Abstract
Dynamic stabilisation system for the spine (Dynesys) relies on titanium screw purchase within the pedicle. Decision on osseointegration is important especially when the patient becomes symptomatic following initial good outcome. Loose screws make the construct non-functional especially in symptomatic patients. Removal of Dynesys may become necessary to control patient’s symptoms. In this study, we report interobserver reliability of X-ray for the interpretation of Dynesys pedicle screw osseointegration based on the diagnosis of “halo zone” and “Double halo zones” surrounding loose screw. Lumbar spine X-ray images of 50 patients in two views (AP and lateral) were selected from a random sample of 420 Dynesys patients. The total number of pedicle screws reviewed in this study was 260. The investigators (observers) were asked to state whether or not each pedicle screw is loose using “radiolucent zone sign”. Observers were two expert orthopaedic spine consultant surgeons and one expert consultant radiologist and four specialist registrars (SpR) in orthopaedics and radiology. SpR assessments were repeated after 4 months with instructions to use “double-halo sign” for loose screws. The evaluation of interobserver agreement was performed by obtaining a Kappa (K) index. Using “radiolucent zone sign”, Kappa Index (KI) among three consultants was 0.2198 at 95% CI (0.0520, 0.4916) while for all of the seven assessors (3 consultants and 4 SpR), KI was 0.1462 at 95% CI (0.0332, 0.2592). The use of “double-halo sign” was associated with KI of 0.666 at 95% CI (SE 0.83) among all of the 4 SpR. Based on plain X-ray “radiolucent zone sign”, the inter-observer reliability of detecting loose Dynesys pedicle screw was poor (Kappa index of 0.2). On the other hand, using plain X-ray “double-halo sign” was associated with improved inter-observer reliability and validity.
Keywords: Pedicle fixation, Lumbar spine, Dynesys
Introduction
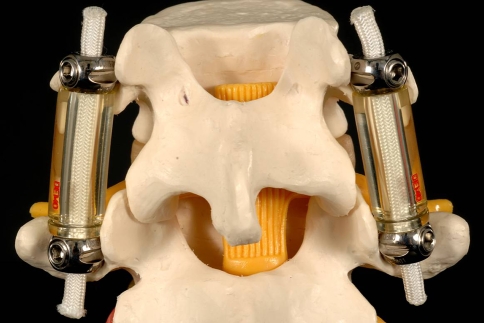
Dynesys® (Fig. 1) is designed to off-load the diseased spinal segment [36] while maintaining a controlled movement at the treated disc level(s) [26]. It is a pedicle screw construct. On each side of the spine, screws are joined through flexible cord (made of Sulene polyethylene terephthalate) and flexible spacers (made of polycarbonate urethane). There is no cross link between the two sides.
Fig. 1.
Dyensys® implant consists of: titanium pedicle screws, cords and spacers
Dynesys pedicle screws (Fig. 2) are made of titanium alloy (Protasul®100) and since 2002, Hydroxyapatite (HA) coated screws were made available. The screws are self-tapping and are conical in shape. Different sizes are available; the smallest is 5.2 cm (length) × 35 mm (cross section) and the largest is 8.0 cm × 55 mm. Placement of screw can be subfacetal (in posterior approach surgery) or screws can be positioned lateral to the facet joints (in posterolateral approach) [5]. The manufacturer recommended posterolateral approach with screws placed lateral to facet joints.
Fig. 2.

Dynesys HA coated pedicle screw
Dynesys was successful in controlling symptoms associated with degenerative disc disease as shown by a previous papers by the same authors [6, 7]. Early clinical outcome was also promising in the Food and Drug Administration (FDA) trial [47]. Bordes-Monmeneu et al. [2] reported a reduction of 35 points in Oswestry Disability Index (ODI) following the application of Dynesys in 94 patients for a period of 14–24 months.
Being a pedicle screw system, the construct loading may force the screws to move within the pedicle and loose their bone-purchase. Reports on the incidence of loose pedicle screw based on “halo zone sign” vary in the literature and depends on the interpreter’s experience (3.6–17%) [12, 15, 37, 41]. Similarly, loosening within pedicle screw lumbosacral fusion is reported [28]. Some studies were associated with interestingly high rates than others. Ohlin et al. (1994) [27] reported an incidence of 20.8% in his series of 153 patients.
Identifying symptomatic loose screws is important. A loose pedicle-dependant construct may move with spinal movements and trigger painful paraspinal muscle spasms. The decision to subject the patient for a second surgery with or without reinstrumentation must be evaluated carefully. Conventional plain X-rays are relatively easy to obtain. Standard AP and Lateral views are helpful. However, these views are limited with the information they provide.
Early diagnosis of screw loosening can save the patient not only painful spasms but also late macromovements and possible serious neural damage or screw breakage [23, 29, 30].
