Abstract
Sulcus deepening trochleoplasty is a technically demanding procedure with precise indications: high grade trochlear dysplasia with patellar instability and/or abnormal tracking. The main goal is to decrease the prominence of the trochlea and to create a new groove with normal depth, thus optimising patellar tracking. Associated abnormalities should be specifically treated. Recurrence of instability is very rare after this procedure and is more likely to result from missed associated abnormalities. Although results seem very good in terms of instability, further evidence is still needed since the groups of patients in the published series are heterogeneous. Trochleoplasty is not indicated for patellofemoral arthritis or pain. As any surgical procedure, sulcus deepening trochleoplasty is liable to complications.
Introduction
The normal trochlea is located in the anterior aspect of the distal femur. It is composed of two facets divided by a longitudinal groove, the trochlear sulcus. The lateral facet is the biggest; it extends more proximally than the medial facet and is more protuberant in the anteroposterior aspect. Proximally, the trochlea extends to the junction of the articular cartilage with the femoral anterior cortex, which is covered by adipose tissue and synovium. Distally, it is limited by the condylotrochlear grooves, one on each of the facets of the corresponding femoral condyle. The trochlear groove extends distally and laterally from the femoral axis [1, 2].
Dysplastic trochleas are shallow, flat or convex. It is easy to consider and define their abnormality in terms of function, or deviation from the normal pattern. These trochleas are not effective in constraining mediolateral patellar displacement. Radiological features are also easier to define and measure than those observed during the surgical procedures. It is fundamental, however, that the surgical mark of these trochleas is their abnormal shape (flat or convex). A bump in the superolateral aspect is also common.
Radiologic features
X-ray lateral projections of normal trochleas (obtained with perfect superimposition of both femoral condyles) will typically show the contour of the facets, and posterior to them, the line representing the bottom of the sulcus is visualised. The lateral facet is distinguished from the medial one by its more visible condylotrochlear groove, and by the greater opacity to the rays of the lateral condyle, which is more perpendicular than the medial to the X-ray beam in the lateral projection. The line representing the bottom of the sulcus is continuous with the intercondylar notch line, and extends anteriorly and proximally. It may end posterior to the condyles line (type A) or join the medial condyle line in the superior part of the trochlea (type B) [3].
On lateral projections, trochlear dysplasia is defined by the crossing sign, where the radiographic line of the trochlear sulcus crosses (or reaches) the projection of the femoral condyles. The crossing point represents the exact location where the deepest point of the trochlear sulcus reaches the same height as that of the femoral condyles, meaning that the trochlea becomes flat in this exact location. The position of the deepest point of the trochlear sulcus is also abnormal (prominent) in relation to the anterior femoral cortex. While in normal knees it is usually at a mean distance of 0.8 mm posterior to a line projected from the anterior femoral cortex, in knees with dysplastic trochlea its mean position is 3.2 mm forward the same line [4].
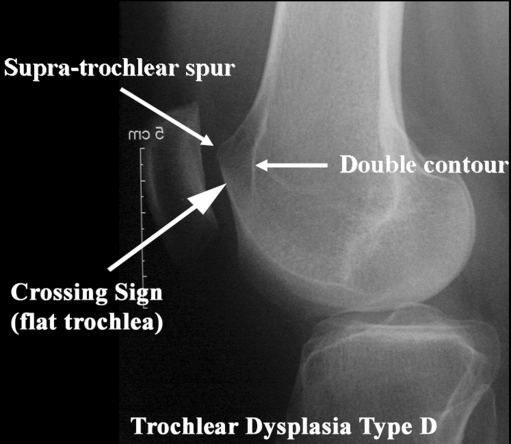
Two other features are typical of dysplastic trochleae in lateral views: the supratrochlear spur and the double-contour sign (Fig. 1). The supratrochlear spur corresponds to an attempt to contain the lateral displacement of the patella. The double-contour represents the medial hypoplastic facet, seen posterior to the lateral one in this projection. Based on these signs, trochlear dysplasia may be classified into four types [5, 6]:
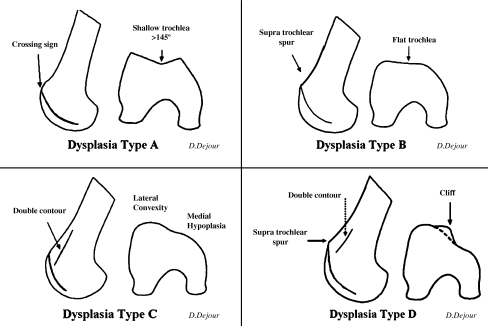
Type A: presence of the crossing sign in lateral true view. The trochlea is shallower than normal, but still symmetrical and concave.
