Abstract
The aim of this study was to present the different surgical procedures of tibial tubercle osteotomies for patellar instability or patellar mispositioning such as patella alta or patella infera. This study analysed the Caton–Deschamps index used for assessment of vertical patella height in order to make a precise plan for tibial tuberosity osteotomies. This study included 61 knees (50 patients) treated for patellar instability with patella alta and 24 patients treated for patella infera of mechanical origin. The results of medial transfer of the tibial tuberosity, with or without distal transfer in cases of patellar instability with patella alta, gives excellent results for stability in 76.8% of the cases. The results of the proximal transfer of the tibial tuberosity in cases of patella infera were excellent or good in 80% of the cases in our series of 24 patients. A precise preoperative plan is needed with determination of the vertical patellar height using the Caton–Deschamps index and the situation of the tibial tuberosity and the Tibial Tubercle to Trochlear Groove distance (TT-TG) of the knee on CT scan in order to obtain satisfactory results.
Introduction
Patellar instability and abnormal patellar vertical height are defined by clinical and radiological criteria.
Patellar instability and patella alta are defined by passive and active clinical criteria. The recurrent dislocation of the patella may show radiological signs such as dysplasia of the trochlea with the Dejour’s crossing sign [10, 11] and sometimes a patella alta on the sagittal view of the knee with a Caton Deschamps’ index [4, 5] equal or more than 1.2 and a TT-TG (distance between the tibial tubercle and the trochlear groove) on the CT scan (D. Goutallier and J. Bernageau) [12–1] with a normal value in full extension between 10 and 15 mm.
The clinical criteria for diagnosing the patella infera are pain, loss of mobility in flexion and sometimes instability. Radiological criteria are a low patella on the sagittal view of the knee and a Caton–Deschamps index equal or less than 0.6.
The most common surgical procedure for the treatment of femoro patellar dysplasia, patella alta or patella infera is a tibial tubercle osteotomy. The Roux Elmslie-Trillat [17–19] procedure is recommended for the treatment of instability without patella alta. Complete detachment of the tibial tubercle with proximal transfer is recommended for patella infera and distal transfer is recommended for correction of the patella alta.
The aim of this study was to present the results of tibial tubercle osteotomy and transfer in a clinical series of patients operated upon for patellar height disturbances.
Materials and methods
Assessment of the patellar height
Preoperative planning requires assessment of the patellar vertical height and of the patellar tendon length.
There are different methods to evaluate patellar height. The oldest was the Blumensaat method using a femoral landmark [3]. The most accurate methods use tibial landmarks. This category includes the Insall and Salvati’s index [13], the Blackburne and Peel’s index, the Caton–Deschamps index or Linclau and De Carvalho’s index, which is practically the same as the Caton–Deschamps index [6–5] and the Southern Chinese reference (PAI) only for patella alta [14].
In our opinion the most accurate diagnostic method is the Caton–Deschamps index because this ratio relies on readily identifiable and reproducible anatomical landmarks and is possible regardless of the quality of the X-rays, knee size, radiological enlargement or position of the tibial tubercle or patellar modification and knee flexion between 10° and 80°
Described for the first time by J. Caton in 1976, this ratio was modified in 1982 and is currently known as the Caton–Deschamps index [4, 5].
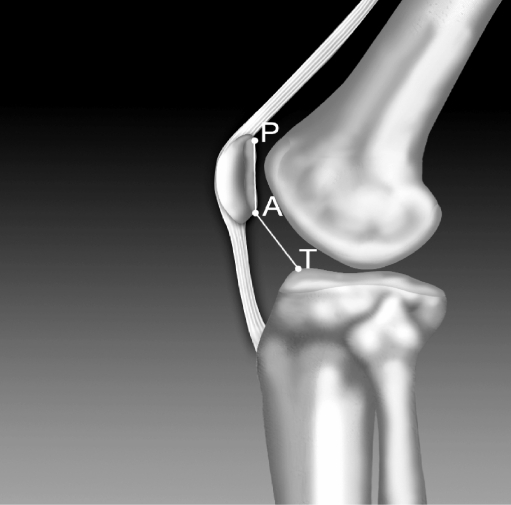
The method (Fig. 1) consists of plotting the distance between the inferior edge of the patellar joint surface and the antero-superior angle of the tibia on sagittal X-rays (AT) and the joint length of the patella (AP).
Fig. 1.
