Abstract
Internal fixation is the established dorsal standard procedure for the treatment of thoracolumbar fractures. The main problem of the procedure is the false positioning of the pedicle screws. The exact determination of pedicle screws has up to now only been possible through postoperative computed tomography. This study was intended to clarify the diagnostic value of intraoperative 3D scans after pedicle screw implantation in thoracolumbar spine surgery. The direct intraoperative consequences of the 3D scans are reported and the results of the 3D scans are compared with the postoperative computed tomography images. Intraoperative 3D scans were prospectively carried out from June 2006 to October 2008 on 95 patients with fractures of the thoracolumbar spine that have been treated with internal fixation. Screws positions were categorised intraoperatively, screws in relevant malposition were repositioned immediately. A computed tomography of the involved spinal section was carried out postoperatively for all patients. The positions of the pedicle screws were determined and compared in the axial reconstructions of both procedures. Four hundred and fourteen pedicles with enclosed screws were evaluated by the 3D scans. The time needed for carrying out the 3D scan amounts to an average of 8.2 min. Eleven screws (2.7%) in ten patients were primarily intraoperatively repositioned on the basis of the 3D scan evaluation. Two of 95 patients had to have false positions of the screws revised secondarily following evaluation of the computed tomographies. The secondary postoperative revision rate of the patients amounts to 2.1%. In relation to the number of screws, this is a revision rate of 0.5%. The postoperative computed tomographies showed 323 pedicles without cortical penetration by the screws (78.0%). Ninety-one screws penetrated the pedicle wall (22%). It was possible to postoperatively compare the position classifications of 406 pedicle screws. The CT showed 378 correct screw positions, while 28 screws were positioned falsely. On the basis of the 3D scans, 376 of 378 correct positions were correctly assessed. Twenty-one of 28 false positions could be correctly classified. The sensitivity of all 3D scans reached 91.3% and the specificity 98.2%. The position of 97.8% of the pedicle screws was correctly recognised by the intraoperative 3D scan. Nine screws were classified falsely (2.2%). The comparison of the classification results showed significantly higher error findings by the 3D scan in the spinal section T1–10 (P = 0.014). The image quality of the 3D scan correlates significantly with the width of the scanned pedicle, with the body mass index, the scanned spinal section and the extent of the fixation assembly. 3D scans showed a high accuracy in predicting pedicle screw position. Primary false placement of screws and primary neurovascular damage cannot be avoided. But intraoperative evaluation of the 3D scans resulted in a primary revision rate of 2.7% of the pedicle screws and we could lower the secondary revision rate to 0.5%.
Keywords: Three-dimensional fluoroscopy, Intraoperative 3D-imaging, Pedicle screws, Thoracolumbar fracture, Spine
Introduction
Vertebral body fractures with an accompanying neurological deficit, relevant axis deviation and instability criteria represent an indication for operative stabilisation [28]. Dorsal, ventral and combined fusions are standard methods of treatment. The dorsal repositioning and stabilisation of fractures of the thoracic and lumbar portions of the spine with transpedicle screws was introduced by Roy-Camille [23]. Internal fixation is in the meantime the established standard procedure for the care of thoracolumbar fractures and is an indispensible instrument in degenerative dorsal fusion surgery. The main problem of the procedure is the false positioning of the pedicle screws, which affects up to 40% of the screws [7]. This results in revision rates from 2.8 to 6.6% [16, 24]. Lateral malpositions affect the stability and can cause loosening of the fixateur. Medially misplaced screws can cause primary and secondary neurological damages.
Navigation-supported procedures can reduce the rate of false positioning, but cannot exclude the possibility of considerable false positions [12, 26]. The exact determination of pedicle screw positions has up to now only been possible through computed tomography of the spinal section involved. Conventional X-rays and intraoperative image intensifier examinations offer no adequate diagnostic certainty [4]. However, intraoperatively stationed computed tomographies are only seldom available.
Meanwhile mobile 3D image intensifiers that provide multiplanar reconstructions of the scanned body section from isocentrically acquired conventional X-ray images are available [22]. They could be used as a pure diagnostic tools and in combination with a navigation system. Intraoperative use of 3D image intensifier as a diagnostic tool cannot prevent primary damage of neurovascular structures by pedicle screws. But, reliable intraoperative identification of misplaced screws can reduce secondary operative revision rates of the patients.
This study was intended to clarify the diagnostic value of intraoperative 3D scans after pedicle screw placement during treatment of dorsal fractures of the thoracolumbar spine in comparison with postoperative computed tomography and to evaluate the immediate intraoperative consequences of the 3D scans.
Materials and methods
In the course of a prospective study carried out between June 2006 and October 2008 with 95 consecutive patients (55 male, 40 female) who were treated for a fracture of the thoracolumbar spine with internal fixation, an intraoperative 3D-imaging scan with the mobile “Ziehm Vario 3D” fluoroscopic unit (Ziehm Imaging GmbH, Nuremberg, Germany) was carried out. The patients were aged between 11 and 82 years old with a mean age of 54. Indications for stabilisation were traumatic instable fractures (type A2.3/3.1/3.2/3.3, all type B and C).
