Abstract
Owing to failure to achieve positive long-term effects, the currently performed treatment methods for lumbar facet joint syndrome (LFJS) are still under debate. Interspinous distraction devices unload the facet joints. Thus, these devices might be an alternative surgical treatment method for LFJS. The aim of this study was to evaluate the clinical and radiological outcome of an interspinous distraction device for the treatment of LFJS. Subjects had verified single level LFJS at level L4–5. They received percutaneous facet joint denervation (PFJD). If pain persisted, they were offered implantation of an interspinous device (Coflex) and/or repeat PFJD. Clinical and radiological outcome was determined before and after PFJD or surgery up to 2 years afterwards in all cases. Forty-one patients with LFJS at L4–5 underwent PFJD. Twenty patients with persisting pain underwent a subsequent surgery for implantation of an interspinous device. Five patients with recurrent pain at 6–12 months opted for an additional PFJD. Three obese patients (body weight >100 kg) had persistent pain at 3 months after surgery and received additionally dorsal semi-dynamic stabilization. The clinical outcome improved significantly in the surgically treated patients; however, it did not differ compared with patients receiving PFJD only after 24 months. Radiological evaluation revealed a restricted range of motion (ROM) of the operated and an elevated ROM of the adjacent segment. Surgical or device-related complications were not observed. In conclusions, the implantation of an interspinous Coflex device in case of recurrent facet joint pain succeeds to improve facet joint pain in clinical short-and mid-term settings. However, it does not exceed the outcome of denervated patients.
Keywords: Back pain, Interspinous distraction, Percutaneous neurotomy, Lumbar spine, Facet joint
Introduction
The lumbar facet joint syndrome (LFJS) is a common cause of chronic low back pain [5, 15, 17, 18]. Facet joint therapy consists of injections into or at the facet joint itself or at the medial branches of the dorsal rami [27, 28, 33, 47], percutaneous radiofrequency denervation or kryorhizotomie [38–40, 44–47, 49], or surgery [4, 10–12, 15, 19, 32, 34]. The recurrence rate 6–12 months after radiofrequency denervation is over 60% [1, 42]. The failure to achieve a positive long-term effect often leads to fusion surgery. On the basis of the results of prospective [11, 32] and retrospective [12, 19] studies, fusion surgery is not broadly supported in the treatment of the degenerative LFJS [8]. Moreover, fusion surgery possibly accelerates degeneration of the adjacent segments [24, 26, 41].
An alternative to fusion surgery in patients suffering from LFJS might be the use of interspinous distraction devices. Patients with spinal canal stenosis or re-herniated lumbar disc experience a reduction in back pain following the insertion of such devices [43, 55, 56]. This beneficial effect is probably due to the release and stabilization of the facet joint [6, 43, 55, 56] as demonstrated in cadaver model studies [14, 21, 37, 48, 53].
In this study, the surgical treatment of recurrent lumbar facet joint pain with a dynamic interspinous device (Coflex; Paradigm Spine; New York, NY, USA) in patients with an additional relative spinal canal stenosis, but without claudicatio spinalis was evaluated after 2 years of follow-up.
Methods
This study, retrospectively, reviewed 143 patients who were diagnosed with LFJS between February 2004 and May 2005. The diagnosis was verified by facet joint infiltration (FJI). The history and physical examination revealed low back pain in all cases, sometimes with pain to the dorsal thigh. There were no radicular symptoms, claudicatio spinalis, or reduction in walking distance. Hyperextension had an additive effect; whereas, the flexion lead to a pain relief in most of cases. Pain could be provoked by paramedian pressure over the facet joints in many cases. Pressure above the sacroiliac joint did not provoke the characteristic pain.
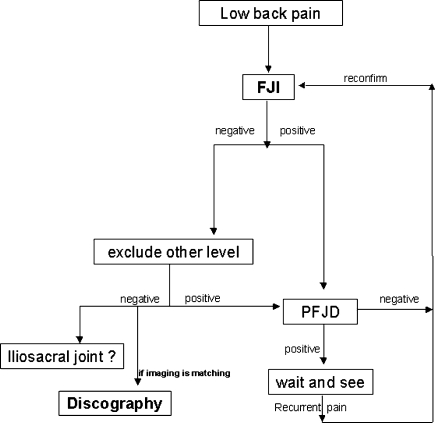
To establish a differential diagnosis between discogenic pain and facet joint pain, all patients underwent the same diagnostic algorithm at our department as shown in Fig. 1. According to our diagnostic algorithm, an X-ray-controlled FJI was performed first, as it is less invasive than discography. If the patients did not respond to the FJI and if the segment showed degeneration on imaging, discography was performed. If the patients responded to the FJI with clinically relevant pain relief, a discography was not performed, even when there were radiological signs of DDD.
Fig. 1.
Algorithm showing the diagnostic procedures for differentiating the origin of low back pain at our department
Facet joint infiltration was performed at a single level. If this did not lead to substantial pain relief, another level was infiltrated several days later to isolate the segment of main pain. All FJIs were performed bilaterally under fluoroscopic guidance by the same neurosurgeon. One milliliter of bupivacain 0.5% and 0.5 ml triamcinolone acetonide were injected with a 22 GA needle in or around the joints. Patients with a pain relief of at least 70% after FJI were considered to have an LFJS. Back pain was measured with a visual analog scale (VAS) before the injection and again one day after the injection.
Out of these patients, 43 patients had LFJS at level L4–5. In these patients, CT scans showed a relative spinal canal stenosis, defined as an anterior-posterior diameter between 10 and 13 mm.
