Abstract
The insufficient investigations on the changes of spinal structures during traction prevent further exploring the possible therapeutic mechanism of cervical traction. A blind randomized crossover-design study was conducted to quantitatively compare the intervertebral disc spaces between axial and anterior lean cervical traction in sitting position. A total of 96 radiographic images from the baseline measurements, axial and anterior lean tractions in 32 asymptomatic subjects were digitized for further analysis. The intra- and inter-examiner reliabilities for measuring the intervertebral disc spaces were in good ranges (ICCs = 0.928–0.942). With the application of anterior lean traction, the statistical increases were detected both in anterior and in posterior disc spaces compared to the baseline (0.29 mm and 0.24 mm; both P < 0.01) and axial traction (0.16 mm and 0.35 mm; both P < 0.01). The greater intervertebral disc spaces obtained during anterior lean traction might be associated with the more even distribution of traction forces over the anterior and posterior neck structures. The neck extension moment through mandible that generally occurred in the axial traction could be counteracted by the downward force of head weight during anterior lean traction. This study quantitatively demonstrated that anterior lean traction in sitting position provided more intervertebral disc space enlargements in both anterior and posterior aspects than axial traction did. These findings may serve as a therapeutic reference when cervical traction is suggested.
Keywords: Axial traction, Anterior lean traction, Intervertebral disc space, Image analysis
Introduction
One of the main function of the intervertebral disc is to damp the compressive loadings during daily activities. Disc injury or degeneration could lead to mechanical compression or chemical irritation of the nerve root causing neurological deficits [9, 18]. Spinal traction is generally regarded as a conservative management in treating various types of neck or back disorders. Several mechanisms have been proposed for the possible therapeutic effects of traction [5, 10, 17, 21, 27, 28, 36]. DeLacerda et al. [5] reported that the axial traction reduced pain by improving circulation or preventing adhesions and contractures of spinal structures. Spinal traction could widen the intervertebral disc space reflecting a stretching of the posterior longitudinal ligaments. This condition might be associated with the suction effect of the negative intradiscal pressure and the pushing effect of the posterior longitudinal ligaments [21, 27]. Wong et al. [36] observed that the traction significantly decreased the electromyographic activity of paraspinal muscles during the whole traction phase. Krause et al. [17] concluded that the separation of vertebrae by increasing the diameter of intervertebral foramen could reduce radicular pain and normalize neurological deficits by relieving direct pressure or contact forces in the sensitized neural tissues. Although the exact mechanisms for pain relief and function recovery are still controversial, the generally recognized biomechanical effects of cervical traction are to enlarge the intervertebral disc spaces around foramen levels and tighten the posterior longitudinal ligament [17, 21, 27, 28, 36].
The intervertebral disc was reported to decrease its space and lead to the disc degeneration if the duration and extent of spinal compressive loadings exceeded the physiological set point [18, 23]. The decrease in the intervertebral disc space would constrict the intervertebral foramen sufficiently to cause entrapment or compression of the spinal nerve root. A 1 mm narrowing of the intervertebral disc space was reported to correspond to a reduction of 20–30% in the foraminal area [23]. In contrast, the long-term axial distraction could separate the intervertebral disc space and induce the signs of disc tissue recovery on biological and biomechanical levels [19]. Although several studies have assessed the traction effects determined by clinical pain as well as disability scales, or signs of neurological deficits [2, 24, 26], the associated underlying changes of spinal structures need to be investigated for a better understanding of the possible therapeutic mechanisms.
Cervical traction is usually administered with patients in supine or sitting position and the previous studies related to clinical applications mainly focused on the supine position [1, 3, 4, 13, 37]. Deets et al. [4] pointed out that the head weight in supine position was eliminated, thereby increasing the efficiency of cervical traction compared to that in the sitting posture. On the other hand, some researches reported high cervical myoelectric activity and untoward cardiovascular reactions especially in elderly patients and patients with unstable cardiovascular systems during the supine traction procedure [1, 13]. Wong et al. [36] reported a significant decrease in paraspinal muscle activity during sitting traction with a rope angle of 25°. The distribution of forces in cervical traction was documented to have a better efficacy with the neck flexion ranging from 20 to 35° [3, 27, 30, 37]. Lee and Evans [21] noted that a flexion moment produced during the spinal traction should not be overlooked. This flexion moment could lead to an increase in the posterior disc height, which in turn could increase the tension of the posterior annular fibers and the posterior longitudinal ligament to obtain a better traction effect. However, the insufficient investigations on the changes of spinal structures prevent the further explorations on the possible therapeutic mechanism of cervical traction. Therefore, the purpose of this study was to quantitatively compare the changes on the intervertebral disc spaces between axial and anterior lean cervical tractions in sitting position.