The patients were operated on in a face-down position on a radiolucent carbon table. As fixation we used the “Universal Spine Systems” (USS, Synthes, Umkirch, Germany) with screws with a thickness of 4.0–7.2 mm. Each pedicle diameter was measured at the preoperative CT to implant screws with the largest possible diameters.
Pedicle screws were placed using anatomical landmarks as guided by lateral fluoroscopic imaging and preoperative computed tomography scan review. Thoracic starting point was at the junction of horizontal line along the inferior border of the facet joint and a vertical line at the junction of the outer third to central third of the facet joint. Lumbar starting point was the junction of mammillary process, inferior aspect of transverse process and pars interarticularis. The entry point was opened sharply and an awl was used to cannulate the pedicle and vertebral body to the anterior cortex. Anteroposterior fluoroscopic view was used when problems with awl or screw insertion occurred.
The 3D scan was carried out with 63 patients following the placement of the pedicle screws and with 32 patients following the complete installation of the fixation. The period following the calibration of the devices until the end of the isocentric image acquisition loop was defined as a “scan process” and recorded in minutes. The isocentric recording of the image data took place in a condition of apnoe through the fully automatic, motorised, orbital movement of the C-arm with a maximum rotational radius of 135° around the patient. A total of 100–120 individual images were required for each patient. Upon conclusion of the isocentric scan, the device calculates a 3D data record from the images of the film loop through algebraic reconstruction algorithms, for which the scan volume corresponds to a cube with edge lengths of 12 cm. The data record allows reconstructions on the axial, sagittal and coronary levels.
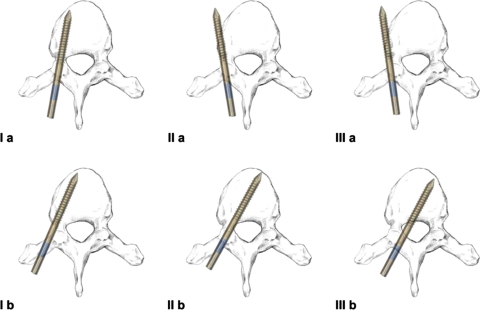
The 3D scan was evaluated intraoperatively by the surgeon. The foundation for the evaluation was the classification according to Zdichavsky [31]. This was followed by a breakdown into six possible positions. These were defined by the location of the pedicle screws and the diameter of the pedicle screws in relation to the pedicle and the corpus. A precise explanation is provided in Table 1 and in Fig. 1.
Table 1.
Scoring system of pedicle screws by Zdichavsky et al. [31]
| Grade | Criteria of the pedicle screw scoring system |
|---|---|
| Ia | ≥Half of PSD within the pedicle and ≥half of PSD within the vertebral body |
| Ib | ≥Half of PSD lateral outside the pedicle and >half of PSD within the vertebral body |
| IIa | ≥Half of PSD within the pedicle and >half of PSD lateral outside the vertebral body |
| IIb | ≥Half of PSD within the pedicle and tip of PS crossing the middle line of the vertebral body |
| IIIa | >Half of PSD lateral outside the pedicle and >half of PSD lateral outside the vertebral body |
| IIIb | >Half of PSD medial outside the pedicle and tip of PS crossing the middle line of the vertebral body |
PS pedicle screw, PSD pedicle screw diameter
Fig. 1.
Scoring system of pedicle screws by Zdichavsky et al. [31]
Where false positions requiring revision were found, the relevant screws were repositioned. False positions absolutely requiring revision were those of type IIIa and IIIb; those false positions with a relative need for revision were of type II a and II b. A second 3D scan was carried out on three patients following repositioning. In the case of intraoperative repetition of the scan, the second 3D scan was evaluated in comparison to the CT.
A postoperative computed tomography of the relevant spinal section was carried out on all patients (Aquilion 32, Toshiba Computer Systems, Neuss, Germany). A program to reduce metal artefacts was used with a kollimation thickness of 0.5 mm.
The postoperative appraisal of the 3D scan and of the computed tomography was carried out at different times by two experienced spinal surgeons (T. Mittlmeier, M. Beck) using the consensus procedure. In the event of differences in their findings, the “higher grade” false position was automatically taken. The CT results are evaluated as the “gold standard” for the comparisons.
In the axial reconstructions of both procedures, the positions of the pedicle screws were defined using the classification of Zdichavsky et al. [31] (Fig. 1). The maximum width of the pedicle involved was measured in the CT in millimetres. The thoracolumbar spine was divided up into the sections T1–T10 and T11–L5 in accordance with its anatomic-functional structure.
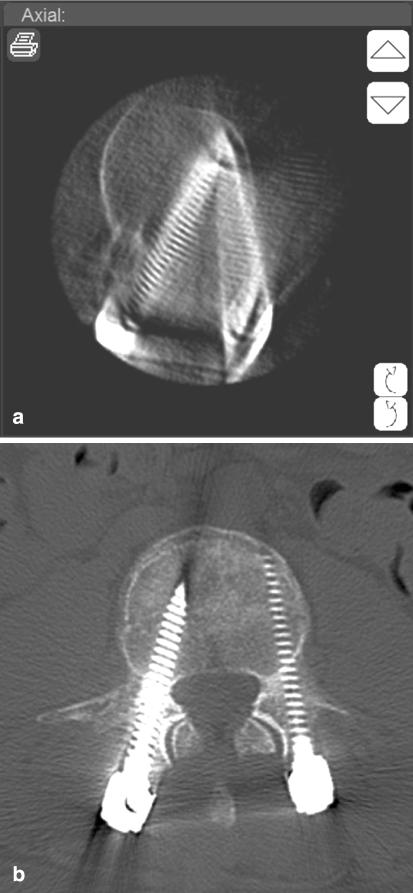
The image quality of the 3D scan was classified as good, average or poor for each screw (Fig. 2). The evaluation criteria are explained in Table 2.
