Abstract
Nonunions of the distal femur are relatively rare but can occur with or without previous surgery. Many surgical methods have been described for the treatment of these nonunions including external fixation, intramedullary nailing, arthroplasty, and fixed angle plating. While arthroplasty may have a limited role in the elderly patient with osteoporosis and severe communiution, most nonunions can be reliably treated with revision fixation using a fixed angled device, lag screws, and bone grafting as needed. Fixed-angle plating also has the advantage of stabilising a small distal segment where intramedullary nailing has proven to be less effective. Any surgical intervention must include restoration of the normal mechanical axis of the distal femur for a satisfactory clinical outcome. Proximal tibia nonunions are a similarly rare clinical entity due to the excellent blood supply in the metaphysis. Extra-articular proximal tibial nonunions are often due to malreduction during the index surgery resulting in poor bone contact and biomechanical stability. Soft tissue forces and improper use of intramedullary implants often predispose these fractures to malalignment. Revision surgery consisting of deformity correction and at least a lateral tension band plate with lag screws has led to predictable union and good clinical results. Tibial plateau nonunions are exceedingly uncommon but are difficult to treat because of small, often devascularised fragments, post-surgical scarring, and osteopenia. Revision surgery with meticulous soft tissue handling to restore the articular surface and mechanical axis with repair of meniscal pathology gives the patient the best chance of recovering knee function.
Nonunions of the distal femur
Epidemiology
Nonunions of distal femur fractures are a relatively rare and difficult problem to treat. They can arise after operative and nonoperative treatment with similar frequency. Historical series using closed reduction and casting or cast bracing yielded nonunion rates from 2–6% [1–3]. These are similar to modern series using various forms of fixation including external fixation, intramedullary nailing and various plating methods that have rates from 0–6% [4–7]. These series are retrospective and feature heterogeneous populations and treatments. They are not of sufficient size to predict nonunion based on patient or injury related factors. Though these sequelae are rare, they present significant morbidity to the patient and a treatment challenge to the surgeon.
Evaluation
While no consensus exists in the literature, work-up of distal femur nonunions begins with an assessment of why the fracture failed to unite. Was there inadequate fixation leading to a hypertrophic nonunion or a failure of biology leading to an atrophic nonunion or both? Indolent infection should be ruled out as it may be the underlying aetiology and would necessitate a two-staged approach. Evaluation should include a thorough history and examination including wound healing following the previous surgery. If there is a concern for infection, blood work including complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels should be performed.
There is no universally accepted definition of nonunion, but most series use six months without healing or hardware failure as inclusion criteria. Radiographic evaluation should include plain films to evaluate deformity and the condition of the joints above and below the fracture. If deformity exists, long-leg standing X-rays should be performed. Computed tomography (CT) can more predictably assess lack of bony union as hardware may obscure bridging callus. CT can also allow for assessment of rotational malalignment and CT scanogram can accurately assess limb length inequality.
Surgical technique
Many techniques have been described for the treatment of distal femur nonunions. These include external fixation, intramedullary nailing, and open reduction and internal fixation (ORIF; Fig. 1). Many of these studies group distal femur nonunions with other fracture types making analysis difficult, but some general conclusions can be reached. All series with infected nonunions were treated with staged irrigation and debridement (I&D), and hardware removal if present. This was followed by a course of antibiotic treatment, generally for six weeks, before definitive management.
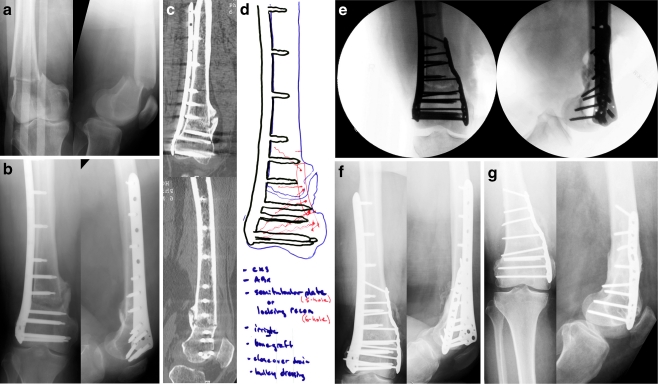
Fig. 1.
A 50-year-old female was involved in a motor vehicle accident and sustained a right-sided supracondylar distal femur fracture. Locking plate fixation was placed percutaneously using a less invasive stabilization system (LISS) plate and screws. She was diagnosed with a nonunion at six months and surgical revision was planned and performed with debridement and osteotomy of the nonunion site, placement of demineralized bone matrix (DBM) bone graft, and a medially placed locking compression plate (LCP) and screws including interfragmentary lag screws and screws for additional compression and stability. She returned at regular follow-up intervals and healed uneventfully. The LISS plate was removed two years following revision surgery due to tenderness near the plate. She last returned at 39 months following surgical revision with excellent clinical and radiographic results including a healed distal femur fracture, resolution of pain symptoms, and a return to all pre-injury activities. a Anteroposterior (AP) and lateral injury radiographs illustrating a right-sided supracondylar distal femur fracture. b AP and lateral films at six months revealing a nonunion. c CT scan images further illustrating the nonunion. d Preoperative plan for revision surgery. e Intraoperative fluoroscopic AP and lateral images. f AP and lateral images at one year following revision surgery revealing a healed distal femur nonunion. g AP and lateral images at 39 months (and 18 months following removal of the lateral plate and screws)
External fixation
Ali et al. [4] treated a series of 15 patients with distal femur nonunions with monolateral external fixation. These were a mix of open and closed fractures as well as a nonunion of an osteotomy. In 12 of these, the fixator spanned the knee joint due to difficulty with fixation in small distal fragments. Eleven patients underwent lengthening as a part of their nonunion treatment due to shortening deformities. The authors mention the importance of gentle soft tissue handling and attribute their success to this. Fourteen of 15 patients united with the remaining patient requiring removal of the fixator and intramedullary nailing prior to healing. The average range of motion of the study, including four patients that required quadricepsplasty, was 80°. All patients had minor pin tract infections, but there were no deep infections. The authors recommend that external fixation be used primarily in cases where significant shortening is present as the technique allows concurrent lengthening.
