Abstract
Extremely severe Pott’s kyphotic deformity cannot be completely corrected by conventional techniques, including vertebral body resection, Smith-Peterson, pedicle subtraction osteotomy or even vertebral column resection (VCR). The authors developed a new technique combining transpedicular eggshell osteotomies and VCR as multilevel modified vertebral column resection (MVCR) through a single posterior approach for surgical treatment of Pott’s kyphosis with Konstam’s angle beyond 90°. A total of 9 patients (6 males, 3 females) in our institution with severe Pott’s kyphosis who underwent single-stage posterior-only multilevel MVCR were retrospectively reviewed. The candidates for multilevel MVCR were those with a sharp, angular kyphosis in the lower thoracic or upper lumbar spine with a Konstam’s angle beyond 90°. The follow-up averaged 30.6 months (ranging from 21 to 50 months). Fusion status was evaluated at each follow-up by CT three-dimensional reconstruction images. An average of 2.5 vertebrae was removed in each case (ranging from 2 to 4 vertebrae). A mean of 7 vertebrae were fused (ranging from 6 to 11 vertebrae). The mean duration of surgery was 285 min (ranging from 246 to 400 min), the average intraoperative blood loss was 2,933 ml (ranging from 2,000 to 6,000 ml). The mean preoperative kyphus was 100.3° (ranging from 90° to 132°). The mean kyphosis in the immediate postoperative period was 15.9° (ranging from 4° to 30°) with an average postoperative kyphos correction of 84.4° (ranging from 63° to 126°). Fusion of the resection site was confirmed on radiographs in all patients at the minimum 12 months follow-up. No pseudoarthrosis was found. No loosening or breakage of pedicle screws occurred. A single-stage posterior-only multilevel MVCR is an effective way to correct extremely severe Pott’s kyphosis with Konstam’s angle beyond 90°.
Keywords: Pott’s kyphosis, Multilevel, Vertebral column resection, Osteotomy
Introduction
Worldwide, tuberculosis (TB) has experienced a marked resurgence on the past two decades. Approximately 30 million patients annually suffer from TB and 8 million new cases are added every year [19]. Within the musculoskeletal system TB mostly involves (nearly 50%) the spinal column primarily in the upper lumbar and lower thoracic spine [10]. The bony destruction and vertebral collapse often results in significant kyphosis, presenting clinically as a painful gibbus, creased instability, vertebral body translations and increased risk of neurologic involvement [4, 17]. An extremely severe kyphosis, however, with the sagittal Konstam’s angle beyond 90°, not only disfigures the body, but also carries psychological implications, difficulties with employment. Patients so affected may develop late-onset paraplegia, cardiopulmonary dysfunction or painful costo-pelvic impingement [9–12, 17].
Various techniques have been used to describe to correct the kyphotic deformity associated with advanced Pott’s disease. The traditional two-stage technique allows a thorough decompression but requires two operations and its increased morbidity [6]. A single-stage posterior Smith-Peterson osteotomy or PSO may not be suitable to correct extremely severe kyphotic deformity with a Konstam’s angle exceeding 90°. Vertebral column resection (VCR) through a single-stage anterior–posterior approach is associated with significant blood loss and morbidity with major complications [3].
To overcome the disadvantages of the techniques mentioned above, a modified multilevel vertebral column resection (MVCR) through a single posterior approach was developed. The present study aimed to report the technique and results of posterior-only MVCR for correction of severe Pott’s kyphosis with the Konstam’s angle above 90°, and evaluate the efficacy and safety of this technique.