Methods
This blind, randomized crossover-design study was approved by the ethics committee on human research of a medical center. Thirty-two healthy adult subjects (13 males and 19 females) without neck disorder symptoms participated in this study. Subjects were excluded if they had history of cervical trauma or surgery, bone pathology, arthritic or other articular inflammatory disorders, pregnancy, and restrictive muscle spasm. The experimental procedures and potential risks were fully explained to each subject and signed informed consent was obtained.
All subjects received 20-min hot packs and then the lateral radiographs of cervical spine were collected in the sitting position for baseline measurements. A crossover research design was adopted to ensure no possibility of covariate imbalance or selection bias. After baseline radiographic evaluations, 32 subjects were randomly divided into two groups according to individual identification numbers for receiving different sequences of traction methods described below. A cervical traction machine system (Integ-trac 920, Ever Prosperous Instrument, Inc., Taipei, Taiwan) was set up in the radiographic room for radiographic assessments before and at the end of tractions. The head harness with metal support rings included two leather straps offering the chin and occiput supports during cervical traction. Previous researches suggested that traction forces of 11–16 kg were necessary to elicit a measurable change in cervical spine structures [3, 32, 36, 37]. The sustained traction was usually applied to the disc herniation patients with a time period from 2 to 20 min depending on their conditions, and the 3–5 min was often suggested for the first treatment [22, 32, 34]. Therefore, the cervical traction force was adjusted to 25% of individual body weight for a 5 min continuous traction in our experiments.
Group A
Subjects assigned to this group received the seated axial traction first with neck in neutral position. The rope angle was set at 0° (vertical plane) for a 5-min sustained traction. The second lateral radiograph of cervical spine was collected just before the end of traction. After a 3-day washout period, these subjects were arranged to receive the 20-min hot packs for the preparation of anterior lean traction. The rope angle was adjusted to 20° relative to the vertical plane by the goniometer reading and the subjects were in anterior leaned posture on a custom-made chair. The adjustable sternum and forearm supports prevented the spine from going into a slump posture during traction (Fig. 1). The pivot points of anterior leaned trunk were mainly at hip joints, and subjects were asked to maintain their neck in neutral position. During the traction procedure, no subjects complained of discomfort and the third lateral radiograph was taken just before the end of 5-min anterior lean traction.
Fig. 1.
Anterior lean traction in the sitting position. The rope angle was adjusted to 20° relative to the vertical plane and the subject was in the anterior leaned posture on a custom-made chair. The adjustable sternum and forearm supports prevented the subject’s spine from going into a slump posture during traction
Group B
The traction procedures of two groups were the same, except for the reversed sequences of traction methods. Subjects received the first cervical traction in anterior leaned posture (rope angle = 20°) for 5 min. Then they underwent the axial traction in sitting posture (rope angle = 0°) 3 days later. Two radiographs were taken before the end of different traction modes.
During radiographic image analysis, the positions of 22 bony landmarks were digitized utilizing SigmaScan 5.0 (SPSS Inc., Chicago, USA) on high-resolution monitors. The anatomical identifications of vertebral landmarks were based on the method of Frobin et al. [7, 38]. They were two inferior corners of the second vertebra (C2), and the anterior–posterior corners of two endplates from C3 to C7. This method of vertebral identification has been proved valid, accurate, and reliable for detecting the intervertebral disc spaces and movements [19, 25, 29, 38]. Examiners were blinded to the activities for identifying vertebral landmarks and totally two sets of 96 images were digitized by two experienced members of the spine laboratory. The examiners were also blinded to the group identity with different traction sequences. These vertebral landmarks were digitized 3 times each, and mean values of the three measurements were used for subsequent analysis.
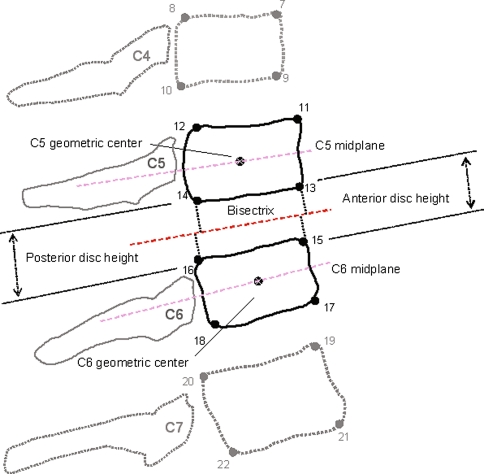
A computer program was written to construct the midplanes of vertebrae defined as a line running through the midpoints between anterior and posterior two corners and the bisectrix between two midplanes were derived. The perpendiculars were constructed from anterior-inferior corner of cranial vertebra and anterior-superior corner of caudal vertebra onto the bisectrix. Anterior disc height was defined as the sum of the perpendicular distances of these two corners to the bisectrix [7, 38]. To compensate for variations in stature and radiographic magnification, the mean depth of the caudally adjacent vertebra was used to normalize the measurement of intervertebral disc spaces (Fig. 2).
