Abstract
The aim of this study was to present long-term results of sagittal osteotomy of the patella after Morscher. The study included 70 patients treated for patellar dysplasia with a postoperative follow-up from nine to 20 years. There were 59 females and 11 males with an average age of 21 years at the time of operation. Results were evaluated for the entire group of 70 patients and then presented separately for the 30 patients in whom sagittal osteotomy of the patella was performed as a single procedure and 40 patients in whom, in addition to sagittal osteotomy of the patella, medialisation and ventralisation or distalisation of the tibial tuberosity were also performed. The mean value of the Wiberg patellar angle was 112 degrees preoperatively and 140 degrees postoperatively. In the whole group of patients excellent results were obtained in 24 (35%), good results in 30 (42%), fair results in 13 (19%) and poor results in three (4%) patients. In 30 patients with sagittal osteotomy as a single operation excellent results were obtained in 13 (43%), good results in 14 (47%) and fair results in three (10%) patients, while in the 40 patients with sagittal osteotomy and additional surgical procedures, 11 (27%) were excellent, 16 (40%) good, ten (25%) fair and three (8%) had poor results. Sagittal osteotomy of the patella after Morscher is an enrichment of the spectrum of the secondary-causal and preventive procedures for the treatment of patello-femoral disorders.
Introduction
When discussing osteotomies around the knee joint, it is rarely appreciated that this term also encompasses patello-femoral osteotomies. Furthermore, it is necessary to differentiate between osteotomies of the distal femur and trochlea, osteotomies of the tibial tubercle in procedures used to correct biomechanical malalignment of the knee extensor apparatus and the osteotomies of the patella.
Osteotomies of the patellofemoral joint date back to 1891 when Pollard chiselled out the lateral wall of the trochlea and imbricated the medial joint capsule [21]. In patients with femoral torsional deformities, Graser in 1904 described a rotational supracondylar osteotomy of the femur for the correction of habitual patellar dislocation [21]. To prevent lateral dislocation of the patella, Luxembourg [16] reported in 1914 a bone barrier procedure where a fibular strut was placed in a trough created on the antero-lateral trochlea. In 1915, Albee [1] performed an open-wedge osteotomy of the antero-lateral condyle in patients with patello-femoral dysplasia and recurrent dislocation. Albee's procedure has been extensively modified over time, but is still used in clinical practice. In 1960, Brissard described a more proximal osteotomy of the femoral cortex aiming to give the patella more stability in full extension, and he termed this procedure Albee Superior osteotomy [21]. Kuroda et al. [15] indicated that a 6 to 10-mm anterior osteotomy of the lateral condyle significantly elevates patello-femoral contact pressures. Keene and Marans have presented the indications for osteotomy of the patella and the femoral sulcus [14]. It is debatable whether it is semantically correct to classify Dejour’s trochleoplasty [6] as osteotomy, but it is unequivocally true that this procedure aims to increase patellar stability and increase the patello-femoral joint congruency.
Osteotomies of the patella may be classified with respect to the plane of osteotomy as sagittal (longitudinal) and coronal (frontal). In 1977, Dellis [7] suggested that coronal osteotomy of the patella should be used in order to decrease thickness of the patella as well as to decrease intraosseous pressure within the patella. Changing these biomechanical (patellar thickness) and biological (intraosseous pressure) parameters would eventually result in a decrease in pain within the patellofemoral joint. The coronal osteotomy and some of its variations have been advocated or questioned by several authors [7, 17, 22, 28, 29]. The senior author of this article (M.P.) has used a procedure which combines lateral release and coronal osteotomy in a lateral to medial direction using an oscillating saw with excision of an approximately 7 mm slice of cancellous bone and fixing two fragments of the osteotomised patella with four transosseous sutures at the corners of the patella. Vaquero and Arriaza [29] described an original procedure, the patella thinning osteotomy, as an alternative to advancement of the tibial tuberosity or patellectomy in cases of severe anterior knee pain. This technique decompresses the patello-femoral joint and produces the biological effect found after other osteotomies.
