Abstract
Neurogenic intermittent claudication, caused by lumbar spinal stenosis (LSS), usually occurs after the age of 50 and is one of the most common degenerative spinal diseases in the elderly. Among patients over the age of 65 with LSS, open decompression is the most frequently performed spinal operation. The recently introduced interspinous spacers are a new alternative under discussion. In this retrospective study, we reviewed medical records and radiographs of patients with LSS and NIC treated from June 2003 to June 2007. All included patients (n = 129) were treated with interspinous implants (X Stop® Wallis®, or Diam®). Evaluations of pain, using a visual analog scale (VAS), and radiographic signs, using two-plane X-rays of the lumbar spine, were performed preoperatively (preop), postoperatively (postop) and after discharge (FU 2–3). Gender ratio (m:w) was 1.1:1. Mean age of the patients was 60.8 ± 16.3 years. Foraminal height, foraminal width, foraminal cross-sectional area, intervertebral angle, as well as anterior and posterior disc height changed significantly (P < 0.0001) after implantation of the interspinous device. Postoperatively, symptom relief (VAS) was significant (P < 0.0001). The X Stop implant improved (in some cases significantly) the radiographic parameters of foraminal height, width, and cross-sectional area, more than the Diam and Wallis implants; however, there was no significant difference among the three regarding symptom relief. FU 1 was on average 202.3 ± 231.9 and FU 2 527.2 ± 377.0 days postoperatively. During FU, the radiological improvements seemed to revert toward initial values. Pain (VAS) did not increase despite this “loss of correction.” There was no correlation between age and symptom improvement. There was only very weak correlation between the magnitude of radiographic improvement and the extent of pain relief (VAS). The interspinous implant did not worsen low-grade spondylolisthesis. Provided there is a strict indication and fusion is not required, implantation of an interspinous spacer is a good alternative to treat LSS. The interspinous implant offers significant, longlasting symptom control, even if initially significant radiological changes seem to revert toward the initial values (“loss of correction”).
Keywords: Interspinous spacer, Interspinous process device, Interspinous process decompression, Lumbar spinal stenosis, Neurogenic intermittent claudication
Introduction
Neurogenic intermittent claudication (NIC), caused by lumbar spinal stenosis (LSS), usually occurs after the age of 50 [29] and is one of the most common degenerative spinal diseases in the elderly [20, 39].
Therapy options run the gamut from conservative management with non-steroidal antiinflammatory drugs, braces for instability, physical therapy, and epidural injections, to surgery. Operative therapy has shown significantly better results than conservative management [1, 9, 26, 41]. Open decompression is the most frequent spinal operation for patients over 65 years with LSS [8, 19, 21].
The more recently applied interspinous spacers are an alternative under discussion. These devices are used either as “stand alone” implants or to augment open decompression by preventing instability [4, 33]. The main principle for these implants is to limit the dynamic extension of the concerned segment. Early clinical trials are promising [2, 35, 43], and long-term studies are still pending.
It is well known in cases of back pain that even with modern techniques (MRI, CT), there is often no correlation between radiologic and clinical signs. Pain-free patients can show considerable degenerative changes radiographically [1, 3, 28, 35], and correspondingly, the radiologic extent of LSS shows no correlation with the magnitude of symptoms [36]. Radiologic studies have demonstrated that the use of interspinous devices affects changes of spinal alignment as well as the dimensions of the spinal canal and neural foramina [22, 30, 34]. To our knowledge, no study has confirmed the correlation between plain X-ray changes post-implantation of various interspinous spacer devices and clinical outcome. The purpose of this study was to examine the relationship between radiographic changes of the concerned vertebral segments prior to and after implantation of three different interspinous spacer devices (X Stop, Diam, and Wallis) and clinical outcome (VAS).
Methods
In this retrospective study, we reviewed the medical records and radiographs of LSS patients with NIC treated from June 2003 to June 2007. All included patients (n = 129) felt relief in flexion and were treated with one of the following interspinous implants:
X Stop® (Medtronic, Tolochenaz, Switzerland)
The X Stop implant is an all-titanium (PEEK-surrounded since end of 2004) oval spacer with two lateral wings to prevent lateral migration. It is inserted as two components.
Wallis® (Abbott Spine, Bordeaux, France)
The Wallis implant is a floating system, consisting of a PEEK (Polyetheretherketone) block. It is augmented by two woven Dacron ribbons, which are wrapped around the spinous processes and fixed under tension.
Diam® (Medtronic, Tolochenaz, Switzerland)
The Diam implant is a silicon core covered by a polyester sleeve. It is held in position by three mesh bands, two around each spinous process and one around the supraspinous ligament.
All implantations were performed by the same experienced surgeon (PS). Evaluations of pain, using a visual analog scale (VAS), and radiographic signs, using two-plane X-rays of the lumbar spine, were performed preoperatively (preop), postoperatively (postop) and after discharge (FU 2–3).
The measuring program DicomWorks (digital Imaging and Communications in Medicine) v 1.3.5© 2000 (Philippe Puech & Loic Boussel, Lyon, France) was used to quantify radiologic parameters. Radiographic measurements were carried out by two independent experienced physicians. The radiologic parameters were determined as follows:
Foraminal height (FH) (cm)
Maximum distance between the inferior margin of the pedicle of the superior vertebra and the superior margin of the pedicle of the inferior vertebra.
Foraminal width (FW) (cm)
The anterior–posterior width of the foramen measured in the horizontal plane as extension of the tangent of the inferior endplate.
Foraminal cross-sectional area (FA) (cm2)
The margins of the foramen were marked with the cursor, and the program DicomWorks measured the cross-sectional area of the foramen.
Anterior disc height (aDH) and posterior disc height (pDH) (cm)
The anterior and posterior disc heights were measured in the planes of the anterior and posterior surfaces of the adjacent vertebral bodies. Therefore, the distance between the intersections of the vertical line of the tangent of the superior endplate and the tangent of the inferior endplate was measured. The vertical line started at the superior-anterior, respectively superior-posterior edge of the lower vertebra.