Fig. 2.

T12 with two pedicle screws in good picture quality. Both cortices are visible
Table 2.
Evaluation criteria of 3D-imaging picture quality
| Picture quality | Exposure of cortical bone at PS level | Screws, n = 414 |
|---|---|---|
| Good | Two cortices visible | 134 |
| Moderate | One cortex visible | 254 |
| Poor | No cortex visible | 26 |
The “body mass index” (BMI) of the patients was defined in accordance with the recommendations of the WHO and the patients divided into three groups (overweight, normal weight, underweight). Three patients were underweight (BMI < 20kg/m2), 37 were of normal weight (BMI 20–24.99 kg/m2) and 55 were overweight (BMI > / = 25 kg/m2).
The statistical calculations were carried out with the software programme SPSS Version 15 (Chicago, USA). The Chi-square test according to Pearson was used for the statistical evaluation. A value of P < 0.05 was accepted as statistically significant.
Results
Intraoperative scans were carried out on 95 patients in the period examined. Four hundred and fourteen pedicles with enclosed screws were recorded and evaluated by the 3D scans. The distribution of the pedicle screws to the individual vertebral bodies and the two spinal sections are shown in Table 3.
Table 3.
Distribution of screws, malpositions and revisions in relationship to the vertebrae and the vertebral level
| Vertebra | n | T2 | T3 | T4 | T5 | T6 | T7 | T8 | T9 | T10 | T11 | T12 | L1 | L2 | L3 | L4 | L5 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Screws | 414 | 2 | 6 | 6 | 8 | 14 | 8 | 10 | 12 | 10 | 42 | 76 | 64 | 80 | 48 | 12 | 16 |
| Revision of screws | 11 | 1 | 1 | 2 | 1 | 3 | 1 | 2 | |||||||||
| Malposition of screws | 30 | 1 | 1 | 2 | 3 | 7 | 2 | 6 | 1 | 4 | 1 | 2 | |||||
| Vertebral level | T1–T10 | T11–L5 | |||||||||||||||
| Screws | 76 | 338 | |||||||||||||||
| Intraoperative revision of screws | 2 | 9 | |||||||||||||||
| Average diameter of the pedicles (mm) | 4.6 | 8.3 | |||||||||||||||
| Malposition of screws | 16 | 14 | |||||||||||||||
The installations encompassed 85 × 4 screws, 3 × 6 screws and 7 × 8 screws. In all cases all screws were scanned in only one cycle.
Eleven screws in ten patients were primarily intraoperatively repositioned on the basis of the 3D scan evaluation. Three screws were conspicuous in the intraoperative 3D scan as lateral type IIIa false positions and were primarily repositioned. Postoperatively the computed tomographies showed all three corrected screws as being in the correct type Ia position.
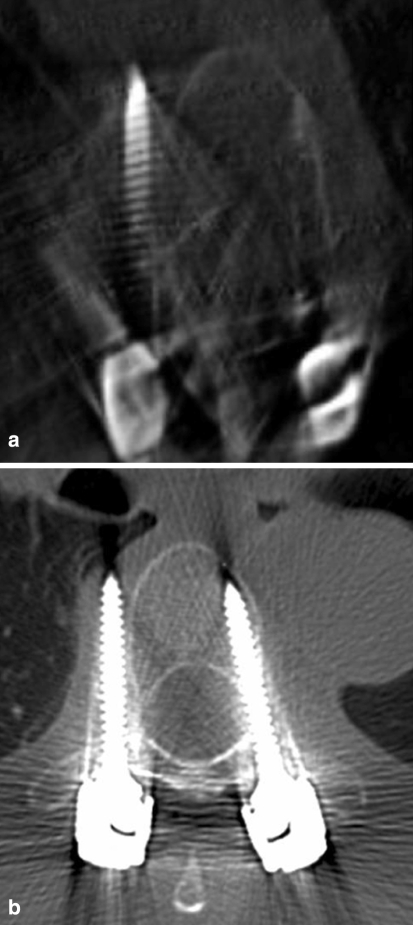
The intraoperative evaluation of the 3D scan classified eight screws as having medial malpositions with a need for primary revision (Fig. 3a, b). Four type IIIb screws were revised and the CT showed two as moderate type IIb false positions and two as ideal type Ia positions following correction. Four screws in the type IIb position were corrected and were conspicuous in the CT as a type Ia position. Of 11 screws primarily evaluated as falsely positioned, 9 could be corrected to an ideal type Ia position, while 2 screws showed a tolerable medial false positions of type IIb.