Sagittal (longitudinal) osteotomy of the patella was introduced in clinical practice by Morscher [18]. In 1978 he published preliminary results of the application of this technique in the treatment of patellar chondromalacia; he subsequently presented the pathophysiological explanation and developed the indications and possibilities for its application [13, 19, 20]. There are two distinct types of saggital osteotomies: Morscher’s saggital or “plus” osteotomy which uses insertion of osseous wedge into the patella, and saggital “minus” or “reduction” osteotomy [5]. The latter procedure is indicated in cases where “patella permagna” (enlarged patella) is present and consists of osseous wedge excision followed by osteosynthesis of the fragments with a single screw. Morscher’s saggital osteotomy was introduced in the Department of Orthopaedic Surgery, School of Medicine University of Zagreb in 1980, and the preliminary, mid-term and long-term results have been reported in numerous articles and conferences [24–27]. With the use of the sagittal osteotomy of the patella it is possible to enlarge the contact surface of the patello-femoral joint and improve the kneading action on the cartilage and hence its nutrition. Osteotomy of the patella according to Morscher [18] may produce the following effects:
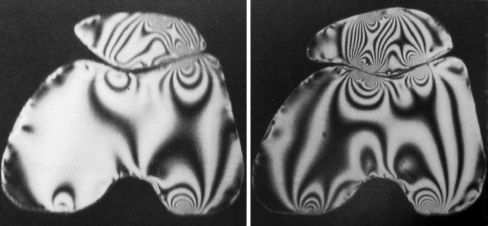
An improved use of the patellar cartilage by enlarging the area of surface contact taking pressure (Fig. 1)
Improvement in nutrition of the cartilage due to a greater area of contact between the medial facet of the patella and the medial femoral condyle
Immediate reduction in intramedullary pressure and thus reduction or elimination of pain as a result of the osteotomy itself
Fig. 1.
Photoelasticimetric model of sagittal osteotomy of the patella constructed according to the pre-(left) and postoperative roentgenograms of a treated knee. Preoperatively, an unequal isochromatic distribution was visible. Following sagittal osteotomy of the patella the stresses were uniformly distributed throughout the patello-femoral joint
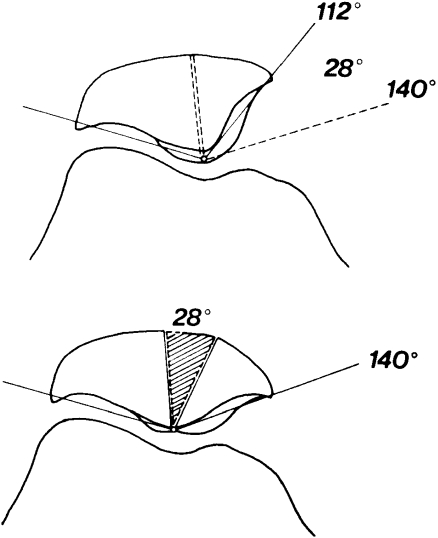
Indications for longitudinal osteotomy of the patella include patellar dysplasia (Wiberg type II/III, III and IV) as well as “hunter’s hat” shaped patella. Longitudinal osteotomy of the patella can be combined with other surgical procedures such as realignment of the knee extensor apparatus or transposition of the patellar ligament insertion, including ventralisation, medialisation and distalisation of the tibial tubercle [24]. The technique of Paar combines an open-wedge longitudinal patellar osteotomy with deepening of the femoral trochlea in patients with patello-femoral dysplasia [23]. All osteotomies require careful preoperative planning and should always include preoperative drawing which should match the postoperative radiograph (Fig. 2). In our experience the best principle to follow during the preoperative planning is to aim for equalisation of Wiberg’s patellar angle and the angle of the femoral trochlea.
Fig. 2.
The mean value of Wiberg's angle preoperatively and postoperatively
The purpose of this article is to present our results of the application of sagittal osteotomy of the patella after Morscher in the treatment of anterior knee pain in patients with patellar dysplasia Wiberg III and IV [30].
Materials and methods
The study included 70 patients treated for patellar dysplasia from 1980 to 1990, with a postoperative follow-up from nine to 20 years. There were 59 females and 11 males with an average age of 21 years at the time of operation. Sagittal osteotomy of the patella was carried out according to the procedure originally described by Morscher [18]. Osteotomy was carried out longitudinally in the region of the ridge between the medial and lateral facet of the patella. After severing the aponeurosis, the osteotomy was performed with an oscillating saw through approximately two thirds of the thickness of the patella. Subsequently, the osteotomy was continued carefully, using an osteotome, down to the cartilage. The patella was then gently opened to the width of the previously calculated bony wedge. A bony wedge was fashioned from homologous bony graft from the bone bank. The wedge must be well sharpened in order to prevent cracking of the patellar cartilage when it is firmly driven into the osteotomy. Postoperatively the knee joint was immobilised in a Robert Jones bandage over a period of 12 days, during which isometric contraction of the quadriceps and flexion of the knee up to 30 degrees was practised. Subsequently, flexion was increased to 60 degrees until the 30th postoperative day, and by the 45th postoperative day flexion of the knee to 90 degrees should be possible. Ten to twelve weeks after operation full range of motion of the knee should be possible. The results were evaluated on the basis of the Bandi and Ficat criteria as excellent, good, fair and poor [3, 8].