Intervertebral angle (IA) (°)
The angle between the tangent of the superior endplate and that of the inferior endplate of the vertebral segment was measured. A kyphotic angle was measured as a negative (“−”) value and a lordotic angle as positive (“+”).
Listhesis
The grade of listhesis was measured according to Meyerding. The antelisthesis was marked with “+” and the retrolisthesis with “−”.
Diameter of the superior endplate (D) (cm)
Diameter of the superior endplate of the inferior vertebral body of the deformed segment.
Multiplication factor for standardization of measured values
For correction of differences in magnification of radiographs, the postoperative measurements of FH, FW, FA, aDH and pDH were multiplied by the quotient of the diameters of the respective superior endplates (e.g. D preop/D postop, D preop/D FU 2).
Statistics
Owing to the observational nature of this study, all outcome variables were analyzed in a purely explorative manner, and thus no formal adjustment of P values for multiple comparisons was carried out. Explorative comparisons were performed between described groups—respecting the actual scale levels as well as distributional characteristics—using appropriate parametric and non-parametric test statistics [e.g. t test, ANOVA, rank statistics (Wilcoxon–Mann–Whitney) and contingency table analysis] as well as measures of stochastic association (e.g. correlation analyses). Depiction of observed effects was given by histograms, box plots and scatter grams. Dimensional demographic variables (e.g. age) and diseases were summarized by mean, median, standard deviation (SD), standard error (SE), quartiles, minimum, and maximum if appropriate. Qualitative demographic variables (e.g. gender) and disease characteristics as well as potential prognostic categories were summarized by counts and percentages. Differences were considered to be significant at a probability level of 95% (P < 0.05). Statistical evaluation was done with SPSS 16.0.
Results
General
Gender ratio (m:w) was 1.1:1. Mean age of the patients was 60.8 ± 16.3 years (median 64, range 18–91). Forty-eight percent of the patients were ≥65 years, 51.2% <65 years, 24.8% <50 years, and 12.4% <40 years. There was no statistical difference in age by gender.
The frequency distribution of concerned vertebrae showed 72.9% for the segment L4/5, 15.5% for L3/4, 5.4% for both L2/3 and L5/S1, and 0.8% for L1/2.
The X Stop was implanted in 78 (60.5%) patients, the Diam in 33 (25.6%), and the Wallis in 18 (14.0%). If an X Stop was applied, the most frequently used size was 14 mm, in 66.2% of the cases, followed by 12 mm in 19.5%, 16 mm in 13.0%, and 10 mm in 1.3%.
At follow-up (FU), all patients were examined radiologically and clinically. The first postoperative examination (postop) was at 4 ± 21.7 days (median 1.0, range 1–29) after the operation and included all patients (100%). Mean FU 1 was 202.3 ± 231.9 days (median 97.0, range 6–878) post surgery, which 35.7% of patients attended. A third postoperative examination (FU 2) with only 8.5% of the patients represented, took place on average 527.2 ± 377.0 days (median 423.0, range 240–1,494) postoperatively.
Spacer without differentiation (total sample)
Foraminal height (FH)
Foraminal height postoperatively increased significantly (P < 0.0001) compared with preoperatively, but decreased in the FU period (see Fig. 3). At FU 1, the mean percentile increase compared with preoperative measurements was 9.2 ± 9.5% (see Table 1). At FU 2, it was 5.6 ± 7.0%. The increased FH remained statistically significant (P < 0.05) over the entire FU period. The decrease between postop and FU 1, although not between FUs 1 and 2, was also significant (P < 0.001).
Fig. 3.
Relative radiographic changes, preoperative versus postoperative (*significance between X Stop and the other implants P < 0.05)
Table 1.
Mean radiological and clinical (VAS) changes between preop, postop and FU 1 with standard deviation (SD) and range (min–max)
| X Stop | Diam | Wallis | All | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min | Max | Mean | SD | Min | Max | Mean | SD | Min | Max | Mean | SD | Min | Max | |
| FH | ||||||||||||||||
| pre (cm) | 1.93 | 0.30 | 1.10 | 2.67 | 1.90 | 0.32 | 1.23 | 2.61 | 2.01 | 0.25 | 1.32 | 2.41 | 1.93 | 0.30 | 1.10 | 2.67 |