Fig. 2.
Definition of the anterior and posterior disc heights between segments C5 and C6. The perpendiculars were constructed from anterior-inferior corner of cranial vertebra C5 and anterior-superior corner of caudal vertebra C6 onto the bisectrix between two midplanes. Anterior disc height was defined as the sum of the perpendicular distances of these two corners to the bisectrix
To detect the traction difference at a two-sided 5% significance level, if the true difference between tractions is 0.10 mm, at least 26 subjects are required in a crossover study with a power of 90% [8, 11, 14]. Therefore, 32 healthy adult subjects were recruited into this study (power = 0.95). The ANOVA was performed to determine whether there was an effect of traction order in our crossover design. The reliabilities of digitizing procedures within examiners at a 2-week interval and between examiners were assessed with intraclass correlation coefficient (ICC) and mean absolute difference (MAD) methods in six different randomly selected subjects. For the comparison between baseline and traction protocols, a paired t test with probability level of P < 0.05 was selected as the criterion for noting significant difference. Independent-sample t tests were used to test post-traction change in disc spaces between axial and anterior lean tractions. Analyses were performed using the Scientific Package for Social Sciences (version 12; SPSS, Chicago, IL, USA).
Results
The mean age of the 32 subjects (19 female and 13 male) was 22.0 ± 2.7-years-old (female: 22.1 ± 2.7 years; male: 21.9 ± 2.8 years). The mean body height was 165.5 ± 7.2 cm (female: 161.7 ± 5.3 cm; male: 171.8 ± 5.2 cm), and mean body weight was 59.2 ± 9.6 kg (female: 53.8 ± 7.3 kg; male: 68.3 ± 4.8 kg). About 25% of the individual body weight was selected as the amount of traction force with an average of 14.9 ± 2.5 kg (female: 13.6 ± 1.9 kg; male: 17.2 ± 1.3 kg).
Evaluation of errors and repeatability
The intraclass correlation coefficients (ICC) for calculating the intervertebral disc spaces varied between 0.891 and 0.966 (average = 0.942) and the corresponding MAD averaged 0.12 mm within examiners. The inter-examiner ICC values of the calculated disc spaces ranged from 0.874 to 0.952 (average = 0.928) and the corresponding MAD averaged 0.15 mm between examiners. In order to test the reproducibility of traction methods, four different subjects were randomly selected to receive the same cervical traction protocols 1 month later. The average ICC was 0.933 with a MAD of 0.14 mm in measuring the anterior and posterior disc spaces.
Intervertebral disc spaces
The effect of traction order was examined by ANOVA and results showed that the different orders of cervical traction in two groups did not significantly affect the intervertebral disc space changes across traction applications (P = 0.302; 0.619). The mean values of anterior and posterior intervertebral disc spaces with 95% confidence intervals at each spinal level are summarized in Tables 1 and 2. In general, there were significant increases in anterior intervertebral disc spaces with axial traction compared to baseline neutral position (P < 0.01). For the changes in posterior intervertebral disc spaces, most cervical segments revealed the significant decreases during axial traction except for C2/3 level (P = 0.365; Table 1). Considering the disc space changes with the application of anterior lean traction, our results showed that the statistical increases were detected both in anterior and in posterior disc spaces (both P < 0.01; Table 2).
Table 1.