Materials and methods
Fifteen patients diagnosed with Pott’s kyphosis and sagittal Konstam’s angles beyond 90° were admitted to our department from August 2004 to October 2006, nine of whom provided informed consent to undergo a single-stage posterior-only MVCR. There were 6 males and 3 females, with a mean age of 26.2 years old (ranging from 16 to 46 years old) and an average sharp, angular kyphosis of 100.3° (ranging from 91 to 135 ) with Konstam’s method [9]. The mean number of vertebral bodies resected was 2.6 (ranging from 2 to 4). The main complains of these patients were cosmetic problem, fatigue or low back pain, and being not able to lie down in dorsal position. One patient suffered digestive system dysfunction and painful costo-pelvic impingement. One patient was Grade C neurologic deficit according to ASIA grade system. The surgical plan, including the resection site and degree of correction, was determined based on clinical radiographs, CT scans, 3-D reconstruction images and MRI.
All patients were evaluated before and immediately after surgery, the 3rd, 6th, 12th month postoperatively, and then once a year. The Konstam’s angle was measured on lateral radiographs in standard standing position. The external appearance was noted. CT 3-D reconstruction was used to assess fusion status.
Operative technique
All surgeries were performed by the senior author with somatosensory-evoked potential monitoring. The patients were placed in the prone position on the operating table under general anesthesia. A posterior midline incision was made over the kyphotic spinous processes. Pedicle screws were inserted into several segments above and below (typically three pairs, respectively) the vertebral levels to be resected. C-arm fluoroscopy was used to confirm the appropriate insertions.
The screws were connected through a temporary rod on one side. The pedicle of the vertebral body to be removed was probed. A high-speed drill was used to enlarge the hole cephalically and caudally by until the corresponding walls was penetrated. Care should be taken during this process to keep the medial wall of the pedicle as intact as possible for the protection of the nerve roots. After the exposure of the end-plates of the upper and lower intervertebral space, a Kerrison rongeur or drill was used to thin the anterior and lateral walls of the vertebral body, which were then collapsed under pressure laterally to expose the posterior walls further. A similar vertebral body resection was subsequently advanced to cross the midline in an abrasive way with the drill. The upper and lower cartilaginous end-plates of the resected vertebra and intervertebral discs were removed with a curette.
After the vertebral bodies are resected, the posterior elements, including the spinous processes, laminae, facet joints and transverse processes are removed. A dome decompression is then performed by obliquely resecting the underlying part of residual proximal and distal laminar edges to enlarge the vertebral canal as to avoid injuring the spinal cord when closing the resection gap. Stabilized by a temporary rod, the kyphotic spine is then corrected through gradual segmental compression. After the confirmation of correction on fluoroscopy, the final internal fixation is applied. The residual autogenous bone can then be placed for posterior lateral fusion.
Result
An average of 2.5 vertebrae was removed in each case (ranging from 2 to 4 vertebrae). A mean of 6.4 vertebral levels were instrumented and fused (ranging from 6 to 11 vertebrae). The mean duration of surgery was 285 min (ranging from 246 to 400 min), the average intraoperative blood loss was 2,933 ml (ranging from 2,000 to 6,000 ml). The mean preoperative kyphosis was 97.2° (ranging from 90° to 135°). The mean kyphosis in the immediate postoperative period was 17.2° (ranging from 4° to 30°) with a mean correction of 80° (ranging from 43° to 129°) (Table 1) (P = 0.001). The mean correction loss at a minimum 20 months follow-up was 1.6° (ranging from 0° to 5°). Fusion of the resection site was confirmed on radiographs in all patients at a minimum 12 months follow-up.
Table 1.