On the other hand, asymptomatic metal failure (loosening or breakage) may not need more than monitoring. Schnake et al. [37] reviewed 26 patients and showed that implant failure in four patients was not related to patient satisfaction or back pain.
In this study, we are have challenged our assessors to make a diagnosis on loose pedicle screws based on the identification of two signs; namely “halo zone sign” and “double-halo sign”.
Material and methods
Lumbar spine X-ray images of 50 patients in two views (AP and lateral) were selected from our prospective cohort of 420 patients. Patients’ data was presented on excel spreadsheet format from when we first used Dynesys (September 2000) until now. For the purpose of this study, we decided to choose an end point as (June 2008). Clinical data collection is ongoing for the rest of the cohort.
Simple randomisation was achieved through computerised random number generator (RNG) method. Patients were operated on and followed up at the Conquest Hospital in Hastings, UK.
The study was approved by the Committee on Ethics in Research of the hospital.
Anterioposterior and lateral radiographs were obtained from the digital PACS® radiographic imaging review system. Each view was magnified and the contrast was adjusted to obtain the best accurate image. Images then saved as JPEG files with an average size of 85 K byte. Each photograph showed no more than three vertebral levels and their corresponding pedicle screws. Additional images were made to show vertebra/screws if they exceeded three levels. Authors were made aware of any additional pictures. Pictures were then coded alphabetically and the file name was amended to include AP or Lateral views with further images if present. Photos were deployed onto a CD-ROM and distributed among observers. All of the seven reviewers were supplied with scoring sheets to record their results.
For the first part of this study, the investigators were asked to state whether or not each pedicle screw is loose (total of 260 pedicle screws) based on the presence of “a radiolucent halo zone sign” surrounding suspicious screws. In AP views, a lucent ring surrounding the screw is considered “halo zone” and it is confirmed in lateral view as tracking line along part or the entire length of the screw. Assessors were made aware of the possible silhouette shadow of bowel gases. All of the 260 screws were evaluated independently by all of the seven observers.
Observers were composed of seven physicians; two expert orthopaedic spine consultant surgeons, one expert consultant radiologist with special interest in musculoskeletal radiology and four specialist registrars (SpR trainees) in orthopaedic surgery and radiology. SpRs were in their 3rd–4th year of specialist training programme and they spent at least three months with the two “expert” consultants doing Dynesys. Consultants were considered “experts”, while Specialist Registrars were considered “trainees”.
Four months later, all of the four SpR(s) were asked to repeat their assessment using “double-halo sign” for the diagnosis of loose screws. “Double-halo” was described as a radiolucent rim surrounding the screw which is framed by rim of radio-opique dense bone trabiculae.
Statistical methods
The evaluation of interobserver agreement was performed by obtaining a Kappa index (KI). For continuous variables comparison, the Fisher’s exact test was employed, with a significance level of 0.05.
Z value at CI 95% was used to compare the significance in specificity of both signs.
Results
“Halo zone sign”
Table 1 shows the proportions of loose screws identified by each of the seven evaluators based on their interpretation of the X-ray films. The mean number of screws identified as being loose by experts was 11 (i.e. 4.2% of screws), while the mean number of loose screws identified by trainees was 59.3 (i.e. 23%).
Table 1.
Percentage of loose screws based on “halo zone sign”
| Assessors | Numbera (percentage) |
|---|---|
| Observer 1 (consultant) | 9 (3.4%) |
| Observer 2 (consultant) | 11 (4.2%) |
| Observer 3 (consultant) | 13 (5%) |
| Observer 4 (specialist registrar) | 9 (3.4%) |
| Observer 5 (specialist registrar) | 56 (21.7%) |
| Observer 6 (specialist registrar) | 59 (22.8%) |
| Observer 7 (specialist registrar) | 113 (43.7%) |
ªNumbers and percentages out of 260 X-ray pictures of screws
Table 2 shows that the Kappa Index among three experts was 0.2198 at 95% CI (0.0520–0.4916) while for all of the seven assessors (3 Experts and 4 trainees), Kappa index was 0.1462 at 95% CI (0.0332–0.2592).
Table 2.
Percentage of Kappa index for pedicle screw loosening based on “halo zone sign”
| Kappa/CI | 3 Experts | 3 Experts and 4 SpR |
|---|---|---|
| Kappa index | 0.2198 | 0.1462 |
| 95% confidence interval | CI (−0.0520, 0.4916) | CI (0.0332, 0.2592) |
“Double-halo sign”
Table 3 reports the incidence of screw loosening based on “double- halo sign”. The mean number for all of the four assessors for was 8.5%.
Table 3.