The techniques of Ilizarov were used by Paley et al. [8] on a variety of femoral malunions and nonunions. The authors describe in great detail the planning and technique of ring fixator use for numerous types of lower extremity nonunions. All patients underwent at least 1.5 cm of lengthening up to 8 cm. At a mean of 7.1 months (range 3.6–13) all patients had their deformity corrected. Since their analysis does not specifically refer to distal femur nonunions, it is difficult to make specific recommendations based on these results.
Saridis et al. [9] treated 13 patients using Ilizarov techniques. These were a mix of infected and noninfected cases with an average of 3.1 prior procedures. After an average of 309.8 days in external fixation, all went on to union, full weight bearing, and resolution of infection. According to the evaluation system devised by Paley et al. [8], eight of 13 patients had excellent results. These techniques appear to offer the ability to achieve union and regain length, but at the cost of several months using the device limiting knee motion and a high incidence of superficial infection.
Intramedullary nailing
Several studies have used intramedullary devices in the treatment of supracondylar nonunions. One of the earliest was Beall et al. [10] who used a transarticular technique to achieve union in ten of 11 patients who had previously undergone a variety of prior treatments. Three of eleven patients developed a chronic infection, and one of these needed above knee amputation (AKA) to eradicate the infection. The average range of motion after treatment was 40°, but after four patients underwent quadricepsplasty this increased to 80°. Kempf et al. [11] treated 25 out of 27 femoral nonunions to union at an average of 15 weeks with locked antegrade nailing, six of which were supracondylar. The authors did not specify if the two failures were supracondylar fractures. McLaren et al. [12] treated a variety of metaphyseal nonunions with locked nailing. Four of these were in the supracondylar femur of which three went on to heal with one patient requiring revision with a blade plate. All patients in this series had cancellous allograft added to the nonunion site at the time of fixation. Wu et al. [13] treated 24 distal femur nonunions with Gross-Kempf nailing and 22 out of 24 (91.7%) united by one year with an average time to healing of 4.5 months. The authors stress the importance of cast bracing and protected weight bearing in patients that have nonunions distal enough to allow only one interlocking screw in the distal fragment. Only seven nonunions were supracondylar with the majority being diaphyseal fractures distal to the isthmus. Range of motion was also not reported.
With the advent of retrograde femoral nailing, these instruments have also been used to repair distal nonunions. Koval et al. [14] treated 16 distal femur nonunions at an average of 33 months post injury with a specialised supracondylar nail. They noted a 25% union rate at a mean of 17 months. These were a mix of hypertrophic and atrophic nonunions, and 13 of 16 were grafted at the time of nailing. Nine of 16 had nail breakage. Complications included an intraoperative tibial plateau fracture while manipulating the knee to allow for nail insertion. The authors suggested that though healing rates were poor for both, the infra-isthmic fractures may be better suited to nailing than supracondylar fractures, though only 50% of these healed. They also suggested design changes to the nails that included stronger tubes and dynamic holes that might help to enhance healing.
Arthroplasty
Given that patients with distal femur nonunions may have concurrent arthritis, some authors have advocated treating them with arthroplasty. Kress et al. [15] treated five supracondylar fractures with long stem total knee arthroplasty (TKA). Three of these patients had prior TKA, three had prior attempts at ORIF, and two were previously infected. All patients healed by six months at an average of two months, and all had an improvement in their HSS knee scores. The authors recommended this procedure as a salvage if the patient has pre-existing arthritis or prior TKA. Freedman et al. [16] treated five patients with a tumor prosthesis—three of these had nonunion and two had “difficult” acute fractures. All had pre-existing arthritis with an average age of 65 years. At 28 months, there was an average flexion arc of 99°, though there was also an average 15° extensor lag. This obviated the need for fracture fixation and allowed immediate weight bearing, though it was not without complications. One patient had a deep infection that required above knee amputation, one patient had a dislocation of the modular stem requiring operative re-seating, and there was one deep infection at 25 days post-op that required irrigation, debridement, and polyethylene liner exchange. Davila et al. [17] reported on two cases of distal nonunions treated with tumor prosthesis. Both had several prior procedures and no evidence of infection. Both patients were able to bear weight immediately, achieved flexion from 0–100°, and had improved HSS scores at two years. Though small and retrospective, these series suggest arthroplasty may have a role as a salvage procedure in the elderly.
Fixed angle plating
Since interfragmentary compression is desirable and there is difficulty achieving fixation in supracondylar nonunions, fixed angle plating has been used for several years to treat distal nonunions. Early series using blade plates showed the promise of these implants, but these were small and retrospective. In 1949, Altenberg reported on a series using early blade plates [1]. Three of these were for distal femur nonunions and most were treated with balanced traction after fixation. Two of three healed but with severely restricted knee motion. One of the earliest series focusing on the need for compression using a blade plate and the AO articulated tension device achieved healing in four of five supracondylar nonunions [18]. Though the outcome measures were not well defined, only two patients achieved “normal” results. The authors attribute this to one patient dying from pneumonia and one patient being treated for bilateral nonunions. These results are given as part of a larger series of several types of nonunions treated with compression plating and make detailed analysis difficult. In 1987, Moore et al. [19] reported on a heterogeneous population of distal nonunions using a variety of treatments. Six of 16 patients were infected and underwent staged I&D before definitive treatment. Seven of ten noninfected patients were treated with iliac crest bone graft and 95° condylar blade plates. Three were treated with casting and use of a bone stimulator. Two of the patients with infected nonunions required eventual AKA. Six patients required quadricepsplasty to improve motion and 11 of 16 had significant arthritis at final follow-up with eight of 16 having malalignment. These results are difficult to interpret, but this report shows the difficulty in treating these patients, particularly those with prior infection.