The result of correction
| Patient | Gender | Age (years) | Resection segment level | Instrumented vertebrae | Pre-operative Konstam’s angle (°) | Post-operative Konstam’s angle (°) | Complication |
|---|---|---|---|---|---|---|---|
| 1 | Male | 28 | T11, 12 | T7-10, L1-3 | 95 | 30 | |
| 2 | Female | 26 | T12, L1 | T9-11, L2-4 | 100 | 25 | |
| 3 | Female | 26 | T11, 12, L1 | T8-10, L2-4 | 93 | 4 | |
| 4 | Male | 46 | T9, 10 | T6-8, T11-L1 | 90 | 27 | Incomplete paraplegia (ASIA B) |
| 5 | Male | 16 | T11, 12, L1 | T8-10, L2-4 | 91 | 11 | |
| 6 | Male | 19 | T11 T12, L1, L2 |
T6-11, L3-5 | 135 | 6 | |
| 7 | Female | 24 | T11, 12 | T7-10, L1-3 | 97 | 16 | |
| 8 | Male | 19 | T11, 12, L1 | T8-10, L2-4 | 110 | 10 | |
| 9 | Male | 32 | T12, L1 | T9-11, L2-4 | 95 | 14 | |
| Average | 26.2 | 100.3 | 15.9 |
The mean duration of hospital stay after surgery was 15 days (ranging from 11 to 43 days). Sitting with a custom-made plastic thoracolumbosacral orthosis (TLSO) and walking were permitted soon after the removal of drainage in neurally intact patients. Sitting or walking in neurologic deficit patients was dependent on the state of neural recovery. The TLSO was preserved for 3 months and 6 months for two-segment resection patients and three-segment or more MVCR patients, respectively. There was no superficial or deep infection. No pseudoarthrosis was found. No loosening or breakage of pedicle screws occurred.
The preoperative main complain, such as cosmetic problem, fatigue or low back pain, digestive system dysfunction and painful costo-pelvic impingement, were improved obviously and all patients can lie down in dorsal position. One of the principle concerns of aggressive correction of kyphosis by a posterior-only approach is neurologic complications. In this study, a neurological deficit occurred in 1 patient. He complained of numb and weak of both lower extremities for 2 years on admission. Neurological examination revealed slight hypesthesia below T9, grade IV muscle power of both lower extremities, hyperreflexia of bilateral patella tendon and achilles tendon, and positive ankle clonus and Babinski’s sign. The apical vertebrae were situated at T9 and T10, which were removed intraoperatively. He suffered incomplete paraplegia (ASIA B) below T9 soon after the operation. After 8 month continuous rehabilitation exercises, he recovered to ASIA D when followed up. There was neither identifiable event noted at surgery nor radiographically during the postoperative period to explain the cause of the neurologic deficit.
Discussion
Various techniques have described to treat the severe kyphosis of Pott’s TB [1, 2, 6, 11, 20, 21]. A sequential, multistage procedure has described, including fitting of a halo-pelvic distraction apparatus, anterior spinal osteotomy and decompression of the spinal cord, gradual spinal distraction, posterior osteotomy and fusion, additional spinal distraction, and anterior spine fusion after maximum correction [8]. Despite of the volume of surgery, there was only 28% with this technique and a 10% mortality rate. [12] Recently, a single-stage posterior osteotomy or VCR has become increasingly popular as it provides significant correction while minimizing the risk of injury to anterior vascular and visceral structures. Posterior osteotomy surgeries typically are of either the Smith-Petersen osteotomy (SPO) [13] or the PSO [16]. However, a SPO requires a mobile disc space anteriorly, and it is not frequently presented with the rigid deformity of an extremely severe Pott’s kyphosis [4]. A PSO can apply to patients with sharp, angular kyphosis and anterior column fusion [3]. Nevertheless, the excessive shortening of the area variable for the cord can be dangerous with a PSO and authors have recommended limiting the correction to 30–40° [7]. Therefore, neither the SPO nor a PSO would be suitable to correct a severe kyphotic deformity with a Konstam’s angle beyond 90°.
Indication of VCR has emerged as popular means to correct severe, rigid kyphosis with fixed trunk translation [5]. Traditional VCR through a single-stage anterior–posterior approach is a challenging procedure, with a great risk of major complications vascular and neurological injuries. In presence, Suk et al. developed a single posterior vertebral column resection (PVCR) aimed at reducing both operative time as well as complications [15]. PVCR has been offered to produce correction up to 47.5° in the sagittal plane or 53–55% improvement in sagittal imbalance [11, 14]. With this method, the resection of the vertebra was proceeded from lateral to medial, working through the space created by the resection but not proceeding past the midline. Kawahara et al. [8] further modified the procedure by inserting an interbody cage through the posterior approach improving correction further. However, the remaining select situations of PVCR still cannot provide adequate correction.