Percentage of loose screws based on “double-halo sign”
| Assessors | Numbera (percentage) |
|---|---|
| Observer 4 (specialist registrar) | 19 (7.3%) |
| Observer 5 (specialist registrar) | 22 (8.4%) |
| Observer 6 (specialist registrar) | 24 (9.2%) |
| Observer 7 (specialist registrar) | 24 (9.2%) |
ªNumbers and percentages out of 260 X-ray pictures of screws
Table 4 shows the Kappa Index among the same four trainees after changing the instructions. KI was 0.666 at 95% CI (0.496–0.836), SE 0.83.
Table 4.
Percentage of Kappa index for pedicle screw loosening based on “double-halo sign”
| Kappa/CI | 4 SpR |
|---|---|
| Kappa index (95% confidence interval) | 0.666 |
| Standard error | 0.83 |
Table 5 indicates that “Double halo sing” has more specificity for the diagnosis of loose screws than “halo zone sign”.
Table 5.
Both signs are sensitive for the diagnosis, however; “Double halo sign” has more specificity for the diagnosis of loose screws than “halo zone sign”
| Sensitivity | Specificity | Positive predictive value | Negative predictive value | |
|---|---|---|---|---|
| Halo zone sign | 1 | 0.8047 | 0.155 | 1 |
| Double Halo sign | 1 | 0.940 | 0.375 | 1 |
Specificity difference was significant with Z value of 4.604 at CI 95%. Predictive values are low because of the low incidence of screw loosening among the patients cohort
Table 6; based on the assessment of the senior orthopaedic consultant surgeon, overall incidence was 3.4%. Table shows the breakdown of loose versus non-loose for both HA and non-HA screws. Average time to X-ray follow up following surgery was 40.9 months (range from 20 to 74 months). In October 2002, we have moved away from non-HA coated screws because of the potential risk of loosening.
Table 6.
Based on the assessment of the senior orthopaedic consultant surgeon, overall incidence was 3.4%
| HA coated | Non-HA coated | Total | |
|---|---|---|---|
| Loose screw | 3 | 6 | 9 |
| Not loose | 41 | 0 | 41 |
| Total | 44 | 6 | 50 |
Table shows the breakdown of loose versus non-loose for both HA and Non-HA screws
Discussion
“Halo zone sign” analysis: Interobserver Error
The first part of this study showed poor agreement between all observers (Kappa Index 0.1462) see Table 7 also for reference [20]. Even at expert’s level, agreement was not satisfactory to be regarded as reliable (KI 0.2198). Authors were not sure whether the halo surrounding a pedicle screw was anything but the bowel gas shadow interface. Different angles of projection of screws added to the difficulty in making the diagnosis on AP views especially when Wiltse approach was used during surgery. Lateral radiographs were used for confirmation whereas the AP views were useful for initial diagnosis.
Table 7.
Interpretation of Landis and Koch (1977) [20]
| Kappa index | Agreement |
|---|---|
| 0.00 | Less than chance |
| 0.00–0.20 | Slight |
| 0.21–0.40 | Fair |
| 0.41–0.60 | Moderate |
| 0.61–0.80 | Substantial |
| 0.81–1.00 | Almost perfect |
“Double-halo sign” analysis:
In the second phase and when the study was repeated at trainee level, KI was improved significantly. Agreement on loose screws was considered substantial (KI 0.666) Table 6 [20]. Authors were more confident to comment on loose pedicle screw when the immediate radiolucent zone was surrounded by a rim of radiopque dense bone trabiculae. This sign was more reliable and its specificity was significantly superior than halo-zone sign (Z value 4.604 at CI 95%) Table 7.
Effect of examiners’ experience and specialty
Trainee reported loose screws in as much as five times as the expert observers when using “halo zone sign” 23, 4.2% respectively. This was statistically significant (P < 0.05).
The senior radiologist reported a higher figure than both orthopaedic senior authors; 5, 4.2 and 3. 4%, respectively. However; this was not statistically significant (P > 0.05).
Pedicle screw fixation
Approximately 60% of screw fixation strength in the lumbar region is in the pedicle while the cancellous bone within the vertebral body adds no more than 15–20% of strength. On some occasions, the benefits outweigh the risks and advancing the screw to the anterior vertebral cortex offers 20-25% strength [46, 50]. Whereas in the sacral area, the anterior cortex contributes to 60% of the overall screw strength.
Factors influence screw purchase
There are multiple factors which may affect screw purchase directly or indirectly. Some of them are related to screws’ thread design, shape, length, cross-section size or surface roughness. Other factors are related to bone-implant interface e.g., using enhancers like HA or bone cement. Some other factors are generic and may be related to patients themselves, e.g. osteoporosis (see Table 8).
Table 8.