Recent reports show more promising results using plating techniques. In 1999, Chapman et al. [20] reported on a series of 18 supracondylar nonunions treated with plating. Seventeen of 18 were classified as “avascular” based on a lack of callus at the site of the fracture. All were treated with on-lay grafting using autogenous ICBG. Infected patients underwent staged I&D prior to definitive grafting and fixation. The dynamic condylar screw (DCS) was the most frequently used implant, but condylar blade plates and secondary medial plates were used in some patients. All patients healed at an average of eight months. One required revision fixation and grafting to achieve healing. Average range of motion was 101° at final follow-up. One patient required removal of plate and Ilizarov correction of a varus malunion. One patient had a deep infection requiring hardware removal after bony union. Bellarbarba et al. [21] continued the trend of improved results. Using indirect reduction and only enough dissection to allow for removal of hardware, debridement of nonunion and medullary drilling, they were able to achieve union in 20 of 20 patients. Nineteen had been previously plated and 45% of these were grafted at the time of nonunion repair using ICBG to fill defects left by blade plates or DCS. As with earlier studies, care was taken to compress the nonunion using the articulated tension device. Motion was begun immediately and patients used toe touch weight bearing for the first six weeks after surgery. Average time to full weight bearing was 14 weeks. Nineteen of 20 patients had good/excellent results based on the Bostman scale, and 18 of 20 based on the HSS score, both of which improved significantly with surgery. No patient had deformity greater than 5°. Haidukewych et al. [22] published a series of 22 distal femur nonunions treated with a variety of fixation systems including both nailing and fixed angle plating. Twenty-one of 22 healed with significant improvement in Knee society pain and function scores. Twenty-one of 22 patients underwent bone grafting at the time of nonunion repair including allograft, autograft, combination, or vascularised fibular grafting. More recently, Gardner et al. [23] reviewed a series of 31 patients treated with correction of deformity, lag screw fixation, compression plating with fixed angle implants, and bone grafting. A variety of fixed angle devices were used including blade plates and locking condylar plates. Patients early in the series received autologous ICBG with the latter 29% receiving demineralised bone matrix in an attempt to reduce donor site morbidity. All patients healed except for one patient that developed avascular necrosis of the distal femur and went on to revision with a hinged prosthesis. Average time to union was 16 weeks and average knee motion was 103° with only one patient having a flexion contracture (15°). Return to preinjury activity was achieved in 84% of patients. Knee Society rating scales improved significantly.
These recent studies show that high rates of union can be achieved. They also use validated outcome measures to demonstrate clinical improvement in a vast majority of patients. There also appears to be a lower rate of complications with modern plating techniques compared to published series using intramedullary nailing as well as an improved time to healing. Series vary widely in their frequency and type of bone graft used, but it appears that some type of grafting is helpful. Wang et al. [24] focused on this issue using ICBG and cortical strut grafting and a variety of fixation techniques to achieve union in 13 of 13 patients with no prior infection history. Also, in the arthritic patient with poor bone stock or a previous TKA arthroplasty using a long stemmed or tumor prosthesis may be a viable salvage option.
Nonunions of the proximal tibia
Nonunion of the proximal tibia is a relatively rare clinical entity. The several clinical series that exist in the literature concerning both extra-articular proximal tibia fractures and tibial plateau fractures mostly document nonunion rates less than 3%. As a baseline reference, Sarmiento reported on 108 closed proximal tibia fractures treated with functional bracing [25]. The nonunion rate was 2.7%, with the majority of fractures healing with “acceptable” amounts of displacement (20%), shortening (3.5 mm), and angular displacement (<6° in almost 90% of patients).
With respect to operatively treated proximal tibia fractures, Bhandari et al. performed a meta-analysis comparing the use of plates/screws, intramedullary nails, and external fixators [26]. The average nonunion rate was 2% for plate/screw fixation, 3.5% for intramedullary nails, and 8% for external fixators. Their conclusions based on the strength of evidence of the compiled studies was that surgeon preference and experience should guide surgical technique and implant choice. Due to the attractiveness of a load-sharing device along with minimally-invasive insertion with a presumably lower infection rate, the use of intramedullary nails for proximal tibia fractures has received more attention recently. Ricci reported on 12 patients treated with intramedullary nails and blocking screws to counteract the typical apex anterior and valgus deformity seen with these fractures [27]. Using blocking screws to narrow the otherwise capacious proximal tibial canal, malalignment was seen in only one patient and two nonunions resulted, both of whom sustained grade IIIB open fractures. Similarly, Nork et al. reported on 37 patients with proximal tibia fractures treated with intramedullary nailing and had no nonunions despite the use of “open” reduction techniques including unicortical plating, k-wire fixation, femoral distractor alignment, and reduction clamps [28]. However, two patients with segmental fractures had nonunion of the distal, diaphyseal fracture, and two patients underwent staged ICBG due to bone loss from the original injury.