Results
Results were evaluated for the entire group of 70 patients and then presented separately for the group of 30 patients in whom sagittal osteotomy of the patella was performed as a single procedure and for the 40 patients in whom, in addition to sagittal osteotomy of the patella, medialisation and ventralisation or sometimes distalisation of the tibial tuberosity were also performed. The mean value of the Wiberg patellar angle was 112 degrees preoperatively and 140 degrees postoperatively (Fig. 2).
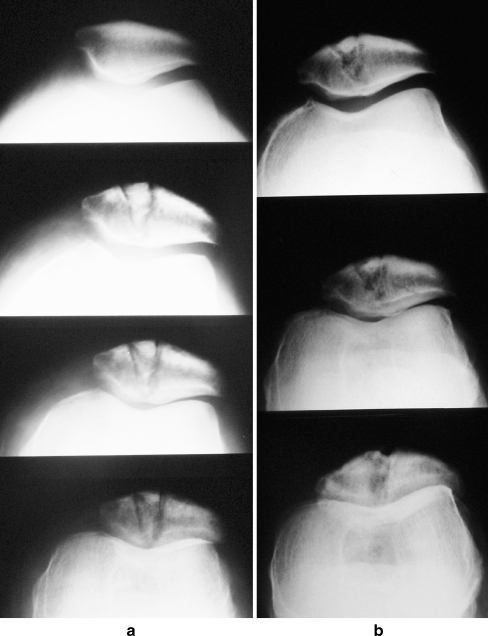
In the whole group of patients excellent results were obtained in 24 (35%), good results in 30 (42%), fair results in 13 (19%) and poor results in three (4%) patients. In 30 patients with sagittal osteotomy as a single operation excellent results were obtained in 13 (43%), good results in 14 (47%) and fair results in three (10%) patients while in the 40 patients with sagittal osteotomy and additional surgical procedures, 11 (27%) were excellent, 16 (40%) good, ten (25%) fair and three (8%) had poor results. Radiographs in Figs. 3, 4, 5 show excellent or good long-term results in the group of patients with sagittal osteotomy as a single operation.
Fig. 3.
Female patient V.G. who was 28 years old at the time of surgery. a Preoperative and immediate postoperative radiographs. b Radiographs 14 years postoperatively
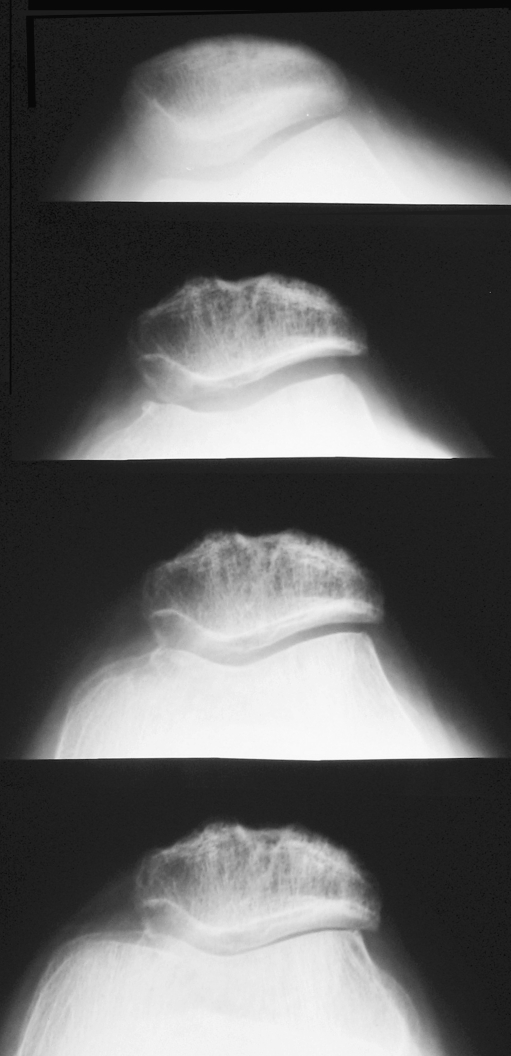
Fig. 4.