Factors influence screw purchase in DDD
Screw failure
One of the major disadvantages of pedicle screw system is late onset backpain. Lonstein et al. [22] examined a total of 879 patients (total screws were 4,790) with rigid pedicle screw fusion. Of which 1,102 screws (23%) were removed due to “pseudarthrosis” or “pain related to instrumentation”. Being a pedicle construct, Dynesys patient might encounter postoperative pain [8]. Persistent pain should be investigated to exclude malposition of screws (1–12.9% of patients) [2, 12, 15, 41], recurrence of disease (21% of patients) [37], infection (1.2–3.2%) [2, 15, 41] metal breakage or loosening (12–19% of patients) [15, 37, 41]. Symptoms may arise from the adjacent spinal segments and it must be investigated as it may require surgical treatment (2.5–29% of patients) [12, 37, 41].
In some patients no cause can be identified for patients’ backpain (8%) [37]. Some surgeons might blame it to “instrumentation” [22] while others believe it is attributed to poor osseointegration of metal screw within the pedicle [38] and leaves the spinal construct dysfunctional.
Poor screw anchor can results in micromotion at the distal end and in distraction construct, like Dynesys, this may lead to stress shielding. Lu et al. [24] found that cyclic loading with 30% of the yield load of human vertebrae significantly increased microcrack density in the vertebral trabeculae at 20,000 cycles of loading but the vertebrae did not fail. This level of cyclic load may be insufficient to cause failure of the entire pedicle screw system in a vertebra but sufficient to cause damage in bone adjacent to the screw. In addition, Movement between screw threads and bone inhibits bone formation, revascularization and remodeling of dead bone. Movement causes the screw to become enveloped by fibrous tissue in response to necrosis and resorption of adjacent dead cortical bone [35]. This results in a radiologically discernible radiolucent “halo” about the screw, a certain sign of screw loosening [33, 35]. Eventually the distraction principle of the construct is lost.
It is rather difficult to predict which screws are going to be loose or which patients are more likely to become symptomatic. Similarly, there is no specific time scale to indicate the most crucial period.
Decision to take the screws out
Identifying symptomatic loose screws is important. A loose pedicle-dependant construct may move with spinal movements and trigger painful paraspinal muscle spasms. The decision to subject the patient for a second surgery with or without reinstrumentation must be evaluated carefully. Conventional plain X-rays are relatively easy to obtain. Standard AP and Lateral views are helpful. However, these views are limited with the information they provide. Our observers could not see a cross sectional view of all screws from a single AP projection due to different projections of the screws in axial and coronal planes. Making a comment on the “halo zone” surrounding all screws from a single AP view is not accurate. Similarly, on the lateral view, the two screws at the same vertebra may be superimposed on each other. The diagnosis of “halo zone” from the lateral radiograph is more difficult and less precise.
Quantifying the lucency is another challenge. Sandén et al. [33] used 1 mm width to differentiate thin and wide radiolucent zones disregarding the length of the lucency. Tokuhashi et al. [44] used 1 mm or greater circumferential lucency around a screw from two or more digitalized plain radiographic directions.
The scientific bases for choosing 1 mm as a cut-off point are not clear. In addition, magnification effects of digital radiographs must be taken into account. Calibration with the screw dimensions might be useful. Furthermore, radiolucency along the entire length of the screw is understandingly more important than isolated lucency around the tip of the screw where cancellous vertebral bone account for not more than 20% of screw strength in the lumbar vertebra [46, 50].
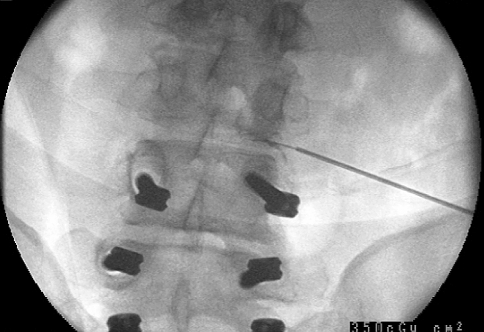
Authors of this study believe that 45° “oblique views” (Fig. 3) was not superior to standard AP view. In fact, a single oblique view necessitates almost double the radiation dose. To sum up, the radiation exposure for two oblique views was three times the standard radiation dose of a single “AP view” and it was unjustified for the low quality of information they provide.
Fig. 3.
