Abstract
The object of this study is to compare radiographic outcomes of anterior cervical decompression and fusion (ACDF) versus cervical disc replacement using the Bryan Cervical Disc Prosthesis (Medtronic Sofamor Danek, Memphis, TN) in terms of range of motion (ROM), Functional spinal unit (FSU), overall sagittal alignment (C2–C7), anterior intervertebral height (AIH), posterior intervertebral height (PIH) and radiographic changes at the implanted and adjacent levels. The study consisted of 105 patients. A total of 63 Bryan disc were placed in 51 patients. A single level procedure was performed in 39 patients and a two-level procedure in the other 12. Fifty-four patients underwent ACDF, 26 single level cases and 28 double level cases. The Bryan group had a mean follow-up 19 months (12–38). Mean follow-up for the ACDF group was 20 months (12–40 months). All patients were evaluated using static and dynamic cervical spine radiographs as well as MR imaging. All patients underwent anterior cervical discectomy followed by autogenous bone graft with plate (or implantation of a cage) or the Bryan artificial disc prosthesis. Clinical evaluation included the visual analogue scale (VAS), and neck disability index (NDI). Radiographic evaluation included static and dynamic flexion-extension radiographs using the computer software (Infinitt PiviewSTAR 5051) program. ROM, disc space angle, intervertebral height were measured at the operative site and adjacent levels. FSU and overall sagittal alignment (C2–C7) were also measured pre-operatively, postoperatively and at final follow-up. Radiological change was analyzed using χ2 test (95% confidence interval). Other data were analyzed using the mixed model (SAS enterprises guide 4.1 versions). There was clinical improvement within each group in terms of VAS and NDI scores from pre-op to final follow-up but not significantly between the two groups for both single (VAS p = 0.8371, NDI p = 0.2872) and double (VAS p = 0.2938, NDI p = 0.6753) level surgeries. Overall, ROM and intervertebral height was relatively well maintained during the follow-up in the Bryan group compared to ACDF. Regardless of the number of levels operated on, significant differences were noted for overall ROM of the cervical spine (p < 0.0001) and all other levels except at the upper adjacent level for single level surgeries (p = 0.2872). Statistically significant (p < 0.0001 and p = 0.0172) differences in the trend of intervertebral height measurements between the two groups were noted at all levels except for the AIH of single level surgeries at the upper (p = 0.1264) and lower (p = 0.7598) adjacent levels as well as PIH for double level surgeries at the upper (p = 0.8363) adjacent level. Radiological change was 3.5 times more observed for the ACDF group. Clinical status of both groups, regardless of the number of levels, showed improvement. Although clinical outcomes between the two groups were not significantly different at final follow-up, radiographic parameters, namely ROM and intervertebral heights at the operated site, some adjacent levels as well as FSU and overall sagittal alignment of the cervical spine were relatively well maintained in Bryan group compared to ACDF group. We surmise that to a certain degree, the maintenance of these parameters could contribute to reduce development of adjacent level change. Noteworthy is that radiographic change was 3.5 times more observed for ACDF surgeries. A longer period of evaluation is needed, to see if all these radiographic changes will translate to symptomatic adjacent level disease.
Keywords: Bryan, Arthroplasty, Arthrodesis, Radiologic degenerative change, Adjacent level
Introduction
Anterior cervical decompression and fusion (ACDF) with autologous bone graft is a well established and commonly performed procedure for symptomatic cervical disc disorder. Since its introduction in the 1950s by Robinson and Smith as well as Cloward, excellent clinical reports have been reported in the treatment of degenerative disorders of the spine [7, 24]. Long-term results have shown excellent pain relief and 73–90% fusion rates [6, 7, 9, 24, 32]. But, despite the high success of ACDF, there have been complications such as persistence of neurologic symptoms, donor site morbidity and pseudoarthrosis; hence the development of newer techniques and additional devices for fixation and improved stability [6, 7, 9, 24, 32].
The emergence of the use of anterior cervical plates has improved fusion rates especially in multi-level cases through added stability and rigid fixation [15, 29, 30].
However, other complications of fusion such as the development of late symptomatic adjacent level disease still have to be addressed. These may include radiographic changes like anterior osteophyte formation or ossification of the anterior longitudinal ligament (ALL) and these have been reported following anterior cervical arthrodesis regardless of the use of plates or not [13, 14, 26].
A retrospective study showed that ossification of the ALL developed in 70 (59%) of the 118 cephalad adjacent disc spaces and 29 (29%) of the 100 caudal adjacent disc spaces in patients who underwent ACDF (p < 0.001) [22].
Long-term outcome data (5–10 years) suggests that in patients who underwent ACDF, there were significant radiographic changes at adjacent levels such as narrowing of disc space or development of new posterior osteophytes that were translated clinically like new onset radiculopathy or myelopathy referable to the adjacent degenerated level [13].
More recently, Goffin et al. [11] showed that after at least a 60 month follow-up, they had 6.11% reoperation rate due to symptomatic adjacent level degeneration.
Cervical disc replacement is an emerging technology indicated for reconstruction following anterior cervical discectomy in patients having cervical disc disorders. The primary goal of cervical arthroplasty is to remove the pathologically herniated disc while maintaining disc height, and preserving motion. By preserving motion, the disc arthroplasty may decrease the incidence of adjacent segment degeneration [3, 17, 18, 27, 33].
The Bryan disc (Medtronic Sofamor Danek, Memphis, USA) arthroplasty device was developed to preserve the kinematics of the functional spine unit (FSU) thus preventing adjacent level disease. It is an unconstrained, biarticulating, metal-on-polyurethane sheath surrounding the nucleus; the sheath is filled with saline, which acts as synovial fluid [2, 10].
To the best of our knowledge, there have been only a few studies comparing the incidence of adjacent level changes in patients who underwent ACDF with a plate compared to implantation of a cervical artificial disc such as the Bryan disc [21, 23]. In addition, there have been only a few reports regarding the intermediate term effects of these adjacent segment changes to the overall cervical alignment or FSU in single and bi-level cases [11].
Thus, this will be a novel study to compare the clinical and radiologic outcomes of patients who underwent ACDF or Bryan cervical disc arthroplasty in single and bi-level cases. We also hope to understand ongoing processes and any possible underlying changes at the adjacent level during the follow-up period.
Materials and methods
This is a prospective cohort study that consisted of 105 patients with symptomatic single or two-level cervical disc disease who received the Bryan Cervical Artificial Disc Prosthesis (Medtronic Sofamor Danek, Memphis, TN, USA). A total of 63 Bryan discs were placed in 51 patients (Table 1). Among these 51 patients, a single level procedure was performed in 39 patients and a two-level procedure in the other 12. There were 54 patients who underwent ACDF with autogenous bone and used different types of anterior cervical plates or stand-alone cages. There were two cases that used the Blackstone cage (Blackstone Medical Inc, USA), three cases that used the Solis cage (Stryker Spine, USA). The ABC plate (Aesculap, USA) was used in 16 cases while 33 used the Atlantis plate (Medtronic, Sofamor Danek, Memphis, TN, USA). There were 26 who underwent single level ACDF and 28 who underwent double level procedures (Table 1).
Table 1.