Male patient T.P. who was 18 years old at the time of surgery. Preoperative radiograph and radiographs 12 years postoperatively
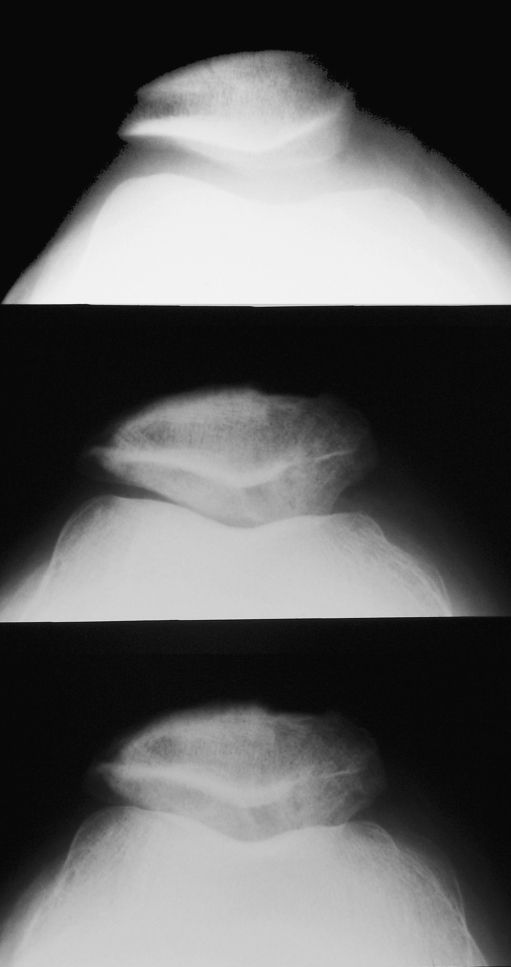
Fig. 5.
Female patient D.P. who was 26 years old at the time of surgery. Preoperative radiograph and radiographs 20 years postoperatively
Out of all the osteotomies of the patella, 16 were done in top-level athletes or ballet dancers, of which there were 12 females and three males (in one female both knees were operated upon) with an average age of 19 years (range 15–28). Among the operated athletes there were five basketball players, two handball players, one volleyball player, two track and field athletes, one gymnast, one karate fighter with both knees operated on (Fig. 6) and three ballet dancers. Successful application of the sagittal osteotomy of the patella has been confirmed by the fact that all, i.e. 16 of the operated athletes except one (karate fighter), returned to competitive sports and three ballerinas returned to professional ballet dancing.
Fig. 6.
Radiographs nine years postoperatively in karate fighter with both knees operated on
We had no intraoperative or postoperative complications in the surgically-treated athletes. However, in the entire group of 70 surgically-treated patients we did have some complications. Among the complications encountered were five cases requiring manipulation of the knee under anaesthesia some six weeks after the initial operative intervention. In one patient osteosynthesis of the patella had to be carried out. The ultimate result, however, was good because the patient consented to undergo surgery of the other knee.
Discussion
Sagittal (longitudinal) osteotomy was advocated by Morscher [19], and in his report of four-year follow-up only one patient had a poor result and underwent a second procedure. Subjectively, the patients were enthusiastic and satisfied. Hejgaard and Arnoldi [12] reported that 92% of patients had highly significant relief of pain five to 19 months following this procedure.
At first sight it seems inappropriate to claim that no poor results were obtained in treatment. We had 13 patients in whom only a fair result was obtained and three patients with a poor result. In 30 patients with sagittal osteotomy as a single operation (without additional procedures) no poor results were obtained and fair results were recorded in only in three patients. In 30 patients with sagittal osteotomy performed as a single surgical procedure the cause of the chondromalacia (anterior knee pain) was obviously dysplasia of the patella without any other biomechanical disorders in the patello-femoral joint. To obtain optimal results in the treatment of patellar chondromalacia, it is necessary to tailor surgical procedures in accordance with the aetiological factors. It would then be possible to avoid complications such as lateralisation of the patella following sagittal osteotomy as mentioned by Goymann in 1980 [9]. A question also arises in this case on the necessity of modifications in the application of patellar sagittal osteotomy [10]. According to Biedert [4] skeletal geometry, soft tissues, and neuromuscular control influence the patello-femoral gliding mechanism. Osteotomy with soft tissue repair might be the best treatment depending on the primary pathology. Surgery aims to eliminate the underlying pathomorphology.