Right and left 45° oblique views
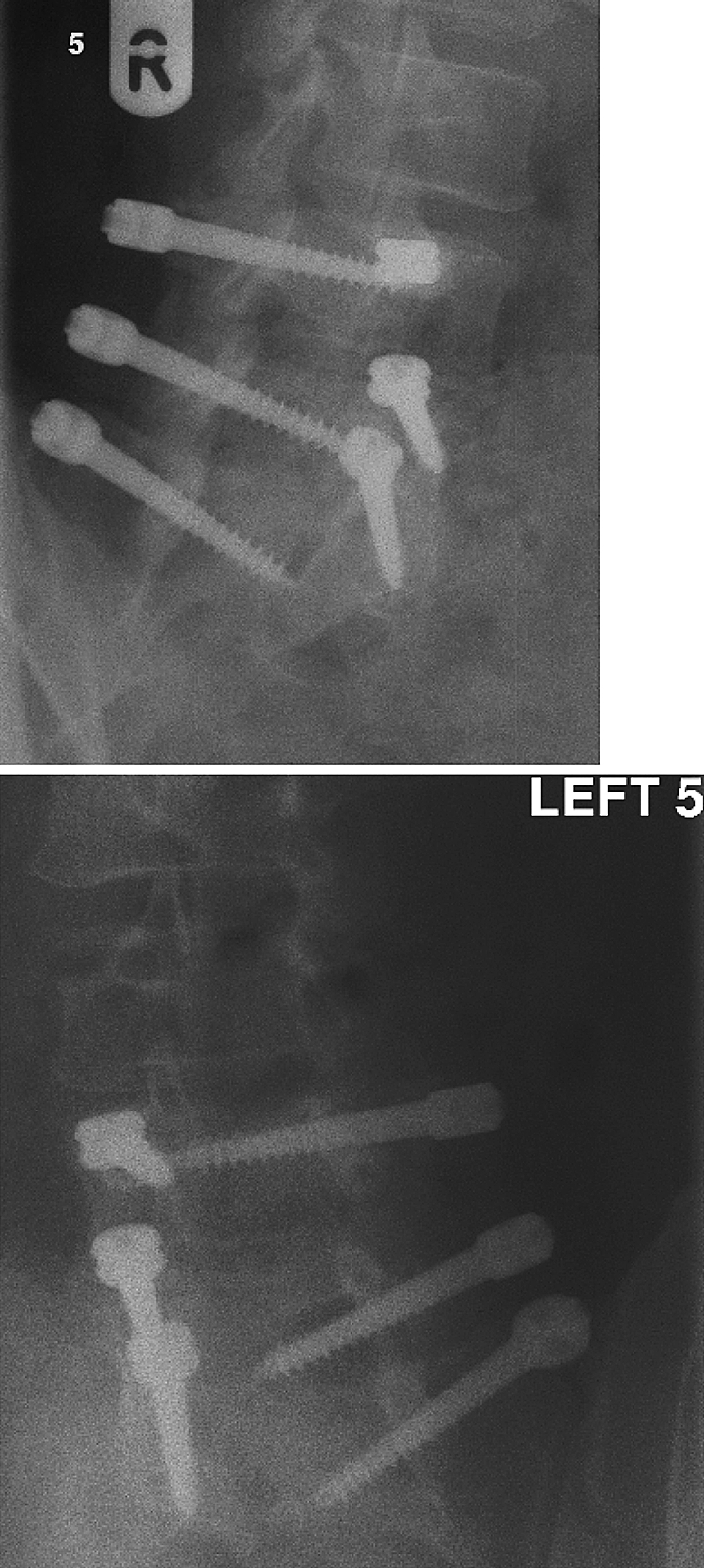
Current practice for the diagnosis at our Spinal Unit
The senior author of this paper prefers screening suspicious screws under direct fluoroscopic control at the surgical room. The C-arm can be adjusted to follow vertebral inclinations and face the screw’s head directly. The “double halo sign” can be identified much easier.
The difficulty with applying this diagnostic procedure is to all suspicious screws arises from the fact that it requires the availability of resources and expertise. It is best to combine visualisation of screws with another diagnostic or therapeutic procedures, e.g., spinal probe or caudal epidural injections (Figs. 4, 5, 6]
Fig. 4.
“Double halo sign” surrounding right L4 screw; inner radiolucent zone surrounded by an outer radio-opaque rim of dense bone trabeculae
Fig. 5.
Different screw projections with overlapping bowel gas shadow make “radiolucent zone” difficult to interpret
Fig. 6.
loose right L4 and right L5 screws confirmed by fluoroscopy. A spinal probe was applied in the same time for L3–L4 disc level
Measures to reduce screw loosening
Improving screw-bone bonding was the target for many studies [13, 16, 31, 32, 34, 39, 42, 45, 48, 49]. The most successful among these was the use of plasma-sprayed HA screws [13, 16, 32, 34, 45, 49]. Osteoblast adhesion and differentiation is enhanced when bioactive titanium implant is used in comparison to titanium alone [49]. The bone-implant interface was different from mineralizing bone matrix or osteoid. Histologicaly, the interface was rich in proteoglycans and glycoproteins [3, 10, 11]. In addition, osteoblastic matrix proteins such as osteopontin and alpha HS—glycoprotein has been demonstrated to facilitate interface synthesis [17, 25].
Hydroxyapatite coating can increase surface area which improves the biomechanics as well as the load bearing capacity of the structure. HA has been shown to decrease corrosion rates and accelerate the rate of bone formation and maturation [1, 43]. HA-bone interface exhibit more organised bone pattern and a superior degree of mineralisation than for other materials. The bone-HA interface has been proven to be stronger than the HA-implant interface [1, 43].