In these special cases, we have known that this posterior-only multilevel MVCR described by the senior author has been performed satisfactorily in the past, and most cases restored nearly normal sagittal profile [18]. In this study, the spinal sagittal Konstam’s angle was corrected from a preoperative kyphosis 100.3° to a postoperative angle of 15.9° (p = 0.001) and with a mean correction of 84.1%.
The key steps of MVCR technique are summarized as follows [18]: (1) at the start, the posterior structure, such as spinous processes and lamina were left intact to minimize the blood loss. (2) Once the transpedicular process was completed, a 5-mm burr was used for decancellation through the pedicle. The use of burr was thought to be safer and more effective to control bleeding by the author. (3) When performing ‘eggshell’ technique, the inner wall of the pedicle shall be kept intact to protect the nerve roots from upper and lower segments. (4) Once entering into the vertebra, leave a thin wall of cortical bone at the anterior, lateral, and posterior parts of the vertebra. This was different from PVCR technique, in which the anterior and lateral walls were removed, and only the soft tissue anterior to the vertebral body is left intact. The entry was further enlarged both cephalically and caudally to penetrate the end-plates of the vertebra to expose the upper and lower intervertebral spaces. (5) Adjacent upper and lower end-plates as well as intervertebral discs shall then be removed with a curette. (6) It should be noted that removal of posterior structures shall begin with lateral elements, and posterior structures such as spinal processes and lamina shall all be removed. MVCR technique allows the upper and lower cancellous surfaces of resection gap to contact directly or indirectly by grafting autogenous bone chips and intervertebral compression. This bone-on-bone contact may not only obviate the need for anterior reconstruction by titanium mesh, but also ensure rapid fusion (see Fig. 1).
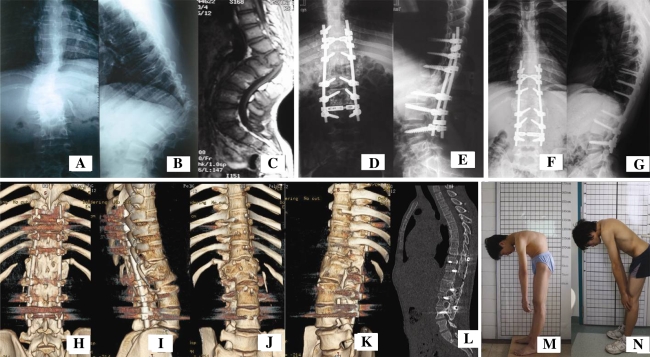
Fig. 1.
A 16-year-old patient had been infected with spinal tuberculosis when he was only 1 year old, the main complains were low back pain and cosmetic problem. a–c Preoperative pictures showed a remarkable kyphosis in thoracolumbar spine, with a Konstam’s angle of 90° on lateral radiographic view and MRI; d, e Multilevel modified vertebral column resection was performed at T12, L1, L2 (L1 was removed totally, and T12, L2 were removed partly for “bone-on-bone”). The kyphosis was corrected to only 11° immediately after the surgery; f, g X-ray 3.5 years postoperatively shows that the correction was maintained. h–l Three-dimensional reconstruction demonstrated that solid fusion of resection site was achieved. m, n Clinical picture shows that the cosmetic disfigurement was improved obviously
It is not necessary to use titanium mesh to bring anterior support, which is based on the recognition of following assumption. Firstly, the cord and nerve roots were elongated and were in stress state (one reason of neurologic symptom) during the progression of deformity, which means it may restore to their normal length after the deformed vertebrae were removed. In addition, displacement of dura may occur during the reduction (to maintain the balance of sagittal plane, the severe sharp kyphosis means proximal thoracic spine was lordosis, see in Fig. 2). Then, the needed shortening of the cord at osteotomy site was diminished. Secondly, one objective of resection of the deformed vertebrae was to realign the anterior column. Therefore, it is not necessary to resect the anterior column totally. In general, we removed one or two deformed vertebrae totally, one vertebrae above and below partly for “bone-on-bone” and for realignment of anterior column. The residual vertebrae take the role of titanium mesh in other methods. Of course, it is necessary to resect the posterior element of all deformed vertebrae totally for avoiding compressing the buckled cord/dura.
