Abstract
Surgical correction of bowed legs should be performed as early as possible. Overload osteoarthritis, even without significant varus deformity of the knee, is a further indication for open-wedge high-tibial osteotomy. Progression of damage to the joint surfaces due to overloading can be significantly retarded by realigning the extremity with the aim to, at least, reduce overload on the medial compartment to a value close to physiological. Significant improvement to open-wedge high-tibial osteotomy (OWHTO) has been made on two fronts: (a) by the use of a more appropriate surgical technique and (b) by promoting osteogenesis through an angular-stable fixation device with just the correct amount of elasticity. A retrospective study of 53 consecutive cases in which no interposition material was used to fill the wedge, with gap openings between 5 mm and 20 mm, showed that ossification of the gap always progressed from the lateral hinge towards the medial side. Standard radiographs showed 75% of the gap filled in with new bone within 6−18 months. In conclusion, we believe that open-wedge high-tibial osteotomy using the TomoFix® plate has proved to be successful in treating unicompartmental gonarthrosis, even without bone grafts or bone-substitute material.
Introduction
Pain and difficulties in ambulation encountered by individuals with bowed legs and knocking knees have been well known and reported for centuries. However, these disorders were only clearly defined by Mikulicz-Radecki who in 1880 first observed that in most “normal” individuals, a straight line could be drawn in the frontal plane, with the knee extended, through the centres of three joints: the hip, the knee and the ankle. He then defined genu varum, or genu valgum, as the condition when the centre of the knee joint appreciably deviated from the line connecting the other two centres. Mikulicz himself termed this the “Direktionslinie”, or direction line [7].
Biomechanical reflections early in the twentieth century already indicated that a varus knee would load the medial compartment excessively, whereas a valgus knee would expose the lateral compartment to overload, and Mikulicz’s line began to be referred to as the load-carrying line or the mechanical axis [7]. Whereas the concept of such terminology might be acceptable when the patient is standing on both legs, it does not apply to one-legged stance—a common situation in human walking—where the line of gravity passes medial to the whole knee. Total tibiofemoral forces (that include stabilising muscle forces) have been estimated to amount to well over twice the body weight in normal walking, and in some activities, such as walking down stairs, forces might even be close to five times the body weight. Furthermore, the greater part of this force is transmitted through the medial compartment of the joint [12, 13, 16]. Cartilaginous degeneration is also more commonly encountered in the medial compartment. Subsequent osteoarthritic deformation of the region results in marked varisation, which further increases the distance between the line of gravity and the joint, calling for still more muscular activity to stabilise the joint in the frontal plane, hence creating more overload in this area and subsequently accelerating progression of the deformity. Furthermore, soft tissue distension on the lateral side of the joint gives rise to severe pain.
The most widely used surgical technique for unicompartmental osteoarthritis of the knee in the second half of the twentieth century was that advocated by Coventry—a lateral closed-wedge, high-tibial valgisation procedure [5]. This approach and the medial open-wedge high-tibial technique [9] have been used since the 1990s especially, but not exclusively, in sports medicine for young, active patients with medial compartment osteoarthritis [19, 20]. The closed-wedge technique, which requires removal of a wedge of bone from the lateral aspect of the tibia in the metaphyseal region, necessitates cutting along two planes. Also, shortening of the fibula is involved. Apart from the leg-shortening that ensues, neurological deficits of up to 27% and several shortcomings have been reported that include difficulty in intraoperatively controlling the amount of achieved correction, the need to re-insert the extensor muscle, persistent ligamentous instability and problems associated with implantation of an artificial knee at a later date [2, 17, 21]. Because of these disadvantages, the open-wedge technique gained importance. Particularly interesting were the encouraging results published by Hernigou on open-wedge high-tibial osteotomy (OWHTO) [10]. Stimulated by this, a group of orthopaedic surgeons joined forces as a Knee Expert Group with the support of the AO-Foundation® with the aim of closely examining the advantages and disadvantages of the open-wedge technique and to further develop this procedure, as required [11].
Open-wedge high-tibial osteotomy (OWHTO)
Open wedge osteotomies might be traced back to the earliest methods of correcting deformities in long bones: by forcefully breaking the bone, then allowing healing to occur in the desired position with the aid of suitable splints. Modern techniques involve sawing and chiselling through the bone and the application of an internal (or external) splint to fix the fragments in the required juxtaposition until bone healing is complete. Inclusion of a bone graft within the open wedge, or some other material to enhance bone healing, is sometimes advocated. In treating varus knee deformity, the saw cut is basically made from the medial aspect of the tibia within the metaphysis, proceeding parallel to the subchondral cortex towards the lateral side, leaving a narrow margin of bone undivided at the end of the cut. The cleft thus made is then distended on the medial side in a controlled manner to form an open-wedge-shaped gap. The narrow margin of uncut bone serves as a hinge at the apex of the wedge while also preventing complete displacement of the tibial fragments with respect to each other.