Limitations of this study
The difference in KI reliability for the second study might be related to more careful interpretation of loose screw. It is difficult to disprove it in the absence of intraobserver record of the first study.
The second review involved only trainees. It would be of greater significance to involve all of the seven assessors.
Conclusion
The Inter-observer reliability of detecting loose Dynesys pedicle screw using “double-halo sign” was associated with improved inter-observer reliability and validity. We suggest using “double halo sign” to describe established loose pedicle screw.
Acknowledgment
For Guy R, Selmon G, Bowman N, Shah D, El-Metwally A for their contribution in this study.
Conflict of interest statement None.
References
- 1.Block MS, Kent JN, Kay JF. Evaluation of hydroxylapatite-coated titanium dental implants in dogs. J Oral Maxillofac Surg. 1987;45:601–607. doi: 10.1016/0278-2391(87)90270-9. [DOI] [PubMed] [Google Scholar]
- 2.Bordes-Monmeneu M, Bordes-Garcia V, Rodrigo-Baeza F, Saez D. A dynamic neutralisation system for the spine. DYNESYS SYSTEM. Experience in 94 cases. Neurosurgery. 2005;16:499–506. [PubMed] [Google Scholar]
- 3.Clokie CML, Warshawky H. Morphologic and radioauto-graphic studies of bone formation in relation to titanium implants using rat tibia as a model. Int J Oral Maxillofac Implants. 1995;10:155–165. [PubMed] [Google Scholar]
- 4.Cook SD, Salkeld SL, Whitecloud TS, et al. Biomechanical evaluation and preliminary clinical experience with an expansive pedicle screw design. J Spinal Disord. 2000;13:230–236. doi: 10.1097/00002517-200006000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Dakhil-Jerew F, Shepperd J (2008) Outcome following posterior vs. Wiltse approaches to Dynesys. Abstract, Japanese Orthopaedic Association Congress, Sapporo, Japan. May 2008
- 6.Dakhil-Jerew F, Shepperd J (2007) Outcome following Dynesys for the treatment of degenerative disc disease. Abstract. European Association of Neurosurgical Societies (EANS) Conference, Glasgow. 4th September 2007. Acta Neurochiurgica: PLIV
- 7.Dakhil-Jerew F, Shepperd J (2007) Refinement of the clinical indications for the Dynamic Neutralisation System for the Spine. Abstract, British Orthopaedic Research Society. Manchester, 2008
- 8.Dakhil-Jerew F, Shepperd J. (2007) Functional outcome following removal of Dynnesys. British Orthopaedic Research Society meeting, Dundee 2nd July 2007
- 9.DeCoster TA, Heetderks DB, Downey DJ, et al. Optimizing bone screw pullout force. J Orthop Trauma. 1990;4:169–174. doi: 10.1097/00005131-199004020-00012. [DOI] [PubMed] [Google Scholar]
- 10.Lange G, Putter C. Structure of the bone interface to dental implants in vivo. J Oral Implantol. 1993;19:123–135. [PubMed] [Google Scholar]
- 11.Lange GL, Putter C, Wijs FLJA. Histological and ultrastructural appearance of the hydroxyapatite-bone interface. J Biomed Mater Res. 1990;24:829–845. doi: 10.1002/jbm.820240704. [DOI] [PubMed] [Google Scholar]
- 12.Dubois B, Germay B, Schaerer NS, Fennema P. Dynamic neutralization: a new concept for restabilization of the spine. Philadephia: Lippincott Williams & Wilkins; 1999. [Google Scholar]
- 13.Fini M, Giavaresi G, Greggi T, Martini L, Aldini NN, Parisini P, Giardino R. Biological assessment of the bone-screw interface after insertion of uncoated and hydroxyapatite-coated pedicular screws in the osteopenic sheep. J Biomed Mater Res A. 2003;66(1):176–183. doi: 10.1002/jbm.a.10605. [DOI] [PubMed] [Google Scholar]
- 14.Gila FJ, Padrosb A, Maneroa JM, et al. Growth of bioactive surfaces on titanium and its alloys for orthopaedic and dental implants. Barcelona, Spain: Universidad Politecnica de Cataluna; 2001. [Google Scholar]
- 15.Grob D, Benini A, Junge A, Mannion AF. Clinical experience with the Dynesys semirigid fixation system for the lumbar spine: surgical and patient-oriented outcome in 50 cases after an average of 2 years. Spine. 2005;30(3):324–331. doi: 10.1097/01.brs.0000152584.46266.25. [DOI] [PubMed] [Google Scholar]