Type B: crossing sign and trochlear spur. The trochlea is flat or convex in axial images.
Type C: presence of the crossing sign and, in addition, one can find the double-contour sign on the lateral view, representing the medial hypoplastic facet. There is no spur, and in axial views the lateral facet is convex and the medial hypoplastic.
Type D: combines all the mentioned signs, i.e. crossing sign, supratrochlear spur and double-contour sign. In the axial view, there is clear asymmetry of the height of the facets, also referred to as a cliff pattern (Fig. 2).
Fig. 1.
To analyse trochlear dysplasia a true profile is needed with a perfect superimposition of the posterior condyles. The three trochlear dysplasia signs are: the crossing sign, the supra-trochlear spur and the double-contour (which appears below the crossing sign)
Fig. 2.
Trochlear dysplasia classification according to D. Dejour. In type A, there is the crossing sign is present in lateral true view. The trochlea is shallower than normal, but still symmetrical and concave. Type B features include the crossing sign and trochlear spur. The trochlea is flat or convex in axial images. In type C there is a crossing sign, and in addition the double-contour sign representing sclerosis of the subchondral bone of the medial hypoplastic facet. On axial CT scan views, the lateral facet is convex. Type D combines all the mentioned signs: crossing sign, supratrochlear spur and double-contour sign going below the crossing sign. In axial CT scan views, there is a cliff pattern
In axial X-ray projections, dysplastic trochleae will show abnormally high congruence angles [7], and at times, no measurement can be made, since there is no sulcus. The subjective impression of the trochlear shape is also important, and should be taken in no more than 45° of knee flexion. Greater flexion angles show the lower part of the trochlea, which is anatomically more normal. Finally, any signs of patellar instability, like those evidenced in other projections and with other methods (abnormal lateral patellofemoral angle [8, 9], tilt [4], medial patellar bony avulsions, MPFL rupture, and others), serve as clues to the dysplasia diagnosis, since 96% of patients with at least one true patellar dislocation will present it [4].
The computed tomography scan will help the axial views and allow the assessment of associated features (patellar tilt, tibial tubercle–trochlear groove distance, femoral anteversion and external tibial torsion) that should be taken into consideration at the time of surgery. Magnetic resonance imaging is another modality in which dysplasia is well documented. The cartilaginous shape of the sulcus can be evaluated, and this is particularly interesting since the cartilaginous anatomy does not follow exactly the underlying bony anatomy [10]. However, in flat or convex trochlea, the bony and cartilaginous anatomies seem to match more frequently.
Surgical indications
Trochleoplasty indications are specific: high grade trochlear dysplasia with patellar instability and/or abnormal patellar tracking in the absence of established osteoarthritis, which would otherwise indicate a patellofemoral arthroplasty. Open growth plates are a contraindication to trochleoplasty.
The type of dysplasia should be observed when deciding the procedure, since not all procedures fit all deformities. Types B and D are the most suitable to deepening trochleoplasty. Lateral facet elevating trochleoplasty is advocated by some authors, and although no consensus of indication criteria exists, type C dysplasia would be the appropriate candidate for it. Type A dysplasia, in our opinion, does not merit any procedure.
As important as a specific indication are the evaluation and correction of associated abnormalities including tibial tubercle–trochlear groove distance (TT–TG), patella alta and patellar tilt. Specific procedures should address each abnormality. When performing trochleoplasties, it is our common approach to always perform an associated medial patellofemoral ligament (MPFL) reconstruction.
Surgical techniques
Trochleoplasty
This procedure was first described by Masse in 1978 [11]; it was modified and standardised by Henri Dejour in 1987. The main goal is to decrease the prominence of the trochlea and to create a new groove with normal depth. This procedure is technically more demanding than a lateral facet elevating trochleoplasty, but it is more anatomical. It has the advantage of treating the root cause of the dislocation by correcting the abnormal patterns underlying the different grades of trochlear dysplasia.
The procedure is performed under regional anaesthesia, supplemented with patient sedation. The patient is positioned supine. The entire extremity is prepared and draped, and incision is performed with the extremity flexed to 90 degrees. A straight midline skin incision is carried out from the superior patellar margin to the tibiofemoral articulation. The extremity is then positioned in extension and a medial full thickness skin flap is developed. The arthrotomy is performed through a modified mid-vastus approach with medial retinaculum sharp dissection starting over the 1–2 cm medial border of the patella, and blunt dissection of VMO fibres starting distally, at the patellar superomedial pole, extending approximately 4 cm into the muscle belly.