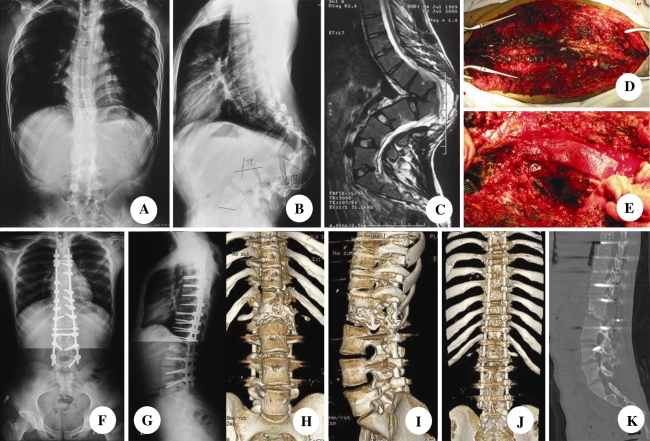
Fig. 2.
A 19-year-old patient had been infected with spinal tuberculosis when he was 4 year old, the preoperative main complains were that cannot lie in dorsal position and low back pain. a–c Preoperative pictures showed a sharp angle in thoracolumbar spine with a Konstam’s angle of 135° on lateral radiographic view and MRI, and lordosis can be found in thoracic spine to maintain the balance of sagittal plane; d, e Intraoperative picture demonstrated vertebral column resection was performed at T11, T12, L1, L2 (L1, T12 was removed totally, and T11, L2 were removed partly); f, g Final follow-up X-ray shows that the correction was maintained; h–k Three-dimensional reconstruction confirmed that solid fusion between L2 and T11 was achieved
In conclusion, our modified MVCR can safely provide excellent clinical and radiographic results for patients who have extremely severe Pott’s kyphotic deformity requiring an aggressive correction. The indications of this procedure may be those severe Pott’s kyphosis at or below lower thoracic spine necessitating more than 70° correction.
Our study is limited somewhat by accomplishing of a relatively small group of patients, for further evaluation of this techniques efficiency and improvement of this technique, a study of a larger group of patients with the set of control group, such as PSO, PVCR, would be necessary. This procedure is technically demanding and should be done by an experienced team of surgeons. The risk of neurological complication should also be seriously considered, which makes it important to select the appropriate surgery candidate.