Fig. 3.
a Intraoperative 3D-scan of L4. Malposition type IIIb of the right pedicle screw. Intraoperative correction of the screw. b Postoperative CT of L4. Correct position type 1a of the right pedicle screw after intraoperative revision. No neurological deficit after catastrophic malposition of the right screw
A second intraoperative 3D scan was carried out on three patients following the correction of the screws, which confirmed a correction of the position for each. Carrying out a second 3D scan was an individual decision of the responsible surgeon, especially when he was in doubt about the result of the correction.
Two of 95 patients had to have false positions of the screws and were revised secondarily following evaluation of the computed tomographies. In one case a type IIIa malpositioned screw (T7) compromised the stability of the fixateur (Fig. 4a, b). In the other case a type IIIb malpositioned screw (T6) narrowed the diameter of the spinal canal. To prevent secondary lesions of the myelon and the root we decided to correct the screw. No patient of the study had a neurological deficit.
Fig. 4.
a, b T 7 with a pedicle screw in type IIIa malposition right. Intraoperativly the 3D-scan was misinterpreted by the surgeon as a type IIb position and no correction was performed. Postoperative 3D-scan visualisation shows clearly a type IIIa malposition in good picture quality, corresponding postoperative CT-scan. Secondary screw revision was done. Mistake caused by a lack of experience with the image intensifier console in the context of the “learning curve”
The total revision rate of the patients amounts to 2.1%. In relation to the number of screws used, there was a secondary revision rate of 0.5% (2 of 414 screws).
The postoperative computed tomographies showed 323 pedicles without cortical perforation by the screws (78.0%). Ninety-one screws penetrated the pedicle wall (22%); there were 36 medial false positions (27 × 1–2, 7 × 3–4, 2 × 5–6 mm) and 55 lateral injuries (44 × 1–2, 11 × 3–4 mm).
It was possible to postoperatively compare the position classifications of 406 pedicle screws. Eight corrected and not re-scanned pedicle screws were excluded. The CT showed 378 correct screw positions of position type Ia while 28 screws were falsely positioned. There were lateral false positions in 18 cases respectively and 10 screws showed medial false positions. A precise breakdown is shown in Table 4.
Table 4.
Distribution of the screw positions using the classification of Zdichavsky et al. [31]
| Screws n = 406 | Position | Number of pedicle screw positions in CT | Correct assessment of 3D-imaging |
|---|---|---|---|
| Correct | Ia | 378 | 376 |
| Lateral malposition | Ib | 12 | 9 |
| IIa | 5 | 5 | |
| IIIa | 1 | 1 | |
| Medial malposition | IIb | 9 | 6 |
| IIIb | 1 | 0 | |
| Disagreement | – | 9 | |
| 406 | 406 |
On the basis of the 3D image converter reconstructions, 376 of 378 correct positions were correctly assessed (correct negative). Twenty-one of 28 false positions could be correctly classified (correct positive). One lateral (Ib) and one medial (IIb) false position was evaluated as correctly positioned in the 3D scan (false negative). Two correct screw positions were interpreted in the 3D scan as medial lateral false positions (false positive). Five false positions were correctly recognised as such, but their expansion was underestimated (false positive).
The sensitivity of the 3D scan for the classification used amounts to 91.3%, and the specificity of the 3D image intensifier examination amounts to 98.2%. The position of the pedicle screws was correctly recognised by the intraoperative 3D scan in 97.8% (397/406) of all cases. Nine screws were classified falsely (2.2%). Four of the nine falsely classified screws were located in the thoracic section (T1–10).
A significantly higher rate of false findings of the 3D scan was determined in the spinal section T1–10 in comparison to T11–L5 (P = 0.014; Table 5).
Table 5.
Comparison of misjudgement, rates of secondary screw revisions and error rates in correlation to the vertebral level
| Vertebral level | ||
|---|---|---|
| T1–T10 | T11–L5 | |
| Number of pedicle screws (n = 406) | 75 | 331 |
| Misjudgement of screwposition | 4 | 5 |
| Pedicle screws requiring revision after CT | 2 | 0 |
| Error rate of 3D-imaging | 5.3% | 1.5% |
The image quality of 134 screws in the 3D scan was evaluated as good, of 252 as moderate and of 28 screws as poor (Table 2). The image quality of the 3D scan is significantly influenced by the width of the scanned pedicle (P = 0.031), by the BMI of the test subject (P = 0.001) and by the scanned spinal section (P = 0.032). Wide pedicles, the section T11–L5 and a lower BMI allow for good image quality. The image quality of the 3D scan is also influenced by the extent of the fixation assembly. Complete assemblies significantly worsen the image quality (P < 0.001).
For the entire scan process we required an average of 8.2 min (6–18 min), the first 25 scans took a mean time of 9.9 min (7–18), the last 25 scans took 7.4 min (6–8). The pure screening time of the 3D scan amounted to 112 s (91–152 s).
Discussion
The exact determination of pedicle screws is only possible with computed tomography. Standard X-ray images and intraoperative image intensifier examinations have a higher rate of uncertainty [4]. CT devices integrated into the operating room area are only rarely available. 3D image converters that create 2D and 3D reconstructions from an isocentrically acquired image data record are beginning to close this gap.