Numerous examinations and observations suggest an increase in the patellar intraosseous pressure as the cause of the pain [2, 11, 12, 18, 21] and all the authors concluded that relief of pain following osteotomy is attributable to a reduction in elevated intraosseous pressure. Attempts have been made in the past to calculate the compression forces and contact pressures in the patello-femoral joint mathematically. Apart from these studies, experiments have been designed to provide information on the pressure and contact areas in the joint [13]. Hehne et al. [11] experimentally measured contact area after sagittal osteotomy of the patella on 11 cadaver knees of the types II, II/III and III according Wiberg. They concluded that less incongruence is present, as can be expected, from the bone cross-section of the patella. In our experience the most important aspect of planning sagittal osteotomy of the patella is to follow the principle that, postoperatively, Wiberg's angle of the patella and the angle of the femoral trochlea notch should be approximately equal. This is necessary to avoid so-called bridging of the patella over the trochlear groove.
This article presents the results of the treatment of patellar dysplasia using the classical medial parapatellar surgical approach. The length of the incision was dependent on whether additional procedures, such as transposition of the tibial tubercle, were used in addition to saggital osteotomy. After 1990 the authors modified the original procedure to an arthroscopically-assisted procedure. Arthroscopy was used to inspect the knee joint and perform lateral release, followed by saggital osteotomy. After the osteotomy, the articular cartilage of the patella was checked for congruency. If transposition of the tibial tuberosity was necessary, the incision was extended distally. None of the observed complications with the open procedure (patello-femoral adhesions or fractures of the joint surface) were present after the arthroscopically-assisted procedure. Nagel and Scuderi [21] concluded: “Osteotomy remains an alternative; however, we feel that more controlled long-term studies with greater numbers are needed before its true value can be measured”.
Conclusion
In conclusion it should be emphasised that the results achieved by the application of sagittal osteotomy of the patella are very good. Depending on the malalignment of the extensor mechanism of the knee and the extent of damage of the cartilage of the patella, sagittal osteotomy of the patella should be applied in combination with medialisation and ventralisation or distalisation of the tibial tuberosity. Sagittal (longitudinal) osteotomy of the patella after Morscher is an enrichment of the spectrum of the secondary-causal and preventive procedures for the treatment of patello-femoral disorders.
References
- 1.Albee FM. The bone graft wedge in the treatment of habitual dislocation of the patella. Med Rec. 1915;88:257–259. [Google Scholar]
- 2.Arnoldi CC. Patellar pain. Acta Orthop Scand Suppl. 1991;244:1–29. doi: 10.3109/17453679109153923. [DOI] [PubMed] [Google Scholar]
- 3.Bandi W. Les resultats de l'avancement da la tuberosite anterieure du tibia. Rev Chir Orthop. 1980;66(4):275–278. [PubMed] [Google Scholar]
- 4.Biedert RM. Osteotomies. Orthopade. 2008;37(9):872. doi: 10.1007/s00132-008-1294-5. [DOI] [PubMed] [Google Scholar]
- 5.Bornand F. Treatment of chondritis of the patella using reduction osteotomy. Rev Med Suisse Romande. 1988;108(7):577–581. [PubMed] [Google Scholar]
- 6.Dejour D, Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc. 2007;15(1):39–46. doi: 10.1097/JSA.0b013e31803035ae. [DOI] [PubMed] [Google Scholar]
- 7.Deliss L. Coronal patellar osteotomy: preliminary report of its use in chondromalacia patellae. Proc R Soc Med. 1977;70(4):257–259. doi: 10.1177/003591577707000413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ficat P. Pathologie femoro-patellaire. Paris: Masson et Cie; 1970. [Google Scholar]