The mean values of the anterior and posterior intervertebral disc spaces with 95% confidence intervals at each spinal level with and without cervical axial traction
| Level | Disc space (n = 32) | Without traction | With traction | Disc space change | Individual 95% confidence interval | Paired t test | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (mm) | SD | Mean (mm) | SD | Mean (mm) | SD | Lower bound | Upper bound | P | ||
| C2/3 | Anterior | 4.87 | 0.54 | 4.94 | 0.53 | 0.07* | 0.04 | 0.06 | 0.09 | <0.001 |
| Posterior | 5.13 | 0.45 | 5.15 | 0.44 | 0.02 | 0.14 | −0.03 | 0.07 | 0.365 | |
| C3/4 | Anterior | 4.94 | 0.57 | 5.03 | 0.75 | 0.08* | 0.06 | 0.06 | 0.10 | <0.001 |
| Posterior | 5.17 | 0.50 | 5.05 | 0.53 | −0.12* | 0.14 | −0.17 | −0.07 | <0.001 | |
| C4/5 | Anterior | 5.53 | 0.75 | 5.68 | 0.71 | 0.14* | 0.12 | 0.10 | 0.19 | <0.001 |
| Posterior | 4.97 | 0.52 | 4.83 | 0.51 | −0.14* | 0.12 | −0.18 | −0.09 | <0.001 | |
| C5/6 | Anterior | 6.14 | 0.69 | 6.27 | 0.76 | 0.13* | 0.25 | 0.03 | 0.21 | 0.009 |
| Posterior | 5.19 | 0.54 | 4.99 | 0.56 | −0.20* | 0.14 | −0.25 | −0.15 | <0.001 | |
| C6/7 | Anterior | 6.67 | 0.71 | 6.88 | 0.73 | 0.21* | 0.17 | 0.15 | 0.27 | <0.001 |
| Posterior | 4.59 | 0.57 | 4.48 | 0.57 | −0.11* | 0.17 | −0.17 | −0.05 | <0.001 | |
* P < 0.05 compared between the baseline measurement and axial traction
Table 2.
The mean values of the anterior and posterior intervertebral disc spaces with 95% confidence intervals at each spinal level with and without anterior lean traction
| Level | Disc space (n = 32) | Without traction | With traction | Disc space change | Individual 95% confidence interval | Paired t test | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (mm) | SD | Mean (mm) | SD | Mean (mm) | SD | Lower bound | Upper bound | P | ||
| C2/3 | Anterior | 4.87 | 0.54 | 5.04 | 0.54 | 0.16* | 0.07 | 0.14 | 0.19 | <0.001 |
| Posterior | 5.13 | 0.45 | 5.28 | 0.47 | 0.15* | 0.08 | 0.12 | 0.18 | <0.001 | |
| C3/4 | Anterior | 4.94 | 0.57 | 5.25 | 0.59 | 0.31* | 0.14 | 0.26 | 0.36 | <0.001 |
| Posterior | 5.17 | 0.50 | 5.44 | 0.52 | 0.27* | 0.20 | 0.20 | 0.25 | <0.001 | |
| C4/5 | Anterior | 5.53 | 0.75 | 5.93 | 0.72 | 0.40* | 0.13 | 0.36 | 0.45 | <0.001 |
| Posterior | 4.97 | 0.52 | 5.29 | 0.56 | 0.32* | 0.13 | 0.27 | 0.36 | <0.001 | |
| C5/6 | Anterior | 6.14 | 0.69 | 6.42 | 0.69 | 0.28* | 0.08 | 0.25 | 0.31 | 0.009 |
| Posterior | 5.19 | 0.54 | 5.44 | 0.57 | 0.25* | 0.14 | 0.20 | 0.30 | <0.001 | |
| C6/7 | Anterior | 6.67 | 0.71 | 6.94 | 0.68 | 0.27* | 0.12 | 0.22 | 0.31 | <0.001 |
| Posterior | 4.59 | 0.57 | 4.81 | 0.58 | 0.22* | 0.16 | 0.17 | 0.28 | <0.001 | |
* P < 0.05 compared between the baseline measurement and anterior lean traction
Comparison between axial and anterior lean tractions
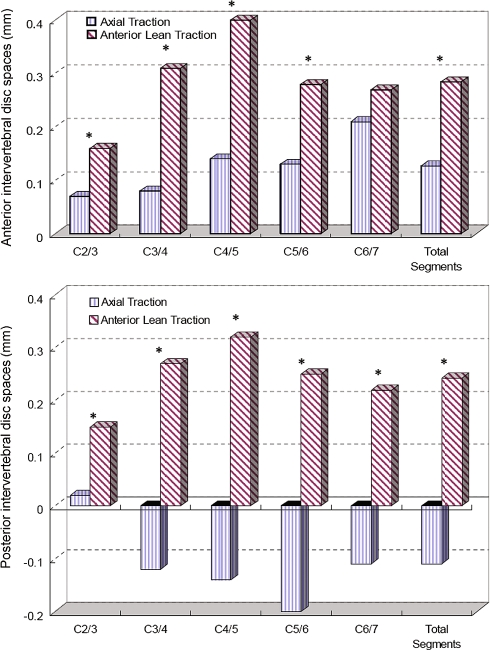
The independent sample t tests showed that the increases both in anterior and in posterior disc spaces were significantly greater with the application of anterior lean traction than with axial traction (both P < 0.01). The intervertebral disc space changes at the individual spinal levels (C2/3–C6/7) were also greater in the anterior lean traction (P < 0.01) except for the anterior disc space at C6/7 segment (P = 0.152). The traction effects of the paired intervertebral disc spaces at each spinal level are illustrated in Fig. 3.
