Abstract
A total of 29 consecutive knee joint arthroplasties in 24 patients who underwent previous high tibial osteotomy (HTO) for medial unicompartment osteoarthritis of the knee and followed up for a mean of 97 months were compared with a control group of 28 patients with 29 primary total knee arthroplasty (TKA) without previous HTO. Results for the osteotomy group were satisfactory in 96.5% of cases. In one patient loosening of the implant occurred after 37 months, which required prosthesis revision. Three patients underwent a further operation of secondary patella resurfacing for patella pain. The group without osteotomy reported a similar percentage of satisfactory results.
Introduction
Proximal tibial osteotomy is an established method for treating the varus−osteoarthritic knee. Rationale for the operation is based on mechanical axis change of the lower limb, with load stress transfer from the pathological medial compartment to the still healthy lateral side [1, 2]. Most clinical studies report a high percentage of short-term positive results. Nevertheless, the results tend to deteriorate gradually over time, and as tibial osteotomy is indicated in young and active patients, many subsequently have to undergo knee joint arthroplasty [3–9].
The clinical and radiographic results of knee joint arthroplasty performed after tibial osteotomy vary considerably. Some authors [10–12] report results similar to those of primary joint arthroplasty, whereas others [13–17] describe worse results and a higher number of complications in cases previously treated by tibial osteotomy. In addition, a review of the literature shows greater difficulty in the execution of the surgical operation.
The aim of our study was to assess patients treated by knee arthroplasty after a previous operation of tibial osteotomy and to compare these cases with a cohort of primary total knee arthroplasty (TKA).
Materials and methods
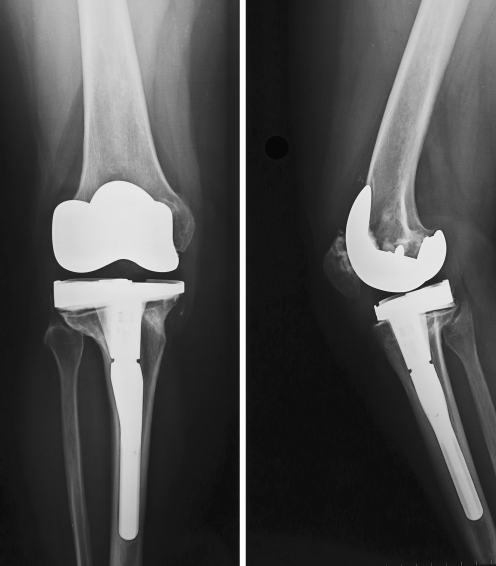
At our Institution, all patients who underwent TKA have been followed up prospectively since 1994. A total of 606 procedures were performed up to 2005. During that period, we identified 24 patients who had previously undergone high tibial osteotomy (HTO). Five of these patients were treated bilaterally, bringing the total number of prosthetic implants studied to 29. All patients who were followed up for a mean of 97 (range 36−156) months constitute our study group. The group included 19 women and five men. Seventeen cases involved the right side and 12 the left. Mean age at the time of proximal tibial osteotomy was 55 (median 56, range 46–63) years. Age at the time of TKA ranged between 52 and 80 (mean 68.5, median 64) years. Mean time interval between the two operations was 100.7 (median 96, range 34–124) months. The mechanical axis of the lower limb before arthroplasty varied between 15° of varus deviation and 15° of valgus deviation (mean 0°). The tibial osteotomy was performed using two different techniques: 19 lateral subtraction osteotomies (closing-wedge osteotomy), ten medial addition osteotomies and homoplastic graft (opening-wedge osteotomy). Types of prostheses implanted were 29 NexGen LPS (Zimmer Inc, Warsaw, IN, USA). In two cases, a NexGen modular tibial component with intramedullary stem and metal wedge was used to fill the large bone defect secondary to the osteotomy (Fig.1a–b). This index group was matched with a control group of 29 primary total knee arthroplasties in 28 patients selected from the same cohort and without a history of HTO.