Patient’s demographics (ACDF and Bryan artificial disc)
| Single level ACDF | Single level Bryan | Bi-level ACDF | Bi-level Bryan | |
|---|---|---|---|---|
| Number of patients | 26 | 39 | 28 | 12 |
| Mean age (age range in years) | 47.4 (33–74) | 43.6 (24–74) | 52.7 (30–78) | 46.91 (30–58) |
| Gender | 17 men, 19 women | 21 men, 18 women | 17 men, 11 women | 8 men, 4 women |
| Clinical diagnosis | ||||
| Radiculopathy | 22 | 36 | 24 | 10 |
| Myelopathy | 4 | 3 | 4 | 2 |
| Level implanted | C3–C4 (n = 5); C4–C5 (n = 4); C5–C6 (n = 13); C6–C7 (n = 4) | C3–C4 (n = 3); C4–C5 (n = 4); C5–C6 (n = 24); C6–C7 (n = 8) | C4–C5–C6 (n = 13); C5–C6–C7 (n = 15) | C4–C5–C6 (n = 4); C5–C6–C7 (n = 8) |
n number of cases done at this level
The study group consisted of 29 men and 22 women in the artificial disc group, 34 men and 18 women in the ACDF group. Their mean age was 43.85 years in the Bryan group and 46.44 years in the ACDF group (Table 1). All patients were evaluated using static and dynamic cervical spine radiographs as well as magnetic resonance (MR) imaging.
The Bryan study was begun on November 2003, and the last patient’s complete follow-up review was in January 2008. The mean follow-up period was 19 months (12–38 months). ACDF study was begun on June 2003, and the last patient’s complete follow-up review was in January 2008. The mean follow-up period was 20 months (12–40 months) (Table 2).
Table 2.
Follow-up period in months
| Single level ACDF | Single level Bryan | Double level ACDF | Double level Bryan | Total |
|---|---|---|---|---|
| 17 (12–36) | 18 (13–40) | 21 (14–38) | 18 (13–37) | 19 (12–40) |
All patients underwent anterior cervical discectomy and fusion with autogenous iliac or fibular bone graft followed by anterior cervical plating/Stand-alone cage filled with autogenous bone or implantation of the Bryan artificial disc prosthesis. All procedures were completed through a transverse skin incision made on the right side of the neck, and all procedures were performed by one surgeon (S. W. K.)
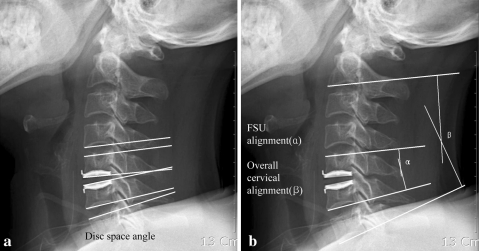
Clinical evaluation included the visual analogue scale (VAS), and neck disability index (NDI). Radiographic evaluation included static and dynamic flexion-extension radiographs in an upright position. Measurements on digital radiographs were made using the computer software (Infinitt PiviewSTAR 5051) program. The disc space angle at the operative site was taken and defined as the angle formed preoperatively by the natural endplates and postoperatively by the shells of the shells of the prosthesis (Fig. 1a). The angle of the FSU was determined by the angle of intersection of tangential lines drawn along the superior end plate of the cephalad vertebral body, and the inferior end plate of the caudal body. The Cobb angle from C2 to C7 was used as a measure of the overall sagittal alignment, which was determined by the angle of intersection of tangential lines drawn along the inferior end plate of C2 and the inferior end plate of C7 [31]. A positive angle reflects a kyphotic angulation, whereas a negative measurement denotes lordosis. The sum of disc space angle at full flexion and extension was used to calculate ROM. In FSU or C2–C7 alignment, curvatures were defined as follows: lordosis-Cobb angle <0°; straight- 0° ≤ Cobb angle < 5°; kyphosis-Cobb angle ≥5°.
Fig. 1.
a Disc space angle. b α Functional Spinal Unit (FSU), β Overall sagittal alignment
The radiologic evidence of adjacent level change included the presence of any of the following radiographic parameters above or below the operated level:
new anterior or enlarging osteophyte formation;
increase or new narrowing of disc space defined as 30% ≤ narrowing of the intervertebral disc space;
The distance between the most anterior points of the upper and lower endplates was measured as the anterior interbody height (AIH). The distance between the most posterior points of the upper and lower endplates was measured as the posterior interbody height (PIH) (Fig. 1).
Radiographic measurement data were collected from three observers. Each of them measured three times, and the mean value was used for analysis to correct the intraobserver and interobserver reliability of the radiologic measurement.
Radiologic change was analyzed using χ2 test (95% confidence interval). Other Data were analyzed using mixed model (SAS enterprise guide 4.1 version).
Results
Clinical and surgical outcome
Single level ACDF vs. single level Bryan
Both single level ACDF and single level Bryan implanted groups showed improvement of their VAS and NDI scores (Table 3).
Table 3.
Clinical results of ACDF compared with Bryan disc using visual analog scale (VAS) and neck disability index (NDI)
| Single level ACDF | Single level Bryan | Double level ACDF | Double level Bryan | |
|---|---|---|---|---|
| VAS | ||||
| Pre-op | 8.3 ± 0.9 | 8.3 ± 1.0 | 8.1 ± 1.0 | 8.8 ± 0.9 |
| Post-op | 6.2 ± 0.8 | 6.4 ± 0.7 | 5.8 ± 0.8 | 6.5 ± 0.8 |
| Follow-up | 3.8 ± 1.1 | 3.7 ± 0.9 | 3.4 ± 1.1 | 3.3 ± 0.8 |
| p value | 0.8371 | 0.2938 | ||
| NDI | ||||
| Pre-op | 25.5 ± 1.5 | 25.3 ± 1.8 | 26.2 ± 1.9 | 26.4 ± 1.5 |
| Post-op | 16.6 ± 2.0 | 17.1 ± 1.7 | 17.6 ± 1.5 | 16.8 ± 1.8 |
| Follow-up | 7.2 ± 1.6 | 7.6 ± 0.9 | 8.0 ± 0.9 | 7.8 ± 1.3 |
| p value | 0.2872 | 0.6753 | ||
p = 0.05 set value for statistical significance using the mixed model
Compared to pre-op scores, the VAS score for both ACDF and Bryan groups decreased. NDI scores at last follow-up compared to pre-op scores for the ACDF and Bryan group also decreased.
Double level ACDF vs. double level Bryan
All patients in the double level ACDF and double level Bryan groups improved their VAS and NDI scores. Compared to pre-op scores, the VAS scores for both the ACDF and Bryan groups decreased. NDI score at last follow-up compared to pre-op scores for the ACDF and Bryan groups also decreased (Table 3).
Clinical and surgical outcome summary and comparison
There was no significant difference between ACDF and Arthroplasty group for both single (VAS p = 0.8371, NDI p = 0.2872) and double (VAS p = 0.2938, NDI p = 0.6753) level surgeries, although there was a clinical improvement within each group in terms of VAS and NDI scores from pre-op measurements to final follow-up. The results comparing the two groups were not significantly different (Tables 3, 9).
Table 9.