Fig. 3.
The post-traction changes in the anterior (upper panel) and posterior (lower panel) intervertebral disc spaces at each spinal level (C2/3–C6/7) between axial and anterior lean tractions. The intervertebral disc space changes were significantly greater in the anterior lean traction (P < 0.01) except for the anterior disc space at C6/7 segment (P = 0.152). *P < 0.05 compared between the axial and anterior lean tractions
Discussion
This blind, randomized crossover-design study quantitatively demonstrated that anterior lean traction in sitting position provided more anterior and posterior intervertebral disc space enlargements than axial traction did for the healthy adult subjects. The application of the valid radiographic image protocol in the measurement of the disc space alternations during cervical traction revealed good reliabilities within and between examiners.
Evaluation of errors and repeatability
Considering the reliability tests within and between examiners in the present study, the ICCs for measuring the intervertebral disc spaces were consistent with those in the previous studies [7, 34]. Our percentage of relative errors in measuring the disc heights among segments (2.1%–3.2%) was similar to the measurement error in the study by Frobin et al. [7]. The methods used in the identification of vertebral landmarks and definition of disc spaces were basically the same for both experiments. Vaugh et al. [34] reported a slightly lower inter-rater reliability of 0.887 for intervertebral space measurements. One possible explanation for the discrepancy might be associated with the differences in the mathematical constructions of measurements. Their intervertebral space was simply derived through connecting two points between adjacent vertebral corners. In contrast, our method, using precisely calculated perpendicular distances between the vertebral landmarks to bisectrix was considered to be more reproducible than connecting corners between adjacent vertebrae [31].
Intervertebral disc spaces
The mean disc heights of the normal or mild degenerated discs were 4.69–6.82 mm measured by computed tomography or magnetic resonance imaging [33, 35]. The mean anterior and posterior disc spaces in neutral sitting posture were 5.63 mm and 5.01 mm, respectively, in the present study. These results were consistent with the findings of published researches [33–35, 37]. The intervertebral disc injury, aging process, and disc degeneration are believed to contribute to the disc height loss and related clinical manifestations [16, 18, 20, 23, 33, 35]. Wang et al. reported that the disc heights in patients with severe disc degeneration were 2.45 ± 0.64 mm at corresponding intervertebral spaces of spinal cord compression [35]. In addition to the acceptable range of our measurements, the derived intervertebral disc heights were also supported by the ratio of 1/3 between disc height (about 5 mm) and vertebral height (about 15–17 mm) from radiographic studies [7, 16].
The scientific rationale for the biomechanical role of cervical traction is based on the separations between the intervertebral disc spaces [34, 37]. The intervertebral disc spaces significantly increased anteriorly and decreased posteriorly with axial traction compared to baseline. However, the cervical spine might extend to a certain extent due to the increased anterior and decreased posterior intervertebral spaces. The upward traction force applied on the mandible was documented to cause some extension movement in the neck [3, 34]. Wong et al. [37] reported that the posterior intervertebral spaces did not significantly decrease during axial traction in spine position. One possible explanation for the discrepancy might be that the traction table prevented subject’s neck from moving into an excessive extension movement. Conventional axial traction of cervical spine applied the head harness to fit under chin and occiput, so traction forces were transmitted mainly through the chin strap to teeth and temporomandibular joints (TMJ). Demir et al. [6] suggested that a mouthguard could be used to reduce the tooth pain if cervical tractions were arranged. Vaughn et al. [34] further adopted a traction device to direct the traction forces toward occiput thereby avoiding the TMJ compression and neck extension. The excessive neck extension would decrease the posterior disc spaces and in turn the efficacy of traction for improving the available course of nerve roots through neural foramens.
The statistically greater anterior and posterior disc spaces during anterior lean traction in sitting position were in agreement with the published reports in the supine position [37]. The neck extension vector caused by the traction force through mandible could be counteracted by the downward force of head weight due to gravity. It has been reported that traction forces with a flexion moment were especially effective on the posterior elements of spinal vertebral column, such as posterior intervertebral discs, apophyseal joints, spinal muscles, and ligaments [12, 21]. The increase in the posterior disc spaces implied that there would be an increase in the tension of posterior annular fibers and posterior longitudinal ligament. The stretching of the posterior annulus might prevent the posterior movement of herniated nuclear materials and reduce the posterior disc bulges [21, 27]. However, clinical caution was suggested because cervical flexion might aggravate an existing tear in the annulus fibrosis, compress the anterior disc part, and cause further extrusion of herniated nucleus pulposus [21, 32, 34]. Cervical traction with excessive flexion might not be well tolerated by patients with spinal diseases [12].
