Abstract
Unicompartmental changes in the knee of a young athlete remains a difficult and controversial problem in orthopaedics. Excessive premature loading of articular cartilage, most often the result of a knee injury, has been shown to result in increased degenerative changes and pain in the younger patient. Instability may also contribute to the degeneration of cartilage and must therefore be considered in the treatment of osteoarthritis in the young adult. High tibial osteotomy has been described as a treatment option for malalignment in the older, less active adult and has shown promising results in a younger, more active population. Osteotomies for instability are more controversial and should be considered in more complex injury patterns.
Introduction
High tibial osteotomy was first described in 1958 as a successful treatment for moderate to severe unicompartmental, degenerative arthritis of the knee associated with angular deformity [1]. Malalignment is frequently associated with knee arthrosis and can influence the mechanical load through either the medial or lateral compartment. The increased stress on the articular cartilage may lead to a higher probability of developing arthritis. Many studies have analysed the results of this operation with respect to age, activity, gender, degree of arthritic change, weight, previous injury treatment, and preoperative and postoperative angulation, in an effort to identify the risk factors for failure [2–5]. Ligamentous injuries in the setting of varus alignment may also have a higher rate of failure as soft tissue grafts may stretch out over time in this setting. The goal of an osteotomy, regardless of anatomical site or technique, is to reposition the weight bearing line as near normal as possible to reduce the stress through the medial and lateral compartments or the ligamentous structures. Findings indicate that factors predicting favourable outcomes include decreased relative weight, increased angle correction, and lower overall level of disease. For the younger, active patient with angular deformity beyond the average range of physiological variation and/or chronic instability, osteotomy remains the procedure of choice.
Osteoarthritis of the knee is generally considered to be a mechanical phenomenon. In the young adult, pathological phenomena such as meniscal injury or menisectomy, osteochondral injury, and ligamentous insufficiency can predispose an individual to develop arthritis [6]. Knee malalignment, whether induced by injury or underlying anatomical variability, has been shown to place abnormal stresses on the articular cartilage of an affected compartment and promote the development of these changes [7–10].
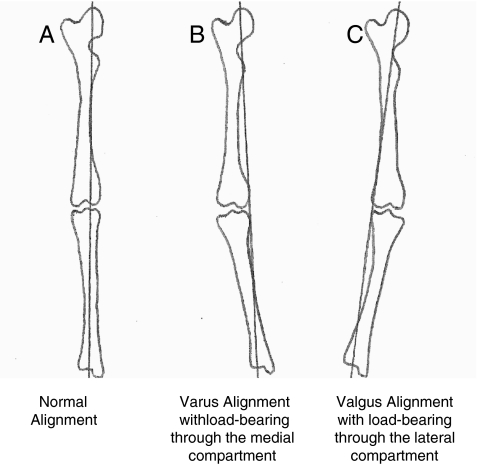
The normal anatomical load-bearing axis of the knee ranges from five to seven degrees of valgus (see Fig. 1). The medial side of the knee transmits 60% of the force through the joint. The remaining 40% is transmitted through the lateral compartment. Instability further increases the load by adding lateral thrust or an adduction moment varying somewhat with gait pattern [11]. Younger patients may be more prone to theses changes resulting from injury in an isolated compartment, thus altering the biomechanical axis and accelerating this process.
Fig. 1.
Alignment drawn by authors
Indications and contraindications
The indications for an osteotomy are malalignment with arthrosis, and/or instability, with or without an articular cartilage procedure. Morrey stated that patients with secondary degenerative arthritis, a varus knee, and localised medial joint pain are also candidates for an osteotomy [12]. Total joint replacement remains a viable alternative for the older, less active patient, but long-term outcomes in the young adult have been less reliable and more complex. As a result, clinicians have recommended osteotomy as a means of altering malalignment to more evenly distribute these forces over both the medial and lateral compartment and delay or prevent degenerative changes in this population.