Summary of the results of ACDF compared with Bryan disc using clinical and radiologic parameters
| Parameters | Single level ACDF and Bryan | Double level ACDF and Bryan | ||
|---|---|---|---|---|
| VAS score | p = 0.8371 | p = 0.2938 | ||
| NDI score | p = 0.2872 | p = 0.6753 | ||
| ROM (implanted level) | p < 0.0001* | p < 0.0001* | ||
| ROM (upper adjacent level) | p = 0.2872 | p < 0.0001* | ||
| ROM (lower adjacent level) | p < 0.005* | p < 0.0001* | ||
| FSU alignment | p < 0.0001* | p = 0.0280* | ||
| Overall C2–C7 alignment | p < 0.0001* | p < 0.0001* | ||
| Disc height(Implanted –AIH) | p < 0.0001* | p < 0.0001* | ||
| Disc height(Implanted –PIH) | p = 0.0052* | p < 0.0001* | ||
| Disc height(upper–AIH) | p = 0.1264 | p = 0.0172* | ||
| Disc height(upper–PIH) | p < 0.0001* | p = 0.8363 | ||
| Disc height(lower–AIH) | p = 0.7598 | p < 0.0001* | ||
| Disc height(lower–PIH) | p < 0.0001* | p < 0.0001* | ||
p = 0.05 set value for statistical significance using the mixed model
* Statistically significant
AIH Anterior interbody height, PIH posterior interbody height, ACDF anterior cervical discectomy and fusion, FSU functional spinal unit, VAS visual analogue scale, NDI neck disability index
Range of motion
Implanted level (disc space angle)
Single level ACDF vs. single level Bryan
The ROM for the ACDF group decreased from pre-op to last follow-up by 21%. In the Bryan group, there was an increase in range of motion (ROM) from pre-op to last follow-up by 9%. The ROM from pre-op to final follow-up of the Bryan group compared to the ACDF group was relatively well maintained and the difference was significant (p < 0.0001) (Table 4).
Table 4.
Sagittal ROM at the implanted level for ACDF vs. Bryan groups
| Single level ACDF | Single level Bryan | Double level ACDF | Double level Bryan | |
|---|---|---|---|---|
| Pre-op (°) | ||||
| Flex | 7.5 ± 2.5 | 6.2 ± 1.4 | 8.2 ± 1.3 | 6.2 ± 1.1 |
| Ext | −3.7 ± 0.6 | −4.9 ± 1.4 | −4.5 ± 0.8 | −5.3 ± 0.9 |
| ROM | 11.1 ± 2.7 | 11.1 ± 2.1 | 12.7 ± 1.7 | 11.9 ± 1.2 |
| Post-op (°) | ||||
| Flex | 0.7 ± 0.2 | 6.4 ± 1.5 | 0.8 ± 0.1 | 6.3 ± 1.2 |
| Ext | −1.5 ± 0.5 | −5.1 ± 1.4 | −0.9 ± 0.3 | −5.5 ± 1.1 |
| ROM | 2.3 ± 0.5 | 11.5 ± 1.9 | 1.7 ± 0.3 | 11.7 ± 1.1 |
| Follow-up (°) | ||||
| Flex | 0.7 ± 0.2 | 6.7 ± 1.6 | 0.7 ± −0.1 | 6.5 ± 1.1 |
| Ext | −1.7 ± 0.6 | −5.3 ± 1.4 | −0.6 ± 0.1 | −5.7 ± 0.9 |
| ROM | 2.3 ± 0.8 | 12.1 ± 2.0 | 1.3 ± 0.2 | 12.3 ± 1.9 |
| p value | <0.0001 | <0.0001 | ||
p = 0.05 set value for statistical significance using the mixed model
Double level ACDF vs. double level Bryan
The ROM for the ACDF group decreased from pre-op to last follow-up by 10%. In the Bryan group, there was an increase in ROM from pre-op to last follow-up by 3%. The ROM of the double level Bryan group compared to the double level ACDF group was relatively well maintained and the trend was found to be significant (p < 0.0001) (Table 4).
Implanted level ROM comparison and summary
There was a significant (p < 0.0001) difference in ROM at the operated site between the ACDF and Bryan group in both single and double level cases (Tables 4, 9).
Upper level
Single level ACDF vs. single level Bryan
In both the single level Bryan and the single level ACDF group, the adjacent level ROM increased at the upper level. Comparing the radiographic measurements from pre-op to final follow-up, the ROM of the ACDF group was increased by 8% and the Bryan group by 9%. The difference in the pattern between the two groups was not statistically significant (p = 0.2872) (Table 5).
Table 5.
Sagittal ROM of adjacent levels
| Single level ACDF | Single level Bryan | Double level ACDF | Double level Bryan | |
|---|---|---|---|---|
| Upper level (°) | ||||
| Pre-op | ||||
| Flex | 5.1 ± 1.2 | 4.4 ± 1.4 | 5.0 ± 0.4 | 4.6 ± 1.3 |
| Ext | −4.4 ± 1.5 | −4.3 ± 1.4 | −2.7 ± 1.2 | −4.4 ± 1.2 |
| ROM | 9.4 ± 1.3 | 8.7 ± 2.1 | 7.7 ± 1.1 | 9.0 ± 1.6 |
| Post-op | ||||
| Flex | 5.8 ± 1.2 | 4.5 ± 1.4 | 1.6 ± 0.4 | 5.1 ± 1.5 |
| Ext | −4.3 ± 1.7 | −4.5 ± 1.4 | −1.3 ± 0.3 | −3.8 ± 0.6 |
| ROM | 10.1 ± 1.7 | 9.1 ± 2.0 | 2.8 ± 0.7 | 9.0 ± 2.0 |
| Follow-up | ||||
| Flex | 5.5 ± 1.6 | 4.6 ± 1.5 | 2.4 ± 0.2 | 4.9 ± 1.4 |
| Ext | −4.7 ± 1.6 | −4.8 ± 1.5 | −2.1 ± 0.2 | −4.9 ± 1.5 |
| ROM | 10.2 ± 1.4 | 9.5 ± 2.1 | 4.3 ± 0.9 | 9.9 ± 1.8 |
| p value | 0.2872 | <0.0001 | ||
| Lower level (°) | ||||
| Pre-op | ||||
| Flex | 7.5 ± 1.6 | 4.5 ± 1.5 | 3.5 ± 0.8 | 4.9 ± 1.4 |
| Ext | −3.9 ± 0.9 | −3.8 ± 1.2 | −2.3 ± 0.8 | −3.6 ± 0.7 |
| ROM | 11.4 ± 2.3 | 8.3 ± 2.3 | 5.5 ± 1.7 | 8.5 ± 1.9 |
| Post-op | ||||
| Flex | 5.0 ± 1.3 | 4.7 ± 1.5 | 2.0 ± 0.6 | 5.1 ± 1.5 |
| Ext | −4.0 ± 1.9 | −4.0 ± 1.2 | −2.6 ± 0.8 | −3.8 ± 0.6 |
| ROM | 9.0 ± 2.5 | 8.7 ± 2.3 | 4.5 ± 1.5 | 9.0 ± 2.0 |
| Follow-up | ||||
| Flex | 6.2 ± 2.0 | 4.8 ± 1.8 | 3.0 ± 0.4 | 5.4 ± 1.4 |
| Ext | −4.6 ± 2.1 | −4.4 ± 1.4 | −3.4 ± 0.7 | −4.0 ± 0.8 |
| ROM | 10.8 ± 3.4 | 9.2 ± 2.4 | 6.2 ± 1.5 | 9.4 ± 2.1 |
| p value | <0.005 | <0.0001 | ||
p = 0.05 set value for statistical significance using the mixed model
Double level ACDF vs. double level Bryan
The double level ACDF group showed an initial decrease in ROM from pre-op to post-op by 64% but the decrease eventually became 44% by last follow-up. In the double Bryan group, the ROM from pre-op was increased by 5% at post-op and then 10% by final follow-up. Comparing the change of ROM pattern from pre-op to final follow-up between the two groups, the difference in their ROM was found to be statistically significant (p < 0.0001) (Table 5).