Fig. 1.
a Preoperative planning (conventional tibial templating) for pronounced deformity and bone-stock loss secondary to high tibial osteotomy (HTO). b Modular tibial component with intramedullary stem and metal wedge
The match was made for age at the time of arthroplasty, American Knee Society (AKS) score before TKA, preoperative deformity in the frontal view and length of follow-up period (Table 1).
Table 1.
Data used to match patients with previous high tibial osteotomy (HTO) (index group) and patients with primary total knee arthroplasty (TKA) (control group)
| Index (SD) | Control (SD) | Significance | ||
|---|---|---|---|---|
| Age | 68.5y (7.5) | 71y (5.4) | NS a | |
| AKS | ||||
| AKSS | 38.5 (9.7) | 35 (14.6) | NS a | |
| AKFS | 47 (13.1) | 45 (22.6) | NS a | |
| Alignment | 0° (9.1) | 3° (9.4) | NS b | |
| FU | 97 m (28.4) | 97 m (27.1) | NS a | |
SD standard deviation, AKS American Knee Society, AKSS American Knee Society Knee Score, AKFS American Knee Society Functional Score, FU follow-up
aMann−Whitney test
bOne-way analysis of variance
The indication for TKA in all patients was symptomatic osteoarthritis. In all patients, a NexGen LPS prosthesis was implanted. To assess the results, we adopted the clinical and radiographic criteria proposed by the AKS. The AKS Clinical Rating System [18] is subdivided into two scores: Knee Score (AKSS) and Functional Score (AKFS). The AKSS assesses only the knee joint and is based on three main clinical parameters: pain, joint stability and range of movement expressed as positive values and, if present, other parameters, i.e. fixed deformity in flexion, extension deficit and malalignment in double stance that are expressed as negative values to be subtracted. The AKFS is based on the patient’s perception of general knee function in specific activities: it assesses walking ability and ascending/descending stairs as positive values that must be subtracted from the negative value, if present, which is represented by the need to use to walking aids. The best score, both for specific and general knee function, is 100 points. A score between 85 and 100 points is considered excellent, 70−84 good, 60−69 fair and <60 negative.
All the patients were assessed pre-operatively and at follow-up (three, six and 12 months and then yearly) by horizontal radiography of the knee in the two standard views: an antero-posterior (AP) view on a long plate in loaded single stance and an axial view of the patella. Radiographic assessment of the prosthesis was performed according to the Knee Society Total Knee Arthroplasty Roentgenographic Evaluation and Scoring System [19]. This involves studying the prosthetic components in relation to the femoro-tibial anatomical axes by measuring the specific angles. On the frontal plane, angle α refers to the femoral component, and β refers to the tibial component. On the AP view, angle Ω of total valgus prosthesis deviation was also assessed. On the sagittal plane, angle γ of femoral component flexion and σ of posterior inclination of the tibial component were measured. Radiolucent lines were also assessed at the bone−cement or prosthesis−bone interface by subdividing the prosthetic components into seven zones for the femur in the latero-lateral (LL) view and the tibia in the AP view, and three zones for the tibia in the LL view. The numerical score of the radiolucent lines for each component comes from the sum of the thickness in millimetres of the lines detected in each zone of the interface. For a component divided into seven zones, a score of 4 or less means component stability, a score between 5 and 9 requires close component surveillance for possible progression, whereas a score ≥10 points suggests loosening, independent of possible clinical symptoms.
Both pre- and post-operatively, patella height was also assessed radiographically on a lateral view using the Caton Index [20]. According to Caton, patella height comes from the relationship between the distance connecting the lowest point of the patella articular surface with the tibial joint line and the length of the patella articular surface. The normal value in these cases is 1 ± 0.2; a value > 1.1 indicates a high patella, whereas a value < 0.6 indicates a low patella.