Contraindications for HTO include the use of nicotine products because of the high risk of nonunion, particularly with medial open wedge osteotomies. HTO should be avoided in knees that demonstrate larger areas (15 × 15 mm) of exposed bone on both the tibial and femoral surfaces according to Markolf et al. [13]. Relative contraindications include body weight greater than 90 kg, severe patellofemoral symptoms, or patients with abnormal patella infera or alta since an osteotomy may increase the forces on articular cartilage in these patients [14].
History
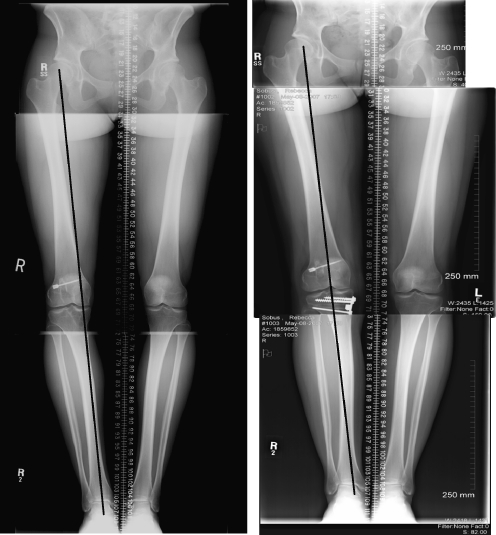
Age, weight, and activity level should be assessed in all patients as selection of appropriate surgical candidates may be influenced by these factors. Patients with unicompartmental arthritis generally complain of localised knee pain. A history of injury or previous surgery should be sought out. It is important to delineate the nature, location, and duration of pain symptoms. Patients with a varus-angulated ACL-deficient knee may complain of instability and medial-sided pain. Varus stress places increased force on the medial compartment and stretches the lateral stabilising structures as well as the ACL. In Fig. 2 the patient had an ACL deficient knee following a previous ACL reconstruction with medial joint line pain.
Fig. 2.
ACL deficient knee with varus angulation. Pre- and post-op radiographs
Pain may be vague in nature and related to repetitive, high-stress weight bearing activities such as running or jumping. Stiffness may or may not accompany pain, but more frequently occurs after prolonged immobilisation. More chronic symptoms may be more difficult to characterise, and may occur with lesser activities. Patients in this category will most often demonstrate more advanced disease. Advanced cartilage degeneration leads to advanced clinical symptoms and should be correlated with radiographic findings.
Physical examination
Examination of affected patients should include the following assessments: gait, stance, range of motion, localisation of tenderness, ligamentous stability, neurological evaluation, and lower extremity alignment. Comprehensive physical examination should include a patellofemoral evaluation, medial tibiofemoral crepitus, tenderness of the lateral soft tissues, gait abnormalities during walking and running, and limits of motion or subluxation of the femoral tibial articulation. Classification as varus, valgus, or neutral alignment should be made. Unicompartmental osteoarthritis can be determined by localised joint line tenderness, crepitus, tenderness elicited with loading of the involved compartment, and joint space collapse, but may be related to loss of meniscal or cartilage height rather than true laxity. End point determination should be made to confirm integrity of the collateral ligaments.
Preoperative planning
The assessment of lower limb alignment is based on an examination of full standing radiographs. Double-stance, full-length anteroposterior radiographs that show both lower extremities from the femoral head to the ankle joint should be obtained. The knee should be flexed to five degrees to avoid the abnormal varus recurvatum position.
The following method was used to determine the corrective wedge on preoperative radiographs. First, the centres of the femoral head and tibiotalar joint are located on the full-length radiograph. The selected WBL coordinate of the tibial plateau is identified and marked. We usually place this at 62% of the width of the tibia, which will allow the WBL to pass through the lateral tibiofemoral compartment. One line is drawn from the centre of the femoral head to the tibial coordinate, and a second line is drawn from the centre of the tibiotalar joint to the tibial coordinate. The angle formed by the two intersecting lines represents the angular correction required to realign the WBL through this coordinate [15].
