data of the first acquisition session only. The intra-observer ICC was calculated for each observer from the data of both acquisition sessions. The ICC’s were based on a two-way random effects model with absolute agreement. The strength of the reliability values was assessed according to the recommendations made by Landis and Koch [18]: 0–0.20 slight agreement, 0.21–0.40 fair agreement, 0.41–0.60 moderate agreement, 0.61–0.80 substantial agreement, 0.81–1.00 almost perfect agreement. The relationship between the parameters and the slip percentage was assessed using the Pearson correlation coefficient and was interpreted according to the recommendations made by Cohen et al. [7]. A small correlation was between ±0.01–0.29; a medium correlation was between ±0.30–0.49, and a large correlation was between ±0.50–1.00. The level of significance was set at 0.05. Baseline characteristics of the subjects are given in Table 1.
Table 1.
Baseline information of the 60 selected subjects
| Normals (n = 20) | Low grade (n = 20) | High grade (n = 20) | ANOVA | |
|---|---|---|---|---|
| Age average (SD) years | 13.8 (2.0) | 12.6 (3.6) | 14.8 (2.9) | 0.07 |
| Males/females (number) | 4/16 | 7/13 | 5/15 | – |
| Avg slip % (SD) | – | 29.1 (8.5) | 71.7 (16.3) | – |
Results
There was no statistically significant difference in subject’s age among the three groups (Table 1). The different LSK angles as computed by the computer software are given in Table 2. Of the parameters measured, only Dub-LSA and k-Cobb showed a clear gradation along the spectrum of normal to low and high grade spondylolisthetic subjects. The other parameters showed no such clear gradation. The greatest change in values was seen when passing from a low grade to a high grade spondylolisthetic group.
Table 2.
Average LSK angles (all raters)
| Parameter | Controls (n = 20) Angle (°) (SD) |
Low grade (n = 20) Angle (°) (SD) |
High grade (n = 20) Angle (°) (SD) |
|---|---|---|---|
| Boxall’s slip angle | 20.8 (8.2) | 15.1 (8.1) | 39.7 (18.8) |
| Dubousset’s LSA | 119.0 (8.3) | 110.3 (13.3) | 71.0 (15.9) |
| SDSG LSA | 13.6 (6.4) | 13.7 (6.3) | 30.1 (20.2) |
| SDSG-dys LSA | 21.7 (6.3) | 21.7 (8.2) | 14.0 (13.9) |
| Sagittal rotation | 28.1 (7.5) | 21.7 (7.5) | 26.1 (15.8) |
| Kyphotic Cobb | 34.8 (9.9) | 27.9 (10.5) | 18.2 (15.1) |
The intra-rater ICC was slightly better than the inter-rater ICC. Both spondylolisthetic groups showed almost perfect agreement for both intra- and inter-rater ICC for all parameters, based on the criteria of Landis and Koch [18]. In addition, it was observed that one subject in the normal group had a transitional vertebra. One of the raters identified a different set of points during the two sessions such that in the first data acquisition session the four corners of L5 and S1 were chosen and in the second session the four corners of S1 and S2 were chosen. Consequently, the value of intra- and inter-observer ICC for the normal group was consistently lower than the spondylolisthetic groups except for the SDSG LSA (Table 3). It was decided that the statistical analysis include this error in order to reflect the potential mistakes that can occur with the misidentification of the vertebral level.
Table 3.
Intra- and inter- observer reliability
| Parameter | Intra-observer ICC (95% CI) | Inter-observer ICC (95% CI) |
|---|---|---|
| Boxall’s slip angle | High grade: 0.96 (0.93–0.97) | High grade: 0.94 (0.92–0.96) |
| Low grade: 0.95 (0.92–0.96) | Low grade: 0.93 (0.90–0.95) | |
| Normal: 0.89 (0.84–0.93) | Normal: 0.87 (0.81–0.90) | |
| Dubousset’s LSA | High grade: 0.97 (0.95–0.98) | High grade: 0.95 (0.92–0.96) |
| Low grade: 0.97 (0.96–0.98) | Low grade: 0.98 (0.97–0.98) | |
| Normal: 0.91 (0.87–0.94) | Normal: 0.91 (0.87–0.94) | |
| SDSG LSA | High grade: 0.96 (0.93–0.97) | High grade: 0.93 (0.90–0.95) |
| Low grade: 0.87 (0.81–0.92) | Low grade: 0.84 (0.77–0.88) | |
| Normal: 0.89 (0.80–0.93) | Normal: 0.84 (0.78–0.89) | |
| SDSG-dys LSA | High grade: 0.94 (0.91–0.96) | High grade: 0.88 (0.83–0.91) |
| Low grade: 0.92 (0.88–0.95) | Low grade: 0.89 (0.85–0.92) | |
| Normal: 0.90 (0.85–0.93) | Normal 0.87 (0.82–0.91) | |
| Sagittal rotation | High grade: 0.96 (0.94–0.97) | High grade: 0.93 (0.90–0.95) |
| Low grade: 0.90 (0.85–0.93) | Low grade: 0.87 (0.82–0.91) | |
| Normal: 0.81 (0.74–0.88) | Normal: 0.74 (0.65–0.82) | |
| Kyphotic Cobb | High grade: 0.94 (0.91–0.96) | High grade: 0.91 (0.87–0.93) |
| Low grade: 0.94 (0.94–0.96) | Low grade: 0.90 (0.86–0.93) | |
| Normal: 0.84 (0.76–0.89) | Normal: 0.84 (0.78–0.89) |
Pearson’s correlations between slip percentage and LSK parameters were all statistically significant, except for SR. They ranged from −0.1 for the SR parameter to −0.78 for Dubousset’s LSA. Only Dubousset’s LSA and the k-Cobb were in the large correlation category while SR had a small correlation with slip percentage. All other parameters were in the medium correlation category (Table 4).