Statistical analysis
Data collection and analysis were performed using SPSS version 13.0. Differences between the two groups were examined and compared using the Mann−Whitney test and one-way analysis of variance (ANOVA) and Pearson chi-square test. Statistical significance was defined as p ≤ 0.05 The study was authorised by the local ethical committee.
Results
Mean preoperative clinical score, assessed by the AKS system, was 38.5 (range 6−52) for the knee score and 47 (range 5−75) for the functional score in the study group, and 35 (range 6−68) for the knee score and 45 (range −20 to 70) for the functional score in the control group (Table 1). There was no significant difference found when comparing the postoperative average scores between the two groups of patients. The mean increment was 92.7 and 89.8 points, respectively, for the knee and functional score in the study group and 91 and 84, respectively, in the control group (Table 2).
Table 2.
Functional and radiological outcome in index and control groups
| Index (SD) | Control (SD) | Significance | |
|---|---|---|---|
| AKS | |||
| AKSS | 92.7 (3.9) | 91 (7) | NS a |
| AKFS | 89.8 (12.2) | 84 (21.4) | NS a |
| Percentage of area of tibial surface covered by implant | 98.5 (0.71) | 98.5 (0.81) | NS a |
| Femoral component (α) | 94.8° (2.6) | 94° (2.4) | NS b |
| Tibial component (β) | 88.9° (1.9) | 88° (2.7) | NS b |
| Angle of total valgus prosthesis deviation (Ω) | 4.31° (2.2) | 4° (1.1) | NS a |
| Angle of femoral component flexion (γ) | 3.6° (2.8) | 3° (0.8) | NS a |
| Angle of posterior inclination of the tibial component (σ) | 88° (2.4) | 87° (1.0) | NS a |
| Caton Index | 0.70 (0.1) | 0.81 (0.1) | p = 0.001 b |
| Loosening | |||
| Femoral (mm) | N = 7( 1); 6 (2); 1 (3) | N = 4( 1); 4 (2) | NS a |
| Tibial AP (mm) | N = 2( 1); 1 (2); 1 (3); 3 (4); 1(7); | N = 2 (1); 6 (2); 1 (3) | NS a |
| Tibial LL (mm) | N = 8 (1); 4( 2); 2 (4); 1( 5); 1( 6); 1 (17) | N = 5( 1); 1 (2); 1 (3) | p = 0.019 c |
SD standard deviation, AKS American Knee Society, AKSS American Knee Society Knee Score, AKFS American Knee Society Functional Score, AP antero-posterior, LL latero-lateral, NS not significant
aMann−Whitney test
bOne-way analysis of variance
cChi-square (Pearson)
Overall clinical evaluation of the replaced knee at the end of the follow-up period revealed that for patients previously undergoing osteotomy, a satisfactory result was found in 96.5% of cases (28/29): excellent AKSS score in 25 (90−100 points), good in three (80−89 points), fair in none (70−79 points) and poor in one (<70 points), which required revision. A similar percentage of satisfactory results was reported in the control group: 23 cases had excellent results, five good and one poor. At the last follow-up in 29 implants of the study group, pain at rest was absent in 25 cases and mild or occasional in the remaining four. No patient complained of severe or continuous pain. During walking, pain was absent in 19 cases, mild in six, moderate in four, but never severe. Ascending staircases, the pain was present in 23 cases and mild in six.
Mean flexion at last follow-up was 103° (median 100°, range 80–120°); flexion ≥90° was present in 28/29 cases. Active extension was complete in all cases, and none had a fixed flexion deformity. Mean alignment found clinically in dual stance was 5° in valgus deviation (range 3–7°): ten implants had valgus deviation between 5° and 7° and 19 between 4° and 3°. We observed only one case of medio-lateral laxity between 6 and 9 mm. Walking autonomy was unlimited in 18 cases, limited to 1,600 m in eight, reduced to 800 m in three, but was never lower. Ability to climb stairs was normal in 25 cases. Two patients were able to climb stairs but needed support to descend; the remaining two patients needed support both to ascend and descend. Walking aids were needed in only two cases. Three patients (AKSS range 80−89 points) had persistent anterior pain, which required a further joint arthroplasty of the patella performed, respectively, 18, 19 and 27 months after the primary prosthetic implant, with a marked clinical improvement. We observed a case of implant aseptic loosening 37 months after surgery, which required revision due to persistent and severe pain. We used a NexGen CCK prosthesis (Zimmer) with a full tibial wedge with 7° to fill residual defect and a cementless intramedullary stem.