Because of the high force transmitted through the medial compartment of the joint, some means of supporting the disrupted tibial structure is necessary. The initial and most obvious way to deal with this is to insert a bone graft inside the open wedge. Further stabilisation of the tibial structure with a splint has been recommended until bone healing is complete. The bone graft is expected to exercise a dual function: (a) to enhance bone healing and (b) to afford mechanical support by transmitting a considerable part of the high axial compressive forces that occur. This expectation is difficult to maintain when factors such as the rigidity of the splint (or any fixation that bridges the wedge) and bone resorption at the two bone/graft interfaces are considered. Nevertheless, angulated blade plates, and other plates of various configurations, have been used in conjunction with bone grafts taken from the pelvic crest. Because of the well known occurrence of significant donor-site problems encountered with autologous bone grafts, various substitute materials have also been employed. However, the results often fall short of expectations, and much effort is still being expended to improve the outcome [3].
After first using commonly available osteosynthesis material (AO stainless steel T plates, 95° titanium blade plates and the first-generation Puddu plate) with standard surgical procedures as practised by Hernigou et al. in OWHTO, we realised that significant improvement could only be made on two fronts: (a) by use of a more appropriate surgical technique and (b) by promoting osteogenesis through an angular stable fixation device with just the correct amount of elasticity [4, 6, 14].
Surgical technique
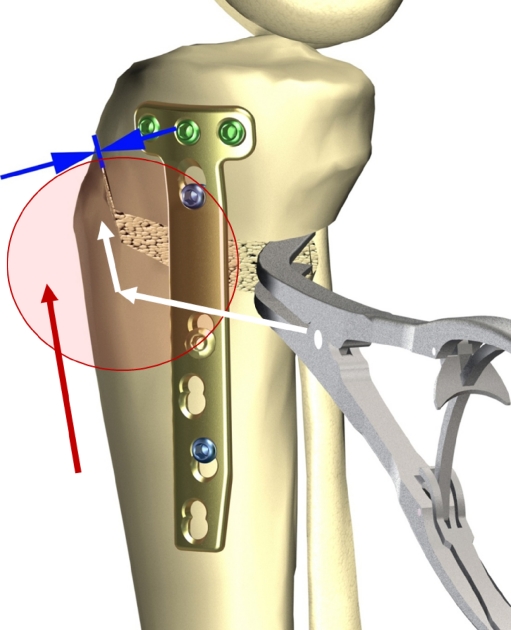
A simple bone cut along a strictly transversal (horizontal) plane would of necessity be located somewhere proximal to the insertion site of the patellar tendon, leaving little room for adequate attachment of any fixation device to the proximal tibial fragment. Therefore, an oblique bone cut starting further distally, medially and terminating close to the upper border of the tibiofibular joint was chosen. The entire patellar tendon attachment to the distal tibia could be preserved by means of a further bone cut located in the frontal plane parallel to the ventral tibial edge, about 1.5 cm behind the ventral surface of the tubercle. The two osteotomy planes make an obtuse angle of about 110° to each other (Fig. 1). Apart from enabling uninterrupted force transmission through the patellar tendon to the distal tibial fragment, the anterior bone contact through buttressing also prevents forward slipping, tilting and rotation of the proximal fragment. Furthermore, it promotes fast bone healing in this area.
Fig. 1.
Biplanar osteotomy with TomoFix® plate showing the two osteotomy planes
Over time, several important improvements to the surgical technique were introduced. It was noted, for example, that the final tibial slope in the sagittal plane was a major issue in determining the range of joint flexion−extension. Inadvertent increase of the tibial slope posteriorly has been attributed to the rather anterior positioning of the fixture that bridges the wedge, together with the tightening effect of the ligaments and muscles on the medial side. Therefore, knees with appreciable extension deficit due to contracture of soft tissues on the medial side especially require sufficient distal release of these structures. It has also been shown that only through adequate release of the medial collateral ligament could the medial compartment be relieved of static pressure from this source [1].