Caton–Deschamps index. Normal value for AT/AP=1; patella alta AT/AP≥1.2; patella infera AT/AP≤0.6
The value ratio AT/AP is normally equal to 1 (0.96 ± 0.134 for men and 0.99 ± 0.129 for women). When the ratio is equal or superior to 1.2 it is defined as patella alta and when the ratio is less than or equal to 0.6 it is a patella infera.
Preoperative planning for patella infera also requires the precise assessment of the patellar tendon length on a sagittal MRI view which is an average 4.2 cm (2.8 to 6.3) according to Shabshin et al. [18].
Using the archives of the authors’ institution [6], we made a retrospective study on two population groups. The first group of 50 patients (61 knees) showed patello-femoral instability with patella alta and the second group of 24 patients showed a mechanical patella infera, notably of tibial tuberosity origin with a patellar tendon length over 2.5 cm.
Technique
Medial tibial tubercle transfer by osteotomy
Tibial tubercle transfer was introduced in clinical practice by Roux in 1888 and then further modified by authors such as Elmslie and A.G. Trillat [19].
Distal or proximal transfers by complete detachment of the tibial tubercle were introduced by J. Caton in 1982 for patella infera [4].
This procedure involves the displacement of the tibial tubercle with its insertion of the patellar tendon in order to realign the extensor mechanism of the knee and/or correct the vertical patellar height.
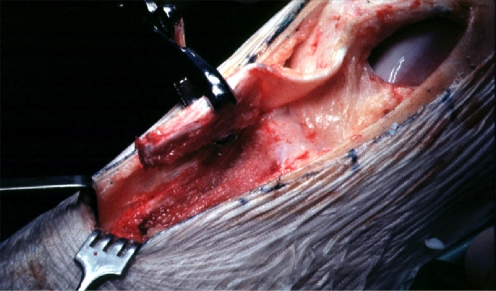
Using the anteromedial approach, there is a lateral retinacular release and verification of the intraarticular space by arthrotomy or arthroscopy, followed by a section of the medial soft tissue to obtain complete exposure of the tibial tubercle. After identification of the patellar tendon insertion it is possible to perform the osteotomy, generally with a bone chisel.
Medial tubercle transfer is indicated for femoro-patellar instability without patella alta.
The tibial tubercle is fully detached with the chisel on three sides leaving only a distal bony hinge before elevating the medial periosteum. Before fixation of the tubercle, medialisation is checked with a ruler in order to correct the misalignment and to bring it to a normal value for the TT-TG. For example, if the TT-TG pre-op is 2 cm, the medialisation will be 1 cm maximum.
After checking the normal position of the tibial tubercle by an awl inserted temporarily along its lateral border, a hole is drilled in the tibial tubercle up to the opposite tibial cortex with a 3.2-mm drill and the tubercle is attached with a cortical 4.5-mm screw. The procedure is completed with a plasty of the medial retinaculum and a suture of the lateral periosteum to the tibial tubercle (Fig. 2).
Fig. 2.
a Medial transfer before screw. b After fixation by screw
Distal or proximal transfer
Through an anteromedial approach, the patellar tendon is dissected, the lateral retinaculum released, followed by sectioning of medial retinacular tissue, allowing an arthrotomy for arthrolysis in cases of stiffness in patella infera. The tibial tubercle is completely detached on three sides as for medial transfer with a chisel and with an oscillating saw for the distal part.
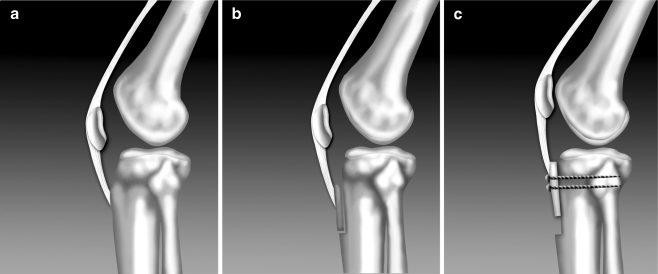
In patella alta we remove a piece of bone from the distal edge of the tibial tubercle in order to correct the Caton–Deschamps index to 1 as planned preoperatively (Fig. 3).
Fig. 3.
Full tibial tubercle osteotomy
Then the proximal portion of the tibial tubercle is pried off, grasped with a bone-holding forceps and fixed distally using a 4.5-mm screw after 3.2-mm drilling. Before complete fixation of the distal screw it is necessary to do a medial transfer of the tibial tuberosity to correct the TT-GT, after which the screw can be tightened. A second 4.5-mm screw is inserted 1.5 cm proximally after 3.2-mm drilling. The medial retinacular tissue and the lateral periosteum on the tubercle are closed as described above (Fig. 4).