Tibial plateau fractures have an even lower rate of nonunion after undergoing open reduction and internal fixation. One retrospective study of 117 operatively treated tibial plateau fractures had only five delayed unions and three nonunions (2.6%) [29]. These fractures were treated with traditional non-locked implants. With the development of early locking systems such as the LISS (Less Invasive Stabilization System, Synthes, Paoli, PA), indications were expanded for lateral implants to include bicondylar tibial plateau fractures since a fixed-angle device could be used to stabilise the medial column in certain fracture patterns. A study by Gosling et al. evaluated the LISS system used alone to treat 69 bicondylar tibial plateau fractures with only one nonunion (1.4%), although 13 patients underwent primary bone grafting [30]. More importantly, 16 patients had a significant malreduction and nine patients had a loss of reduction. Another early study of the LISS system by Stannard et al. in 25 tibial plateau and ten proximal tibia fractures found only one nonunion (2.9%) at short-term follow-up [31]. Barei et al. evaluated complications of treating high-energy bicondylar tibial plateau fractures with a dual-incision (anterolateral and posteromedial) technique as an alternative to a single incision with more extensive soft-tissue stripping [32]. Of the 83 patients in the study, only one patient (1.2%) developed a nonunion which occurred at the metadiaphyseal junction that subsequently required revision plating and bone grafting. In other case series of more than 200 combined tibial plateau fractures, no nonunions were seen [33–35]. Finally, in a study of 125 patients, 101 of whom were treated operatively, the rate of nonunion was 1.6%, occurring in patients with higher energy mechanisms and complex fracture patterns [36].
Many factors can contribute to the development of a nonunion in the proximal tibia. Some factors, such as the soft tissue injury and the extent of bone loss, are dictated by the circumstances at the initial injury. Other factors, such as adequate reduction with apposition of bony surfaces and biomechanical stability of the chosen implant, are surgeon-controlled. Still other factors, such as soft tissue stripping/bone devitalisation, infection, and wound healing complications, are probably multifactorial. The large bed of cancellous bone in the proximal tibia has a large volume of metabolically active trabecular bone which mitigates against the development of nonunion. Indeed, in the previously referenced study of high-energy bicondylar fractures [32], the fact that only one nonunion developed in a large group of fractures with presumably extensive soft tissue injury suggests the healing response of the proximal tibia is robust. In addition, the proximal tibia has a rich vascular supply from the anterior tibial artery as well as the popliteal artery as demonstrated by Borrelli et al. [37]. The anterior tibial artery provides an average of four extraosseous branches to the lateral tibial metaphysis after piercing the intraossesous membrane. The medial and lateral geniculate arteries from the popliteal artery at the level of the popliteal fossa provide branches to the posterior aspect of the proximal tibia, with anastamoses to the anterior and posterior tibial arteries.
Treatment of extra-articular proximal tibial nonunions
As rare as proximal tibial nonunions are, when they do occur, they present a challenge to the treating surgeon. Incisions, scar tissue, and soft tissue/bony devitalisation create an unfavourable environment for further surgery (Fig. 2). In addition, the proximal fragment is often short and compromised by previous hardware tracks, limiting options for revision fixation with good bone purchase. Early attempts to stabilise these fractures acutely with intramedullary devices often led to malignment which predisposed a small subset of these patient to develop nonunions. The use of a medial starting point, the lack of blocking screws, and the use of earlier generation nails with a very distal Herzog bend all contributed to the typical apex anterior/valgus deformity [38]. Presumably, the lack of an anatomical reduction reduces the amount of bone-to-bone contact required for fracture healing. When laterally-based plates are used, the potential for varus deformity and collapse in the setting of medial comminution exists, especially with the use of non-locked implants. This lack of mechanical stability also is a contributing factor to nonunion.
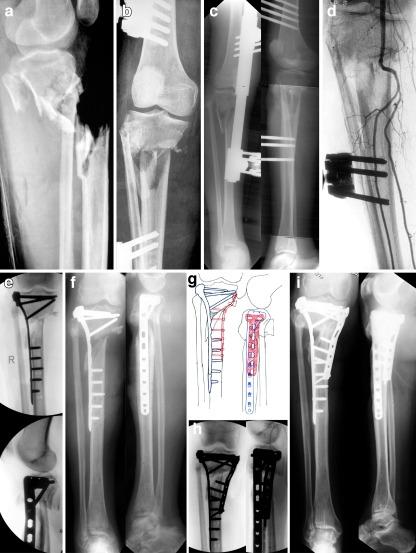
Fig. 2.
A 65-year-old female was skiing and was struck by another skier who was airborne after going off of a jump. She sustained a right-sided Grade IIIC open proximal tibia fracture with segmental metaphyseal bone loss. She was taken to a local trauma centre and also had extensive degloving. A joint spanning external fixator was applied and a vascular reconstruction was performed bypassing her popliteal trunk. She was transferred to our institution at three months following injury for definitive management of her tibia fracture. Presence of an eschar was noted near the fracture site and she had a viable foot but did have a foot drop with numbness on the dorsum and distal plantar aspect of her foot. She underwent multiple irrigation and debridements followed by removal of the external fixator, open reduction and internal fixation (ORIF), correction of varus deformity, and placement of a proximal tibia locking plate. The majority of the anterior compartment was debrided and a free rectus flap was performed to cover the proximal aspect of the tibia followed by a split thickness skin graft for skin coverage. She continued progress but at six months following ORIF, radiographs revealed a nonunion with maintenance of reduction and hardware. Revision ORIF was planned and performed with flap and muscle elevation, placement of DBM bone graft, BMP-7 and a medial proximal tibia locking plate for additional stability. She returned for regular follow-up intervals and at 39 months she presented with excellent radiographic and clinical results including a healed proximal tibia nonunion in excellent alignment with presence of partial lateral defect, significant improvement in pain, recovery of foot function and resolution in numbness symptoms, and a return to all pre-injury activities including skiing. Anteroposterior (AP) (a) and lateral (b) injury radiographs revealing Grade IIIC open proximal tibia fracture with segmental metaphyseal bone loss. c Radiographs following application of a spanning external fixator. d Arteriogram three months following popiteal truck bypass procedure. e Intraoperative fluoroscopic images following ORIF, correction of varus deformity and placement of a proximal tibia locking plate. f AP and lateral injury radiographs at five months revealing a proximal tibia nonunion with maintenance of reduction and hardware. g Preoperative plan for revision ORIF. h Intraoperative fluoroscopic images following ORIF, placement of DBM, BMP-7 and a medial proximal tibia locking plate. i AP and lateral radiographs at 39 months revealing a healed proximal tibia nonunion in excellent alignment with presence of partial lateral defect
Carpenter and Jupiter approached these challenges with the use of an angled blade plate to repair metaphyseal nonunions of the tibia [39]. In their series of 16 metaphyseal unions, nine were distal and seven were proximal tibias. For the proximal tibial nonunions, an extensile anterolateral approach was used 1 cm lateral to the tibial crest. Typically, a femoral distractor was applied on the concave (medial) side allowing correction of a varus deformity, and the blade plate was placed on the convex/lateral side to act as a tension band. All patients received autogenous iliac crest bone graft. Fourteen out of 16 patients went on to union, although the two treatment failures required conversion to ring fixators without union at the time of writing. The authors felt that the use of a femoral distractor allowed for controllable correction of any angular deformities associated with the nonunion and that the blade plate allowed for reliable fixed-angle fixation in a short metaphyseal segment where conventional plates and screws had failed. Functionally, only 12 of 16 (75%) were able to walk without assistance and the remainder required the use of PTB braces. Three of 16 patients had pain on exertion, two of 16 had <30° loss of range of motion, and two of 16 patients required hardware removal.