In the control group , mild or occasional pain occurred in seven cases and was absent in all others. Mean pre-operative flexion was 100° (range 70–120°): flexion ≥90° was present in 25/29 cases. No patient had a mean fixed flexion deformity or deficit in active extension. Mean alignment clinically in dual stance was 4° in valgus deviation (range 10° varus to 7°valgus). We observed three cases of medio-lateral laxity between 6 and 9 mm. Walking unaided was unlimited in 15 cases, limited to 1,600 m in seven, reduced to 800 m in five and to 400 m in two. Ability to climb stairs was normal in 19 cases. Four patients were able to climb stairs but needed support to go down. Five patients needed support to both ascend and descend, and one patient with poor clinical condition was house bound . Walking aids were needed in five cases. In one case, we had poor clinical and functional results: this patient suffered from multiple arthropathies and poor general condition since the preoperative period. No patients in the control group underwent second revision.
On assessing radiological alignment of the prostheses, there were no statistical differences postoperatively comparing specific angles measured in index and control groups at the last follow-up (Table 2). Mean percentage of surface coverage of the tibial section by the prosthetic component was 98.5%; there were no statistical differences between index and control groups at the last follow-up (Table 2). During follow-up in the index group, no radiolucent lines were observed around the femoral component suggesting loosening or requiring close surveillance. Twenty-six tibial components in both AP and LL views were totally devoid of or had very small non-progressive radiolucencies, whereas three had suspected radiolucencies (total for the whole component approximately 5 mm). Of these last three cases, two were stationary during subsequent follow-ups, whereas the third case showed progressive signs of loosening. In this case, the radiolucencies were altogether >10 mm (Fig. 2) and indicated a possible imminent loosening, which then actually occurred, and the patient underwent revision three years after the first operation.
Fig. 2.
Progressive radiolucent lines under the tibial component following total knee arthroplasty (TKA)
No significant radiological component loosening was seen in the control group. Patients showed a numerical score ≤3 in the different prosthetic components. A significant difference (p = 0,019) in radiolucencies between index and control groups was found only in the AP view of the tibial component at the last follow-up (Table 2). In the study group, the mean Caton Index before joint arthroplasty was 0.69 (range 0.51–0.85), whereas at the last follow-up, a mean of 0.70 (range 0.51–1.05) was observed. The Caton Index was in the normal range in 26 cases after knee joint arthroplasty. In the remaining three, we found a low patella; in only two of these was it also present before the prosthetic implant. These three cases were symptomatic, so postoperative patella arthroplasty was performed. In the control group, patients showed a normal postoperative Caton index. A significant difference between index and control group was found in patella height using the Caton Index postoperatively (p = 0,001) (Table 2).
Discussion
Tibial osteotomy is a surgical operation aimed at treating medial knee arthritis. Its rationale is based on the transference of load stresses from the medial region of the degenerate knee to the healthy side [1, 2]. When patients have been appropriately selected, most clinical studies show high percentage of satisfactory results in the short term. However, with longer follow-up, progressive arthritic deterioration may develop, requiring conversion to TKA [3–9]. There have been conflicting reports in the literature regarding the outcome of TKA in patients who have had a previous proximal tibial osteotomy, with some studies describing results comparable with primary joint arthroplasty [10–12] and others [13–17] describing worse results and a higher number of complications in cases. A reduced rate of satisfactory results and increased difficulty in exposing the knee was reported by Windsor et al. [15] as early as the mid-1980s. These authors attributed such results to the presence of a low patella after tibial osteotomy, which reached 80% in their series. Alterations related to patella height seem to be especially related to surgical technique. In fact, a higher rate of low patella was observed after medial opening wedge osteotomy in comparison with lateral subtraction osteotomy [21]. Another condition seems to be the type of fixation and postoperative treatment provided. The rate of low patella is much less when stable fixation and early postoperative movement is achieved [22] in comparison with immobilisation in a cast, where the rate of low patella can reach 89% [23].