Fig. 4.
Patella alta before and after lowering of the patellar
Finally, knee flexion is tested to ensure that the distal portion of the bone block fits the tibial anatomy and that the amount of medial transfer is correct.
The proximal transfer for patella infera correction follows the same procedure after articular release if the patellar tendon is equal or superior to 2.5 cm in order to avoid a too proximal transfer of the tibial tuberosity (Fig. 5).
Fig. 5.
Proximal transfer of the tibial tubercle for patella infera. a Before operation. b After tibial tubercle osteotomy. c Proximal transfer of the patella with two screws
Postoperative care is common to all tibial tubercle osteotomies
A drain is inserted before suture in medial proximal or distal transfers and removed at 48 hours after surgery. Postoperative immobilisation with a splint at 30° flexion is maintained for three weeks. Walking without weight bearing is recommended for three weeks. Rehabilitation begins immediately after operation in order to preserve knee mobility, a good tension in the patellar tendon and avoid excessive stress on the fixation of the tibial tubercle. Flexion is limited during this three-week period to 100°.
After splint removal full flexion is progressively allowed and closed kinetic exercises between 0 and 60° permit muscle strengthening. Sports activities are permitted at six months.
Results
Patella alta and patello femoral instability
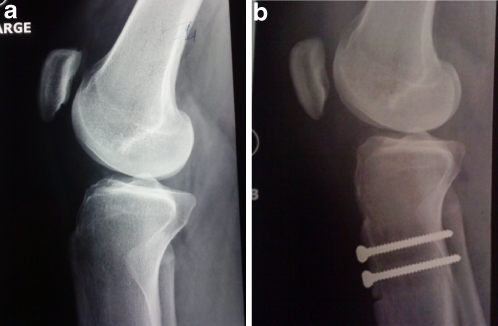
Sixty-one knees in 50 patients were operated upon and reviewed by the first author, 50% had an isolated medial transfer and 50% a medial transfer and with advancement of the tibial tuberosity. In eight cases the lowering was performed secondarily after failure of an isolated medial transfer to correct a patella alta. The mean age at the time of the surgery was 17 years, after closure of the growth cartilage. The mean preoperative Caton–Deschamps index was 1.34, the mean medial translation was 9.5 mm and the mean distal translation was 7 mm, thus allowing a correction of the Caton–Deschamps patellar index. A perfect postoperative stability was found in 76.8% of patients (Fig. 6a,b).
Fig. 6.
a Femoro-patellar dysplasia with patella alta before operation (Caton–Deschamps index AT/AP=1.4) b After lowering of patella (AT/AP = 1)
Patella infera
Our experience includes a study of 24 patients using the procedure described above. The postoperative results were assessed at a minimum of two years follow-up by the first author for pain, mobility, stability and resistance to fatigue with 83% of excellent and good results (Fig. 7).
Fig. 7.
Patella infera good result after proximal transfer (Caton–Deschamps index AT/AP=1)
Discussion
Patella alta is rarely an isolated finding and it is most often a symptom of a regional patello-femoral dysplasia with four major instability factors, i.e. trochlear dysplasy, patella alta, excessive TT-TG, and patellar tilt [11]. Others factors such as external femoral or tibial rotation, genu recurvatum or genu valgum are factors do not influence the surgical decision or treatment. These factors define the misalignment. H. Dejour established a classification of these disorders with three patterns:
Objective patellar instability with true dislocation of the patella with or without patella alta and trochlear dysplasia
Potential patellar instability without patellar dislocation but with at least one anatomical abnormality
Painful patella syndrome: patients with neither dislocation of the patella nor anatomical abnormalities
Surgery is only required for objective or potential patellar instability. The surgeon will always need to combine soft tissue and bony procedures such as tibial tubercle osteotomies.
The treatment of patella infera provides satisfactory results if the aetiology is mechanical and mostly of tibial tuberosity in origin with a patellar tendon equal or longer than 2.5 cm.
For inflammatory patella infera of quadricipital origin [16] the patellar tendon length generally is shorter than 2.5 cm and must be managed by patellar tendon lengthening as described by D. and H. Dejour in 1995 [9]. Treatment of patella infera is determined after the preoperative planning described above.
Surgery when the Caton–Deschamp’s index is over 0.6 (between 0.6 and 0.8) gives unsatisfactory results.