More recently, Wu [40] reported on his series of proximal tibial nonunions and malunions approached with a medial blade plate. Twenty-five patients with bicondylar tibial plateau fractures that had failed single lateral plating comprised the study group. Revision surgery consisted of plate removal, fibular osteotomy, transverse tibial osteotomy distal to the tibial tubercle, and realignment of the mechanical axis. After trimming the now-prominent medial proximal tibia, a medially based 95° blade plate was inserted. Local bone graft from the lateral proximal tibia was used to fill the open osteotomy wedge. All patients healed by four months, mechanical alignment was restored in all patients, and 22 of 25 had improvement in knee function. However, the use of a single anterior incision in this series to remove the previous hardware and apply a large medial plate may cause excessive soft tissue stripping, and a large medial plate in the relatively subcutaneous proximal tibia may be a cause for concern. In addition, with the common varus deformity encountered in these fractures, plating the lateral/tension side is more biomechanically advantageous.
A series of 18 proximal tibial nonunions was treated with multiple modalities by Lonner et al. [41], including ORIF with compression or blade plating, cast treatment, external fixation, and long-stemmed arthroplasty. While all patients went onto osseous union, 44% of patients required the use of a cane, 66% of patients had pain on activity, and patients continued to have problems with knee stiffness. A study by McLaren et al. reported on 14 patients with either malunion or nonunion of the proximal tibia treated with locked intramedullary fixation with residual deformity or chronic knee pain in the three nonunion patients of the cohort [12].
Our institution’s experience [42] with these fractures illustrates some of the surgical principles employed to obtain a successful result. Sixteen patients with a proximal tibial nonunion (either purely extra-articular or with intra-articular involvement initially but extra-articular nonunion) were treated with the same surgical protocol. Prior to definitive treatment, patients had previously been treated nonoperatively, with rigid IM nails, Ender’s nails, external fixation, lateral compression and locked plates, as well as bicondylar plates. With IM nail fixation, failure to contain the large volume of the proximal tibia typically led to malreduction and decreased contact of fracture edges, creating a mechanically unstable scenario predisposing to nonunion. With lateral plate fixation, failure to address medial comminution often led to varus collapse.
Pre-operative work-up consisted of full-length radiographs of the lower extremity, a scanogram, and CT scans to document rotational deformity as well as to assess the nature of the nonunion. In our patient cohort, 14 of 16 patients had a malalignment of at least 5° in the coronal or sagittal plane. Preoperative planning using all the above studies led to the decision to use at least a laterally-based plate in all circumstances. At the time of surgery, an anterolateral S-incision was used if possible given pre-existing surgical incisions. Critical to the treatment of these nonunions was a meticulous arthrolysis of the knee joint made possible by extending the incision proximally. At the nonunion site, lamina spreaders were used for exposure and all fibrous tissue and pseudocapsule was excised. Fenestration of the intramedullary canal on both sides of the fracture allowed ingress of blood, and healing potential was augmented with either autogenous iliac crest bone graft or demineralised bone matrix.
Deformity correction was essential and obtained and maintained using a femoral distractor in many cases, although this often was supplemented with fibular osteotomy to allow restoration of the mechanical axis. Provisional fracture reduction was obtained using clamps and a lateral tibial plate was fixed proximally, allowing the use of the articulating tensioning device distally to compress the fracture. Fixation was also supplemented with lag screws across the fracture site when possible. A supplemental anterior plate was used for transverse fractures placed just distal to the tibial tubercle to counteract the pull of the extensor mechanism where lag screws were not possible. The arthrolysis of the knee also decreased the forces seen across the nonunion when motion is hampered by a stiff knee joint.
Postoperatively, 100% of patients had their mechanical axis restored to within 5° of anatomical and all patients healed by an average of four months both clinically and radiographically. Fourteen of 16 returned to their pre-injury activity level and were ultimately satisfied with their result. Knee Society function and knee scores increased from 25.6 and 50.1 to 87.4 and 89.4 (P < 0.05), respectively, at an average follow-up of more than three years.
Treatment of tibial plateau nonunions
As evidenced by the previously mentioned studies, nonunion of tibial plateau fractures is an exceedingly rare entity. When encountered, reliable osteosynthesis is often complicated by the small remaining articular fragments, osteopenic bone, and post-surgical scarring leading to limited mobility and devascularisation of the fracture fragments. Historically, only a single case report discussing treatment of a tibial plateau nonunion existed in the literature [43]. This medial condyle nonunion from a conservatively treated fracture was treated with arthrotomy, mobilisation and over-reduction of the nonunited segment, compression buttress plating, and bone grafting. This resulted in healing by three months and good function by six months.