The transverse oblique osteotomy is done with two 65-mm-long and 0.9-mm-thick saw blades (narrow and broad, with depth scale), starting immediately proximal to the pes anserinus muscle insertion site and proceeding laterocranially, with the cut directed towards the upper border of the tibiofibular joint. Care must be taken to ensure that 1.5 to 2 cm of bone stock is preserved at the base of the tibial tuberosity and that the bone cut ends about 1−1.5 cm away from the lateral margin of the tibia in unidirectional valgisation. The second cut, parallel to the ventral edge of the tibial diaphysis, is made with a thinner 0.5-mm blade. Cooling the oscillating saw by continuous irrigation is important to avoid heat necrosis.
The bone cut is now slowly prised open from the medial side to form an open wedge of the required size by sequentially inserting a series of chisels overlying each other. Sufficient time must be allowed for the bone in the region of the lateral hinge to gradually distend by controlled fissuring without the occurrence of a complete fracture. The chisels are then replaced by a dorsomedially intercortically positioned spreader, and the fixation device is applied as posteriormedially as possible. The desired amount of wedge opening (varus correction)—as previously determined on radiographs with the patient standing on both legs in full knee extension—is monitored through fluoroscopy during surgery. A straight alignment rod (Synthes®) placed strictly anterior to the centres of the hip and ankle joints is a reliable aid to check the position of the Mikulicz line in relation to the knee (beware of parallax error and consistent rotation!).
Bone graft, or substitute, might be used to fill in the open wedge if desired, but the first author (AES) considers this unnecessary. Suction within the open wedge during surgery is discouraged: the blood clot with bone cells should be preserved. Haemostatic fleece, or just a periosteal flap with the adjacent soft tissues, and the plate, covers the gap adequately.
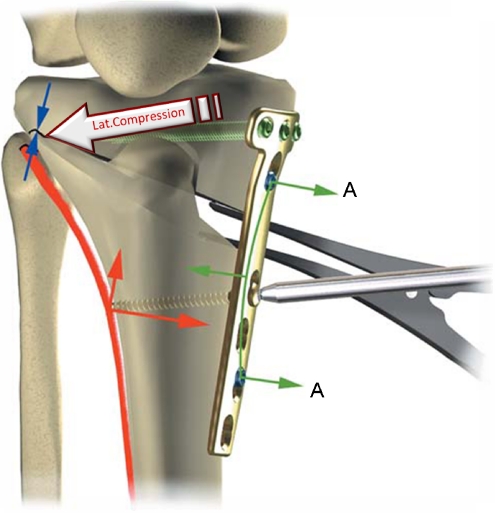
In cases in which an extension deficit is present due to contracture of the medial and dorsomedial soft tissues, the lateral hinge might have to be severed. This is carried out under fluoroscopic guidance. The knee is brought into full extension, taking care not to go beyond a tibial slope of 0°. Reduction of the intentionally disrupted lateral hinge may be greatly facilitated through the use of the TomoFix® plate described below.
The internal fixation device (splint)
In the course of our endeavours, it was realised that a more successful internal fixation device might be arrived at by use of angular-stable, locked compression bone screws with special heads that lock to the plate that bridges the open wedge. The locking compression plate (LCP), as devised by Synthes®, served as the basis on which further development evolved. By this means, not only was an angular stable supporting device obtained, but also one that exhibited the elasticity required to maintain pre-tension across interposition material, if this be used at all, or across the lateral bone hinge. Elasticity of the device could also prove to be an important factor in encouraging bone growth inside the wedge by mechanical stimulation according to Wolff’s law [18, 22].
The device that ultimately emerged under the trade name of TomoFix® (Synthes GmbH; Solothurn, Switzerland) (Fig. 2), consists of a T-shaped titanium plate with three locking holes in the cross-bar and a combination hole for the four screws that engage with the proximal tibial fragment, and a staggered row of four combination holes in the shank for fixation to the distal part of the bone. Combination holes serve for compression of bone fragments by permitting the screw head to glide along the plate while being tightened and enable the head to be locked in place. The plate is 115-mm long and has been made to suit the bone form for an average of 10° wedge opening. The three proximal locking screws are seated at a fixed angle of 4° to the plate, thus ensuring the screws do not enter the joint space of the lateral compartment. All four screws in the proximal fragment converge to support the lateral hinge. The tapered threaded plate holes distal to the osteotomy are fitted with screws that might be chosen to engage either monocortically or bicortically with the bone. It is important that all four holes are fitted with screws, since a vacant hole would give rise to high stress concentration and promote fracture of the plate under load. The fixation device is so designed that on tightening a screw inserted into the first plate hole distal to the osteotomy, the distal bone segment is pulled towards the plate, and by virtue of the oblique osteotomy, the two tibial fragments are brought together giving rise to compression of the lateral hinge. This compression effect serves to stabilise the lateral hinge, even when it has been disrupted (Fig. 3).
Fig. 2.