The great variability reported in the literature with respect to the results of knee joint arthroplasty after failure of a tibial osteotomy is, in our opinion, due to the wide heterogeneity of patients undergoing joint arthroplasty after osteotomy who have varying degrees of deformity on the frontal and sagittal planes, bone loss, ligament imbalance, low patella and damaged soft tissues [24]. Another reason may be the different osteotomy techniques, types of prostheses implanted, follow-up period and especially the different time periods after which the secondary joint arthroplasty was performed. In fact, the most recent series show comparable results to those of the primary prostheses [25, 26], and this can be explained by a better understanding of the technical difficulties involved in knee joint arthroplasty after tibial osteotomy.
In an attempt to minimise the effect of variables such as age, gender, prosthetic selection, use of cemented or uncemented components and duration of follow-up, we compared the results of TKA in 24 patients who had a previous HTO with those obtained in a control group of 29 patients who had not had a previous osteotomy. After an average follow-up of over eight years, 96.5% of patients in the study group had a good or excellent result compared with the same percentage in the control group. In our study HTO did not adversely affect prosthetic component fixation: only in one case was it necessary to perform a revision for aseptic loosening. However, we observed a significant difference in the percentage of patella infera and greater number of revisions for anterior knee pain.
As observed by several authors [13, 15, 27], the difficulties encountered during osteotomy revision are normally higher in comparison with those in primary surgery. Therefore, certain technical considerations must be made. The first point to consider during knee arthroplasty after osteotomy is the choice of approach in relationship to the presence of a previous skin incision, with the possibility of removing possible fixation devices. A medial parapatella incision performed for an opening wedge medial osteotomy can be performed without difficulty, as it allows the joint to be reached through a medial arthrotomy and any fixation devices on the proximal metaphysis of the tibia to be removed. Conversely, a previous lateral closing wedge osteotomy can pose more problems. Although a short transverse or oblique incision can be intersected at an angle between 60° and 90° by a new longitudinal anterior incision without risks of necrosis, great care must be taken when addressing a previous lateral longitudinal approach [24]. A lateral incision near the midline can be performed, thus allowing the joint to be reached through a medial arthrotomy, by the elevation of a thin cutaneous flap. If the incision is placed more laterally, it is preferable to use the approach described by Buechel [28], which allows lateral approach to the joint using an osteotomy of the anterior tibial tuberosity. The main difficulties encountered during the surgical approach concern the exposure of the knee that, due to the presence of peripatellar scarring fibrosis or low patella, may require supplementary procedures, such as release of the lateral alar ligament of the patella [13, 15], snipping of the quadriceps [29] or osteotomy of the anterior tibial tuberosity [30]. In our series, we performed lateral release in three cases, snipping the quadriceps in three, and osteotomy of the anterior tibial tuberosity in one.
When planning a joint arthroplasty secondary to proximal tibial osteotomy, some variations of the tibial anatomy necessarily related to the previous operation [24] should also be taken into account. On AP radiographs of the knee, a lateral inclination of the articular line is visible, with a higher medial plateau in comparison with the lateral side and often a real lateral translation of the epiphysis. This situation is the opposite to that normally observed in an arthritic genu varum. This creates further difficulty during knee joint arthroplasty secondary to tibial osteotomy, and in our series, we found this defect to be severe in four cases. Therefore, after a tibial osteotomy, regardless of the technique previously used, the thickness of bone resected from the lateral region of the tibia must be very small to re-establish the anatomical position of the lateral articular line [11, 24]. This precaution helps to reduce the possibility of instability or the use of excessively thick tibial inserts, which might in turn lead to an increase in the rate of patella infera.