Lower level
Single level ACDF vs. single level Bryan
In the single ACDF group at the lower level, there was an initial decrease of ROM by 21% compared to pre-op but at last follow-up, the decrease eventually became 6% compared to pre-op measurements. In the single Bryan group, ROM was increased by 4% and 5% in post-op and final follow-up, respectively. The difference in their changing pattern was significant (p < 0.005) (Table 5).
Double level ACDF vs. double level Bryan
In the double level ACDF group, the ROM decreased by 18.5% immediately post-op but eventually increased by 13% from pre-op measurements. While in the double level Bryan group, at immediately post-op, there was an increase by 5% which further increased to 10% at final follow-up when compared to pre-op measurements. The difference between the two groups was also significant (p < 0.0001) (Table 5).
Adjacent level ROM comparison and summary
ROM at the upper level increased significantly (p < 0.0001) for double level Bryan surgeries but the increase was not significant (p = 0.2872) for single level surgeries. At the lower level for single level surgeries, ROM of the Bryan group increased while a decrease was seen for the ACDF group and the difference was significant (p < 0.005). The same significant (p < 0.0001) difference was seen for double level surgeries (Tables 5, 9).
FSU
Single level ACDF vs. single level Bryan
In terms of the functional spinal unit (FSU) angle, both the single level ACDF group and single level Bryan group, there was an observed decrease. In the Bryan group, the decrease from pre-op to immediately post-op was 34% and then to 28% at final follow-up. In the ACDF group, there was a decrease by 76% post-op and 73% at final follow-up when compared with pre-op measurements (p < 0.0001) (Table 6).
Table 6.
Functional spinal unit (FSU) and overall cervical alignment (C2–C7)
| Single level ACDF | Single level Bryan | Double level ACDF | Double level Bryan | |
|---|---|---|---|---|
| FSU | ||||
| Pre-op (°) | ||||
| Flex | 8.0 ± 1.7 | 6.8 ± 2.5 | 9.8 ± 2.1 | 8.0 ± 1.7 |
| Ext | −5.3 ± 0.9 | −5.9 ± 2.9 | −10.9 ± 2.4 | −7.3 ± 3.0 |
| ROM | 13.3 ± 2.1 | 12.7 ± 4.7 | 20.7 ± 2.3 | 15.3 ± 4.3 |
| Post-op (°) | ||||
| Flex | 2.0 ± 0.6 | 4.5 ± 2.0 | 2.5 ± 0.2 | 3.8 ± 1.3 |
| Ext | −1.2 ± 0.4 | −3.9 ± 2.3 | −2.8 ± 0.6 | −3.5 ± 1.6 |
| ROM | 3.3 ± 0.6 | 8.4 ± 3.2 | 5.3 ± 0.5 | 7.3 ± 2.4 |
| Follow-up (°) | ||||
| Flex | 1.8 ± 0.6 | 5.2 ± 2.2 | 2.2 ± 0.3 | 4.5 ± 1.4 |
| Ext | −1.8 ± 0.6 | −4.4 ± 2.4 | −3.2 ± 0.5 | −4.0 ± 1.7 |
| ROM | 3.7 ± 0.6 | 9.6 ± 3.6 | 5.4 ± 0.5 | 8.4 ± 2.7 |
| p value | <0.0001 | 0.0280 | ||
| C2-7 | ||||
| Pre-op (°) | ||||
| Flex | 23.5 ± 3.4 | 24.3 ± 6.0 | 16.6 ± 2.3 | 27.0 ± 5.5 |
| Ext | −27.9 ± 0.9 | −25.2 ± 3.9 | −28.9 ± 3.5 | −24.4 ± 2.7 |
| ROM | 51.4 ± 7.3 | 49.5 ± 6.4 | 43.9 ± 9.5 | 51.4 ± 6.6 |
| Post-op (°) | ||||
| Flex | 13.6 ± 2.7 | 25.6 ± 6.1 | 8.4 ± 2.2 | 28.5 ± 5.9 |
| Ext | −18.6 ± 4.1 | −25.9 ± 3.9 | −23.0 ± 1.6 | −25.1 ± 2.5 |
| ROM | 32.2 ± 3.2 | 51.4 ± 6.5 | 30.3 ± 6.6 | 53.5 ± 6.7 |
| Follow-up (°) | ||||
| Flex | 18.0 ± 4.6 | 26.3 ± 5.8 | 9.9 ± 2.4 | 29.3 ± 5.4 |
| Ext | −21.5 ± 3.7 | −26.9 ± 3.6 | −25.1 ± 1.1 | −26.4 ± 2.6 |
| ROM | 39.6 ± 5.6 | 53.2 ± 5.8 | 35.0 ± 2.3 | 55.7 ± 6.0 |
| p value | <0.0001 | <0.0001 | ||
p = 0.05 set value for statistical significance using the mixed model
Double level ACDF vs. double level Bryan
The pattern observed in the double level ACDF group and double level Bryan group, from pre-op measurements to final follow-up was a decrease in the FSU angle for both groups. The Bryan group, showed an initial decrease by 52% post-op which subsequently became 46% when compared to pre-op measurements. In the ACDF group, there was a decrease by 74.4% post-op and 74% at final follow-up when compared with pre-op measurements (p = 0.0280) (Table 6).
FSU angle summary and comparison
A decrease in the FSU angle was observed for both the Bryan and ACDF groups in single (p < 0.0001) and double (p = 0.0280) level surgeries but the decrease in pattern was significantly different comparing the two arms (Tables 6, 9).
C2–C7 overall sagittal alignment
Single level ACDF vs. single level Bryan
In C2–C7 flexion and extension measurements, the overall sagittal alignment of the single level ACDF group decreased. In contrast, the single Bryan group showed an increase. In the ACDF group, the decrease was 37 and 23% for immediate post-op and final follow up, respectively, when compared to pre-op measurements. In the Bryan group, there was a decrease by 3% post-op and then by 7% at final follow-up when compared with pre-op measurements (p < 0.0001) (Table 6).
Double level ACDF vs. double level Bryan
In double level surgeries, the C2–C7 flexion and extension measurements showed that the overall sagittal alignment of the ACDF group decreased and while that of the Bryan group increased. In the ACDF group, there was a 31% decrease in overall sagittal alignment postoperatively but became 20% at final follow-up from pre-op measurements. In the Bryan group, there was an increase by 4% immediately post-op which further increased to 8% at final follow-up (p < 0.0001) (Table 6).