Evolution of the medial proximal tibia (MPT) TomoFix® plate
Fig. 3.
A “fissured” lateral hinge, and in case of disruption its reduction, by drawing the distal fragment towards the plate. Short spacer screws (A) keep the plate 3 mm away from the cortex at these points
Radiological results
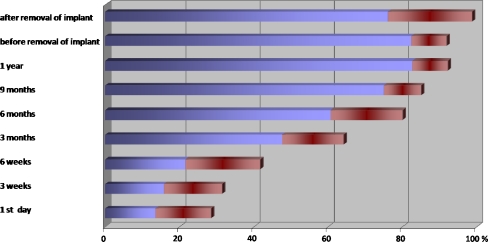
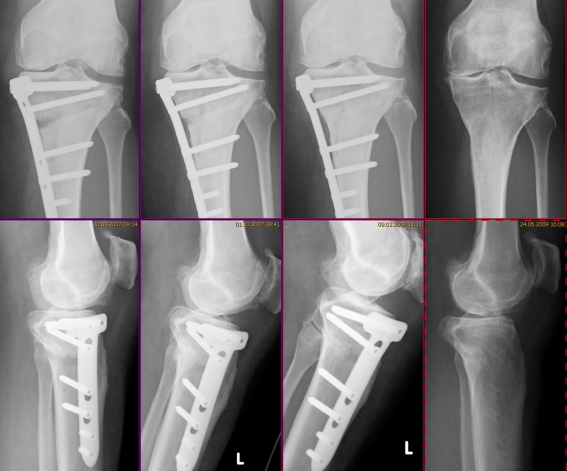
A retrospective study of 53 consecutive cases in which no interposition material was used to fill the wedge, with gap openings between 5 mm and 20 mm (Table 1), showed that ossification of the gap always progressed from the lateral hinge towards the medial side. Standard radiographs showed at least 75% of the gap filled in with new bone within 6−18 months (Figs. 4 and 5). The plate should therefore not be removed before 12−18 months after implantation. Weight bearing up to the point of discomfort was encouraged as early as two days after surgery.
Table 1.
Some details of the 53 patients with open-wedge high-tibial osteotomy (OWHTO)
| Age (years); mean (range) | Men:women; number (%) | Medial post-operative distraction (mm); mean (range) |
|---|---|---|
| 50 (18−71) | 39:14 (74:26) | 10 (5–20) |
Fig. 4.
Bone-to-bone contact at the osteotomy site without interpositioned graft, as seen on anterior−posterior radiographs (bone growth proceeds from lateral to medial)
Fig. 5.
A typical follow-up showing bone growth without interpositioned graft (53-year-old woman; wedge opening 10 mm, 6 weeks, 3 months, 6 months, 23 months postoperatively)
Discussion and conclusion
Surgical correction of bowed legs should be performed as early as possible [15]. Overload osteoarthritis, even without significant varus deformity of the knee, is a further indication for OWHTO. Progression of damage to the joint surfaces due to overloading can be significantly retarded by realignment of the extremity with the aim of at least reducing the overload on the medial compartment to a value close to physiological. Further reduction of medial load by making the line of Mikulicz pass far lateral to the intercondylar eminence would only cause the lateral joint to suffer overload while taking the risk of knee knocking during ambulation [9, 10]. The amount of correction (valgisation) to be aimed at is still much debated. Fujisawa et al. reported good results when the Mikulicz line passed through a point between 30% and 40% lateral to the midpoint of the knee (total width of knee being 200%). Based on this, the term “Fujisawa point” has been coined, which is defined as 62% of the entire width, measured from the medial side [4, 8]. We advocate some overcorrection of the varus deformity, but not more than 5°, and not beyond the Fujisawa point.
In conclusion, we can state that OWHTO with use of the TomoFix® plate has proved to be successful in treating unicompartmental gonarthrosis, even without bone grafts or bone substitute material. Currently, an outcome study of more than 500 cases that have undergone OWHTO with the first-generation TomoFix® plate is being carried out.
Acknowledgments
Conflict of interest AES is a scientific consultant for Synthes® and receives financial benefit for this purpose.