Severe bone defects on the lateral plateau, in case of lateral closing wedge osteotomy, may sometimes require bone grafts or metal augmentation. In these cases, to reduce mechanical stresses on the metaphyseal region, it is advisable to use an intramedullary stem [31]. In two cases in our series following HTO, a NexGen modular tibial component with intramedullary stem and metal wedge was used to fill the large bone defect secondary to the osteotomy. Particular care is also required in cases of lateral translation of the tibial epiphysis, with alteration of the position of the medullary canal (which is medialised in the frontal plane) if prostheses are used with a central stem. This is due to a possible conflict with the lateral cortex. The solution in this case may be to reduce the size of the tibial component by moving it more medially or using components with shorter pegs, custom-made prostheses or with offset.
The anatomy of the proximal tibia after osteotomy is often also altered in the sagittal plane, with a reduction or inversion of the normal posterior inclination (tibial slope), which must be restored to varying extents according to the type of used prosthesis [27].
Cases of ligament instability have been described primarily in patients with a valgus overcorrection. Krackow and Holtgrewe [32] developed a complex technique of reconstruction that combines advancing the medial collateral ligament, posterior cruciate and postero-medial capsule and involves the use of unconstrained implants. In the absence of clear guidelines about the correct approach to ligament balancing in these cases, we recommend proceeding with great caution, preferring to perform ligament release after the bone cuts, as suggested by Whiteside [33], using test prostheses or spacers, adapting it to suit intraoperative situations.
In our cases treated after HTO, three secondary patellar resurfacings were necessary 18, 19 and 27 months after the operation due to a low patella, which in only one case was present before the prosthetic implant. Pain resolution was achieved in all three cases. Although lowering of the patella is not necessarily associated with an increase in contact forces in the femoro-patella joint, a higher rate of patella pain under such conditions has been found in other series [25]. Under these conditions, routine joint arthroplasty of the patella might prevent anterior pain. Although in some cases there was a greater difficulty in executing the operation, the tibial osteotomy sufficiently decreased pain and increased knee function in patients who otherwise would have needed a knee arthroplasty, which was postponed but not necessarily eliminated.
In our study the mean time lapse between the osteotomy and the joint arthroplasty was 8.5 years. The criteria for performing a tibial osteotomy are numerous and thus limit the study group. There is a tendency to reserve proximal tibial osteotomy as an operation for young adults. The ideal candidate is a thin, active person in the fifth or sixth decade of life. They must have clear signs of unicompartmental knee arthritis, pain and disability associated with the arthritis that severely interferes with their social and working life. The knee must have a varus deformity, verifiable on radiographs under load, not excessive (generally not >15°). In addition, the knee must be stable (above all, the integrity of the lateral compartment is essential) and must have good articular excursion: full extension of the knee (no flexion contracture >10°) and flexion of at least 90°. Generally, no symptoms in the femoro-patella joint should be present, as its integrity is important. Furthermore, the patient must be able to undergo suitable postoperative rehabilitation.
Conclusion
In this study, knee arthroplasty after proximal tibial osteotomy was satisfactory in 96.5% of cases over a mean follow-up of 97 months. Compared with primary knee arthroplasty without previous HTO, we found no significant difference in clinical and radiological results apart from a greater rate of anterior knee pain and revision for secondary resurfacing of the patella in the patients with previous HTO. Otherwise the surgical approach could be more difficult and require the skill of expert surgeons. Considering that osteotomy has a more restrictive criteria, that the surgical techniques of osteotomy and knee joint arthroplasty are more sophisticated and supported by safer and innovative surgical materials, we believe that proximal tibial osteotomy is still an important procedure that can markedly relive pain and increase knee function in young patients, thereby postponing the need for a TKA, although it does not eliminate the need.