Surgical technique for medial opening wedge tibial osteotomy
We perform the surgery with the patient in the supine position using a tourniquet. Fluoroscopic imaging is used throughout the surgery. After the patient has received preoperative antibiotics, the surgical preparation is performed. An incision is made halfway between the tibial tubercle and the posteromedial border of the tibia. Dissection is then carried down to the sartorius fascia. The fascia is incised in line with the fibres of the pes anserinus tendons, which are then retracted medially, exposing the superficial medial collateral ligament. A periosteal elevator is used to retract the MCL medially, exposing the underlying tibial cortex. The patellar tendon is retracted laterally. The most superior fibres of the patellar tendon may be released to improve visualisation of the osteotomy site. A guide pin is placed under fluoroscopic guidance starting 4 cm distal to the medial tibial plateau and angling 1 cm to the lateral tibial plateau. Orientation of this pin is marked to determine the angle of the osteotomy. An oscillating saw is placed below and parallel to the guide pin to begin the osteotomy, taking care to only cut the medial and posteromedial cortex. Thin osteotomes are used to complete the osteotomy ending approximately 1 cm short of the lateral femoral cortex to maintain a lateral hinge. Larger osteotomes are then used to slowly open the osteotomy site. A calibrated osteotome is then used to open the osteotomy to the desired correction. A four-holed osteotomy plate (e.g. Puddu, EBI) is then placed into the osteotomy site; 6.5-cancellous screws are placed through proximal holes, taking care not to violate the articular surface; 4.5-cortical screws are then used to fill the distal holes. Tricortical auto- or allograft is then placed into the defect (see Figs. 3, 4, 5, 6).
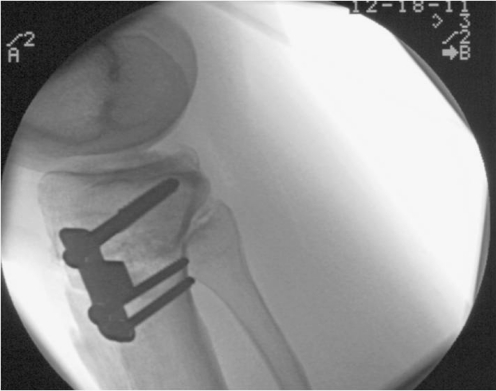
Fig. 3.
Preoperative radiograph demonstrating varus alignment
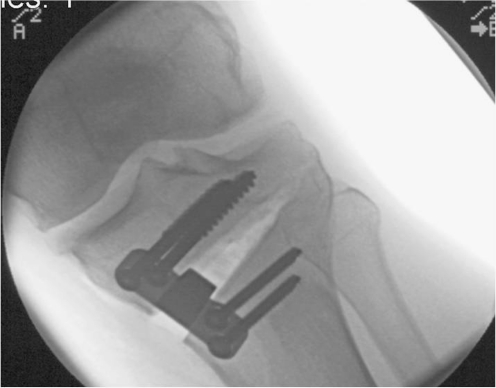
Fig. 4.
Intraoperative lateral radiograph after fixation
Fig. 5.
Intraoperative AP radiograph after fixation
Fig. 6.
Postoperative weight-bearing radiograph demonstrating correction of alignment
Postoperative rehabilitation
The patient is allowed touchdown weight-bearing in a knee brace for the first six weeks. Early knee range of motion is initiated. This has been shown to benefit joint healing and articular cartilage nourishment. Isometric quadriceps exercises are initiated. After six weeks, weight-bearing is increased. Full weight-bearing is allowed when radiographic consolidation has taken place [16] (see Fig. 7).
Fig. 7.
Final postoperative radiographs with bone consolidation a) AP view, b) lateral view
Outcomes for malalignment with osteoarthrosis
Successful long-term results for high tibial osteotomies have been linked to a number of patient and surgical factors. Risk factors that may contribute to a poor outcome include increased body weight, increased severity of the arthritis, and under/over correction of the patients’ alignment. Long-term results in the literature are often difficult to interpret because of the nonhomogenous patient populations, nonstandardised operations and rehabilitation protocols, and variety of indications for the procedures [17].