Comparison between axial and anterior lean tractions
The cervical flexion movement was proposed to enlarge the intervertebral spaces, whereas the extension movement narrowed them [15, 37]. The finding of statistically greater increase in anterior disc spaces during anterior lean traction was consistent with the study by Wong et al. [37]. They concluded that there was a greater percentage of improvement in anterior intervertebral spaces during the 30° flexion traction compared to the axial traction. The anterior lean posture that initiated mainly through the hip joints might still result in small artifacts of the disc-height changes; however, the results of the increased anterior and posterior disc heights emphasized the balanced separation effect of traction forces. The spinal nerve roots are located on the posterior part of the spine, where the nerve roots exit the spinal canal through the bony tunnels called the neural foramens. In order to improve the efficiency of traction treatment, the increment of posterior intervertebral space is essential for the greater dimension of neural foramen. The results of the greater posterior disc spaces obtained in the present study during anterior lean traction were supported by the previously published researches. These researches advocated a better traction effect on the separation of intervertebral spaces by traction with spinal flexion [12, 21, 22]. The efficacy of cervical traction was usually investigated in supine position despite of the frequent application in a sitting condition at clinics [1, 3, 4, 13, 37]. Based on our results, the biomechanical efficacy of anterior lean seated traction was manifested through the statistical increase in the anterior and posterior intervertebral disc spaces. With the sternum and forearm supports during anterior lean position, the neck extension vector caused by the traction force applied on mandible was counteracted by the downward force of head weight to obtain the more evenly distributed traction forces over the anterior and posterior cervical structures. In contrast, the axial traction significantly decreased the posterior disc spaces because the upward traction force mainly through the mandible might introduce the extension moment around neck. This scenario might occur less frequently in the supine position due to the support of traction table.
The spinal traction was documented to increase in intervertebral foramen and in the traction via flexion could increase the degree of the opening of foraminal spaces [21, 22]. Humphreys et al. [12] further demonstrated that the flexion moment created by traction forces improved the volume of intervertebral foramen by 14% compared to the axial traction in neutral position. The significantly increased posterior disc spaces during anterior lean traction might infer an increase in the tension of the posterior annular fibers and posterior longitudinal ligament for reducing the posterior herniated nuclear materials. This blind, randomized crossover study quantitatively demonstrated that the anterior lean traction in sitting position provided greater enlargements of both anterior and posterior intervertebral disc spaces than axial traction did in the healthy subjects. The findings of this study might serve as a therapeutic reference when cervical traction is suggested. This study was performed on young healthy subjects without signs and symptoms of cervical diseases. The future randomized clinical trial studies on a wider age range of the patients with disc herniation or foraminal stenosis disease will be helpful to explore the effects on the intervertebral disc space changes that resulted from the axial and anterior lean traction in sitting position.
Acknowledgments
No funds were received in support of this study.