Aknowledgements
To Mr. Keith Smith, for his help in translating portions of this manuscript. To Mrs. Elettra Pignotti, who carried out the statistical analysis and was involved in data interpretation.
Conflict of interest statement The authors declare that they have no conflict of interest related to the publication of this manuscript.
References
- 1.Coventry MB. Osteotomy about the knee for degenerative and rheumatoid arthritis: indications, operative technique, and results. J Bone Joint Surg Am. 1973;55(1):23–48. [PubMed] [Google Scholar]
- 2.Jackson JP. Osteotomy for osteoarthritis of the knee. In Proceedings of the British Orthopaedic Association. J Bone Joint Surg Br. 1958;40:826. [Google Scholar]
- 3.Aglietti P, Buzzi R, Vena LM, Baldini A, Mondaini A. High tibial valgus osteotomy for medial gonarthrosis: a 10- to 21-year study. J Knee Surg. 2003;16(1):21–26. [PubMed] [Google Scholar]
- 4.Berman AT, Bosacco SJ, Kirschner S, Avolio A., Jr Factors influencing long-term results in high tibial osteotomy. Clin Orthop Relat Res. 1991;272:192–198. [PubMed] [Google Scholar]
- 5.Coventry MB, Illstrup DM, Wallrichs SL. Proximal tibial osteotomy. A critical long-term study of eighty cases. Bone Joint Surg Am. 1993;75(2):196–201. doi: 10.2106/00004623-199302000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Hernigou P, Medevielle D, Debeyre J, Goutallier D. Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987;69(3):332–354. [PubMed] [Google Scholar]
- 7.Insall JN, Joseph DM, Msika C. High tibial osteotomy for varus gonarthrosis. A long term follow-up study. J Bone Joint Surg Am. 1984;66(7):1040–1048. [PubMed] [Google Scholar]
- 8.Rudan JF, Simurda MA. Valgus high tibial osteotomy. A long term follow-up study. Clin Orthop Relat Res. 1991;268:157–160. [PubMed] [Google Scholar]
- 9.Yasuda K, Majima T, Tsuchida T, Kaneda K. A ten - to 15-year follow-up observation of high tibial osteotomy in medial compartment osteoarthrosis. Clin Orthop Relat Res. 1992;282:186–195. [PubMed] [Google Scholar]
- 10.Amendola A, Rorabeck CH, Bourne RB, Apyan PM. Total knee arthroplasty following high tibial osteotomy for osteoarthritis. J Arthroplasty. 1989;4((Suppl)):11–17. doi: 10.1016/S0883-5403(89)80002-6. [DOI] [PubMed] [Google Scholar]
- 11.Meding JB, Keating EM, Ritter MA, Faris PM. Total knee arthroplasty after high tibial osteotomy. A comparison study in patients who had bilateral total knee replacement. J Bone Joint Surg Am. 2000;82(9):1252–1259. doi: 10.2106/00004623-200009000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Staeheli JW, Cass JR, Morrey B. Condylar total knee arthroplasty after failed proximal tibial osteotomy. J Bone Joint Surg Am. 1987;69(1):28–31. [PubMed] [Google Scholar]
- 13.Katz MM, Hungerford DS, Krackow KA, Lennox DE. Results of knee arthroplasty after failed proximal tibial osteotomy for osteoarthritis. J Bone Joint Surg Am. 1987;69(2):225–233. [PubMed] [Google Scholar]
- 14.Mont MA, Alexander N, Krackow KA, Hungerford DS. Total knee arthroplasty after failed proximal tibial valgus osteotomy. A comparison with a matched group. Clin Orthop Relat Res. 1994;299:125–130. [PubMed] [Google Scholar]
- 15.Windsor RE, Insall JN, Vince KG. Technical Considerations of total knee arthroplasty after proximal tibial osteotomy. J Bone Joint Surg Am. 1988;70(4):547–555. [PubMed] [Google Scholar]