Closing wedge osteotomy studies primarily show modest survival rates at ten years after surgery. Ten-year survival rates range from 51% to 93.2%, with an average rate of 64% [4, 18–20]. The highest long-term survival rate for closing wedge osteotomy was reported by Koshino et al., who followed 75 knees up to 28 years postoperatively [21]. At the final follow-up examination, 93.2% of the patients had neither been converted to a knee arthroplasty nor complained of significant knee pain. The investigations of Naudie et al. [20] and Billings et al. [19] had the lowest ten-year survival rates of 51% and 53%, respectively. The probability of survival was reported to increase in patients who were younger than 50 years of age at the time of the HTO and who had preoperative knee flexion greater than 120 degrees [20]. Koshino et al. attribute the success of their procedure to the achievement of ten degrees of anatomical valgus, avoidance of a flexion contracture, and incorporation of a patellofemoral decompressive procedure in patients with pre-existing patellofemoral degeneration [21].
There is less data available regarding the success following opening wedge osteotomy. Three studies reported 84% [22], 89% [23] and 94% [24] survival rates five years after surgery. Hernigou et al. [25], in 1987, followed 93 knees for an average of 11.5 years. Good to excellent ratings were seen at five years in 90% of patients, which fell to 45% at ten years. Survival rates greater than ten years were available from two studies. First, Weale et al. had a survival rate of 63% in their series of 73 cases [23]. Second, survival rates of 85% were reported by Hernigou and Ma in a series of 203 knees [24]; they provided the only 15-year survival rate for opening wedge osteotomy at 68%.
Throughout the literature, pain relief has been uniformly reported as satisfactory. Aglietti et al. followed 61 patients clinically up to 21 years postsurgery and reported that 79% had no pain to only mild knee pain [18]. Aglietti et al. [5] followed 60 knees up to 21 years after surgery and reported that pain on walking was absent or mild in 55%, moderate in 27%, and severe in 18%.
Outcomes for malalignment with instability
Veterinary medicine has reported the beneficial results of high tibial osteotomy in several animal studies [26]; however, outcomes in human models have been more limited. Harner et al. reported their biomechanical results of changing tibial slope in a human cadaveric model and found that increasing tibial slope does not affect AP translation or in situ forces on the ACL, but did result in anterior positioning of the tibia. In 2008, LaPrade et al. [27] also reported that in cadaveric models following transection of posterolateral structures, high tibial osteotomy decreased varus and external rotation laxity.
Noyes et al. [28] reported a series of 41 patients with ACL deficiency and varus angulation and varying amounts of posterolateral corner deficiency who underwent closed tibial osteotomy and ACL reconstruction. Eighteen knees also underwent PLC reconstruction. Mean follow-up was 4.5 years. Reduced pain was reported in 71%, and residual instability was reported in 15%. Mean Cincinnati knee rating scores improved from 63 to 82 points. In a prospective clinical study Arthur et al. [29] reported that opening wedge medial tibial osteotomy in 21 patients with genu varum and instability was effective in controlling pain and instability symptoms in 38% of patients. Subsequent surgery to reconstruct the posterolateral corner resulted in lower Cincinnati knee rating scores. These patients were more likely to have suffered high velocity injuries. Instability remains a controversial indication for high tibial osteotomy.
Complications
The list of possible complications that can be associated with a high tibial osteotomy is numerous. Any complication that can occur with lower extremity surgery has been reported with realignment procedures. These include infection, neurovascular injury, delayed or nonunion, DVT, pulmonary embolus, and complications from taking autogenous bone graft. Specific intraoperative complications are a concern with osteotomies around the knee. These include intra-articular fractures, intra-articular screw placement, overcorrection, undercorrection, and violation of the opposite cortex resulting in instability of the osteotomy [30]. Failure to relieve pain and conversion to total knee arthroplasty can be considered long-term complications. There are no good long-term outcome studies.