The patella is briefly everted for inspection of chondral injuries and adequate treatment if needed, and then retracted laterally. The trochlea is exposed. The peritrochlear synovium and periosteum are incised along their osteochondral junction, and reflected from the field using a periosteal elevator. The anterior femoral cortex should be visible to orientate the amount of deepening. Changing the degree of flexo-extension allows a better view of the complete operative field and avoids extending the incision.
Once the trochlea is fully exposed, the new version is planned and drawn with a sterile pen. The new trochlear groove is drawn using as starting point the intercondylar notch. From there, a straight line representing it is directed proximally and 3 to 6 degrees laterally. The superior limit is the osteochondral edge. Two divergent lines are also drawn, starting at the notch and passing proximally through the condylotrochlear grooves, representing lateral and medial facet limits. They should not enter the tibiofemoral joint (Fig. 3).
Fig. 3.

Drawing of the new trochlear limits; the medial facet is nearly nonexistent
The next step is accessing the under surface of the femoral trochlea. For this purpose, a thin strip of cortical bone is removed from the osteochondral edge. The width of the strip is similar to the prominence of the trochlea from the anterior femoral cortex (the bump). A sharp osteotome is used and gently tapped. A rongeur is used next to remove the bone.
Subsequently, cancellous bone must be removed from the under surface of the trochlea. A drill with a depth guide set at 5 mm is used to ensure uniform thickness of the osteochondral flap, thus maintaining an adequate amount of bone attached to the cartilage. The guide also avoids injuring the cartilage or getting too close to it, otherwise thermal injury could be produced. The shell produced must be sufficiently compliant to allow modelling without being fractured. Cancellous bone removal is extended up to the notch. More bone is removed from the central portion where the new trochlear groove will lie.
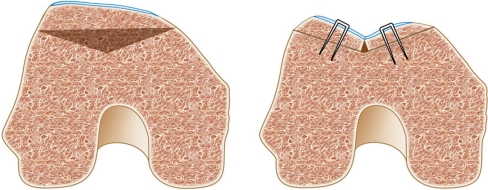
Light pressure should be sufficient to mould the flap to the underlying cancellous bone bed in the distal femur. The bottom of the groove and the external margin of the lateral facet should be cut to allow further modelling, and is achieved by gently tapping over a scalpel. If the correction obtained is satisfactory, the new trochlea is fixed with two staples, one in each side of the groove. The staples are fixed with one arm in the cartilaginous upper part of each facet, and the other arm in the anterior femoral cortex. Patellar tracking is tested and measurements may be obtained. Periosteum and synovial tissue are sutured to the osteochondral edge and anchored in the staples (Figs. 4 and 5).
Fig. 4.
Sulcus deepening trochleoplasty schematic model. Cancellous bone from the trochlear undersurface is removed to allow modelling (gray zone). The bone–cartilage flap is then modelled, and fixation is achieved with staples
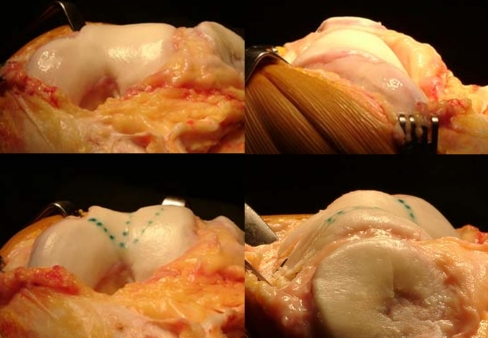
Fig. 5.
Trochlear shape before (above) and after (below) sulcus deepening trochleoplasty. The trochlear sulcus is restored and more “anatomical” shape is achieved
Postoperative care
The postoperative care will need to take into account the associated procedures, since the trochleoplasty is rarely carried out as an isolated procedure. Six weeks postoperatively, check radiographs, including AP and lateral views and an axial view in 30° of flexion, are taken (Figs. 6 and 7). After six months a CT scan is performed in order to document the correction obtained.
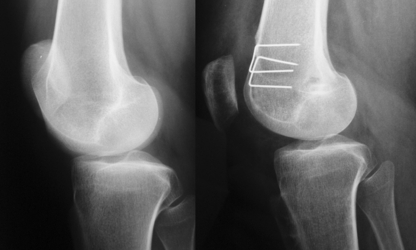
Fig. 6.