Overall sagittal alignment (C2–C7) summary and comparison
The overall sagittal alignment of the cervical spine (C2–C7 alignment), in both single and double level surgeries showed an increase in the Bryan group while that of the ACDF group decreased. The difference was found to be statistically significant (p < 0.0001) (Tables 6, 9).
Intervertebral disc height
Operated level
Single level ACDF vs. single level Bryan
Anterior interbody height (AIH). In the ACDF group, there was a 106% increase of the AIH post-operatively, but eventually became just an increase of 77% at last follow-up compared to pre-op measurements. The single Bryan group showed an initial decrease of the AIH by 26% post-operatively and further decreased to 35% at final follow-up compared to preoperative measurements. This difference in measurements between the two groups was statistically significant (p < 0.0001) (Table 7).
Posterior interbody height (PIH). In double level surgeries, both the ACDF group and Bryan group showed an increase in measurements of the PIH from pre-op measurements. There was a 71% increase post-op and 32% increase at last follow-up compared to pre-op measurements in the ACDF group. In the Bryan group, there was an increase by 19% post-op that became 14% at final follow-up compared to pre-op measurements. Though both groups showed an increase, the changes shown in the ACDF group was more variable and the changing pattern between these two groups was also found to be significant (p = 0.0052) (Table 7).
Table 7.
Summary of disc height measurements at implanted, upper and lower levels
| Single level ACDF | Single level Bryan | Double level ACDF | Double level Bryan | |
|---|---|---|---|---|
| Implanted level (mm) | ||||
| AIH | ||||
| Pre-op | 4.35 ± 1.08 | 3.67 ± 1.27 | 4.35 ± 1.03 | 3.45 ± 0.79 |
| Post-op | 8.98 ± 1.27 | 2.73 ± 1.15 | 8.23 ± 1.76 | 2.98 ± 1.19 |
| F/U | 7.70 ± 1.37 | 2.39 ± 0.35 | 6.76 ± 1.84 | 2.63 ± 0.69 |
| p value | <0.0001 | <0.0001 | ||
| PIH | ||||
| Pre-op | 2.81 ± 0.91 | 2.84 ± 0.99 | 3.74 ± 0.75 | 2.85 ± 0.57 |
| Post-op | 4.81 ± 1.40 | 3.37 ± 1.02 | 6.25 ± 1.18 | 3.29 ± 0.86 |
| F/U | 3.70 ± 1.0 | 3.26 ± 0.88 | 4.8 ± 1.05 | 3.05 ± 0.85 |
| p value | 0.0052 | <0.0001 | ||
| Upper level (mm) | ||||
| AIH | ||||
| Pre-op | 4.27 ± 0.80 | 4.5 ± 1.02 | 5.00 ± 1.27 | 4.20 ± 1.03 |
| Post-op | 4.24 ± 0.71 | 4.33 ± 0.82 | 4.72 ± 1.12 | 4.12 ± 0.70 |
| F/U | 3.92 ± 0.66 | 4.23 ± 0.89 | 4.33 ± 1.03 | 4.27 ± 0.76 |
| p value | 0.1264 | 0.0172 | ||
| PIH | ||||
| Pre-op | 2.99 ± 0.66 | 4.12 ± 0.89 | 4.11 ± 0.95 | 3.53 ± 0.90 |
| Post-op | 3.46 ± 0.66 | 4.20 ± 1.04 | 3.80 ± 0.86 | 3.52 ± 0.87 |
| F/U | 2.95 ± 0.61 | 3.74 ± 0.82 | 3.35 ± 0.75 | 3.48 ± 0.95 |
| p value | <0.0001 | 0.8363 | ||
| Lower level (mm) | ||||
| AIH | ||||
| Pre-op | 4.84 ± 1.23 | 4.77 ± 0.91 | 4.68 ± 1.41 | 4.03 ± 1.15 |
| Post-op | 4.90 ± 1.29 | 4.86 ± 1.04 | 4.41 ± 1.17 | 3.96 ± 0.84 |
| F/U | 4.40 ± 1.14 | 4.57 ± 1.04 | 4.00 ± 1.23 | 4.01 ± 1.05 |
| p value | 0.7598 | <0.0001 | ||
| PIH | ||||
| Pre-op | 2.95 ± 0.52 | 4.24 ± 0.87 | 4.27 ± 0.94 | 4.07 ± 0.57 |
| Postop | 3.35 ± 0.74 | 4.12 ± 0.80 | 3.79 ± 0.74 | 3.78 ± 0.40 |
| F/U | 2.98 ± 0.56 | 4.59 ± 1.88 | 3.38 ± 0.98 | 3.31 ± 0.46 |
| p value | <0.0001 | <0.0001 | ||
p = 0.05 set value for statistical significance using the mixed model
Double level ACDF vs. double level Bryan
Anterior interbody height (AIH). In double level ACDF surgeries, there was an initial increase in the AIH by 89% and became 55% at last follow-up. In the Bryan group, there was a decrease by 14% postoperatively and 24% at final follow-up compared to pre-op measurements (p < 0.0001) (Table 7).
Posterior interbody height (PIH). Both the ACDF group and the Bryan group showed an increasing pattern of change in the PIH. There was an initial increase by 67% at post-op for the ACDF group and eventually became only an increase to 28% compared to pre-op measurements. The increasing change for the Bryan group was less variable in that; PIH initially increased by 15% postoperatively and tapered to 7% at final follow-up. Despite both groups having an increasing trend in measurement, the variability of pattern from pre-op measurements between the two groups still showed a significant difference (p < 0.0001) (Table 7).
Operated level intervertebral height summary and comparison
Intervertebral height measurements, for single level surgeries, showed a decrease in AIH for the Bryan group but an increase was noted for the ACDF group and the difference in the pattern was found to be significant (p < 0.0001). Though, PIH was increased in both the Bryan and ACDF group, the difference in pattern was also significant (p = 0.0052). The difference in radiographic measurements of the AIH and PIH for double level surgeries at the operated level was statistically significant (p < 0.0001) (Tables 7, 9).
Upper level
Single level ACDF vs. single level Bryan
Anterior interbody height (AIH). When we measured the AIH at the upper level for single level surgeries, the ACDF group showed a 1% decrease post-operatively and 9% decrease at last follow-up compared to pre-op measurements. For the Bryan group, there was a decrease by 4% at post-op and 6% at final follow-up. This pattern change for AIH measurements between the two groups was not significant (p = 0.1264) (Table 7).
Posterior interbody height (PIH). PIH measurements for single level surgeries showed an initial 15% increase postoperatively but eventually showed a 2% decrease at last follow-up compared to pre-op measurements. In the Bryan group, there was also an increase by 1% postoperatively but eventually decreased to 10% at final follow-up from preoperative measurements. The difference from pre-op to post-op and final follow-up between both groups were statistically significant (p < 0.0001) (Table 7).
Double level ACDF vs. double level Bryan
Anterior interbody height (AIH). Measurements at the upper level of double level surgeries showed a 6% decrease at post-op and a 13% decrease at last follow-up, compared to pre-op measurements for the ACDF group. On the other hand, the Bryan group showed a decrease by 1% postoperatively and then increased to 1% at final follow-up compared to pre-op measurements. The pattern difference from pre-op to post-op and final follow-up between both groups was statistically significant (p = 0.0172) (Table 7).