Our experience as reported by Toro-Arbelaez et al. [44] constitutes the only known series of tibial plateau nonunions treated by revision open reduction and internal fixation. The five patients in the series all had a nonunion as evidenced by lack of union by six months after the index procedure. The nonunions were all confirmed with plain radiographs, CT scans, and intraoperatively. Patients presented with an average of 2.4 previous operations and at an average delay of 6.4 months from injury.
The surgical technique for these nonunions consisted of an arthrotomy to visualise the status of the menisci and articular cartilage along with subperiosteal exposure of the nonunion site in the most suitable plane based on preoperative CT scans. Any pre-existing deformity was corrected with a femoral distractor once the fracture fragments were mobilised. All previous hardware was removed and cultures were taken prior to administration of antibiotics. Fibrous tissue was excised from the fracture site and intra-articular osteotomy was used to liberate malunited articular segments. Mobilisation and reduction of the nonunited fragments was achieved with elevators, dental picks, and K-wires after arthrolysis of the knee to aid in visualisation. Blood flow to the fracture was restored by using a drill to open the medullary canal. Provisional reduction was achieved using K-wires, and iliac crest graft or demineralised bone matrix with BMP was used to fill any metaphyseal voids. Final fixation consisted of antiglide/buttress plating (Fig. 3). Important surgical principles to be observed include meticulous soft tissue handling with full-thickness flaps as the condition of the soft tissue in these cases is already tenuous.
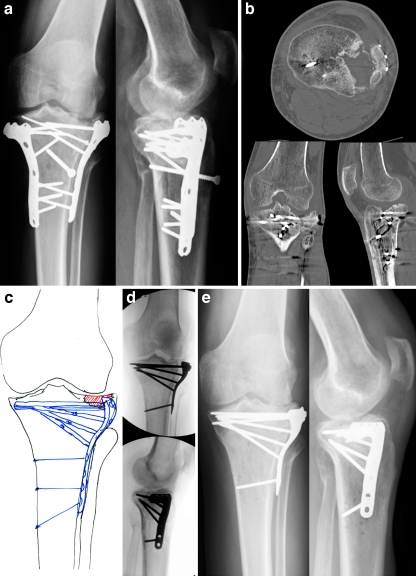
Fig. 3.
A 45-year-old male fell 15 feet off a ladder and sustained a left-sided Shatzker II type tibial plateau fracture. He was taken to a local hospital and open reduction and internal fixation (ORIF) was performed with placement of a locking plate. He followed-up with his treating surgeon and was referred to our institution at seven months for treatment of an intraarticular tibial plateau nonunion. A CT scan was performed for confirmation of the nonunion and further delineation of the depressed fragment in the lateral plateau. Revision ORIF was performed with complete hardware removal, intraarticular osteotomy and elevation of the depressed fragment, placement of DBM bone graft, placement of a proximal tibia locking plate and screws including interfragmentary lag screws, and repair of a lateral meniscus tear. He returned at regular follow-up intervals and at his latest follow-up at six months he presented with good radiographic and clinical results including a healed tibial plateau nonunion, a significant improvement in pain, and a return to his pre-injury activities. His radiographs demonstrate evidence of moderate osteoarthritis (OA) in his lateral joint space which does not limit him from his activities and he has resumed his hobbies of horse riding and competition in polo matches. Anteroposterior (AP) (a) and lateral (b) radiographs and CT scan images seven months following ORIF for a right-sided Shatzker II type tibial plateau fracture illustrating a nonunion with presence of a depressed fracture fragment. c Preoperative plan for revision surgery. d Intraoperative fluoroscopic AP and lateral images. e AP and lateral images at six months following revision surgery revealing a healed tibial plateau nonunion and evidence of moderate OA in the lateral joint space
In our series, all nonunions had healed by 12 weeks and deformity correction was maintained in all patients with pre-existing malalignment. Four patients returned to pre-injury activity level, but two subsequently went on to total knee arthroplasty for end-stage post-traumatic arthrosis. Of the remaining three non-arthroplasty patients, two had marked radiographic osteoarthritic changes. These results are not surprising given the significant articular and meniscal damage observed during revision surgery. In fact, one patient had an entrapped meniscal fragment in the fracture site, leading to nonunion. This underscores the findings of a recent study [45] showing that more than 90% of tibial plateau fractures have some evidence of acute meniscal pathology on MRI. In patients with advanced joint degeneration, it remains unclear whether this is primarily from the initial injury or presence of an intra-articular nonunion.
Conclusion
In summary, both extra-articular and intra-articular nonunions of the proximal tibia are uncommon but challenging to treat. With respect to extra-articular nonunions, restoration of the mechanical axis is paramount to achieving bony union and at the least a lateral tension band plate has been shown to be effective in stabilising these fractures. Basic nonunion principles of fracture debridement, fragment interposition with compression and lag screw fixation still apply in these scenarios. With intra-articular nonunions, successful reduction and stabilisation of the articular surface and attention to any meniscal pathology at the time of surgery gives the patient the best chance to recover knee function. If post-traumatic arthritis does ensue, the restoration of bone stock and normal knee alignment will make a subsequent total knee arthroplasty less complicated. The importance of preoperative planning, careful soft tissue handling and minimal bone devitalisation are most important in these injuries where the soft tissue envelope is already tenuous and compromised by the initial injury or previous surgical procedures.