- 16.Hasegawa T, Inufusa A, Imai Y, Mikawa Y, Lim TH, An HS. Hydroxyapatite-coating of pedicle screws improves resistance against pull-out force in the osteoporotic canine lumbar spine model: a pilot study. Spine J. 2005;5(3):239–243. doi: 10.1016/j.spinee.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 17.Kawaguchi H, McKee MD, Okamoto H, Nanci A. Immunocytochemical and lectin-gold characterization of the interface between alveolar bone and implanted hydroxyapetite in the rate. Cells Mater. 1993;3:337–358. [Google Scholar]
- 18.Krag MH, Beynnon BD, Pope MH, et al. An internal fixator for posterior application to short segments of the thoracic, lumbar or lumbosacral spine: design and testing. Clin Orthop Relat Res. 1986;203:75–98. [PubMed] [Google Scholar]
- 19.Kwok AW, Finkelstein JA, Woodside T, et al. Insertional torque and pull-out strengths of conical and cylindrical pedicle screws in cadaveric bone. Spine. 1996;21:2429–2434. doi: 10.1097/00007632-199611010-00004. [DOI] [PubMed] [Google Scholar]
- 20.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 21.Lapresle P, Missenard G. Hydroxyapatite-coated Diapason screws: first clinical report. J Spinal Disord. 1995;8:31–39. [PubMed] [Google Scholar]
- 22.Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB. Complications associated with pedicle screws. JBJS. 1999;81(11):1519–1528. doi: 10.2106/00004623-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Louis R. Fusion of the lumbar and sacral spine by internal fixation with screw plates. Clin Orthop Relat Res. 1986;203:18–33. [PubMed] [Google Scholar]
- 24.Lu WW, Luk KD, Cheung KC, Gui-Xing Q, Shen JX, Yuen L, Ouyang J, Leong JC. Microfracture and changes in energy absorption to fracture of young vertebral cancellous bone following physiological fatigue loading. Spine. 2004;29(11):1196–1201. doi: 10.1097/00007632-200406010-00007. [DOI] [PubMed] [Google Scholar]
- 25.Nanci A, McCarthy GF, Zalzal S, Clokie CML, Warshawsky H, McKee MD. Tissue response to titanium implants in the rat tibia: ultrastructural, immunocytochemical and lectin-cytochemical characterization of the bone-titanium interface. Cells Mater. 1994;4:1–30. [Google Scholar]
- 26.Niosi CA, Zhu QA, Wilson DC, Keynan O, Wilson DR, Oxland TR. Biomechanical characterization of the three-dimensional kinematic behaviour of the Dynesys dynamic stabilization system: an in vitro study. Eur Spine J. 2006;15:913–922. doi: 10.1007/s00586-005-0948-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ohlin A, Karlsson M, Duppe H, et al. Complications after transpedicular stabilization of the spine: a survivorship analysis of 163 cases. Spine. 1994;19:2774–2779. doi: 10.1097/00007632-199412150-00007. [DOI] [PubMed] [Google Scholar]
- 28.Pihlajamaki H, Myllynen P, Bostman O. Complications of transpedicular lumbosacral fixation for non-traumatic disorders. J Bone Joint Surg Br. 1997;79-B:183–189. doi: 10.1302/0301-620X.79B2.7224. [DOI] [PubMed] [Google Scholar]
- 29.Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986;203:7. [PubMed] [Google Scholar]
- 30.Steffee AD, Biscup RS, Sitkowski DJ. Segmental spine plates with pedicle screw fixation. A new internal fixation device for disorders of the lumbar and thoracolumbar spine. Clin Orthop Relat Res. 1986;203:45. [PubMed] [Google Scholar]
- 31.Renner SM, Lim TH, Kim WJ, Katolik L, An HS, Andersson GB. Augmentation of pedicle screw fixation strength using an injectable calcium phosphate cement as a function of injection timing and method. Spine. 2004;29(11):E212–E216. doi: 10.1097/00007632-200406010-00020. [DOI] [PubMed] [Google Scholar]
- 32.Sandén B, Olerud C, Larsson S. Hydroxyapatite coating enhances fixation of loaded pedicle screws: a mechanical in vivo study in sheep. Eur Spine J. 2001;10(4):334–339. doi: 10.1007/s005860100291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sandén B, Olerud C, Petrén-Mallmin M, Johansson C, Larsson S. The significance of radiolucent zones surrounding pedicle screws. Definition of screw loosening in spinal instrumentation. J Bone Joint Surg Br. 2004;86(3):457–461. doi: 10.1302/0301-620X.86B3.14323. [DOI] [PubMed] [Google Scholar]