Posterior interbody height (PIH). In the ACDF group, there was an 8% decrease at post-op and even further decreased to 19% at last follow-up compared to pre-op measurements. In the Bryan group, there was a decrease by 1% at post-op and decreased by 2% at final follow-up compared to pre-op measurements. This pattern change comparing the two arms for PIH measurements was not significant (p = 0.8363).(Table 7)
Upper level intervertebral height measurement summary and comparison
At the upper level, for single level surgeries there was a decrease in AIH in both groups but was not significant (p = 0.1264). On the other hand, PIH was also decreased for both groups but the difference was found to be significant (p < 0.0001). Also, at the upper level for double level surgeries, AIH was increased for the Bryan group but decreased for the ACDF group and the pattern difference in measurements at final follow-up was significant (p = 0.0172). PIH was decreased for both groups but not significant (p = 0.8363) when comparing the two groups (Tables 7, 9).
Lower level
Single level ACDF vs. single level Bryan
Anterior interbody height (AIH). Measurements taken at the lower level for single level surgeries showed that in the ACDF group, there was a 1% increase postoperatively that eventually decreased to 10% at last follow-up from pre-op measurements. In the single level Bryan group, there was also an initial increase by 1% postoperatively but eventually decreased to 5% at final follow-up compared to pre-op measurements. Results comparing the two trends were not statistically significant (p = 0.7598) (Table 7).
Posterior interbody height (PIH). PIH measurements in the ACDF group showed a 14% increase at post-op but later became just a 1% increase at last follow-up. In the Bryan group, there was a decrease by 3% post-op but increased to 8% at final follow-up compared to pre-op measurements. Results between these two groups were statistically significant (p < 0.0001) (Table 7).
Double level ACDF vs. double level Bryan
Anterior interbody height (AIH). Measurements of the AIH for double level surgeries in the ACDF group showed a 6% decrease postoperatively and decreased further to 15% at last follow-up compared to pre-op measurements. In the Bryan group, there was a decrease by 2% at post-op but the decrease became just 0.5% at final follow-up. Comparing the pattern of change from pre-op, the two groups showed a difference that was significant (p < 0.0001) (Table 7).
Posterior interbody height (PIH). The PIH measurements for the ACDF group showed an initial 12% decrease postoperatively and further decreased to 21% on last follow-up compared to pre-op measurements. In the Bryan group, there was also a decrease by 8% postoperatively and further decreased to 19% at final follow-up compared to pre-op measurements. The difference between the two groups was statistically significant (p < 0.0001) (Table 7).
Lower level intervertebral measurement summary and comparison
At the lower level for single level surgeries, the AIH was decreased for both groups and the difference between groups was not significant (p = 0.7598). PIH increased for both groups but comparison showed a significant (p < 0.0001) difference. At the lower level, for double level surgeries there was a significant (p < 0.0001) difference in the AIH and PIH measurements on final follow-up, though both showed decreasing trends (Tables 7, 9).
Radiologic change
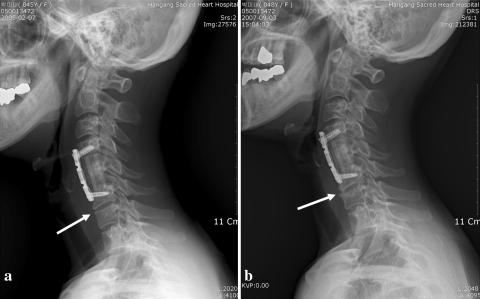
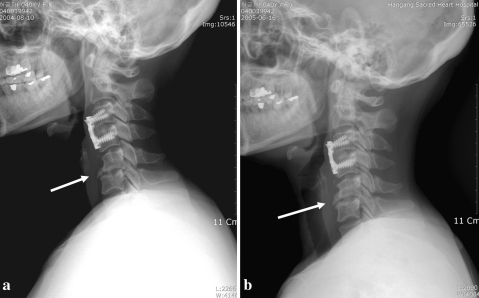
New anterior osteophyte formation was observed in one (2.56%) in the single level Bryan group (Fig. 2a, b), three (10.71%) in the double level ACDF group (Fig. 3a, b) and one (8.33%) in the double level Bryan group. There were no new posterior osteophytes nor did calcification of the ALL observe for any of the radiographs. Osteophyte enlargement was noted in two (7.69%) patients in the single level ACDF group (Fig. 4a, b), one (2.56%) in the single level Bryan group, four (14.28%) in the double level ACDF group and no case in the double level Bryan group. Disc space narrowing was the most common new radiographic finding. It was observed in four (15.38%) patients in the single level ACDF group, 3 (7.69%) in the single level Bryan group, nine (32.14%) in the double level ACDF group and 3 (25%) in the double level Bryan group (Table 8).
Fig. 2.
a Immediately post-op and b final follow-up radiographs showing new anterior osteophyte formation observed in one of the patients from our single level Bryan group
Fig. 3.
a Immediately post-op and b final follow-up radiographs showing new anterior osteophyte formation observed in one of our patients from our double level ACDF group
Fig. 4.
a Immediately post-op and b final follow-up radiographs showing osteophyte enlargement observed in one of our patients from our single level ACDF group
Table 8.
Summary of radiologic changes after surgery
| Single level ACDF (N = 26) | Single level Bryan (N = 39) | Double level ACDF (N = 28) | Double level Bryan (N = 12) | |
|---|---|---|---|---|
| New anterior osteophyte | 0 | 1 (2.56%) | 3 (10.71%) | 1 (8.33%) |
| New posterior osteophyte | 0 | 0 | 0 | 0 |
| Osteophyte enlargement | 2 (7.69%) | 1 (2.56%) | 4 (14.28%) | 0 |
| Calcification of ALL | 0 | 0 | 0 | 0 |
| Disc space narrowing | 4 (15.38%) | 3 (7.69%) | 9 (32.14%) | 3 (25%) |
| Upper level | 2(7.69%) | 1 (2.56%) | 4 (14.29%) | 0 |
| Implanted level | 0 | 0 | 0 | 0 |
| Lower level | 2 (7.69%) | 2 (5.13%) | 5 (17.86%) | 3 (25%) |
| Total of X-ray changes | 6 (23.07%) | 5 (12.82%) | 16 (57.14%) | 4 (33.33%) |
p = 0.05 set value for statistical significance using the mixed model
N total number of patients in each group
Overall, we noted six of 26 (23.07%) patients in the single level ACDF group developed new X-ray changes as compared to 5 of 39 (12.82%) in the single level Bryan group. Comparing the radiographic findings of patients who underwent double level surgeries, it was observed that in the double level ACDF group, 16 of 28 (57.14%) had radiographic changes in their X-ray while in the double level Bryan group 4 of 12 (33.33%) had new radiographic changes (Table 8).
Using the χ2 test at 95% confidence interval, the ACDF group was 3.5 times more likely to have radiological changes.
Discussion
For over 50 years, ACDF has been the treatment used for symptomatic cervical disc disease [11]. The advent of anterior plating has even further added to the success of fusion after decompression [20, 28]. It has been proven to clinically provide stability after decompression. However, despite it is long standing success, ACDF is not without complications as there have been reports of pseudoarthrosis, implant failure and more recently, adjacent level disease [4, 5, 11].