Table 4.
Pearson’s correlations between LSK parameters and percent slip
| Boxall slip angle | Dub LSA | SDSG LSA | Dys SDSG | SR | k-Cobb | |
|---|---|---|---|---|---|---|
| Pearson | 0.43 | −0.78 | 0.41 | −0.31 | −0.10 | −0.50 |
| P value | 2.5 × 10−12 | 3.6 × 10−50 | 5.0 × 10−11 | 9.7 × 10−07 | 0.11 | 1.7 × 10−16 |
Discussion
This is the first study that specifically compares measurements of LSK with cohorts of normal as well as low and high grade spondylolisthetic groups. Timon et al. [27] has previously reported on the reliability of four measurements of LSK (BSA, Dub-LSA, SR, k-Cobb). However, they had a sample size of 30 subjects with 2/3 assigned a Meyerding’s grade 0 or 1 such that it is not known if their results also apply to high grade spondylolisthesis. In addition, the two parameters proposed by the SDSG (SDSG LSA and dys-SDSG) were not evaluated in the study by Timon et al. [27].
The inter-rater reliability was less in the study by Timon et al. [27] with a range from slight to moderate agreement as compared to substantial to almost perfect agreement in the present study. This could be explained by the use of high quality digital radiographs, and a computer-assisted method in the current study. Interestingly, Timon et al. [27] found that Dubousset’s LSA had the worst inter-rater reliability. In contrast, in the present study, Dubousset’s LSA had the best inter-rater reliability by a small margin. This can be explained by extrapolating a straight line from the curved posterior surface of the sacrum in the study by Timon et al. [27], while specifically identifying the posterior border of S1 in the present study. In addition, Dubousset’s LSA possessed the best correlation with slip percentage at −0.78 thus suggesting that progression of spondylolisthesis tends to be associated with worsening of Dubousset’s LSA. We, therefore, recommend the use of the posterior border of S1 as the landmark to measure Dubousset’s LSA.
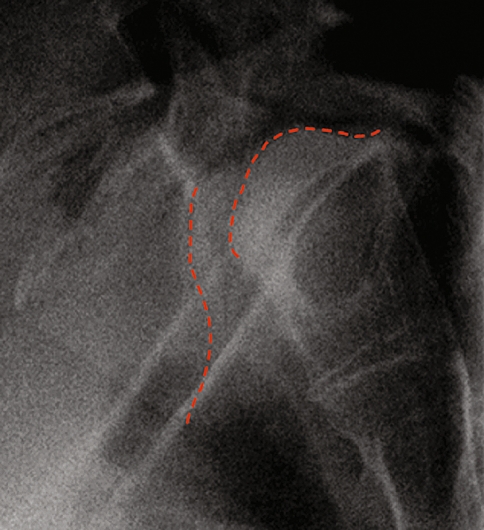
With progression of slippage, the inferior endplate of L5 tends to become dysplastic [19, 28] and the L5 vertebral body may adopt a trapezoidal shape [31]. Moreover, remodeling of the S1 endplate can occur and is referred to as sacral doming or rounding [20, 31] (Fig. 2). These changes can make the identification of the inferior endplate of L5 and superior endplate of S1 quite difficult. The k-Cobb and Dubousset’s LSA are not subtended by lines drawn through these dysplastic changes which may explain why they had the best correlation with slip percentage. However, the intra- and inter-rater reliability was not adversely affected. In contrast, the BSA, SDSG LSA, dys-SDSG LSA, and SR are subtended by points passing through dysplastic endplates. Although this may have the theoretic advantage of better reflecting the pathologic changes of spondylolisthesis, it comes at the cost of decreasing correlation with slip percentage. However, reliability measures were once again not affected.
Fig. 2.