Summary
Malalignment problems in the young patient can result in increased unicompartmental contact pressures and articular degeneration. It has been shown that early surgical intervention improves long-term outcomes. Total joint replacement has been shown to improve functional outcome scores in the older and less active patient; however, the younger, more active patient presents a difficult problem. Correction of malalignment in young patients with unicompartmental disease has shown promising results. More long-term prospective studies are needed to determine functional results.
With regard to instability, high tibial osteotomy remains controversial. Early studies have shown some promising results in patients with combined instability and malalignment for treatment of instability [31]. Furthermore, malalignment may be associated with early graft failure. Further study of this topic is warranted.
References
- 1.Jackson JP, Waugh W, Green JP. High tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg. 1969;51B:88–94. [PubMed] [Google Scholar]
- 2.Matthews LS, Goldstein SA, Malvitz TA, Katz BP, Kaufer H. Proximal tibial osteotomy: factors that influence the duration of satisfactory function. Clin Orthop. 1988;229:193–200. [PubMed] [Google Scholar]
- 3.Holden DL, James SL, Larson RL, Slocum DB. Proximal tibial osteotomy in patients who are fifty years old or less: a long-term follow up study. J Bone Joint Surg. 1988;70A:977–982. [PubMed] [Google Scholar]
- 4.Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy: a critical long-term study of eighty seven cases. J Bone Joint Surg Am. 1993;75(2):196–201. doi: 10.2106/00004623-199302000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Aglietti P, Rinonapoli E, Stringa G, Taviani A. Tibial osteotomy for the varus osteoarthritic knee. Clin Orthop. 1983;176:239. [PubMed] [Google Scholar]
- 6.Allen PR, Denham RA, Swan AV. Late degenerative changes after menisectomy. Factors affecting knee after operation. J Bone Joint Surg. 1984;66B:666–671. doi: 10.1302/0301-620X.66B5.6548755. [DOI] [PubMed] [Google Scholar]
- 7.Phillips MJ, Krackow KA. High tibial osteotomy and distal femoral osteotomy for valgus and varus deformity around the knee. Instr Course Lect. 1998;47:429–436. [PubMed] [Google Scholar]
- 8.Reimann I. Experimental osteoarthritis of the knee in rabbits induced by alterations by alteration of the load-bearing. Acta Orthop Scand. 1973;44:496–504. doi: 10.3109/17453677308989085. [DOI] [PubMed] [Google Scholar]
- 9.Tetsworth K, Paley D. Malalignment and degenerative arthropathy. Orthop Clin North Am. 1994;25:367–377. [PubMed] [Google Scholar]
- 10.Wu DD, Burr DB, Boyd RB, Radin EL. Bone and cartilage changes following experimental varus or valgus tibial angulation. J Orthop Res. 1990;8:572–585. doi: 10.1002/jor.1100080414. [DOI] [PubMed] [Google Scholar]
- 11.Coventry M. Upper tibial osteotomy for osteoarthritis. J Bone Joint Surg. 1985;67A:1136–1140. [PubMed] [Google Scholar]
- 12.Morrey BF. Upper tibial osteotomy for secondary osteoarthritis of the knee. J Bone Joint Surg Br. 1989;71:554–559. doi: 10.1302/0301-620X.71B4.2768296. [DOI] [PubMed] [Google Scholar]
- 13.Markolf KL, Bargar WL, Shoemaker SC, Amstutz HC. The role of joint load in knee stability. J Bone Joint Surg. 1981;63(4):570–585. [PubMed] [Google Scholar]
- 14.Tigani D, Ferrari D, Trentani P, Barbanti-Brodano G, Trentani F. Patellar height after high tibial osteotomy. Int Orthop. 2001;24:331–334. doi: 10.1007/s002640000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop. 1992;274:248–264. [PubMed] [Google Scholar]