Preclinical studies carried out on cadaveric specimens and on the high-contrast phantom showed sufficient image quality for the axial skeleton [21]. Although 3D image intensifiers have been used clinically for almost a decade, only a few studies are available that examine the diagnostic value of intraoperative 3D imaging in spinal surgery. In clinical studies, Deinsberger and Baldauf used 3D image intensifiers for quality control following ventral cervical decompression and for inspecting the position of ventral implants [2, 8, 9]. The intraoperative evaluations of the 3D scan resulted for 12.5–14.3% of the patients to the continuation and correction of the surgical measure and to the avoidance of a secondary revision. Mauer and Kunz used a 3D image intensifier in ten cases following dorsal lumbar decompression, which resulted in a change of the operative procedure for two patients [17]. In combination with an intraoperative myelography, Patel et al. carried out a 3D image intensifier examination of ten patients following dorsal lumbar decompression, and the decompression was expanded for three patients on the basis of the 3D imaging [20]. In an experimental study, Verlaan compares measurement results from 3D image data records from fractured and operated vertebral bodies with the measured values of the anatomical specimens [29]. He reports of a high degree of precision of the 3D scan measurement. In an attempt to answer the question of whether pedicle injuries caused by screws can be discovered with 3D imaging, Wang et al. positioned 216 transpedicle screws from T1–S1 on cadaveric spines [30]. Visual inspections of the reinforced vertebral bodies were carried out with 3D scans, CT scans and visual inspections as the gold standard. The sensitivity of all 3D scans reached 71.6% and the specificity 78.9%. Problematic for both experimental studies was the fact that the examinations were carried out on spinal specimens consisting entirely of bone. With our examinations we were able to demonstrate that the image quality is significantly influenced by the BMI of the patients and thus by the surrounding soft-tissue parts. The study results of Verlaan and Wang can thus have only limited applicability for clinical usage.
The entry of pedicle perforations in millimetres is important for the comparison of imaging procedures and can determine the precision of an implantation method. However, an intraoperative measurement in millimeter steps is not practicable and not decisive for the objective. In the middle thoracic area, the average pedicle diameter amounts to <4 mm [5, 15]. This must result in a penetration of the pedicle walls by even the smallest pedicle screws (4 mm), but this has no clinical consequences.
A clear, easily applicable and relevant classification is necessary for intraoperative evaluation. For this reason we have applied the classification of Zdichavsky et al. [31]. It allows for the differentiation of a correct position from three medial false positions and two false positions requiring revision. Taking into account the thickness of the pedicle and the screws considers the anatomical relationships of the entire thoracolumbar spine. With the aim of creating an “outcome-based classification” for thoracic pedicle screws that is relevant for therapy, Upendra et al. published a slightly modified version in 2008 [27].
The dorsal transpedicle screw implantation requires precise anatomical knowledge of the surgeon. The intraosseous corridor of the pedicle for the positioning of the screws is limited [15]. Even lateral deviations in millimetre scale can damage the stability of the fixation and medial pedicle penetrations can cause damage to the bone marrow and the nerve roots. While Castro et al. first anticipate a lesion of the nerve root in the lumbar portion of the spine with a medial false position of the screw as of 6 mm, more recent anatomical examinations by Lien et al. show that the distance between the pedicle wall and the nerve root varies considerably in the lumbar region of the spine and occasionally amounts to only 2.4 mm [7, 15].
The implantation of pedicle screws can take place on the basis of anatomical landmarks, supported by an image converter or navigated. Zdichavsky et al. had to revise secondarily 5% of pedicle screws in the thoracic spine implanted with fluoroscopic monitoring, 14% of the patients (6/43) were affected [32]. Bransford et al. revised 1.2% of the patients and 0.26% of the screws following fluoroscopically assisted thoracic pedicle screw instrumentation in the thoracic region of the spine [6]. Laine reports a 3% screw-induced secondary patient revision rate in the lumbar region of the spine [13].
Navigation systems were developed to lower misplacement rates of pedicle screws. Arand et al. using 2D fluoroscopic navigation at the thoracic spine, had a pedicle perforation rate of 43.4% and pointed out an unsatisfactory inaccuracy of this method especially at the thoracic spine [1]. A higher accuracy achieved CT- and 3D-based navigation. An experimental study showed no significant difference in accuracy comparing CT- and 3D-based navigation [11].
Laine and Schnake documented significantly lower pedicle penetration rates for CT navigation-supported procedures [12, 26]. However, despite navigation, considerable false positions in the thoracic area of >4 mm (1.9%) could not be avoided. Navigation for all vertebral bodies was not possible for a fifth of the patients. A total of 0.5% of the screws positioned with navigation or 1.8% of patients had to be revised due to a false position of the screws [26]. Using 3D navigation Lekovic et al. had 1.1% of thoracic screws in a non acceptable position completely outside the vertebral body [14].
Several authors favour the exclusive implantation of the screws on the basis of anatomical landmarks both in the upper area of the thoracic spine and for spines with scoliotic deformations [19, 25]. Schizas reports of a rate of 11.7% falsely positioned screws in the area T1–T6, but with no need for operative revision [25]. Of 1,009 manually inserted pedicle screws in cases of scoliosis, 73% were intrapedicular, 20.3% penetrated the pedicle limits in an acceptable false position and 6.7% of the screws were classified as requiring revision [19].