Reference
- 1.Benli IT, Acarog˘ lu E, Akalin S, et al. Anterior radical debridement and anterior instrumentation in tuberculosis spondylitis. Eur Spine J. 2003;12:224–234. doi: 10.1007/s00586-002-0403-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bradford DS, Tribus CB. Vertebral column resection for the treatment of rigid coronal decompensation. Spine. 1997;22:1590–1599. doi: 10.1097/00007632-199707150-00013. [DOI] [PubMed] [Google Scholar]
- 3.Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine. 2006;31:S171–S178. doi: 10.1097/01.brs.0000231963.72810.38. [DOI] [PubMed] [Google Scholar]
- 4.Jain AK, Aggarwal PK, Arora A, et al. Behavior of the kyphotic angle in spinal tuberculosis. Int Orthop. 2004;28:110–114. doi: 10.1007/s00264-003-0516-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Justin SS, Vincent YW, Christopher PA. Vertebral column resection for rigid spinal deformity. Neurosurgery. 2008;63:A177–A182. doi: 10.1227/01.NEU.0000320429.32113.85. [DOI] [PubMed] [Google Scholar]
- 6.Kalra KP, Dhar SB, Shetty G, et al. Pedicle subtraction osteotomy for rigid post-tuberculous Kyphosis. J Bone Joint Surg Br. 2006;88-B:925–927. doi: 10.1302/0301-620X.88B7.17366. [DOI] [PubMed] [Google Scholar]
- 7.Kawahara N, Tomita K. Influence of acute shortening on the spinal cord: an experimental study. Spine. 2005;30:613–620. doi: 10.1097/01.brs.0000155407.87439.a2. [DOI] [PubMed] [Google Scholar]
- 8.Kawahara N, Tomita K, Baba H, et al. Closing-opening wedge osteotomy to correct angular kyphotic deformity by a single posterior approach. Spine. 2001;26:391–402. doi: 10.1097/00007632-200102150-00016. [DOI] [PubMed] [Google Scholar]
- 9.Konstam PG, Blesovsky A. The ambulant treatment of spinal tuberculosis. Br J Surg. 1962;50:26–38. doi: 10.1002/bjs.18005021908. [DOI] [PubMed] [Google Scholar]
- 10.Nigg AP, Schulze-Koops H, Wirth S, et al. Tuberculous Spondylitis (Pott’s Disease) Infection. 2008;36:293–294. doi: 10.1007/s15010-008-2003-3. [DOI] [PubMed] [Google Scholar]
- 11.Pappou IP, Papadopoulos EC, Swanson AN, et al. Pott disease in the thoracolumbar spine with marked kyphosis and progressive paraplegia necessitating posterior vertebral column resection and anterior reconstruction with a cage. Spine. 2006;31:E123–E127. doi: 10.1097/01.brs.0000199900.56446.ee. [DOI] [PubMed] [Google Scholar]
- 12.Rajasekaran S. The problem of deformity in spinal tuberculosis. Clin Orthop Relat Res. 2002;398:85–92. doi: 10.1097/00003086-200205000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Smith-Peterson MN, Larson CB, Aufranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. J Bone Joint Surg. 1945;27:1–11. [PubMed] [Google Scholar]
- 14.Suk S, Chung ER, Kim JH. Posterior vertebral column resection for severe rigid scoliosis. Spine. 2005;30:1682–1687. doi: 10.1097/01.brs.0000170590.21071.c1. [DOI] [PubMed] [Google Scholar]
- 15.Suk S, Kim JH, Kim WJ. Posterior vertebral column resection for severe spinal deformities. Spine. 2002;27:2374–2382. doi: 10.1097/00007632-200211010-00012. [DOI] [PubMed] [Google Scholar]
- 16.Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res. 1985;194:142–152. [PubMed] [Google Scholar]
- 17.Tuli SM. Severe kyphotic deformity in tuberculosis of the spine: Current concepts. Int Orthop. 1995;19:327–331. doi: 10.1007/BF00181121. [DOI] [PubMed] [Google Scholar]
- 18.Wang Y, Zhang Y, Zhang X, et al. A single posterior approach for multilevel modified vertebral column resection in adults with severe rigid congenital kyphoscoliosis: a retrospective study of 13 cases. Eur Spine J. 2008;17:361–372. doi: 10.1007/s00586-007-0566-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.HO W. World tuberculosis toll on the rise. Asian Med News. 1991;3:9. [Google Scholar]
- 20.Yau ACMC, Hsu LCS, O’Brien JP, et al. Tuberculosis kyphosis-correction with spinal osteotomy, halo-pelvic distraction and anterior and posterior fusion. J Bone Joint Surg. 1974;56A:1419–1434. [PubMed] [Google Scholar]
- 21.Zdemir HM, Kemal AU, Öğün T (2003) The role of anterior spinal instrumentation and allograft fibula for the treatment of pott disease. Spine 28:474–479. doi:10.1097/00007632-200303010-00012 [DOI] [PubMed]