Contraindications for surgical treatment of patella infera are mainly depressive and neurotic subjects.
Patella infera treatment of quadricipital origin is difficult, especially in the reflex sympathetic dystrophy syndrome [16].
Conclusion
At the completion of this study it appears that patella alta is rarely an isolated finding and is most often part of a regional patello-femoral dysplasia. The existence of excessive TT-TG, patella alta or patella infera when responsible for a functional problem must be considered and treated after precise preoperative planning by medial, distal or proximal transfer of the tibial tuberosity, often combined with a soft tissue procedure in order to obtain a satisfactory result.
References
- 1.Bernageau J, Goutallier D (1984) Examen radiologique de l’articulation fémoro-patellaire. In: L’actualité rhumatologique, de Seze et Coll. Expansion Scientifique Française, Paris, pp 105–110
- 2.Blackburne JS, Peel TE. A new method of measuring patella height. J Bone Jt Surg (Br) 1977;59:241–242. doi: 10.1302/0301-620X.59B2.873986. [DOI] [PubMed] [Google Scholar]
- 3.Blumensaat C. Die Lageabweichungen und Vezzenkungen der Kniescheibe. Ergeb Chir Orthop. 1938;31:149–229. [Google Scholar]
- 4.Caton J, Deschamp G, Chambat P, Lerat JL, Dejour H. Les rotules basses (Patellae inferae) – A propos de 128 observations. Rev Chir Orthop. 1982;68:317–325. [PubMed] [Google Scholar]
- 5.Caton J. Méthode de mesure de la hauteur de la rotule. Acta Orthop Belg. 1989;55:385–386. [PubMed] [Google Scholar]
- 6.Caton J, Mironneau A, Walch G, Levigne C, Michel CR. La rotule haute idopathique chez l’adolescent. A propos de 61 cas opérés. Rev Chir Orthop. 1990;76:253–260. [PubMed] [Google Scholar]
- 7.Cox JS. An evaluation of the Elmslie Trillat procedure for management of patellar dislocation and subluxation. A preliminary report. Am J Sports Med. 1976;4:72–77. doi: 10.1177/036354657600400204. [DOI] [PubMed] [Google Scholar]
- 8.Carvalho A, Andersen AH, Topp S, Jurik AG. A method for assessing the height of the patella. Int Orthop. 1985;9:195–197. doi: 10.1007/BF00268170. [DOI] [PubMed] [Google Scholar]
- 9.Dejour D, Levigne CH, Dejour H. La rotule basse post-opératoire. Traitement par allongement du tendon rotulien. Rev Chir Orthop. 1995;81:286–295. [PubMed] [Google Scholar]
- 10.Dejour H, Walch G, Neyret P, Adeleine P. La dysplasie de la trochlée fémorale. Rev Chir Orthop. 1990;76:45–54. [PubMed] [Google Scholar]
- 11.Dejour H, Walch G, Nove Josserand L, Guier CH. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 12.Goutallier D, Bernageau J, Lecudonnec B. Mesure de l’écart tubérosité tibiale antérieure-gorge de la trochlée (TA.GT). Technique Résultats Intérêts. Rev Chir Orthop. 1978;64:423–428. [PubMed] [Google Scholar]
- 13.Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101–104. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 14.Leung YF, Wai YL, Leung YC. Patella alta in southern China. A new method of measurement. Int Orthop. 1996;20:305–310. doi: 10.1007/s002640050083. [DOI] [PubMed] [Google Scholar]
- 15.Linclau L. Measuring patellar height. Act Orthop Belg. 1984;50:70. [PubMed] [Google Scholar]
- 16.Noyes FR, Wostys E, Marshall MT. The early diagnosis and treatment of developmental patella infera syndrome. Clin Orthop. 1991;265:241–252. [PubMed] [Google Scholar]
- 17.Pors WRR, Fulkerson JP. Distal realignment of the patella femoral joint. Indications, effects, results and recommendations. Orthop Clin North Am. 1992;23:631–643. [PubMed] [Google Scholar]
- 18.Shabshin N, Schneitzer ME, Morrison WB, Parker L. MRI Criteria for patella alta and Baja. Skelet Radio. 2004;33:445–450. doi: 10.1007/s00256-004-0794-6. [DOI] [PubMed] [Google Scholar]
- 19.Trillat A, Dejour H, Couette A. Diagnostic et traitement des subluxations récidivantes de la rotule. Rev Chir Orthop. 1964;50:813–824. [PubMed] [Google Scholar]