- 9.Goymann V. Die Biomechanik des patellofemoralen Gleitwegs. Orthop Praxis. 1980;16:451–461. [Google Scholar]
- 10.Griss P. Modification of sagittal osteotomy of the patella as treatment of excentric chondromalacia or retropatellar arthrosis. Preliminary communication. Z Orthop Ihre Grenzgeb. 1980;118(5):822–824. doi: 10.1055/s-2008-1053543. [DOI] [PubMed] [Google Scholar]
- 11.Hehne HJ, Schlageter M, Riede UN. Experimental patello-femoral contact print measurements. 2. Report: sagittal osteotomy of the patella according to Morscher. Z Orthop Ihre Grenzgeb. 1981;119(4):405–411. doi: 10.1055/s-2008-1051647. [DOI] [PubMed] [Google Scholar]
- 12.Hejgaard N, Arnoldi CC. Osteotomy of the patella in the patellofemoral pain syndrome. The significance of increased intraosseous pressure during sustained knee flexion. Int Orthop. 1984;8(3):189–194. doi: 10.1007/BF00269915. [DOI] [PubMed] [Google Scholar]
- 13.Henche HR, Kunzi HU, Morscher E. The areas of contact pressure in the patello-femoral joint. Int Orthop. 1981;4(4):279–281. doi: 10.1007/BF00266069. [DOI] [PubMed] [Google Scholar]
- 14.Keene GCR, Marans HJ. Osteotomy for patellofemoral dysplasia. In: Fox JM, Pizzo W, editors. The patellofemoral joint. New York: McGraw-Hill; 1993. pp. 169–176. [Google Scholar]
- 15.Kuroda R, Kambic H, Valdevit A, Andrish J. Distribution of patellofemoral joint pressures after femoral trochlear osteotomy. Knee Surg Sports Traumatol Arthrosc. 2002;10(1):33–37. doi: 10.1007/s00167-001-0256-9. [DOI] [PubMed] [Google Scholar]
- 16.Luxembourg H. Zur Behandlung der habituellen Patella Luxation. Med Klin. 1914;10(I):1013–1014. [Google Scholar]
- 17.Maquet P, Vaquero J, Arriaza R. The patella thinning osteotomy. Int Orthop. 1993;17(3):205. doi: 10.1007/BF00186388. [DOI] [PubMed] [Google Scholar]
- 18.Morscher E. Osteotomy of the patella in chondromalacia. Preliminary report. Arch Orthop Trauma Surg. 1978;92(2–3):139–147. doi: 10.1007/BF00397950. [DOI] [PubMed] [Google Scholar]
- 19.Morscher E. Indications and possibilities of patella wedge osteotomy. Orthopade. 1985;14(4):261–265. [PubMed] [Google Scholar]
- 20.Morscher E, Dick W. Die sagitalle Patellaosteotomie bei Chondromalacia patellae. Orthop Prax. 1980;8:692–696. [Google Scholar]
- 21.Nagel A, Scuderi RG. Osteotomy of the patellofemoral joint. In: Scuderi RG, editor. The patella. New York: Springer-Verlag; 1995. pp. 247–252. [Google Scholar]
- 22.Nerubay J, Katnelson A. Osteotomy of the patella. Clin Orthop Relat Res. 1986;207:103–107. [PubMed] [Google Scholar]
- 23.Paar O. Deepening of the trochlea femoris and osteotomy of the patella as possible causal therapy of recurrent traumatic patellar dislocations. An experimental study. Unfallchirurg. 1987;90(9):435–440. [PubMed] [Google Scholar]
- 24.Pećina M. Longitudinal osteotomy of the patella after Morscher. In: We M, We H, editors. Surgery and arthroscopy of the knee. Berlin Heidelberg: Springer; 1988. pp. 471–476. [Google Scholar]
- 25.Pećina M (1992) Longitudinal osteotomy of the patella in the treatment of chondromalacia in top-level athletes. First World Congress of Sports Trauma, Palma De Mallorca, Spain, pp 205–206
- 26.Pećina M (1995) Longitudinal (sagittal) osteotomy of the patella in the treatment of anterior knee pain. Sports medicine 2000. Book of abstracts. Stockholm, p 56
- 27.Pećina M (1997) Long-term results of sagittal osteotomy of the patella. Abstracts of posters and videos. Third congress of EFORT, Barcelona, p 325
- 28.Sloan KW. Osteotomy of the patella. Clin Orthop Relat Res. 1988;234:309–310. [PubMed] [Google Scholar]
- 29.Vaquero J, Arriaza R. The patella thinning osteotomy. An experimental study of a new technique for reducing patellofemoral pressure. Int Orthop. 1992;16(4):372–376. doi: 10.1007/BF00189622. [DOI] [PubMed] [Google Scholar]
- 30.Wiberg G. Roentgenographic and anatomic studies on the femoro-patellar joint. Acta Orthop Scand. 1944;12:319–410. [Google Scholar]