| pre–post | ||||||||||||||||
| (cm) | 0.33a | 0.17 | −0.04 | 0.71 | 0.25 | 0.18 | −0.07 | 0.66 | 0.22 | 0.14 | 0.02 | 0.50 | 0.29 | 0.20 | −0.07 | 0.71 |
| (%) | 17.5 | 10.5 | −1.8 | 46.7 | 13.7 | 9.8 | −2.7 | 34.9 | 10.8 | 6.1 | 1.1 | 21.6 | 15.6 | 10.1 | −2.7 | 46.7 |
| post-FU 1 (%) | −5.6 | 6.9 | −23.3 | 11.7 | −9.3 | 4.7 | −16.3 | −3.8 | −6.7 | 4.5 | −13.0 | −1.6 | −6.3 | 6.3 | −23.3 | 11.7 |
| FW | ||||||||||||||||
| pre (cm) | 0.92 | 0.34 | 0.24 | 1.90 | 0.67 | 0.27 | 0.25 | 1.27 | 0.82 | 0.29 | 0.32 | 1.41 | 0.84 | 0.33 | 0.24 | 1.90 |
| pre–post | ||||||||||||||||
| (cm) | 0.19 | 0.18 | −0.21 | 0.68 | 0.27 | 0.21 | 0.00 | 0.69 | 0.17 | 0.21 | −0.13 | 0.56 | 0.21 | 0.20 | −0.21 | 0.69 |
| (%) | 28.3 | 36.8 | −32.8 | 182.9 | 52.0 | 50.4 | 0.0 | 180.0 | 24.2 | 31.5 | −21.0 | 83.3 | 34.1 | 41.4 | −32.8 | 182.9 |
| post-FU 1 (%) | −10.4 | 12.5 | −48.8 | 16.7 | −8.8 | 13.5 | −30.2 | 3.7 | −1.1 | 16.8 | −23.8 | 28.6 | −8.2 | 13.8 | −48.8 | 28.6 |
| FA | ||||||||||||||||
| pre (cm2) | 1.57 | 0.45 | 0.68 | 2.79 | 1.40 | 0.51 | 0.54 | 2.77 | 1.62 | 0.38 | 1.05 | 2.41 | 1.53 | 0.46 | 0.54 | 2.79 |
| pre–post | ||||||||||||||||
| (cm2) | 0.51b | 0.26 | −0.02 | 1.20 | 0.43 | 0.29 | 0.03 | 1.07 | 0.33 | 0.33 | −0.17 | 0.93 | 0.46 | 0.28 | −0.17 | 1.20 |
| (%) | 35.5 | 21.0 | −1.1 | 104.4 | 36.2 | 29.1 | 1.1 | 109.3 | 20.7 | 20.4 | −9.1 | 62.0 | 33.6 | 23.8 | −9.1 | 182.9 |
| post-FU 1 (%) | −11.4 | 8.5 | −27.0 | 11.2 | −12.1 | 19.4 | −45.1 | 1.6 | −9.2 | 7.7 | −23.1 | 2.0 | −11.0 | 10.0 | −45.1 | 11.2 |
| IA | ||||||||||||||||
| pre (°) | 6.21 | 4.89 | −5.00 | 16.00 | 8.26 | 4.97 | −7.00 | 17.00 | 9.28 | 3.58 | 5.00 | 15.00 | 7.2 | 4.9 | −7.0 | 17.0 |
| pre–post (°) | −5.52c | 3.36 | 1.40 | −12.00 | −3.76 | 4.58 | 11.00 | −12.00 | −4.53 | 2.67 | 0.00 | −11.00 | −4.90 | 3.70 | 11.00 | −12.00 |
| post-FU 1 (°) | 2.3 | 3.3 | 8.0 | −5.9 | 3.1 | 3.0 | 7.0 | 0.0 | 1.9 | 2.8 | 7.0 | −2.0 | 2.3 | 3.1 | 8.0 | −5.9 |
| aDH | ||||||||||||||||
| pre (cm) | 1.07 | 0.40 | 0.33 | 1.94 | 1.38 | 0.32 | 0.53 | 2.21 | 1.32 | 0.30 | 0.89 | 1.86 | 1.18 | 0.40 | 0.33 | 2.21 |
| pre–post | ||||||||||||||||
| (cm) | −0.15 | 0.18 | −0.68 | 0.20 | −0.09 | 0.18 | −0.35 | 0.38 | −0.11 | 0.19 | −0.56 | 0.24 | −0.13 | 0.18 | 0.68 | −0.38 |
| (%) | −12.6 | 16.7 | −52.0 | 32.6 | −4.9 | 18.1 | −31.3 | 71.7 | −8.2 | 12.0 | −30.1 | 16.0 | −10.0 | 16.8 | −52.0 | 71.7 |
| post-FU 1 (%) | 4.7 | 18.1 | −41.6 | 47.6 | 4.4 | 15.6 | −18.1 | 27.3 | 2.1 | 7.5 | −6.9 | 18.9 | 4.1 | 15.8 | −41.6 | 47.6 |
| pDH | ||||||||||||||||
| pre (cm) | 0.59 | 0.22 | 0.00 | 1.17 | 0.77 | 0.18 | 0.34 | 1.21 | 0.65 | 0.23 | 0.11 | 1.01 | 0.64 | 0.22 | 0.00 | 1.21 |
| pre–post | ||||||||||||||||
| (cm) | 0.27 | 0.15 | −0.09 | 0.58 | 0.22 | 0.17 | −0.21 | 0.68 | 0.20 | 0.15 | 0.01 | 0.59 | 0.25 | 0.16 | −0.68 | 0.38 |
| (%) | 52.8 | 39.5 | −7.7 | 216.7 | 33.2 | 36.0 | −23.9 | 200.0 | 40.7 | 39.2 | 1.2 | 163.6 | 46.0 | 39.2 | −23.9 | 216.7 |
| post-FU 1 (%) | −17.9 | 18.8 | −100.0 | 3.1 | −13.1 | 7.5 | −19.1 | −1.7 | −14.8 | 13.6 | −33.3 | 0.0 | −16.6 | 16.6 | −100.0 | 3.1 |
| VAS | ||||||||||||||||
| pre | 67.2 | 26.4 | 0.0 | 100.0 | 59.5 | 23.2 | 0.0 | 100.0 | 57.5 | 31.0 | 0.0 | 100.0 | 63.8 | 26.4 | 0 | 100 |
| pre–post | −26.3 | 36.5 | 50.0 | −100.0 | −34.0 | 34.3 | 40.0 | −92.0 | −14.7 | 34.4 | 55.0 | −100.0 | −26.7 | 35.8 | 55.0 | −100.0 |
| post-FU 1 | −0.5 | 31.6 | 60.0 | −80.0 | −2.6 | 41.9 | 75.0 | −82.0 | 2.6 | 31.2 | 59.0 | −60.0 | −0.6 | 34.6 | 75.0 | −82.0 |
pre preoperative values, pre–post changes between preoperative and postoperative values, post-FU 1 changes between postoperative values and values at follow-up 1
aSignificant difference X Stop versus Diam and Wallis
bSignificant difference X Stop versus Wallis
cSignificant difference X Stop versus Diam
Foraminal width (FW)
Foraminal width postoperatively increased significantly (P < 0.0001) compared with preoperatively, but decreased in the FU period (see Fig. 3). At FU 1, the mean percentile increase compared with preoperative measurements was 17.0 ± 21.8% (see Table 1) and at FU 2 was 8.2 ± 18.7%. The increased FW remained statistically significant (P < 0.001) over the entire FU period. The decrease between postop and FU 1, but not between FUs 1 and 2, was also significant (P < 0.001).