Different theories have been proposed for the cause of adjacent segment disease in patients undergoing ACDF. Matsunaga et al. [19] analyzed the strain distribution of intervertebral discs after anterior cervical disc fusion and showed an increase in longitudinal strain most frequently at the levels immediately adjacent to the fused segment. A biomechanical cadaveric cervical spine study by some authors noted motion compensation after fusion in different levels. They concluded that Increase in motion was compensated at segments immediately adjacent to a single-level fusion. Significant differences occurred at the level above the fusion site for the C3–C4 and C4–C5 fusion in both flexion and extension. When the lower levels (C5–C6, C6–C7) were fused, a significant amount of increased motion was observed at the levels immediately above and below the fusion. However, greater compensation occurred at the inferior segments than the superior segments for the lower level fusions (C5–C6, C6–C7) [25].
This theory is also supported by other in vitro studies that have shown that fusion at the operated level increases intersegmental motion and load and intradiscal pressure at the adjacent levels which are believed to induce progressive degeneration at these levels [1, 8].
In a 2-year clinical follow-up, Goffin et al. [12] identified a 92% rate of adjacent level radiologic degeneration after fusion over a mean of 8.6 years. The authors also noted a correlation between these radiographic findings and clinical deterioration. Furthermore, Hilibrand et al. [13] followed up 374 patients having a total of 409 anterior cervical arthrodesis for up to 21 years after anterior cervical fusion. They found symptomatic adjacent segment disease occurring at an average rate of 2.9% per year (range 0.0–4.8%). Survivorship analysis predicts 25.6% of patients (95% CI 20–32%) will have new onset of symptoms within 10 years of fusion.
It is partly because of this that the advent of the cervical disc replacement came about. By theoretically preserving motion and maintaining disc height, it may be possible to preserve the normal kinematics of the spine and maybe decrease the incidence of adjacent segment degeneration.
In 2005, Robertson et al. [23] did a prospective study that compared the incidence of radiologic changes and symptomatic adjacent level disease after fusion with an interbody cage or arthroplasty with the Bryan Artificial Cervical Disc. In the cage fusion series, the incidence of symptomatic adjacent level disease was statistically greater than that in the group treated with the artificial disc (p = 0.018), and the patients required a statistically greater number of medical treatments related to episodic symptoms of neck, shoulder, and arm pain attributed to new disc disease (p = 0.001, OR 35.8) [23].
Our study showed that 22 (40.74%) of the ACDF group developed radiographic adjacent level changes as compared to 9 (17.6%) of those who underwent cervical disc arthroplasty. Interestingly, we noted that in those patients who underwent double level ACDF surgeries, the number of patients noted to have adjacent degenerative changes [16 patients (57.14%)] were more than double those who underwent single level ACDF surgeries [6 patients (23.07%)]. Likewise, the percentage of patients that showed adjacent segment radiologic changes was also more than double comparing those that underwent single level Bryan disc replacements [5 patients (12.82%)] against double level disc replacements [4 patients (33.33%)].
As a whole, results of this study showed that radiologic evidence of adjacent level disease was 3.5 times more likely for our ACDF group at the time of last follow-up.
These new radiographic evidence of adjacent level disease were, however, not translated symptomatically as there was no difference between our two arms in both the VAS and NDI scores at a mean of 19 months follow-up. Though all of our groups had decreased VAS and NDI scores on last follow up, we believe it is due to the initial surgical decompression and removal of pathologically herniated discs.
Results of our study also show that even after a mean of 19 (12–40) months post surgery, the other parameters related with kinematics such as ROM, FSU and overall sagittal alignment were relatively well maintained in the Bryan group compared to the ACDF group for both single and double level surgeries at the operated site and adjacent levels. We think these factors might be related with the development of radiographic change at adjacent levels.
This is similar to a study by Nabhan et al. [21] where radiostereometric analysis was used to quantify intervertebral motion in a group treated with cage and plate construct compared to a group with disc prosthesis. They noted that there was a significant difference in the segmental motion between the fusion group and the arthroplasty group after 3–24 weeks (p = 0001).
Likewise, the study by Goffin et al. [12] reported excellent, good, or fair outcomes in 44 of 49 patients (90%) implanted with a single level Bryan disc. Furthermore, cervical movement was preserved in 88% of patients treated with single level and 86% of those with double level prosthesis at 1 year.
In terms of intervertebral disc height measurements, the Bryan group maintained these measurements better compared to the ACDF group nearly at all levels. Whether in single or double level surgeries, the Bryan group was able to maintain its interbody height better than the ACDF group. As evidenced by our results, changes in the ACDF group were more variable especially on post-operative measurements. This could be caused by the difference in the operative procedure itself in doing fusion surgery compared to implanting a Bryan disc.
The need for an interbody graft at the operated level, whether it is a cage or bone graft, used to be a bigger size than the original disc height to provide inherent stability. This is necessary whether or not it is supplemented by a plate. In these cases, distraction may be quite variable. Therefore, this could possibly cause added movement and stress at adjacent levels.
In contrast, implanting a Bryan disc uses more standardized tools such as a milling-jig etc., to prepare the superior and inferior endplates at the intended operative site, decreasing surgeon related factors in preparing the endplates. This is coupled with pre-operative and intra-operative measurements to determine the proper size of the prosthesis thereby maintaining kinematics almost the same as pre-operative measurements.
Most biomechanical and kinematic studies suggest that it is the preservation of motion at the operative site that helps lessen incidence of adjacent level degeneration.[1, 8, 14] To the best of our knowledge, there have been no studies that pertaining to maintenance of original disc height as a possible factor to decrease adjacent segment disease. Our theory is that significant changes from the original interbody height may alter the overall kinematics at adjacent levels as well as overall sagittal alignment. This may cause compensation from adjacent segments and more strain of the supporting ligaments such as the anterior and posterior longitudinal ligaments as well as added load on adjacent discs and facet joints.
Furthermore, maintenance of interbody height is important in that, any changes may denote a possible loss of cervical lordosis or new onset segmental kyphosis [16]. These changes especially at adjacent levels may connote an adjacent disc degeneration.
Although there has already been a significant difference between our two groups in terms of radiographic adjacent segment changes, we believe a longer follow-up period is needed to adequately assess if this difference in radiographic findings will have bearing clinically.
Maintenance of parameters measured in this study such as ROM, overall sagittal balance, FSU, interbody height are all related to normal cervical kinematics. In this study, most of these parameters were relatively better maintained in our Bryan group compared to our ACDF group (Table 9). Even though not all these parameters were found to be significant, these observations of ours might help us to possibly decrease the chances of developing adjacent level disease in the long term. This study suggests the possibility of cervical disc replacement as a worthy alternative to fusion in terms of reducing adjacent level degeneration.
Conclusion
Clinical status of both groups, regardless of the number of levels, showed improvement. Although clinical outcomes between the two groups were not significantly different at final follow-up, radiographic parameters, namely ROM and intervertebral heights at the operated site, some adjacent levels as well as FSU and overall sagittal alignment of the cervical spine were relatively well maintained in our Bryan group compared to our ACDF group. We surmise that to a certain degree, the maintenance of these parameters could contribute to reduce development of adjacent level change. Noteworthy is that radiographic change was 3.5 times more observed for ACDF surgeries. A longer period of evaluation is needed, to see if all these radiographic changes will translate to symptomatic adjacent level disease.