References
- 1.Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P. The effects of valgus medial open wedge high tibial osteotomy on articular cartilage pressue of the knee: a biomechanical study. Arthroscopy. 2007;23:852–861. doi: 10.1016/j.arthro.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 2.Aydoğdu S, Cullu E, Arac N, Varolgüneş N, Sur N. Prolonged proneal nerve dysfunction after high tibial osteotomy: pre- and postoperative electrophysiological study. Knee Surg Sports Traumatol Arthrosc. 2000;8:305–308. doi: 10.1007/s001670000138. [DOI] [PubMed] [Google Scholar]
- 3.Bekerom MPJ, Patt TW, Kleinhout MY, Vis HM, Albers GHR. Early complications after high tibial osteotomy: a comparison of two techniques. J Knee Surg. 2008;21:68–74. doi: 10.1055/s-0030-1247797. [DOI] [PubMed] [Google Scholar]
- 4.Brinkman J-M, Lobenhoffer P, Agneskirchner JD, Staubli AE, Wymega AB, Heerwarden RJ. Osteotomies around the knee. J Bone Joint Surg Br. 2008;90-B:1548–1557. doi: 10.1302/0301-620X.90B12.21198. [DOI] [PubMed] [Google Scholar]
- 5.Coventry MB. Osteotomy of the upper portion of the tibia for degenerative arthritis of the knee. A preliminary report. J Bone Joint Surg. 1965;47:984–990. [PubMed] [Google Scholar]
- 6.Simoni C, Staubli AE. Neue Fixationstechnik für medial open-wedge Osteotomien der proximalen Tibia. Schweiz Med Wochenzeitschrift. 2000;119:130. [Google Scholar]
- 7.Fick R. Handbuch der Anatomie und Mechanik der Gelenke, Teil 3. Jena: Gustav Fischer; 1911. [Google Scholar]
- 8.Fujisawa Y, Masuhara K, Shiomio S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic stuy of 54 knee joints. Orthop Clin North Am. 1979;10:585–608. [PubMed] [Google Scholar]
- 9.Heller MO, Taylor WR, Perka C, Duda GN. The influence of alignment on the musculo-skeletal loading conditions at the knee. Langenbecks Arch Surg. 2003;388:291–297. doi: 10.1007/s00423-003-0406-2. [DOI] [PubMed] [Google Scholar]
- 10.Hernigou P, Medeveielle D, Debeyre J, Goutallier D. Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987;69:332–354. [PubMed] [Google Scholar]
- 11.Lobenhoffer P, Heerwarden RJ, Staubli AE, Jakob RP. Osteotomies around the knee. Stuttgart and New York: Thieme; 2008. [Google Scholar]
- 12.Morrison JB. Bioengineering analysis of force actions transmitted by the knee joint. Bio-Med Eng. 1968;4:164–170. [Google Scholar]
- 13.Mündermann A, Dyrby CO, D’Lima DD, Colwell CW, Andriacchi TP (2008) In vivo knee loading characteristics during activities of daily living as measured by an instrumented total knee replacement. J Orthop Res: 1167–1172 [DOI] [PubMed]
- 14.Nelissen EM, van Langelaan EJ, Nelissen RGHH (2009) Stability of medial opening wedge high tibial osteotomy: a failure analysis. Int Orthop Feb 3. doi:10.1007/s00264-009-0723-3 [DOI] [PMC free article] [PubMed]
- 15.Odenbring S, Tjönstrand B, Egund N, Hagstedt B, Hovelius L. Function after tibial osteotomy for medial gonarthrosis below aged 50 years. Acta Orthop Scand. 1989;60:527–531. doi: 10.3109/17453678909150116. [DOI] [PubMed] [Google Scholar]
- 16.Paul JP. Loading on normal hip and knee joints and on joint replacements. In: Schaldach M, Hohmann D, editors. Advances in artificial hip and knee joint technology. Heidelberg and New York: Springer, Berlin; 1976. [Google Scholar]
- 17.Rozbruch SR, Parvizi J, Hanssen AD, Spangehl MJ. Total knee arthroplasty following proximal tibial osteotomy. Reply. J Bone Joint Surg (Am) 2004;86:2571. doi: 10.2106/00004623-200411000-00043. [DOI] [PubMed] [Google Scholar]
- 18.Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a balance between stability and biology. J Bone Joint Surg Br. 2002;84:1093–1110. doi: 10.1302/0301-620X.84B8.13752. [DOI] [PubMed] [Google Scholar]
- 19.Salzmann GM, Imhoff AB. Sporting activity after tibial osteotomy. Sports Orthop Trauma. 2009;25:84–87. doi: 10.1016/j.orthtr.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 20.Simonian PT, Cole BJ, Bach BR, editors. Sports injuries of the knee: Surgical approaches. New York: Thieme; 2006. [Google Scholar]
- 21.Tunggal JA, Higgins GA, Waddell JP. Complications of closing wedge high tibial osteotomy. Int Orthop. 2009 doi: 10.1007/s00264-009-0819-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wolff J. The Law of Bone Remodeling (translation of the German 1892 edition) Berlin: Springer; 1986. [Google Scholar]