Foraminal cross-sectional area (FA)
Foraminal cross-sectional area postoperatively increased significantly (P < 0.0001) compared with preoperatively, but decreased in the FU period (see Fig. 3). At FU 1, the mean percentile increase compared with preoperative measurements was 19.6 ± 17.5% (see Table 1) and at FU 2 was 5.3 ± 12.1%. The increased FA remained statistically significant (<0.001) over the entire FU period, and the decrease over the FU period was also significant (P < 0.05).
Intervertebral angle (IA)
The use of an interspinous spacer led to a significant (P < 0.0001) decrease in the mean IA, but increased in the FU period (see Table 1). At FU 1, the mean IA measured +4.1° ± 4.5° (median 5.0, range −4.00–12.9), at FU 2 it was +5.2° ± 3.4° (median 4.0, range −1.00–11.0). When compared with the preoperative measurements, the increased IA remained statistically significant (<0.05) over the entire FU period.
Anterior disc height (aDH)
The aDH postoperatively decreased significantly (P < 0.0001) compared with preoperatively (see Fig. 3). At FU 1, the mean percentile decrease in aDH compared with preoperative measurements remained at 10.0 ± 14.2% (see Table 1), and at FU 2 was 8.6 ± 11.0%. The decreased aDH remained statistically significant (P < 0.05) over the entire FU period although the changes within the FU period were not significant.
Posterior disc height (pDH)
The pDH postoperatively increased significantly (P < 0.0001) compared with preoperatively (see Fig. 3). In the FU period, the pDH decreased. At FU 1, the mean percentile increase in pDH compared with the preoperative measurements was 21.7 ± 22.2% (see Table 1) and at FU 2 was 22.0 ± 31.7%. The increased pDH remained statistically significant (P < 0.05) over the FU period, with the decreases between postop and FU 1, and postop and FU 2, also significant (<0.001).
Spondylolisthesis
The differences in spondylolisthesis between preop and postop are depicted in Table 2. The changes over the entire course are shown in Table 2.
Table 2.
Changes of the degree of antelisthesis between preop and postop
| Degree of antelisthesis preoperatively | Degree of antelisthesis postoperatively | ||||
|---|---|---|---|---|---|
| Not done | 0 | 1 | 2 | Total | |
| Not done | 20 | 2 | 0 | 0 | 22 |
| 0 | 0 | 54 | 1 | 0 | 55 |
| 1 | 0 | 2 | 47 | 2 | 51 |
| 2 | 0 | 0 | 0 | 1 | 1 |
| Total | 20 | 58 | 48 | 3 | 129 |
VAS
The VAS postoperatively decreased significantly (P < 0.0001) compared with preoperatively. At FU 1, the patients gave a mean VAS of 34.5 ± 32.5 (median 30.0, range 0.0–100.0) (see Table 1), and at FU 2 reported 33.5 ± 33.2 (median 30.0, range 0.0–100.0). Therefore, improved clinical symptoms (VAS) remained significant (P < 0.0001) for the entire FU. The differences within the FU period were not significant.
For the variable pairs “difference in pain” and “difference in Foraminal cross-sectional area (FA)” we found a significant (P < 0.05), but with a correlation coefficient of r = 0.33 a clinically questionable correlation.
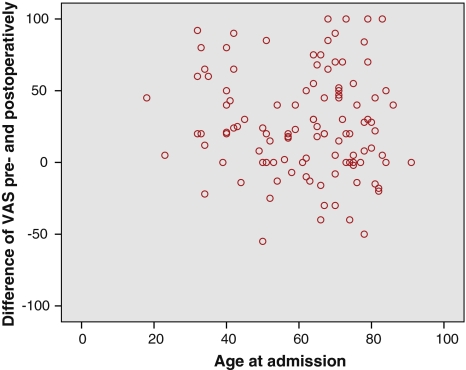
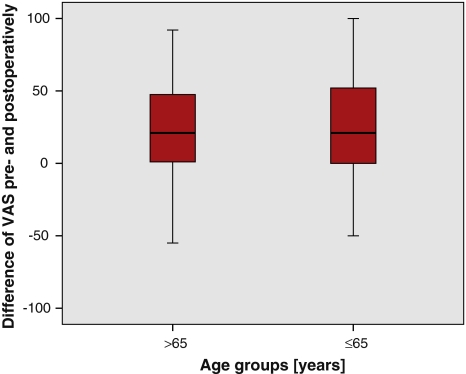
Gender comparison revealed significantly more preoperative pain among females (P = 0.018), and no statistically significant postoperative difference. There was no correlation between age and changes in symptoms (VAS) (see Figs. 1, 2).
Fig. 1.
Scatterplot illustrating the correlation between age and extent of pain relief
Fig. 2.
Boxplot illustrating pain relief between age groups
Differentiation among spacers (X Stop® Wallis®, Diam®)
Comparing the preoperative and postoperative results, we found:
The X Stop group showed a significantly larger change in FH than the other two groups, Diam (P = 0.045) and Wallis (P = 0.034). The difference between Wallis and Diam was not significant (P = 0.613) (see Fig. 3).
The differences in FW among the individual spacer groups were not significant, but the increased FW tended (P = 0.052) to be more with Diam than with X Stop (see Fig. 3).
The difference in FA between X Stop and Wallis was statistically significant (P = 0.022) (see Fig. 3).
The difference in IA between X Stop and Diam was significant (P = 0.022).
There were no significant differences in aDH and pDH among the groups (see Fig. 3).
The postoperative radiological changes relative to preoperative measurements are shown in Fig. 3. Differences among the individual spacers (X Stop, Diam, Wallis) in radiographic and clinical (VAS) improvements were not significant in the FU period up to the time of FU 1 (see Table 1). A statistical evaluation of the particular implants at FU 2 was not useful due to the small numbers of examined patients at that time.
The differences in VAS between the individual spacer groups were not significant, but the improved VAS scores tended (P = 0.083) to be greater with Diam than with Wallis (see Fig. 4).
There was no correlation between the pre- and postoperative radiological changes and the decrease in symptoms (VAS preop–postop) among the individual groups (see Fig. 5).