- 16.Nelissen EM, van Langelaan EJ, Nelissen RG (2009) Stability of medial opening wedge high tibial osteotomy: a failure analysis. Int Orthop 2009 doi:10.1007/s00264-009-0723-3 [DOI] [PMC free article] [PubMed]
- 17.Tungall JA, Higgins GA, Waddell JP (2009) Complications of closing wedge high tibial osteotomy. Int.Orthop 2009 doi:10.1007/s00264-009-0819-9 [DOI] [PMC free article] [PubMed]
- 18.Insall JN, Dorr L, Scott R, Scott N. Rationale of the Knee Society Clinical Rating System. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 19.Ewald FC. The Knee Society Total Arthroplasty Roentgenographic Evaluation and Scoring System. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 20.Caton J. Patella Infera. Apropos of 128 cases. Rev Chir Orthop Réparatrice Appar Mot. 1982;68(5):317–325. [PubMed] [Google Scholar]
- 21.Tigani DS, Ferrari D, Trentani P, Barbanti-Brodano G, Trentani F. Patellar height after high tibial osteotomy. Int Orthop. 2001;24(6):331–334. doi: 10.1007/s002640000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Westrich GH, Peters LE, Haas SB, Buly RL, Windsor RE. Patella height after high tibial osteotomy with internal fixation and early motion. Clin Orthop Relat Res. 1998;354:169–174. doi: 10.1097/00003086-199809000-00020. [DOI] [PubMed] [Google Scholar]
- 23.Scuderi GR, Windsor RE, Insall JN. Observation on patellar height after proximal tibial osteotomy. J Bone Joint Surg Am. 1989;71(2):245–248. [PubMed] [Google Scholar]
- 24.Nelson CL, Haas SB. Total knee arthroplasty following high tibial osteotomy. In: Sculco TP, Martucci EA, editors. Knee arthroplasty. Wien: Springer; 2002. pp. 91–101. [Google Scholar]
- 25.Haddad FS, Bentley G. Total Knee arthroplasty after high tibial osteotomy. A medium term review. J Arthroplasty. 2000;15(5):597–603. doi: 10.1054/arth.2000.6621. [DOI] [PubMed] [Google Scholar]
- 26.Takai S, Yoshino N, Hirasawa Y. Revision total knee arthroplasty after failed high tibial osteotomy. Bull Hosp Jt Dis. 1997;56(4):245–250. [PubMed] [Google Scholar]
- 27.Insall JN, Scott RD. Surgery of the knee. 3. New York: Churchill Livingstone; 2001. [Google Scholar]
- 28.Buechel FF. A sequential three-step lateral release for correcting fixed valgus knee deformities during total knee arthroplasty. Clin Orthop Relat Res. 1990;260:170–175. [PubMed] [Google Scholar]
- 29.Garvin KL, Scuderi GR, Insall JN. Evolution of the quadriceps snip. Clin Orthop Relat Res. 1995;321:131–137. [PubMed] [Google Scholar]
- 30.Whiteside LA, Ohl MD. Tibial tubercle osteotomy for exposureof the difficult total knee arthroplasty. Clin Orthop Relat Res. 1990;260:6–9. [PubMed] [Google Scholar]
- 31.Brooks PJ, Walker PS, Scott RD. Tibial component fixation in deficient tibial bone stock. Clin Orthop Relat Res. 1984;184:302–308. [PubMed] [Google Scholar]
- 32.Krackow KA, Holtgrewe JL. Experience with a new technique for managing severely overcorrected valgus high tibial osteotomy at total knee arthroplasty. Clin Orthop Relat Res. 1990;258:213–224. [PubMed] [Google Scholar]
- 33.Whiteside LA. Selective ligament release in total knee arthroplasty of the knee in valgus. Clin Orthop Relat Res. 1999;367:130–140. doi: 10.1097/00003086-199910000-00016. [DOI] [PubMed] [Google Scholar]