Every implantation procedure can produce a primary damage of neurovascular structures. 3D- and CT-navigation seems to reduce the risk significantly [14, 18]. 3D imaging after screw implantation although cannot avoid primary neurovascular damage, but reliable intraoperative visualization of malposition by 3D scan allows primary revision of the screws and reduces the rate of secondary revisions.
As a consequence of intraoperative 3D imaging, we primary repositioned 11 of 414 screws (2.7%).
Ultimately only two screws were in an unacceptable postoperative false position (0.5%). One false position of the screws results from an intraoperative misinterpretation of the 3D scan with one of the first patients, caused by a lack of experience with the operating console of the image intensifier in the context of the “learning curve.” The postoperative evaluation of this 3D scan clearly showed the unacceptable lateral type IIIa position (Fig. 4a, b). Thus remains, taking only the postoperative findings into account, only one false position of the screw that was underestimated in the 3D scan and required operative revision. The postoperative revision rate thus amounts to only 0.24% in relation to the number of screws.
With the intraoperative pedicle screw inspection with a routine 3D scan we were able to reduce our secondary revision rates in the lower range of the percentage rates found in the literature (Table 6). The immediate intraoperative revision presents no obstacle for the surgeon and is oriented to objective criteria. The diagnosis of postoperative secondary revision precedes the admission of an error. This may influence the objectivity of the diagnosis and lead to the acceptance of screws requiring revision.
Table 6.
Comparison of malposition and revision rates of pedicle screws
| Study | Method of screw placement | Patients (n) | Pedicle screws (n) | Vertebral region | Rate of pedicle cortex perforation (%) | Revision rate of screws (%) | Revision rate of patients (%) |
|---|---|---|---|---|---|---|---|
| Zdichavsky [32] | Image intensifier | 43 | 278 | T1–T10 | 15.5 | 5.0 | 14 |
| Bransford [6] | Image intensifier | 245 | 1,533 | T1–T10 | No data | 0.3 | 1.2 |
| Laine [13] | Image intensifier | 30 | 152 | L2–S1 | 21 | 0.7 | 3.3 |
| Schnake [26] | Image intensifier | 29 | 123 | T1–T10 | 31.9 | 0.0 | 0.0 |
| Schnake [26] | CT navigation | 56 | 211 | T1–T10 | 17.5 | 0.5 | 1.8 |
| Arand | 2D navigation | 29 | 111 | T4–L5 | 40.5 | No data | No data |
| Schizas [25] | Free-hand technique | 13 | 60 | T1–T6 | 11.7 | 0.0 | 0.0 |
| Lekovic [14] | 3D navigation | 12 | 94 | T1–T12 | 19.1 | 3.3 | No data |
| Lekovic [14] | 2D navigation | 25 | 183 | T1–T12 | 17.5 | 1.1 | No data |
| Modi [19] | Free-hand technique | 37 | 1,009 | T1–S1 | 27 | 6.7 | No data |
| Present study | 3D Fluoroscopy controlled | 95 | 414 | T2–L5 | 22 | 0.5/0.25 | 2.0/1.0 |
Our figures also make clear that the risk of penetration of the pedicle and a suboptimal screw position is greatest in the thoracic area T1–T10, caused by the narrow pedicle and corpus anatomy [5, 15]. The 3D imaging process shows the highest error rate of 6% in the area of the most frequent false positioning rates. However, device-related developments also indicate grounds for hope of more precise imaging.
The time required for the entire procedure of less than 9 min is acceptable and will also be reduced as a result of technical developments.
Our datas showed a learning curve in the mechanical usability of the 3D intensifier. Optimizing the secondary sterile draping and continuous training of the perpetual step sequences of the 3D intensifier reduced the time of the scan process. Likewise the optimal visualisation at the operating console with centering the planes of interest at each single screw took some experience and led to an intraoperative classification mistake in the beginning of the study (Fig. 4a, b). Especially, not correctly centred planes lead to false assessment of the 3D scans.
The radiation exposure of image intensifiers is measured as “area dose product” (cGy/cm2), measurement of computed tomographies is done as “length dose product” (Gy/cm). A direct comparison of the individual patient radiation dose parameters is not possible because of the total different application forms of x-radiation. Dose measurement at phantoms showed a considerable lower radiation exposure of the lumbar spine using 3D intensifier compared with a spiral CT standard procedure [21]. Berger et al. confirmed the lower radiation doses using the Ziehm Vario 3D intensifier [3].
The additional radiation level for the operating team is extremely low, because they can leave the area of radiation while the fully automatic acquisition scan is done.
Using a 3D-navigation system the radiation dose is nearly the same plus the necessary shoots placing the implants. CT-navigation reduces radiation exposure for the patient when the first computed tomography after trauma can be used for planning [10]. The radiation dose increases considerably when an additive CT scan for navigation planning is required. Also the recommended additional use of the 2D intensifier during placement of navigated screws increases the radiation doses [26].
Despite this, at the end of a navigation procedure no reliable image method is done to determinate the real screw positions. In this context the additional radiation dose of a 3D scan after pedicle screw placement is acceptable allowing for the diagnostic and therapeutic value.