Sulcus deepening trochleoplasty: pre and postoperative lateral views. The supratrochlear spur resection can be observed and the patellar tilt is corrected
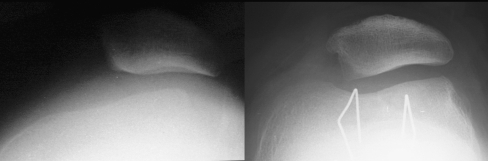
Fig. 7.
Sulcus deepening trochleoplasty: pre and postoperative axial views. The sulcus is almost absent in the preoperative view, and restored in the postoperative. Patellar tilt and subluxation are corrected
Results
Two series reviewing deepening trochleoplasty were published in the “10èmes Journées Lyonnaises de Chirurgie du Genou” in 2002.
The first group included 18 patients, whose patellar surgery for instability had failed. The mean age at surgery was 24 years, there were no patients lost to follow-up. The mean follow-up was six years (range 2–8 years). The revision surgery was indicated six times for pain and 12 times for recurrence of instability. The average number of operations before the trochleoplasty was two. The deepening trochleoplasty was associated with a tibial tubercle medialisation in eight patients, in six to a tibial tubercle distalisation and in 18 to a VMO plasty. All patients were reviewed radiographically and clinically with the IKDC form. Sixty-five percent were satisfied or very satisfied. The knee stability was rated A 13 times and B 5 times. Twenty-eight percent of the patients had residual pain, and this could be correlated to the cartilage status at surgery. Two patients developed patellofemoral arthritis. The mean patellar tilt was 35° (range 18°–48°) in the preoperative setting, and improved to 21° (range 11°–28°) with the quadriceps relaxed and 24° (range 16°–32°) with the quadriceps contracted after the surgery.
In the second group there were 44 patients. They had no previous of patellofemoral surgery. The mean follow-up was seven years (range 2–9 years). Twenty-two tibial tubercle medialisation, 26 distalisations and 32 VMO plasties were associated at the time of surgery. These patients were also reviewed radiographically and clinically with the IKDC form. Eighty-five percent were satisfied or very satisfied. The knee stability was rated A 31 times and B 13 times. Five percent had residual pain, but this could not be correlated with the cartilage status at surgery. No patellofemoral arthritis was noted. The mean patellar tilt preoperatively was 33° (range 24°–52°), and improved postoperatively to 18° (range 9°–30°) with the quadriceps relaxed and 22° (14°–34°) with the quadriceps contracted.
Verdonk et al. [12] described 13 procedures (deepening trochleoplasty) with a mean follow-up of 18 months. Patients were assessed using the Larsen–Lauridsen score considering pain, stiffness, patellar crepitus, flexion and loss of function. Seven patients scored poorly, three fairly and three well. On a subjective scoring system, however, six patients rated the result as very good, four as good and one as satisfactory. Only two patients found the result inadequate and would never undergo the procedure again. Thus, 77% were satisfied with the procedure.
Donnel et al. [13] described 15 patients (17 knees) who underwent deepening trochleoplasty with a mean follow-up of three years. Trochleoplasty was indicated if there was a boss greater than 6 mm, and associated procedures were performed as required. Of the 17 knees, nine had undergone previous surgery for patellar instability. The boss height was reduced, postoperatively, from an average of 7.5 mm to 0.7 mm. Tracking became normal in 11 knees and six had a slight J-sign. Seven knees had mild residual apprehension. Seven patients were very satisfied, six were satisfied, and two were disappointed. The Kujala score improved from an average of 48 to 75 out of 100.
A different procedure (Bereiter’s trochleoplasty [14]) has also been documented in two series by Von Knoch et al. [15] and Schottle et al. [16] with good results.
Complications
Patients submitting to trochleoplasty are at risk for the same complications inherent to any surgical procedure, e.g. infection, deep venous thrombosis, etc. Specific complications include trochlear necrosis, cartilage damage, incongruence with the patella, and under or overcorrection. Schottle et al. performed biopsies in three patients after trochleoplasty, showing cartilage cell viability and flap healing. They concluded that the risk of cartilage damage is low [17].
Incongruence with the patella is another concern. Studies with longer follow-ups are needed before any assumptions can be made about its consequences. Also, arthritis development is multifactorial, and all patients operated upon for patellofemoral instability seem more prone to degeneration than those treated conservatively.
Arthrofibrosis incidence varies between series, but is always a possibility in patellofemoral surgery. Verdonk et al. [12] reported five cases in 13 patients, while von Knoch [15] reported that all patients had full range of motion at the final visit. The number of previous or associated procedures is variable, and this can interfere with data interpretation.