References
- 1.Altenberg AR, Shorkey RL. Blade-plate fixation in non-union and in complicated fractures of the supracondylar region of the femur. J Bone Jt Surg. 1949;31A(2):312–316. [PubMed] [Google Scholar]
- 2.Connolly JF, Dehne E. Closed reduction and early cast-brace ambulation in the treatment of femoral fractures. J Bone Jt Surg. 1973;55-A:1581–1599. [PubMed] [Google Scholar]
- 3.Weil GC, Kuehner HG, Henry JP. The treatment of 278 consecutive fractures of the femur. Surg Gynecol Obstet. 1936;62(435):441. [Google Scholar]
- 4.Ali F, Saleh M. Treatment of isolated complex distal femoral fractures by external fixation. Injury. 2000;31(3):139–146. doi: 10.1016/S0020-1383(99)00249-1. [DOI] [PubMed] [Google Scholar]
- 5.Danziger MB, Caucei D, Zecher SB, Segal D, Covall DJ. Treatment of intercondylar and supracondylar distal femoral fractures using the GSH supracondylar nail. Am J Orthop. 1995;24(9):684–690. [PubMed] [Google Scholar]
- 6.Mize RD, Bucholz RW, Grogan DP. Surgical treatment of displaced, comminuted fractures of the distal end of the femur. J Bone Jt Surg. 1982;64A(6):871–879. [PubMed] [Google Scholar]
- 7.Schatzker J, Horne G, Waddell J. The Toronto experience of the supra-condylar fracture of the femur: 1966–1972. Injury. 1974;6(113):128. doi: 10.1016/0020-1383(74)90005-9. [DOI] [PubMed] [Google Scholar]
- 8.Paley D, Chaudray M, Pirone AM, Lentz P, Kautz D. Treatment of malunions and mal-nonunions of the femur and tibia by detailed preoperative planning and the Ilizarov techniques. Orthop Clin North Am. 1990;21(4):667–691. [PubMed] [Google Scholar]
- 9.Saradis A, Panagiotopoulos E, Tyllianakis M, Matzaroglou C, Vandoros N, Lambiris E. The use of the Ilizarov method as a salvage procedure in infected nonunion of the distal femur with bone loss. J Bone Jt Surg Br. 2006;88(2):232–237. doi: 10.1302/0301-620X.88B2.16976. [DOI] [PubMed] [Google Scholar]
- 10.Beall MS, Jr, Nebel E, Bailey RW. Transarticular fixation in the treatment of non-union of supracondylar fractures of the femur: a salvage procedure. J Bone Jt Surg. 1979;61A(7):1018–1023. [PubMed] [Google Scholar]
- 11.Kempf I, Grosse A, Rigaut P. The treatment of noninfected pseudoarthrosis of the femur and tibia with locked intramedullary nailing. Clin Orthop. 1986;212:142–153. [PubMed] [Google Scholar]
- 12.McLaren AC, Blokker CP. Locked intramedullary fixation for metaphyseal malunion and nonunion. Clin Orthop. 1991;265:253–260. [PubMed] [Google Scholar]
- 13.Wu CC, Shih CH. Distal tibial nonunion treated by intramedullary reaming with external immobilization. J Orthop Trauma. 1996;10(1):45–49. doi: 10.1097/00005131-199601000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Koval KJ, Seligson D, Rosen H, Fee K. Distal femoral nonunion: treatment with a retrograde inserted locked intramedullary nail. J Orthop Trauma. 1995;9:285–291. doi: 10.1097/00005131-199509040-00003. [DOI] [PubMed] [Google Scholar]
- 15.Kress KJ, Scuderi GR, Windsor RE, Insall JN. Treatment of nonunions about the knee utilizing custom: total knee arthroplasty and press-fit intramedullary stems. J Arthroplast. 1993;8(1):49–55. doi: 10.1016/S0883-5403(06)80107-5. [DOI] [PubMed] [Google Scholar]
- 16.Freedman EL, Hak DJ, Johnson EE, Eckardt JJ. Total knee replacement in elderly patients with acute fracture or nonunion. J Orthop Trauma. 1995;9(3):231–237. doi: 10.1097/00005131-199506000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Davila J, Malkani A, Paiso JM. Supracondylar distal femoral nonunions treated with a megaprosthesis in elderly patients: a report of two cases. J Orthop Trauma. 2001;15(8):574–578. doi: 10.1097/00005131-200111000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Solheim K, Vaage S. Delayed union and nonunion of fractures: clinical experience with the ASIF method. J Trauma. 1973;13(2):121–128. doi: 10.1097/00005373-197302000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Moore TJ, Watson T, Green SA, Garland DE, Chandler RW. Complications of surgically treated supracondylar fractures of the femur. J Trauma. 1987;27(4):402–406. doi: 10.1097/00005373-198704000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Chapman MW, Finkemeiere CG. Treatment of supracondylar nonunions of the femur with plate fixation and bone graft. J Bone Jt Surg Am. 1999;81(A):1217–1228. doi: 10.2106/00004623-199909000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Bellabarba C, Ricci WM, Bolhofner BR. Indirect reduction and plating of distal femoral nonunions. J Orthop Trauma. 2002;16(5):287–296. doi: 10.1097/00005131-200205000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Haidukewych GJ, Berry DJ, Jacofsky DJ, Torchia ME. Treatment of supracondylar femur nonunions with open reduction and internal fixation. Am J Orthop. 2003;32(564):567. [PubMed] [Google Scholar]
- 23.Gardner MJ, Toro-Arbelaez JB, Harrison M, Hierholzer C, Lorich DG, Helfet DL. Open reduction and internal fixation of distal femoral nonunions: long-term functional outcomes following a treatment protocol. J Trauma. 2008;64(2):434–438. doi: 10.1097/01.ta.0000245974.46709.2e. [DOI] [PubMed] [Google Scholar]