The different sizes of X Stop led neither to significant percentile changes of the measured radiological parameters, nor to significant differences in symptoms between preop, postop, and the entire FU period.
Fig. 4.
Boxplot illustrating differences in VAS pre- and postoperatively regarding the particular implants
Fig. 5.
Scatterplot illustrating the correlation of differences in VAS and foraminal cross-sectional area (r = 0.33; P < 0.05)
Discussion
Lumbar spinal stenosis is caused by degenerative changes in the spinal canal, e.g. osseous or ligamentous hypertrophy, disc protrusion, and/or degeneration of the disc and instability [23]. Hasegawa et al. and Cinotti et al. identified a significant correlation between disc height and foraminal height [7, 14]. A posterior disc height of 4 mm and foraminal height of 15 mm quite likely lead to nerve compression, although this does not equate to radicular symptomatology [14].
Anatomically, the loss of disc height induces subsidence and subluxation of the articular processes. The superior process of the lower vertebra then slides cephalad and anteriorly, causing the ligamentum flavum to bulge anteriorly, compressing the nerve root [7, 14].
Along with degenerative changes, movement alters spinal canal volumes. Extension of the spine leads to bulging of the ligamentum flavum and the posterior anulus fibrosus into the spinal canal and the lateral recesses. This creates tightness, which may cause NIC [27, 30]. Although extension leads to the reduction in the volumes of the spinal canal, lateral recesses, and foramina [3, 6, 12, 18, 31], flexion causes enlargement by stretching the ligamentum flavum and the posterior longitudinal ligament. In maximal extension, the ligamentum flavum can become 2 mm thicker than in flexion [12, 27, 31]. Anatomical studies have shown that the diameters of both spinal canal and foramina become significantly larger in flexion and significantly smaller in extension [12, 27, 30, 32]. Radiological studies have identified a 16% decrease in the diameter of the spinal canal and a 21–24% decrease in the foraminal cross-sectional area in extension compared with flexion [12, 34].
The normal sagittal diameter of the lumbar spinal canal measures 15–18 mm. A diameter measuring 10–14 mm is deemed “relative stenosis,” and one below 10 mm as “absolute stenosis” [5, 10, 32, 37, 38]. However, the extent of LSS does not appear to correlate with the severity of symptoms [13, 36]. In the literature, parameters for critical foraminal stenosis are mentioned at a posterior disc height of 4 mm or a foraminal height of 15 mm [14]. The mean measures we determined preoperatively (posterior disc height 0.64 ± 0.22 cm; foraminal height 1.93 ± 0.30 cm) are a bit higher.
These anatomic and radiographic findings, as well as the symptomatic improvement with spinal flexion, led to the development of the interspinous implant, which is particularly involved in limiting extension in the affected vertebral segment [11, 24, 33]. To date, the X Stop implant has been best examined in the scientific literature [2, 11, 17, 24, 35, 37, 43]. In a prospectively randomized, controlled multicenter trial, Zucherman et al. examined the clinical results of 191 patients with NIC who were treated either conservatively or operatively with an X Stop. At the 2-year FU, the operated patients had significantly better results [43]. In our study as well, a significant improvement in symptomatic complaints (VAS) was seen postoperatively. Patients noted a significant (P < 0.0001) pain decrease of 26.7 ± 35.8 (VAS 0-100) at postop (Table 1). In subsequent FU (1–2), further discrete improvements of symptoms were evident. The best pain relief was noted for patients who received the Diam (34.0 ± 34.2), followed by the X Stop (26.3 ± 36.5), and the Wallis (14.7 ± 34.4) implants (see Fig. 4), although differences between implants were statistically not significant. A tendency (P = 0.083) was noted for better results using the Diam over the Wallis implants.
In a study of 26 patients with LSS, Siddiqui et al. found on positional MRI that cross-sectional areas of the spinal canal and foramina increased after implantation of an X Stop [34]. Richard et al. used MRI to examine the effects of the X Stop on the dynamic cross-sectional area of the spinal canal and foramina (in 15° flexion and 15° extension) of eight lumbar spines (L3/4). Following the X Stop implantation, the cross-sectional area of the spinal canal increased by 18% and the foramina by 25% in extension. No significant change was observed on adjacent levels [30].
We performed no sectional imaging postoperatively, and hence did not determine spinal canal diameters directly. However, because significant correlations between sagittal diameter of the foramina and spinal canal size [7], and between increased disc height with diminished disc protrusion via ligamentotaxis and thinning of the ligamentum flavum [12, 27, 31] have been previously identified, our measured radiographic changes can be extrapolated to indicate widening of the spinal canal. Thus in our study, all postoperative radiological measurements showed significant changes (see Table 1). In evaluating the individual implants, it was noteworthy that the X Stop implant led to a significantly greater increase in FH than the Diam and Wallis implants.
In a randomized controlled trial, Anderson et al. found that patients with NIC caused by degenerative spondylolisthesis derived significantly better clinical results (ZCQ, SF-36) from the implantation of an X Stop than patients treated conservatively. As well, after 2 years, there was no increased degree of spondylolisthesis (average preoperatively 14.29% and at 2-year FU 14.19%). Only 2° more kyphosis was identified [2]. Over the entire FU of our study, there were no significant changes to the degree of spondylolisthesis (see Tables 2, 3). What was noticeable, however, was a statistically significant (P < 0.0001) postoperative increase in kyphosis of the concerned segment, 4.9° ± 3.7°. In further FU, a decrease was observed, but the differences, compared with preop measurements, remained statistically significant (P < 0.05).
Table 3.