Conclusions
3D scans after pedicle screw positioning cannot avoid false placement of screws and primary neurovascular damages. But screws in malposition can be detected with a high reliability. Immediate correction of malplaced screws lowers the secondary revision rate of the patients and prevents patients ahead secondary neurovascular problems and instability or dislocation of the fixateur.
A postoperative computed tomography for the evaluation of the screw position remains dispensable in the section T11–L5 and with good image quality of the 3D scan.
References
- 1.Arand M, Teller S, Gebhard F, Schultheiss M, Keppler P. Clinical accuracy of fluoroscopic navigation at the thoracic and lumbar spine. Z Orthop Unfall. 2008;146:458–462. doi: 10.1055/s-2008-1038539. [DOI] [PubMed] [Google Scholar]
- 2.Baldauf J, Müller JU, Fleck S, Hinz P, Chiriac A, Schroeder HW. The value of intraoperative three dimensional fluoroscopy in anterior decompressive surgery of the cervical spine. Zentralbl Neurochir. 2008;69:30–34. doi: 10.1055/s-2007-992796. [DOI] [PubMed] [Google Scholar]
- 3.Berger J, Stuby F, Hoffmann J, Heuschmid M, Buchgeister M. Dosimetrie dreidimensionaler bildgebender Verfahren des Beckens in der Unfallchirurgie mit hochempfindlichen Thermolumineszenzdosimetern. Abstract, 39. Oldenburg: DGMP Tagung; 2008. [Google Scholar]
- 4.Berlemann U, Heini P, Müller U, Stoupis C, Schwarzenbach O. Reliability of pedicle screw assessment utilizing plain radiographs versus CT reconstruction. Eur Spine J. 1997;6:406–411. doi: 10.1007/BF01834069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berlet GC, Boubez G, Gurr KR, Bailey SI. The USS pedicle hook system: a morphometric analysis of its safety in the thoracic spine. J Spinal Disord. 1999;12:234–239. [PubMed] [Google Scholar]
- 6.Bransford R, Bellabarba C, Thompson JH, Henley MB, Mirza SK, Chapman JR. The safety of fluoroscopically-assisted thoracic pedicle screw instrumentation for spine trauma. J Trauma. 2006;60:1047–1052. doi: 10.1097/01.ta.0000215949.95089.18. [DOI] [PubMed] [Google Scholar]
- 7.Castro WHM, Halm H, Jerosch J, Malms J, Steinbeck J, Blasius S. Accuracy of pedicle screw placement in lumbar vertebrae. Spine. 1996;21:1320–1324. doi: 10.1097/00007632-199606010-00008. [DOI] [PubMed] [Google Scholar]
- 8.Deinsberger R, Regatschnig R, Ungersböck K. Intraoperative evaluation of bone decompression in anterior cervical spine surgery by three-dimensional fluoroscopy. Eur Spine J. 2005;14:671–676. doi: 10.1007/s00586-004-0852-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deinsberger R, Regatschnig R, Ungersböck K. Intraoperative evaluation of implants in anterior cervical spine surgery by three-dimensional fluoroscopy. J Spinal Disord Tech. 2005;18:216–218. [PubMed] [Google Scholar]
- 10.Gebhard FT, Kraus MD, Schneider E, Liener UC, Kinzl L, Arand M. Does computer-assisted spine surgery reduce intraoperative radiation doses? Spine. 2006;31:2024–2027. doi: 10.1097/01.brs.0000229250.69369.ac. [DOI] [PubMed] [Google Scholar]
- 11.Geerling J, Gösling T, Gösling A, Ortega G, Kendoff D, Citak M, Krettek C, Hüfner T. Navigated pedicle screw placement: experimental comparison between CT- and 3D fluoroscopy-based techniques. Comput Aided Surg. 2008;13:157–166. doi: 10.1080/10929080802102110. [DOI] [PubMed] [Google Scholar]
- 12.Laine T, Lund T, Ylikoski M, Lohikoski J, Schlenzka D. Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. Eur Spine J. 2000;9:235–240. doi: 10.1007/s005860000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Laine T, Mäkitalo K, Schlenzka D, Tallroth K, Poussa M, Alho A. Accuracy of pedicle screw insertion: a prospective CT study in 30 low back patients. Eur Spine J. 1997;6:402–405. doi: 10.1007/BF01834068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lekovic GP, Potts EA, Karahalios DG, Hall G. A comparison of two techniques in image-guided thoracic pedicle screw placement: a retrospective study of 37 patients and 277 pedicle screws. J Neurosurg Spine. 2007;7:393–398. doi: 10.3171/SPI-07/10/393. [DOI] [PubMed] [Google Scholar]
- 15.Lien SB, Liou NH, Wu SS. Analysis of anatomic morphometry of the pedicles and the safe zone for through-pedicle procedures in the thoracic and lumbar spine. Eur Spine J. 2007;16:1215–1222. doi: 10.1007/s00586-006-0245-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB. Complications associated with pedicle screws. J Bone Joint Surg Am. 1999;81:1519–1528. doi: 10.2106/00004623-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Mauer UM, Kunz U. Intraoperative three-dimensional imaging to monitor selective decompression in lumbar spinal stenosis. Orthopade. 2006;35:1258–1260. doi: 10.1007/s00132-006-1025-8. [DOI] [PubMed] [Google Scholar]