Conflict of interest statement No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1.Akinbo SR, Noronha CC, Oke DA, et al. Effect of cervical traction on cardiovascular and selected ECG variables of cervical spondylosis patients using various weights. Niger Postgrad Med J. 2006;13:81–88. [PubMed] [Google Scholar]
- 2.Cleland JA, Whitman JM, Fritz JM, et al. Manual physical therapy, cervical traction, and strengthening exercises in patients with cervical radiculopathy: a case series. J Orthop Sports Phys Ther. 2005;35:802–811. doi: 10.2519/jospt.2005.0201. [DOI] [PubMed] [Google Scholar]
- 3.Colachis SC, Jr, Strohm BR. Cervical traction: relationship of traction time to varied tractive force with constant angle of pull. Arch Phys Med Rehabil. 1965;46:815–819. [PubMed] [Google Scholar]
- 4.Deets D, Hands KL, Hopp SS. Cervical traction. A comparison of sitting and supine positions. Phys Ther. 1977;57:255–261. doi: 10.1093/ptj/57.3.255. [DOI] [PubMed] [Google Scholar]
- 5.DeLacerda FG. Techniques in the application of cervical traction: a review of research findings. J Okla State Med Assoc. 1979;72:79–82. [PubMed] [Google Scholar]
- 6.Demir T, Canakci V, Eltas A, et al. Effectiveness of mouthguards on tooth pain and mobility in cervical traction treatment. J Back Musculoskelet. 2008;21:91–98. [Google Scholar]
- 7.Frobin W, Leivseth G, Biggemann M, et al. Vertebral height, disc height, posteroanterior displacement and dens-atlas gap in the cervical spine: precision measurement protocol and normal data. Clin Biomech (Bristol, Avon) 2002;17:423–431. doi: 10.1016/S0268-0033(02)00044-X. [DOI] [PubMed] [Google Scholar]
- 8.Ghoname EA, Craig WF, White PF, et al. Percutaneous electrical nerve stimulation for low back pain: a randomized crossover study. JAMA. 1999;281:818–823. doi: 10.1001/jama.281.9.818. [DOI] [PubMed] [Google Scholar]
- 9.Graham N, Gross AR, Goldsmith C. Mechanical traction for mechanical neck disorders: a systematic review. J Rehabil Med. 2006;38:145–152. doi: 10.1080/16501970600583029. [DOI] [PubMed] [Google Scholar]
- 10.Hattori M, Shirai Y, Aoki T. Research on the effectiveness of intermittent cervical traction therapy, using short-latency somatosensory evoked potentials. J Orthop Sci. 2002;7:208–216. doi: 10.1007/s007760200035. [DOI] [PubMed] [Google Scholar]
- 11.Hollander E, Allen A, Kwon J, et al. Clomipramine vs desipramine crossover trial in body dysmorphic disorder: selective efficacy of a serotonin reuptake inhibitor in imagined ugliness. Arch Gen Psychiatry. 1999;56:1033–1039. doi: 10.1001/archpsyc.56.11.1033. [DOI] [PubMed] [Google Scholar]
- 12.Humphreys SC, Chase J, Patwardhan A, et al. Flexion and traction effect on C5-C6 foraminal space. Arch Phys Med Rehabil. 1998;79:1105–1109. doi: 10.1016/S0003-9993(98)90179-4. [DOI] [PubMed] [Google Scholar]
- 13.Jette DU, Falkel JE, Trombly C. Effect of intermittent, supine cervical traction on the myoelectric activity of the upper trapezius muscle in subjects with neck pain. Phys Ther. 1985;65:1173–1176. doi: 10.1093/ptj/65.8.1173. [DOI] [PubMed] [Google Scholar]
- 14.Jones B, Kenward MG. Design and analysis of cross-over trials: monographs on statistics and applied probability. New York: Chapman & Hall; 1989. [Google Scholar]
- 15.Kitagawa T, Fujiwara A, Kobayashi N, et al. Morphologic changes in the cervical neural foramen due to flexion and extension: in vivo imaging study. Spine. 2004;29:2821–2825. doi: 10.1097/01.brs.0000147741.11273.1c. [DOI] [PubMed] [Google Scholar]
- 16.Kolstad F, Myhr G, Kvistad KA, et al. Degeneration and height of cervical discs classified from MRI compared with precise height measurements from radiographs. Eur J Radiol. 2005;55:415–420. doi: 10.1016/j.ejrad.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Krause M, Refshauge KM, Dessen M, et al. Lumbar spine traction: evaluation of effects and recommended application for treatment. Man Ther. 2000;5:72–81. doi: 10.1054/math.2000.0235. [DOI] [PubMed] [Google Scholar]
- 18.Kroeber M, Unglaub F, Guehring T, et al. Effects of controlled dynamic disc distraction on degenerated intervertebral discs: an in vivo study on the rabbit lumbar spine model. Spine. 2005;30:181–187. doi: 10.1097/01.brs.0000150487.17562.b1. [DOI] [PubMed] [Google Scholar]
- 19.Kroeber M, Unglaub F, Wang H, et al. New in vivo animal model to create intervertebral disc degeneration and to investigate effects of therapeutic strategies to stimulate disc regeneration. Spine. 2002;27:2684–2690. doi: 10.1097/00007632-200212010-00007. [DOI] [PubMed] [Google Scholar]