Change of antelisthesis over entire course (%)
| Degree of antelisthesis | preop | postop | FU 1 | FU 2 | ||||
|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | n | (%) | |
| Not done | 22 | 17.1 | 20 | 15.5 | 7 | 15.2 | 2 | 15.4 |
| 0 | 55 | 42.6 | 58 | 45.0 | 19 | 41.3 | 6 | 46.2 |
| 1 | 51 | 39.5 | 48 | 37.2 | 20 | 43.5 | 5 | 38.5 |
| 2 | 1 | 0.8 | 3 | 2.3 | ||||
Finally, a regression of all postoperative radiological changes toward the initial values was observed in the FU 1 and 2 periods (see Table 1). It is not clear, to what this “loss of correction” should be attributed. One explanation, for the Diam and Wallis implant groups, at least, might be attributed to implant breakdown. They are composed of softer materials (silicone, PEEK). The X Stop, on the other hand, is constructed of titanium. Because of its barrel-shaped form and angled edges, however, the implant could intersperse with the surrounding soft tissues and depending on the bone density, even displace or fuse with bone of the spinus processes. In any case, the measured differences among the implants were not significant.
The use of interspinous implants leads to significant improvements in both radiologic parameters and subjective pain complaints. However, the magnitude of symptomatic relief (VAS) does only very weakly correlate (r = 0.33; P < 0,05) with that of radiographic changes (see Fig. 5). Therefore, it appears that neither the initial radiologic grade of LSS [36], nor the postoperative radiographic changes correspond directly to clinical symptoms. One explanation for this would be that the position of the nerve root ganglion, with the largest diameter of the nerve root, varies both among individuals and according to the spinal level [15]. In over 50% of cases, the nerve root ganglion lies in the intraforaminal region [15]. In such cases, there would be less intraforaminal space compared with individuals with the ganglion in an extraforaminal position. As well, the average cross-sectional area of the nerve root varies between 10 and 30% of the average cross-sectional area of the foramen [16]. Another explanation of the dichotomy between radiographic evidence and clinical complaints is that the size of the foramina alters dynamically not only in flexion and extension, but also with axial rotation and lateral bending [12]. Axial load also appears to impact dural sac cross-sectional area on MRI [25, 40, 42]. The X Stop and Wallis implants work predominantly to limit extension and flexion, with only minor checks to axial rotation and no effects on lateral bending [33].
On gender-based comparison, female patients complained of significantly more preoperative pain than males (P = 0.018). Postoperatively, however, there were no gender-related differences. Thus, it appears that females benefited slightly more from the intervention.
There was no correlation between age and postoperative symptom improvements (see Figs. 1, 2).
Keypoints
The implantation of an interspinous spacer leads to significant pain relief (VAS).
The implantation of an interspinous spacer leads to significant changes of foraminal height, width, cross-sectional area, intervertebral angle, and anterior/posterior disc heights.
There is only very weak correlation between the magnitude of radiographic improvement and the extent of pain relief (VAS).
The interspinous implant does not worsen low-grade spondylolisthesis.
During FU, the radiological improvements seem to revert toward initial values (“loss of correction”).
Pain (VAS) does not increase despite this “loss of correction”.
The X Stop implant improves (in some cases significantly) the radiographic parameters of foraminal height, width, and cross-sectional area more than the Diam and Wallis implants; however, there is no significant difference among the three regarding symptom relief.
The size of the X Stop implant has no statistical impact on either the percentile change in radiologic measurements or symptom improvement.
There is no correlation between age and symptom improvement.
Female patients complained of significantly more preoperative pain than males, however there were no significant postoperative differences.
Contributor Information
Rolf Sobottke, Phone: +49-221-4784600, FAX: +49-221-4787045, Email: rolf.sobottke@uk-koeln.de.
Klaus Schlüter-Brust, Email: klaus.schlueter-brust@uk-koeln.de.
Thomas Kaulhausen, Email: thomas.kaulhausen@uk-koeln.de.
Marc Röllinghoff, Email: marc.rollinghoff@uk-koeln.de.
Britta Joswig, Email: Britta.joswig@gmail.com.
Hartmut Stützer, Phone: +49-221-4786501, FAX: +49-221-4786520, Email: hartmut.stuetzer@uk-koeln.de.
Peer Eysel, Email: peer.eysel@medizin.uni-koeln.de.
Patrick Simons, Email: spine-center@mediapark-klinik.de.
Johannes Kuchta, Email: spine-center@mediapark-klinik.de.
References
- 1.Amundsen T, Weber H, Nordal HJ, Magnaes B, Abdelnoor M, Lilleas F. Lumbar spinal stenosis: conservative or surgical management: a prospective 10-year study. Spine. 2000;25:1424–1435. doi: 10.1097/00007632-200006010-00016. [DOI] [PubMed] [Google Scholar]
- 2.Anderson PA, Tribus CB, Kitchel SH. Treatment of neurogenic claudication by interspinous decompression: application of the X Stop device in patients with lumbar degenerative spondylolisthesis. J Neurosurg. 2006;4:463–471. doi: 10.3171/spi.2006.4.6.463. [DOI] [PubMed] [Google Scholar]