References
- 1.Alund M, Larsson SE. Three dimensional analysis of neck motion. A clinical method. Spine. 1990;15:87–91. doi: 10.1097/00007632-199002000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Bartels RH, Donk R, Wilt GJ, et al. Design of the PROCON trial: a prospective, randomized multi-center study comparing cervical anterior discectomy without fusion, with fusion or with arthroplasty. BMC Musculoskelet Disord. 2006;7:85–91. doi: 10.1186/1471-2474-7-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boden SD, Balderston RA, Heller JG, et al. An AOA critical issue. Disc replacements: this time will we really cure low-back and neck pain. J Bone Joint Surg Am. 2004;86:411–422. [PubMed] [Google Scholar]
- 4.Bohlman HH, Emery SE, Goodfellow DB, et al. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy: long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75:1298–1307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Brodke DS, Zdeblick TA. Modified Smith-Robinson procedure for anterior cervical discectomy and fusion. Spine. 1992;17(Suppl):427–430. doi: 10.1097/00007632-199210001-00014. [DOI] [PubMed] [Google Scholar]
- 6.Clements DH, O’Leary PF. Anterior cervical discectomy and fusion. Spine. 1990;15:1023–1025. doi: 10.1097/00007632-199015100-00008. [DOI] [PubMed] [Google Scholar]
- 7.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 8.Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine. 2002;27:2431–2434. doi: 10.1097/00007632-200211150-00003. [DOI] [PubMed] [Google Scholar]
- 9.Emery SE, Bolestra MJ, Banks MA, et al. Robinson anterior cervical fusion: comparison of the standard and modified techniques. Spine. 1994;19:660–663. doi: 10.1097/00007632-199403001-00004. [DOI] [PubMed] [Google Scholar]
- 10.Fong SY, DuPlessis SJ, Hurlbert J, et al. Design limitations of Bryan disc arthroplasty. Spine J. 2006;6:233–241. doi: 10.1016/j.spinee.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 11.Goffin J, Geusens E, Vantomme N, et al. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech. 2004;17:79–85. doi: 10.1097/00024720-200404000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Goffin J, Pointillart V, Lind B, et al. Two-year clinical results from a multicenter study of the Bryan cervical disc system. Proceedings of the NASS 19th annual meeting. Spine J. 2004;4:3S–199S. doi: 10.1016/j.spinee.2004.05.085. [DOI] [Google Scholar]
- 13.Hilibrand A, Carlson G, Palumbo M, et al. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg. 1999;81:519–528. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Ishihara MK, Kawaguchi H, et al. Adjacent segment disease after anterior cervical interbody fusion. Spine J. 2004;4(6):624–628. doi: 10.1016/j.spinee.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 15.Kaiser MG, Haid RWJ, et al. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery. 2002;50:229–236. doi: 10.1097/00006123-200202000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Kao FC, Niu CC, Chen LH, et al. Maintenance of interbody space in one- and two-level anterior cervical interbody fusion. Clin Orthop Relat Res. 2005;430:108–116. doi: 10.1097/01.blo.0000142626.90278.9e. [DOI] [PubMed] [Google Scholar]
- 17.Lafuente J, Casey AT, Petzold A, et al. The Bryan cervical disc prosthesis as an alternative to arthrodesis in the treatment of cervical spondylosis. J Bone Joint Surg Br. 2005;87:508–512. doi: 10.1302/0301-620X.87B4.15436. [DOI] [PubMed] [Google Scholar]
- 18.Lin EL, Wang JC. Total disk arthroplasty. J Am Acad Orthop Surg. 2006;14:705–714. doi: 10.5435/00124635-200612000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Matsunaga S, Kabayama S, Yamamoto T, et al. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine. 1999;24:60–675. doi: 10.1097/00007632-199904010-00011. [DOI] [PubMed] [Google Scholar]
- 20.Mobbs RJ, Rao P, Chandran NK. Anterior cervical discectomy and fusion: analysis of surgical outcome with and without plating. J Clin Neurosci. 2007;14(7):639–642. doi: 10.1016/j.jocn.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 21.Nabhan A, Ahlhelm F, Pitzen T, et al. Disc replacement using Pro-Disc C versus fusion: a prospective randomised and controlled radiographic and clinical study. Eur Spine J. 2007;16:423–430. doi: 10.1007/s00586-006-0226-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park JB, Cho YS, Riew D. Ossification in patients with an anterior cervical plate. J Bone Joint Surg Am. 2005;3:558–565. doi: 10.2106/JBJS.C.01555. [DOI] [PubMed] [Google Scholar]
- 23.Robertson JT, Papadopoulos SM, Traynelis VC. Assessment of adjacent-segment disease in patients treated with cervical fusion or arthroplasty: a prospective 2-year study. J Neurosurg Spine. 2005;3:417–423. doi: 10.3171/spi.2005.3.6.0417. [DOI] [PubMed] [Google Scholar]
- 24.Robinson RA, Smith GW. Antero-lateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp. 1955;96:223–224. [Google Scholar]
- 25.Schwab JS, Diangelo DJ, Foley KT. Motion compensation associated with single-level cervical fusion: where does the lost motion go? Spine. 2006;31(21):2439–2448. doi: 10.1097/01.brs.0000239125.54761.23. [DOI] [PubMed] [Google Scholar]
- 26.Seo M, Choi D. Adjacent segment disease after fusion for cervical spondylosis: myth or reality? Br J Neurosurg. 2008;22(2):95–99. doi: 10.1080/02688690701790605. [DOI] [PubMed] [Google Scholar]
- 27.Shim CS, Lee SH, Park HJ, et al. Early clinical and radiologic outcomes of cervical arthroplasty with Bryan cervical disc prosthesis. J Spinal Disord Tech. 2006;19:465–470. doi: 10.1097/01.bsd.0000211235.76093.6b. [DOI] [PubMed] [Google Scholar]
- 28.Traynelis VC. The prestige cervical disc. Neurosurg Clin N Am. 2005;16:621–628. doi: 10.1016/j.nec.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 29.Wang JC, McDonough PW, et al. Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion. Spine. 2000;25:41–45. doi: 10.1097/00007632-200001010-00009. [DOI] [PubMed] [Google Scholar]
- 30.Wang JC, McDonough PW, et al. Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. Spine. 2001;26:643–647. doi: 10.1097/00007632-200103150-00015. [DOI] [PubMed] [Google Scholar]
- 31.White AA, Panjabi MM. Update on the evaluation of instability of the lower cervical spine. Instr Course Lect. 1987;36:513–520. [PubMed] [Google Scholar]
- 32.Williams JL, Allen MB, Harkess JW. Late results of cervical discectomy and interbody fusion: some factors influencing the results. J Bone Joint Surg Am. 1968;50:277–286. doi: 10.2106/00004623-196850020-00006. [DOI] [PubMed] [Google Scholar]
- 33.Yoon DH, Yi S, Shin HC, et al. Clinical and radiological results following cervical arthroplasty. Acta Neurochir (Wien) 2006;148:943–950. doi: 10.1007/s00701-006-0805-6. [DOI] [PubMed] [Google Scholar]