- 18.Mirza SK, Wiggins GC, Kuntz C, York JE, Bellabarba C, Knonodi MA, Chapman JR, Shaffrey CI. Accuracy of thoracic vertebral body screw placement using standard fluoroscopy, fluoroscopic image guidance, and computed tomographic image guidance. Spine. 2003;28:402–413. doi: 10.1097/00007632-200302150-00018. [DOI] [PubMed] [Google Scholar]
- 19.Modi HN, Suh SW, Fernandez H, Yang JH, Song HR. Accuracy and safety of pedicle screw placement in neuromuscular scoliosis with free-hand technique. Eur Spine J. 2008;17:1686–1696. doi: 10.1007/s00586-008-0795-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patel VV, Dwyer A, Estes S, Burger E. Intraoperative 3-dimensional reconstructed multiplanar fluoroscopic imaging for immediate evaluation of spinal decompression. J Spinal Disord Tech. 2008;21:209–212. doi: 10.1097/BSD.0b013e31811ff307. [DOI] [PubMed] [Google Scholar]
- 21.Rock C, Kotsianos D, Linsenmaier U, Fischer T, Brandl R, Vill F, Wirth S, Kaltschmidt R, Euler E, Pfeifer KJ, Reiser M. Studies on image quality, high contrast resolution and dose for the axial skeleton and limbs with a new, dedicated CT system (ISO-C-3 D) Rofo. 2002;174:170–176. doi: 10.1055/s-2002-20107. [DOI] [PubMed] [Google Scholar]
- 22.Rock C, Linsenmaier U, Brandl R, Kotsianos D, Wirth S, Kaltschmidt R, Euler E, Mutschler W, Pfeifer KJ. Presentation of a new mobile C-arm image amplifier (Iso-C-3D): initial results with three-dimensional CT-imaging. Unfallchirurg. 2001;104:827–833. doi: 10.1007/s001130170053. [DOI] [PubMed] [Google Scholar]
- 23.Roy-Camille R, Saillant G, Berteaux D, Salgado V. Osteosynthesis of thoraco-lumbar spine fractures with metal plates screwed through the vertebral pedicles. Reconstr Surg Traumatol. 1976;15:2–16. [PubMed] [Google Scholar]
- 24.Schizas C, Michel J, Kosmopoulos V, Theumann N. Computer tomography assessment of pedicle screw insertion in percutaneous posterior transpedicular stabilization. Eur Spine J. 2007;16:613–617. doi: 10.1007/s00586-006-0221-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schizas C, Theumann N, Kosmopoulos V. Inserting pedicle screws in the upper thoracic spine without the use of fluoroscopy or image guidance. Is it safe? Eur Spine J. 2007;16:625–629. doi: 10.1007/s00586-006-0262-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schnake KJ, König B, Berth U, Schroeder RJ, Kandziora F, Stöckle U, Raschke M, Haas NP. Accuracy of CT-based navitation of pedicle screws in the thoracic spine compared with conventional technique. Unfallchirurg. 2004;107:104–112. doi: 10.1007/s00113-003-0720-8. [DOI] [PubMed] [Google Scholar]
- 27.Upendra BN, Meena D, Chowdhury B, Ahmad A, Jayaswal A. Outcome-based classification for assessment of thoracic pedicular screw placement. Spine. 2008;33:384–390. doi: 10.1097/BRS.0b013e3181646ba1. [DOI] [PubMed] [Google Scholar]
- 28.Vaccaro AR, Kim DH, Brodke DS, Harris M, Chapman JR, Schildhauer T, Routt ML, Sasso RC. Diagnosis and management of thoracolumbar spine fractures. Instr Course Lect. 2004;53:359–373. [PubMed] [Google Scholar]
- 29.Verlaan JJ, Kraats EB, Walsum T, Dhert WJA, Oner FC, Niessen WJ. Three-dimensional rotational X-ray imaging for spine surgery. Spine. 2005;30:556–561. doi: 10.1097/01.brs.0000154650.31781.85. [DOI] [PubMed] [Google Scholar]
- 30.Wang MY, Kim KA, Liu CY, Kim P, Apuzzo ML. Reliability of three-dimensional fluoroscopy for detecting pedicle screw violations in the thoracic and lumbar spine. Neurosurgery. 2004;54:1138–1142. doi: 10.1227/01.NEU.0000119330.70023.8F. [DOI] [PubMed] [Google Scholar]
- 31.Zdichavsky M, Blauth M, Knop C, Graessner M, Hermann H, Krettek C, Bastian L. Accuracy of pedicle screw placement in thoracic spine fractures. Part I: inter- and intraobserver reliability of the scoring system. Eur J Trauma. 2004;30:234–240. doi: 10.1007/s00068-004-1422-9. [DOI] [Google Scholar]
- 32.Zdichavsky M, Blauth M, Knop C, Lotz J, Krettek C, Bastian L. Accuracy of pedicle screw placement in thoracic spine fractures. Part II: a retrospective analysis of 278 pedicle screws using computed tomographic scans. Eur J Trauma. 2004;30:241–247. doi: 10.1007/s00068-004-1423-8. [DOI] [Google Scholar]