- 3.Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects: a prospective investigation. J Bone Joint Surg. 1990;72:403–408. [PubMed] [Google Scholar]
- 4.Bono CM, Vaccaro AR. Interspinous process devices in the lumbar spine. J Spinal Disord Tech. 2007;20:255–261. doi: 10.1097/BSD.0b013e3180331352. [DOI] [PubMed] [Google Scholar]
- 5.Botwin KP, Gruber RD. Lumbar spinal stenosis: anatomy and pathogenesis. Phys Med Rehabil Clin N Am. 2003;14:1–15. doi: 10.1016/s1047-9651(02)00063-3. [DOI] [PubMed] [Google Scholar]
- 6.Chung SS, Lee CS, Kim SH, Chung MW, Ahn JM. Effect of low back posture on the morphology of the spinal canal. Skeletal Radiol. 2000;29:217–223. doi: 10.1007/s002560050596. [DOI] [PubMed] [Google Scholar]
- 7.Cinotti G, Santis P, Nofroni I, Postacchini F. Stenosis of lumbar intervertebral foramen: anatomic study on predisposing factors. Spine. 2002;27:223–229. doi: 10.1097/00007632-200202010-00002. [DOI] [PubMed] [Google Scholar]
- 8.Ciol MA, Deyo RA, Howell E, Kreif S. An assessment of surgery for spinal stenosis: time trends, geographic variations, complications, and reoperations. J Am Geriatr Soc. 1996;44:285–290. doi: 10.1111/j.1532-5415.1996.tb00915.x. [DOI] [PubMed] [Google Scholar]
- 9.Costa F, Sassi M, Cardia A, Ortolina A, Santis A, Luccarell G, Fornari M. Degenerative lumbar spinal stenosis: analysis of results in a series of 374 patients treated with unilateral laminotomy for bilateral microdecompression. J Neurosurg. 2007;7:579–586. doi: 10.3171/SPI-07/12/579. [DOI] [PubMed] [Google Scholar]
- 10.Danielson BI, Willen J, Gaulitz A, Niklason T, Hansson TH. Axial loading of the spine during CT and MR in patients with suspected lumbar spinal stenosis. Acta Radiol. 1998;39:604–611. doi: 10.3109/02841859809175484. [DOI] [PubMed] [Google Scholar]
- 11.Fuchs PD, Lindsey DP, Hsu KY, Zucherman JF, Yerby SA. The use of an interspinous implant in conjunction with a graded facetectomy procedure. Spine. 2005;30:1266–1272. doi: 10.1097/01.brs.0000164152.32734.d2. [DOI] [PubMed] [Google Scholar]
- 12.Fujiwara A, An HS, Lim TH, Haughton VM. Morphologic changes in the lumbar intervertebral foramen due to flexion–extension, lateral bending, and axial rotation: an in vitro anatomic and biomechanical study. Spine. 2001;26:876–882. doi: 10.1097/00007632-200104150-00010. [DOI] [PubMed] [Google Scholar]
- 13.Geisser ME, Haig AJ, Tong HC, Yamakawa KS, Quint DJ, Hoff JT, Miner JA, Phalke VV. Spinal canal size and clinical symptoms among persons diagnosed with lumbar spinal stenosis. Clin J Pain. 2007;23:780–785. doi: 10.1097/AJP.0b013e31815349bf. [DOI] [PubMed] [Google Scholar]
- 14.Hasegawa T, An HS, Haughton VM, Nowicki BH. Lumbar foraminal stenosis: critical heights of the intervertebral discs and foramina: a cryomicrotome study in cadavera. J Bone Joint Surg. 1995;77:32–38. [PubMed] [Google Scholar]
- 15.Hasue M, Kunogi J, Konno S, Kikuchi S. Classification by position of dorsal root ganglia in the lumbosacral region. Spine. 1989;14:1261–1264. doi: 10.1097/00007632-198911000-00021. [DOI] [PubMed] [Google Scholar]
- 16.Hoyland JA, Freemont AJ, Jayson MI. Intervertebral foramen venous obstruction: a cause of periradicular fibrosis? Spine. 1989;14:558–568. doi: 10.1097/00007632-198906000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Hsu KY, Zucherman JF, Hartjen CA, Mehalic TF, Implicito DA, Martin MJ, Johnson DR, 2nd, Skidmore GA, Vessa PP, Dwyer JW, Cauthen JC, Ozuna RM. Quality of life of lumbar stenosis-treated patients in whom the X Stop interspinous device was implanted. J Neurosurg. 2006;5:500–507. doi: 10.3171/spi.2006.5.6.500. [DOI] [PubMed] [Google Scholar]
- 18.Inufusa A, An HS, Lim TH, Hasegawa T, Haughton VM, Nowicki BH. Anatomic changes of the spinal canal and intervertebral foramen associated with flexion–extension movement. Spine. 1996;21:2412–2420. doi: 10.1097/00007632-199611010-00002. [DOI] [PubMed] [Google Scholar]
- 19.Katz JN. Lumbar spinal fusion:surgical rates, costs, and complications. Spine. 1995;20:78S–83S. doi: 10.1097/00007632-199512151-00002. [DOI] [PubMed] [Google Scholar]
- 20.Katz JN, Harris MB. Clinical practice: lumbar spinal stenosis. N Engl J Med. 2008;358:818–825. doi: 10.1056/NEJMcp0708097. [DOI] [PubMed] [Google Scholar]
- 21.Katz JN, Lipson SJ, Chang LC, Levine SA, Fossel AH, Liang MH. Seven- to 10-year outcome of decompressive surgery for degenerative lumbar spinal stenosis. Spine. 1996;21:92–98. doi: 10.1097/00007632-199601010-00022. [DOI] [PubMed] [Google Scholar]
- 22.Kim KA, McDonald M, Pik JH, Khoueir P, Wang MY. Dynamic intraspinous spacer technology for posterior stabilization: case–control study on the safety, sagittal angulation, and pain outcome at 1-year follow-up evaluation. Neurosurg Focus. 2007;22:E7. [PubMed] [Google Scholar]
- 23.Kosaka H, Sairyo K, Biyani A, Leaman D, Yeasting R, Higashino K, Sakai T, Katoh S, Sano T, Goel VK, Yasui N. Pathomechanism of loss of elasticity and hypertrophy of lumbar ligamentum flavum in elderly patients with lumbar spinal canal stenosis. Spine. 2007;32:2805–2811. doi: 10.1097/BRS.0b013e31815b650f. [DOI] [PubMed] [Google Scholar]
- 24.Lindsey DP, Swanson KE, Fuchs P, Hsu KY, Zucherman JF, Yerby SA. The effects of an interspinous implant on the kinematics of the instrumented and adjacent levels in the lumbar spine. Spine. 2003;28:2192–2197. doi: 10.1097/01.BRS.0000084877.88192.8E. [DOI] [PubMed] [Google Scholar]