- 24.Wang JW, Weng LH. Treatment of distal femoral nonunion with internal fixation, cortical allograft struts, and autogenous bone grafting. J Bone Jt Surg Am. 2003;85:436–440. doi: 10.1302/0301-620X.85B3.12451. [DOI] [PubMed] [Google Scholar]
- 25.Martinez A, Sarmiento A, Latta LL. Closed fractures of the proximal tibia treated with a functional brace. Clin Orthop. 2003;417:293–302. doi: 10.1097/01.blo.0000093012.90435.e3. [DOI] [PubMed] [Google Scholar]
- 26.Bhandari M, Audige L, Ellis T, Hanson B. Operative treatment of extra-articular proximal tibia fractures. J Orthop Trauma. 2003;17(591):595. doi: 10.1097/00005131-200309000-00013. [DOI] [PubMed] [Google Scholar]
- 27.Ricci WM, O’Boyle M, Borrelli J, Bellabarba C, Sanders R. Fractures of the proximal third of the tibial shaft treated with intramedullary nails and blocking screws. J Orthop Trauma. 2001;15(4):264–270. doi: 10.1097/00005131-200105000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Nork SE, Barei DP, Schildhauer TA, Agel J, Holt S, Schrick JL, et al. Intramedullary nailing of proximal quarter tibial fractures. J Orthop Trauma. 2006;20(8):523–528. doi: 10.1097/01.bot.0000244993.60374.d6. [DOI] [PubMed] [Google Scholar]
- 29.Ebraheim NA, Sabry FF, Haman SP. Open reduction and internal fixation of 117 tibial plateau fractures. Orthopedics. 2004;27:1281–1287. doi: 10.3928/0147-7447-20041201-18. [DOI] [PubMed] [Google Scholar]
- 30.Gosling T, Schandelmaier P, Muller M, Hankemeier S, Wagner M, Krettek C. Single lateral locked screw plating of bicondylar tibial plateau fractures. Clin Orthop. 2005;439(207):214. doi: 10.1097/00003086-200510000-00036. [DOI] [PubMed] [Google Scholar]
- 31.Stannard JP, Wilson TC, Volgas DA, Alonso JE. Stabilization of proximal tibial fractures with the proximal tibial LISS: early experience. Injury. 2003;34(S1):A36–A42. doi: 10.1016/S0020-1383(03)00256-0. [DOI] [PubMed] [Google Scholar]
- 32.Barei DP, Nork SE, Mills WJ, Henley MB, Bernirschke SK. Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. J Orthop Trauma. 2004;18(10):649–657. doi: 10.1097/00005131-200411000-00001. [DOI] [PubMed] [Google Scholar]
- 33.Burri C, Bartzke G, Coldeway J, Muggler E. Fractures of the tibial plateau. Clin Orthop. 1979;138:84–93. [PubMed] [Google Scholar]
- 34.Rasmussen PS. Tibial condylar fractures: impairment of knee joint stability as an indication for surgical treatment. J Bone Jt Surg. 1973;55A(7):1331–1350. [PubMed] [Google Scholar]
- 35.Tscherne H, Lobenhoffer P. Tibial plateau fractures: management and expected results. Clin Orthop. 1993;292:87–100. [PubMed] [Google Scholar]
- 36.Manidakis N, Dosani A, Dimitriou R, Stengel D, Matthews S, Giannoudis P (2009) Tibial plateau fractures: functional outcome and incidence of osteoarthritis in 125 cases. Int Orthop. doi:10.1007/s00264-009-0790-5 [DOI] [PMC free article] [PubMed]
- 37.Borrelli J, Jr, Prickett W, Song E, Becker D, Ricci W. Extraosseous blood supply of the tibia and the effects of different plating techniques: a human cadaveric study. J Orthop Trauma. 2002;16(10):691–695. doi: 10.1097/00005131-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 38.Lang GJ, Cohen BE, Bosse MJ, Kellam JF. Proximal third tibial shaft fractures. Should they be nailed? Clin Orthop. 1995;315:64–74. [PubMed] [Google Scholar]
- 39.Carpenter CA, Jupiter JB. Blade plate reconstruction of metaphyseal nonunion of the tibia. Clin Orthop. 1996;332:23–28. doi: 10.1097/00003086-199611000-00005. [DOI] [PubMed] [Google Scholar]
- 40.Wu CC. Salvage of proximal tibial malunion or nonunion with the use of angled blade plate. Arch Orthop Trauma Surg. 2006;126:82–87. doi: 10.1007/s00402-006-0106-9. [DOI] [PubMed] [Google Scholar]
- 41.Lonner JH, Siliski JM, Jupiter JB, Lhowe DW. Posttraumatic nonunion of the proximal tibial metaphysis. Am J Orthop. 1999;28(9):523–528. [PubMed] [Google Scholar]
- 42.Gardner MJ, Toro-Arbelaez JB, Boraiah S, Lorich DG, Helfet DL. Surgical treatment and outcomes of extraarticular proximal tibial nonunions. Arch Orthop Trauma Surg. 2008;128:833–839. doi: 10.1007/s00402-007-0383-y. [DOI] [PubMed] [Google Scholar]
- 43.Schatzker J, Schulak DJ. Pseudarthrosis of a tibial plateau fracture: report of a case. Clin Orthop. 1979;145:146–149. [PubMed] [Google Scholar]
- 44.Toro-Arbelaez JB, Gardner MJ, Shindle MK, Cabas JM, Lorich DG, Helfet DL. Open reduction and internal fixation of intraarticular tibial plateau nonunions. Injury. 2007;38(378):383. doi: 10.1016/j.injury.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 45.Gardner MJ, Yacoubian S, Geller D, Suk M, Mintz D, Potter H, Helfet DL, Lorich DG. The incidence of soft tissue injury in operative tibial plateau fractures: a magnetic resonance imaging analysis of 103 patients. J Orthop Trauma. 2005;19(2):79–84. doi: 10.1097/00005131-200502000-00002. [DOI] [PubMed] [Google Scholar]