Dysplastic changes that can occur at the L5 and S1 vertebrae (dotted lines)
This study employed computer aided technique to determine the values of the six angles studied. The software computed the angles from the identification of the four corners of L5 and S1. This provided data acquisition for all six parameters in a quick and a time efficient manner. Similarly, picture archiving and communication systems (PACS) are now widely available in a growing number of institutions and possess angle measurement tools. The authors believe that a study design that would employ PACS software’s angle measurement tools, instead of the custom software in the present study, would be feasible and yield similar results, albeit more time consuming. As such, it is believed that the results of this study can be transposed to the clinical setting that employs PACS software.
Conclusion
The results of this study show that all measures of lumbosacral kyphosis have substantial to almost perfect inter- and intra-rater reliability. Dubousset’s LSA showed the strongest correlation with slip grade. Having shown that Dubousset’s LSA is reliable and strongly correlated to slip percentage, the authors believe that this parameter can appropriately and reliably be used in the clinical setting with PACS software capabilities to assess LSK. Finally, in order to increase the reliability of the measurement of lumbosacral kyphosis in spondylolisthesis, the authors recommend the use of a computer-assisted technique based on the identification of the corners of L5 and S1.
Acknowledgments
This study was supported in part by an educational\research grant from Medtronic Sofamor Danek. This study was assisted with support from the Spinal Deformity Study Group.
Contributor Information
Panagiotis Glavas, Email: pglavas@hotmail.com.
Hubert Labelle, Phone: +1-514-3454876, FAX: +1-514-3454755, Email: hubert.labelle@recherche-ste-justine.qc.ca.
References
- 1.Amundson G, Edwards CC, Garfin SR, et al. Spondylolisthesis. In: Herkowitz HN, Garfin SR, Balderston RA, et al., editors. The spine. Philadelphia: W·B. Saunders; 1992. pp. 913–969. [Google Scholar]
- 2.Antoniades SB, Hammerberg KW, Dewald RL. Sagittal plane configuration of the sacrum in spondylolisthesis. Spine. 2000;25:1085–1091. doi: 10.1097/00007632-200005010-00008. [DOI] [PubMed] [Google Scholar]
- 3.Berthonnaud E, Dimnet J, Labelle H, et al. et al. Spondylolisthesis. In: O’Brien MF, Kuklo TR, Blanke KM, et al.et al., editors. Spinal deformity group radiographic measurement manual. Memphis: Medtronik Sofamor Danek; 2004. pp. 95–108. [Google Scholar]
- 4.Boxall D, Bradford DS, Winter RB, et al. Management of severe spondylolisthesis in children and adolescents. J Bone Joint Surg Am. 1979;61:479–495. [PubMed] [Google Scholar]
- 5.Bradford DS, et al. Spondylolysis and spondylolisthesis. In: Lonstein JE, Winter RB, Bradford DS, et al., editors. Textbook of scoliosis and other spinal deformities. Philadelphia: W·B. Saunders; 1995. pp. 399–430. [Google Scholar]
- 6.Burkus JK, Lonstein JE, Winter RB, Denis F. Long-term evaluation of adolescents treated operatively for spondylolisthesis. A comparison of in situ arthrodesis only with in situ arthrodesis and reduction followed by immobilization in a cast. J Bone Joint Surg Am. 1992;74:693–704. [PubMed] [Google Scholar]
- 7.Cohen J, Cohen P, West SG et al (2003) Applied multiple regression/correlation analysis for the behavioral sciences. Lawrence Erlbaum Associates, Hillsdale
- 8.Dubousset J. Treatment of spondylolysis and spondylolisthesis in children and adolescents. Clin Orthop Relat Res. 1997;337:77–85. doi: 10.1097/00003086-199704000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Faro FD, Marks MC, Pawelek J, et al. Evaluation of a functional position for lateral radiograph acquisition in adolescent idiopathic scoliosis. Spine. 2004;29:2284–2289. doi: 10.1097/01.brs.0000142224.46796.a7. [DOI] [PubMed] [Google Scholar]
- 10.Frennered AK, Danielson BI, Nachemson AL. Natural history of symptomatic isthmic low-grade spondylolisthesis in children and adolescents: a seven-year follow-up study. J Pediatr Orthop. 1991;11:209–213. doi: 10.1097/01241398-199103000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Harris IE, Weinstein SL. Long-term follow-up of patients with grade-III and IV spondylolisthesis. Treatment with and without posterior fusion. J Bone Joint Surg Am. 1987;69:960–969. [PubMed] [Google Scholar]