- 25.Madsen R, Jensen TS, Pope M, Sorensen JS, Bendix T. The effect of body position and axial load on spinal canal morphology: an MRI study of central spinal stenosis. Spine. 2008;33:61–67. doi: 10.1097/BRS.0b013e31815e395f. [DOI] [PubMed] [Google Scholar]
- 26.Malmivaara A, Slatis P, Heliovaara M, Sainio P, Kinnunen H, Kankare J, Dalin-Hirvonen N, Seitsalo S, Herno A, Kortekangas P, Niinimaki T, Ronty H, Tallroth K, Turunen V, Knekt P, Harkanen T, Hurri H. Surgical or non-operative treatment for lumbar spinal stenosis? A randomized controlled trial. Spine. 2007;32:1–8. doi: 10.1097/01.brs.0000251014.81875.6d. [DOI] [PubMed] [Google Scholar]
- 27.Mayoux-Benhamou MA, Revel M, Aaron C, Chomette G, Amor B. A morphometric study of the lumbar foramen: influence of flexion–extension movements and of isolated disc collapse. Surg Radiol Anat. 1989;11:97–102. doi: 10.1007/BF02096463. [DOI] [PubMed] [Google Scholar]
- 28.Moon ES, Kim HS, Park JO, Shin DE, Ha JW, Shim DJ, Kwak YH, Lee KI. Comparison of the predictive value of myelography, computed tomography and MRI on the treadmill test in lumbar spinal stenosis. Yonsei Med J. 2005;46:806–811. doi: 10.3349/ymj.2005.46.6.806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Porter RW. Spinal stenosis and neurogenic claudication. Spine. 1996;21:2046–2052. doi: 10.1097/00007632-199609010-00024. [DOI] [PubMed] [Google Scholar]
- 30.Richards JC, Majumdar S, Lindsey DP, Beaupre GS, Yerby SA. The treatment mechanism of an interspinous process implant for lumbar neurogenic intermittent claudication. Spine. 2005;30:744–749. doi: 10.1097/01.brs.0000157483.28505.e3. [DOI] [PubMed] [Google Scholar]
- 31.Schmid MR, Stucki G, Duewell S, Wildermuth S, Romanowski B, Hodler J. Changes in cross-sectional measurements of the spinal canal and intervertebral foramina as a function of body position: in vivo studies on an open-configuration MR system. AJR. 1999;172:1095–1102. doi: 10.2214/ajr.172.4.10587155. [DOI] [PubMed] [Google Scholar]
- 32.Schonstrom NS, Bolender NF, Spengler DM. The pathomorphology of spinal stenosis as seen on CT scans of the lumbar spine. Spine. 1985;10:806–811. doi: 10.1097/00007632-198511000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Schulte TL, Hurschler C, Haversath M, Liljenqvist U, Bullmann V, Filler TJ, Osada N, Fallenberg EM, Hackenberg L. The effect of dynamic, semi-rigid implants on the range of motion of lumbar motion segments after decompression. Eur Spine J. 2008;17:1057–1065. doi: 10.1007/s00586-008-0667-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Siddiqui M, Karadimas E, Nicol M, Smith FW, Wardlaw D. Influence of X Stop on neural foramina and spinal canal area in spinal stenosis. Spine. 2006;31:2958–2962. doi: 10.1097/01.brs.0000247797.92847.7d. [DOI] [PubMed] [Google Scholar]
- 35.Siddiqui M, Smith FW, Wardlaw D. One-year results of X Stop interspinous implant for the treatment of lumbar spinal stenosis. Spine. 2007;32:1345–1348. doi: 10.1097/BRS.0b013e31805b7694. [DOI] [PubMed] [Google Scholar]
- 36.Sirvanci M, Bhatia M, Ganiyusufoglu KA, Duran C, Tezer M, Ozturk C, Aydogan M, Hamzaoglu A. Degenerative lumbar spinal stenosis: correlation with Oswestry disability index and MR imaging. Eur Spine J. 2008;17:679–685. doi: 10.1007/s00586-008-0646-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Swanson KE, Lindsey DP, Hsu KY, Zucherman JF, Yerby SA. The effects of an interspinous implant on intervertebral disc pressures. Spine. 2003;28:26–32. doi: 10.1097/00007632-200301010-00008. [DOI] [PubMed] [Google Scholar]
- 38.Ullrich CG, Binet EF, Sanecki MG, Kieffer SA. Quantitative assessment of the lumbar spinal canal by computed tomography. Radiology. 1980;134:137–143. doi: 10.1148/radiology.134.1.7350593. [DOI] [PubMed] [Google Scholar]
- 39.Vogt MT, Cawthon PM, Kang JD, Donaldson WF, Cauley JA, Nevitt MC. Prevalence of symptoms of cervical and lumbar stenosis among participants in the osteoporotic fractures in men study. Spine. 2006;31:1445–1451. doi: 10.1097/01.brs.0000219875.19688.a6. [DOI] [PubMed] [Google Scholar]
- 40.Wang YC, Jeng CM, Wu CY, Chang HY, Huang YC, Wang YJ, Wang PC. Dynamic effects of axial loading on the lumbar spine during magnetic resonance imaging in patients with suspected spinal stenosis. J Formosan Med Assoc Taiwan yi zhi. 2008;107:334–339. doi: 10.1016/S0929-6646(08)60095-9. [DOI] [PubMed] [Google Scholar]
- 41.Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Blood E, Hanscom B, Herkowitz H, Cammisa F, Albert T, Boden SD, Hilibrand A, Goldberg H, Berven S, An H. Surgical versus non-surgical therapy for lumbar spinal stenosis. N Engl J Med. 2008;358:794–810. doi: 10.1056/NEJMoa0707136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Willen J, Wessberg PJ, Danielsson B. Surgical results in hidden lumbar spinal stenosis detected by axial loaded computed tomography and magnetic resonance imaging: an outcome study. Spine. 2008;33:E109–E115. doi: 10.1097/BRS.0b013e318163f9ab. [DOI] [PubMed] [Google Scholar]
- 43.Zucherman JF, Hsu KY, Hartjen CA, Mehalic TF, Implicito DA, Martin MJ, Johnson DR, 2nd, Skidmore GA, Vessa PP, Dwyer JW, Puccio ST, Cauthen JC, Ozuna RM. A multicenter, prospective, randomized trial evaluating the X Stop interspinous process decompression system for the treatment of neurogenic intermittent claudication: two-year follow-up results. Spine. 2005;30:1351–1358. doi: 10.1097/01.brs.0000166618.42749.d1. [DOI] [PubMed] [Google Scholar]