Recurrence of instability is very rare after this procedure, and is more likely to result from missed associated abnormalities. The procedure's results for pain are not consistent, and although it seems to decrease pain, some patients may complain of worsening.
Conclusion
Sulcus deepening trochleoplasty is a technically demanding procedure with precise indications. It has the advantage of addressing one of the major causes of patellar instability—trochlear dysplasia—but associated abnormalities should also be treated. As any surgical procedure, complications are a risk. It should not be done for pain or in the presence of osteoarthritis.
References
- 1.Amis AA. Current concepts on anatomy and biomechanics of patellar stability. Sports Med Arthrosc. 2007;15:48–56. doi: 10.1097/JSA.0b013e318053eb74. [DOI] [PubMed] [Google Scholar]
- 2.Shih YF, Bull AM, Amis AA. The cartilaginous and osseous geometry of the femoral trochlear groove. Knee Surg Sports Traumatol Arthrosc. 2004;12:300–306. doi: 10.1007/s00167-003-0414-3. [DOI] [PubMed] [Google Scholar]
- 3.Dejour H, Walch G, Neyret P, Adeleine P. Dysplasia of the femoral trochlea. Rev Chir Orthop Reparatrice Appar Mot. 1990;76:45–54. [PubMed] [Google Scholar]
- 4.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 5.Tavernier T, Dejour D. Knee imaging: what is the best modality. J Radiol. 2001;82(387–405):407–388. [PubMed] [Google Scholar]
- 6.Dejour D, Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc. 2007;15:39–46. doi: 10.1097/JSA.0b013e31803035ae. [DOI] [PubMed] [Google Scholar]
- 7.Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391–1396. [PubMed] [Google Scholar]
- 8.Laurin CA, Dussault R, Levesque HP (1979) The tangential X-ray investigation of the patellofemoral joint: X-ray technique, diagnostic criteria and their interpretation. Clin Orthop Relat Res 144:16–26 [PubMed]
- 9.Laurin CA, Levesque HP, Dussault R, Labelle H, Peides JP. The abnormal lateral patellofemoral angle: a diagnostic roentgenographic sign of recurrent patellar subluxation. J Bone Joint Surg Am. 1978;60:55–60. [PubMed] [Google Scholar]
- 10.Staubli HU, Durrenmatt U, Porcellini B, Rauschning W. Anatomy and surface geometry of the patellofemoral joint in the axial plane. J Bone Joint Surg Br. 1999;81:452–458. doi: 10.1302/0301-620X.81B3.8758. [DOI] [PubMed] [Google Scholar]
- 11.Masse Y. Trochleoplasty. Restoration of the intercondylar groove in subluxations and dislocations of the patella. Rev Chir Orthop Reparatrice Appar Mot. 1978;64:3–17. [PubMed] [Google Scholar]
- 12.Verdonk R, Jansegers E, Stuyts B. Trochleoplasty in dysplastic knee trochlea. Knee Surg Sports Traumatol Arthrosc. 2005;13:529–533. doi: 10.1007/s00167-004-0570-0. [DOI] [PubMed] [Google Scholar]
- 13.Donell ST, Joseph G, Hing CB, Marshall TJ. Modified Dejour trochleoplasty for severe dysplasia: operative technique and early clinical results. Knee. 2006;13:266–273. doi: 10.1016/j.knee.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 14.Bereiter H, Gautier E. Die trochleaplastik als chirurgische Therapie der rezidivierenden Patellaluxation bei Trochleadysplasie des Femurs. Arthroskopie. 1994;7:281–286. [Google Scholar]
- 15.Knoch F, Bohm T, Burgi ML, Knoch M, Bereiter H. Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia. A 4- to 14-year follow-up study. J Bone Joint Surg Br. 2006;88:1331–1335. doi: 10.1302/0301-620X.88B10.17834. [DOI] [PubMed] [Google Scholar]
- 16.Schottle PB, Fucentese SF, Pfirrmann C, Bereiter H, Romero J. Trochleaplasty for patellar instability due to trochlear dysplasia: A minimum 2-year clinical and radiological follow-up of 19 knees. Acta Orthop. 2005;76:693–698. doi: 10.1080/17453670510041781. [DOI] [PubMed] [Google Scholar]
- 17.Schottle PB, Schell H, Duda G, Weiler A. Cartilage viability after trochleoplasty. Knee Surg Sports Traumatol Arthrosc. 2007;15:161–167. doi: 10.1007/s00167-006-0148-0. [DOI] [PubMed] [Google Scholar]