- 12.Harrison DE, Harrison DD, Cailliet R, et al. Radiographic analysis of lumbar lordosis. centroid, Cobb, TRALL, and Harrison posterior tangent methods. Spine. 2001;26:E235–E242. doi: 10.1097/00007632-200106010-00003. [DOI] [PubMed] [Google Scholar]
- 13.Hensinger RN. Spondylolysis and spondylolisthesis in children and adolescents. J Bone Joint Surg Am. 1989;71:1098–1107. [PubMed] [Google Scholar]
- 14.Herman MJ, Pizzutillo PD, Cavalier R. Spondylolysis and spondylolisthesis in the child and adolescent athlete. Orthop Clin North Am. 2003;34:461–467. doi: 10.1016/S0030-5898(03)00034-8. [DOI] [PubMed] [Google Scholar]
- 15.Horton WC, Brown CW, Bridwell KH, et al. Is there an optimal patient stance for obtaining a lateral 36″ radiograph? Spine. 2005;30:427–433. doi: 10.1097/01.brs.0000153698.94091.f8. [DOI] [PubMed] [Google Scholar]
- 16.Hu SS, Bradford DS. Spondylolysis and spondylolisthesis. In: Weinstein SL, editor. The pediatric spine principles and practice. Philadelphia: Lippincott Williams and Wilkins; 2001. pp. 433–451. [Google Scholar]
- 17.Labelle H, Roussouly P, Berthonnaud É, et al. The importance of spino-pelvic balance in L5–S1 developmental spondylolisthesis: a review of pertinent radiological measurements. Spine. 2005;30:S27–S34. doi: 10.1097/01.brs.0000155560.92580.90. [DOI] [PubMed] [Google Scholar]
- 18.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 19.Lonstein JE. Spondylolisthesis in children. Spine. 1999;24:2640–2648. doi: 10.1097/00007632-199912150-00011. [DOI] [PubMed] [Google Scholar]
- 20.Mac-Thiong JM, Labelle H, Parent S, et al. Assessment of sacral doming in lumbosacral spondylolisthesis. Spine. 2007;32:1888–1895. doi: 10.1097/BRS.0b013e31811ebaa1. [DOI] [PubMed] [Google Scholar]
- 21.Mardjetko S, Albert T, Gunnar A, et al. Spine/SRS spondylolisthesis summary statement. Spine. 2005;30:S3. doi: 10.1097/01.brs.0000155556.32449.ae. [DOI] [PubMed] [Google Scholar]
- 22.Meyerding HW. Spondylolisthesis. Surg Gynecol Obstet. 1932;54:371–377. [Google Scholar]
- 23.Molinari RW, Lenke LG. Pediatric spondylolysis and spondylolisthesis. In: Frymoyer JW, Wiesel SW, editors. The adult and pediatric spine. Philadelphia: Lippincott Williams and Wilkins; 2003. pp. 300–423. [Google Scholar]
- 24.Molinari RW, Bridwell KH, Lenke LG, et al. Complications in the surgical treatment of pediatric high-grade, isthmic dysplastic spondylolisthesis. A comparison of three surgical approaches. Spine. 1999;24:1701–1711. doi: 10.1097/00007632-199908150-00012. [DOI] [PubMed] [Google Scholar]
- 25.Petraco DM, Spivak JM, Cappadona JG, et al. An anatomic evaluation of L5 nerve stretch in spondylolisthesis reduction. Spine. 1996;21:1133–1139. doi: 10.1097/00007632-199605150-00002. [DOI] [PubMed] [Google Scholar]
- 26.Speck GR, McCall IW, O’Brien JP. Spondylolisthesis: the angle of kyphosis. Spine. 1984;9:659–660. doi: 10.1097/00007632-198409000-00022. [DOI] [PubMed] [Google Scholar]
- 27.Timon SJ, Gardner MJ, Wanich T, et al. Not all spondylolisthesis grading instruments are reliable. Clin Orthop Relat Res. 2005;434:157–162. doi: 10.1097/01.blo.0000154205.10944.72. [DOI] [PubMed] [Google Scholar]
- 28.Vialle R, Schmit P, Dauzac C, et al. Radiological assessment of lumbosacral dystrophic changes in high-grade spondylolisthesis. Skeletal Radiol. 2005;34:528–535. doi: 10.1007/s00256-005-0948-1. [DOI] [PubMed] [Google Scholar]
- 29.Wiltse LL, Winter RB. Terminology and measurement of spondylolisthesis. J Bone Joint Surg Am. 1983;65:768–772. [PubMed] [Google Scholar]
- 30.Winter JG, Bell D. Lumbosacral joint angles. J Pediatr Orthop. 1991;11:748–751. doi: 10.1097/01241398-199111000-00009. [DOI] [PubMed] [Google Scholar]
- 31.Yue W-M, Brodner W, Gaines RW. Anatomical findings in 27 cases of surgically corrected spondyloptosis. Proximal sacral endplate damage as a possible cause of spondyloptosis. Spine. 2005;30:S22–S26. doi: 10.1097/01.brs.0000155572.72287.92. [DOI] [PubMed] [Google Scholar]