- 16.Amendola A, Mrkonjic L, Clatworthy M, Kirkley A, Litchfield RB, Fowler PJ (1999) Opening wedge high tibial osteotomy using a Puddu distraction plate; focus on technique, early results and complications. Arthroscopy 15(5):S35 [DOI] [PubMed]
- 17.Amendola A, Bonasia DE (2009) Results of high tibial osteotomy: review of the literature. Int Orthop. doi:10.1007/s00264-009-0889-8 [DOI] [PMC free article] [PubMed]
- 18.Aglietti P, Buzzi R, Vena LM. High tibial osteotomy for medial gonarthrosis: a 10- to 21-year study. Am J Knee Surg. 2003;16(1):21–26. [PubMed] [Google Scholar]
- 19.Billings A, Scott DF, Camargo MP, Hofmann AA. High tibial osteotomy with a calibrated osteotomy guide, rigid internal fixation, and early motion: long-term follow-up. J Bone Joint Surg Am. 2000;82(1):70–79. doi: 10.2106/00004623-200001000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Naudie D, Bourne RB, Rorabeck CH, Bourne TJ. Survivorship of the high tibial valgus osteotomy: A 10- to 22-year follow-up study. Clin Orthop. 1999;367:18–27. [PubMed] [Google Scholar]
- 21.Koshino T, Yoshida T, Ara Y. Fifteen to twenty-eight years follow-up results of high tibial valgus osteotomy for osteoarthritic knee. Knee. 2004;11(6):439–444. doi: 10.1016/j.knee.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 22.Sterett WI, Steadman JR. Chondral resurfacing and high tibial osteotomy in the varus knee. Am J Sports Med. 2004;32(5):1243–1249. doi: 10.1177/0363546503259301. [DOI] [PubMed] [Google Scholar]
- 23.Weale AE, Lee AS, MacEachern AG. High tibial osteotomy using a dynamic axial external fixator. Clin Orthop. 2001;382:154–167. doi: 10.1097/00003086-200101000-00022. [DOI] [PubMed] [Google Scholar]
- 24.Hernigou P, Ma W. Open wedge tibial osteotomy with acrylic bone cement as bone substitute. Knee. 2001;8(2):103–110. doi: 10.1016/S0968-0160(00)00061-2. [DOI] [PubMed] [Google Scholar]
- 25.Hernigou P, Medevielle D, Debeyre J, Goutallier D. Proximal tibial osteotomy with varus deformity: a ten to thirteen year follow-up study. J Bone Joint Surg Am. 1987;69:332. [PubMed] [Google Scholar]
- 26.Kim S, Pozzi A, Kowaleski MP, Lewis DD. Tibial osteotomies for cranial cruciate ligament insufficiency in dogs. Vet Surg. 2008;37(2):111–125. doi: 10.1111/j.1532-950X.2007.00361.x. [DOI] [PubMed] [Google Scholar]
- 27.LaPrade RF, Engebretsen L, Johansen S, Wentorf FA, Kurtenbach C. The effect of proximal tibial opening wedge osteotomy on posterolateral knee instability: a biomechanical study. Am J Sports Med. 2008;36(5):956–960. doi: 10.1177/0363546507312380. [DOI] [PubMed] [Google Scholar]
- 28.Noyes F, Barber-Westin SD, Hewett TE (1999) High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Presented at the 66th annual meeting of the American Academy of Orthopaedic Surgeons, Anaheim, California, February 1999
- 29.Arthur A, LaPrade RF, Agel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee: a prospective clinical study. Am J Sports Med. 2007;35(11):1844–1850. doi: 10.1177/0363546507304717. [DOI] [PubMed] [Google Scholar]
- 30.Nelissen EM, van Langelaan EJ, Nelissen RGHH (2009) Stability of medial opening wedge high tibial osteotomy: a failure analysis. Int Orthop. doi:10.1007/s00264-009-0723-3 [DOI] [PMC free article] [PubMed]
- 31.Phisitkul P, Wolf BR, Amendola A. Role of high tibial and distal femoral osteotomies in the treatment of lateral-posterolateral and medial instabilities of the knee. Sports Med Arthroscopy. 2006;14(2):96–104. doi: 10.1097/01.jsa.0000212306.47323.83. [DOI] [PubMed] [Google Scholar]