- 34.Sandén B, Olerud C, Petrén-Mallmin M, Larsson S. Hydroxyapatite coating improves fixation of pedicle screws. A clinical study. J Bone Joint Surg Br. 2002;84(3):387–391. doi: 10.1302/0301-620X.84B3.12388. [DOI] [PubMed] [Google Scholar]
- 35.Schatzker J, Horne JG, Sumner-Smith G. The effect of movement on the holding power of screws in bone. Clin Orthop Relat Res. 1975;111:257–262. doi: 10.1097/00003086-197509000-00032. [DOI] [PubMed] [Google Scholar]
- 36.Schmoelz HuberJ, Nydegger T, Claes L, Wilke H. Influence of a dynamic stabilization system on load bearing of a bridged disc: an in vitro study of intradiscal pressure. Eur Spine J. 2006;15(8):1276–1285. doi: 10.1007/s00586-005-0032-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schnake KJ, Schaeren S, Jeanneret B. Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine. 2006;31(4):442–449. doi: 10.1097/01.brs.0000200092.49001.6e. [DOI] [PubMed] [Google Scholar]
- 38.Sell P, Collins M, Dove J. Pedical screws: axial pull-out strength in the lumbar spine. Spine. 1988;13:1075–1076. doi: 10.1097/00007632-198809000-00018. [DOI] [PubMed] [Google Scholar]
- 39.Shepard MF, Wang JC, Oshtory R, Yoo J, Kabo JM. Enhancement of pedicle screw fixation through washers. Clin Orthop Relat Res. 2002;395:249–254. doi: 10.1097/00003086-200202000-00030. [DOI] [PubMed] [Google Scholar]
- 40.Sidhu KS, Herkowitz HN. Spinal instrumentation in the management of degenerative disorders of the lumbar spine. Clin Orthop Relat Res. 1997;355:39–53. [PubMed] [Google Scholar]
- 41.Stoll TM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine: a multi-center study of a novel non-fusion system. Eur Spine J. 2002;11(Suppl 2):S170–S178. doi: 10.1007/s00586-002-0438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Taniwaki Y, Takemasa R, Tani T, Mizobuchi H, Yamamoto H. Enhancement of pedicle screw stability using calcium phosphate cement in osteoporotic vertebrae: in vivo biomechanical study. J Orthop Sci. 2003;8(3):408–414. doi: 10.1007/s10776-003-0639-6. [DOI] [PubMed] [Google Scholar]
- 43.Thomas KA, Kay JF, Cook SD, et al. Effect of surface microstructure and hydroxylapatite coating on the mechanical strengths and histologic profiles of titanium implantmaterials. J Biomed Mater Res. 1987;21(12):1395–1414. doi: 10.1002/jbm.820211205. [DOI] [PubMed] [Google Scholar]
- 44.Tokuhashi Y, Matsuzaki H, Oda H, Uei H. Clinical course and significance of the clear zone around the pedicle screws in the lumbar degenerative disease. Spine. 2008;33(8):903–908. doi: 10.1097/BRS.0b013e31816b1eff. [DOI] [PubMed] [Google Scholar]
- 45.Turner AW, Gillies RM, Svehla MJ, Saito M, Walsh WR. Hydroxyapatite composite resin cement augmentation of pedicle screw fixation. Clin Orthop Relat Res. 2003;406:253–261. doi: 10.1097/00003086-200301000-00036. [DOI] [PubMed] [Google Scholar]
- 46.Weinstein JN, Rydevik BL, Rauschning W. Anatomic and technical considerations of pedicle screw fixation. Clin Orthop Relat Res. 1992;284:34–46. [PubMed] [Google Scholar]
- 47.Welch WC, Cheng BC, Awad TE, Davis R, Maxwell JH, Delamarter R, Wingate JK, Sherman J, Macenski MM. Clinical outcomes of the Dynesys dynamic neutralization system: 1-year preliminary results. Neurosurg Focus. 2007;22(1):E8. doi: 10.3171/foc.2007.22.1.8. [DOI] [PubMed] [Google Scholar]
- 48.Yazu M, Kin A, Kosaka R, Kinoshita M, Abe M. Efficacy of novel-concept pedicle screw fixation augmented with calcium phosphate cement in the osteoporotic spine. J Orthop Sci. 2005;10(1):56–61. doi: 10.1007/s00776-004-0862-8. [DOI] [PubMed] [Google Scholar]
- 49.Yildirim OS, Aksakal B, Hanyaloglu SC, Erdogan F, Okur A. Hydroxyapatite dip coated and uncoated titanium poly-axial pedicle screws: an in vivo bovine model. Spine. 2006;31(8):E215–E220. doi: 10.1097/01.brs.0000210221.00778.c7. [DOI] [PubMed] [Google Scholar]
- 50.Zindrick MR, Wiltse LL, Doornik A, Widell EH, Knight GW, Patwardhan AG, Thomas JC, Rothman SL, Fields BT. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine. 1987;12(2):160–166. doi: 10.1097/00007632-198703000-00012. [DOI] [PubMed] [Google Scholar]