- 20.Kwon BK, Song F, Morrison WB, et al. Morphologic evaluation of cervical spine anatomy with computed tomography: anterior cervical plate fixation considerations. J Spinal Disord Tech. 2004;17:102–107. doi: 10.1097/00024720-200404000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Lee RYW, Evans JH. Loads in the lumbar spine during traction therapy. Aust J Physiother. 2001;47:102–108. doi: 10.1016/s0004-9514(14)60301-9. [DOI] [PubMed] [Google Scholar]
- 22.Liu J, Ebraheim NA, Sanford CG, Jr, et al. Quantitative changes in the cervical neural foramen resulting from axial traction: in vivo imaging study. Spine J. 2008;8:619–623. doi: 10.1016/j.spinee.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 23.Lu J, Ebraheim NA, Huntoon M, et al. Cervical intervertebral disc space narrowing and size of intervertebral foramina. Clin Orthop Relat Res. 2000;370:259–264. doi: 10.1097/00003086-200001000-00026. [DOI] [PubMed] [Google Scholar]
- 24.Moeti P, Marchetti G. Clinical outcome from mechanical intermittent cervical traction for the treatment of cervical radiculopathy: a case series. J Orthop Sports Phys Ther. 2001;31:207–213. doi: 10.2519/jospt.2001.31.4.207. [DOI] [PubMed] [Google Scholar]
- 25.Muggleton JM, Allen R. Insights into the measurement of vertebral translation in the sagittal plane. Med Eng Phys. 1998;20:21–32. doi: 10.1016/S1350-4533(97)00045-3. [DOI] [PubMed] [Google Scholar]
- 26.Olivero WC, Dulebohn SC. Results of halter cervical traction for the treatment of cervical radiculopathy: retrospective review of 81 patients. Neurosurg Focus. 2002;12:ECP1. doi: 10.3171/foc.2002.12.2.4. [DOI] [PubMed] [Google Scholar]
- 27.Onel D, Tuzlaci M, Sari H, et al. Computed tomographic investigation of the effect of traction on lumbar disc herniations. Spine. 1989;14:82–90. doi: 10.1097/00007632-198901000-00017. [DOI] [PubMed] [Google Scholar]
- 28.Ozturk B, Gunduz OH, Ozoran K, et al. Effect of continuous lumbar traction on the size of herniated disc material in lumbar disc herniation. Rheumatol Int. 2006;26:622–626. doi: 10.1007/s00296-005-0035-x. [DOI] [PubMed] [Google Scholar]
- 29.Pfeiffer M, Geisel T. Analysis of a computer-assisted technique for measuring the lumbar spine on radiographs: correlation of two methods. Acad Radiol. 2003;10:275–282. doi: 10.1016/S1076-6332(03)80101-0. [DOI] [PubMed] [Google Scholar]
- 30.Pio A, Rendina M, Benazzo F, et al. The statics of cervical traction. J Spinal Disord. 1994;7:337–342. doi: 10.1097/00002517-199408000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Reitman CA, Mauro KM, Nguyen L, et al. Intervertebral motion between flexion and extension in asymptomatic individuals. Spine. 2004;29:2832–2843. doi: 10.1097/01.brs.0000147740.69525.58. [DOI] [PubMed] [Google Scholar]
- 32.Saunders HD. Use of spinal traction in the treatment of neck and back conditions. Clin Orthop Relat Res. 1983;179:31–38. doi: 10.1097/00003086-198310000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Sohn HM, You JW, Lee JY. The relationship between disc degeneration and morphologic changes in the intervertebral foramen of the cervical spine: a cadaveric MRI and CT study. J Korean Med Sci. 2004;19:101–106. doi: 10.3346/jkms.2004.19.1.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vaughn HT, Having KM, et al. Radiographic analysis of intervertebral separation with a 0 degrees and 30 degrees rope angle using the Saunders cervical traction device. Spine. 2006;31:E39–E43. doi: 10.1097/01.brs.0000194840.42792.f2. [DOI] [PubMed] [Google Scholar]
- 35.Wang B, Liu H, Wang H, et al. Segmental instability in cervical spondylotic myelopathy with severe disc degeneration. Spine. 2006;31:1327–1331. doi: 10.1097/01.brs.0000218508.86258.d4. [DOI] [PubMed] [Google Scholar]
- 36.Wong AM, Lee MY, Chang WH, et al. Clinical trial of a cervical traction modality with electromyographic biofeedback. Am J Phys Med Rehabil. 1997;76:19–25. doi: 10.1097/00002060-199701000-00005. [DOI] [PubMed] [Google Scholar]
- 37.Wong AM, Leong CP, Chen CM. The traction angle and cervical intervertebral separation. Spine. 1992;17:136–138. doi: 10.1097/00007632-199202000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Wu SK, Kuo LC, Lan HC, et al. The quantitative measurements of the intervertebral angulation and translation during cervical flexion and extension. Eur Spine J. 2007;16:1435–1444. doi: 10.1007/s00586-007-0372-4. [DOI] [PMC free article] [PubMed] [Google Scholar]