As therapy, percutaneous facet joint denervation (PFJD) was conducted within a few days after FJI with the Neuro N50 (F. L. Fischer; Freiburg, Germany). All of the PFJDs were performed at a single level on both sides by the same neurosurgeon, as previously described [9], with a temperature of 85° for 90 s, after application of 0.5 ml lidocaine 2% at the target points of the L4 and L5 transverse processes of both sides. FJI and PFJD were performed with the aid of one nurse at our outpatient department. The patients were released at the same day and could return to normal life activity. 1 min in our outpatient department costs €1.31. The hospital receives €191 for a thermocoagulation according to the diagnosis-related groups (DRG) system in Germany.
Visual analog scale and Oswestry disability index (ODI) version 2.0 were evaluated before and after this intervention. The outcome of all of these patients was evaluated 7 days and 3, 6, 12, 18, and 24 months after PFJD by VAS, ODI, and Odom’s criteria. Clinical success was defined as having both (1) VAS reduction of 50% from pre-op to 2-year follow-up and (2) an Odom’s criteria of “excellent” or “good”.
In cases of recurrent pain after PFJD, FJI was performed again at L4–5 to reconfirm the diagnosis. If positive, the patients were offered either an additional PFJD or implantation of an interspinous device (Coflex; Paradigm; New York, NY, USA) under general anesthesia.
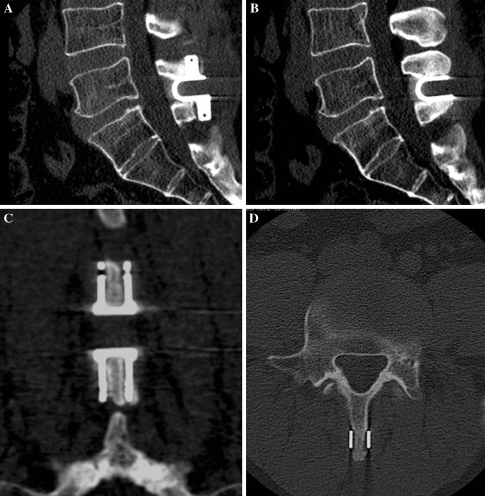
For this surgery, the interspinous ligaments were removed with a rongeur after a midline skin incision of approximately 4 cm. The required size of the device implant was measured using a trial inserter under fluoroscopy. Then, the interspinous distractor was inserted tightly into the interspinous space as deeply as possible. Finally, the wing clamps of the implant were tightened with forceps (Fig. 2). Special care was taken to avoid destruction of the medial branch by excluding the use of a monopolar or bipolar at the level of the facet joints. The operated patients were mobilized the next day after surgery and left the hospital 3–7 days later. They were instructed to avoid heavy labor for 4 weeks. 1 min in our OR costs €2.63. The hospital receives €4,474 for this procedure according to the DRG system in Germany.
Fig. 2.
CT scans showing the tight contact of the interspinous device to the spinous processes. The wing clamps hold the device in the median position. a, b Sagittal, c coronar, d axial
Patients with recurrent pain following implantation of the Coflex device underwent FJI again to confirm the diagnosis of an LFJS at the same level. Then, they were stabilized with a semi-dynamic stabilization system (Cosmic; Ulrich Medical; Ulm, Germany) via a transmuscular approach. Owing to the approach and the placement of the pedicle screws, destruction of the medial branches could be considered probable. The medial Coflex device did not hinder access for pedicle screw insertion and did not need to be removed. All of these operations were performed by the same neurosurgical team. All follow-up examinations were performed by the authors on an outpatient basis at our department.
Plain and flexion–extension radiographs of the lumbar spine were performed before surgery and at 3, 12, and 24 months after surgery. Lumbar lordosis (L1–5), segmental lordosis at L4–5, and adjacent segment lordosis at L3–4 were measured in the neutral position according to Cobb [7]. Lumbar, segmental, and adjacent segmental sagittal range of motion (ROM) were measured on flexion–extension radiographs. The degree of degenerative changes in the facet joints and intervertebral discs was determined by Kellgren’s criteria before surgery [20].
Results
Study sample
Percutaneous facet joint denervation was performed in 43 patients with a single level LFJS at L4–5. Two patients were excluded from the analysis because of a later disc herniation at L5–S1. Pre-operative age, sex, body mass index, smoking behavior, pain medication use, previous operations, employment status, and pain distribution are presented in Table 1 for non-surgical and surgical patients.
Table 1.
Sociodemographic and clinical data of the study patients
| Surgical patients | Non-surgical patients | |
|---|---|---|
| Number of patients | 20 | 21 |
| Gender | ||
| Male | 15 | 11 |
| Female | 5 | 10 |
| Age of patients | 39–71 years | 39–73 years |
| BMI (kg/m2) | 27.15 (±5.5) | 28.62 (±4.4) |
| Employment status | ||
| Employed | 9 | 12 |
| Unemployed | 7 | 3 |
| Retired | 4 | 6 |
| Smoker | 8 | 8 |
| Pain medication | ||
| NSAIR | 20 | 21 |
| Opiates | 9 | 8 |
| Previous surgery at level L4–5 | 6 | 11 |
| Pain distribution | ||
| Back | 20 | 21 |
| Buttock | 6 | 9 |
| Dorsal thigh | 5 | 5 |
| Lower leg | – | – |
Clinical outcomes
At the 7-day follow-up after PFJD, 40 of 41 (98%) patients experienced a relief of back pain greater than 50% according to the VAS. But at 3 months of follow-up, only 18 of 41 (44%) patients reported of a relief of back pain greater than 50%. Twenty-three of 41 patients stated a recurrent back pain intensity of more than 50% at the 3 months follow-up. Radiating pain to the buttock or thigh improved along with the back pain, but while the back pain recurred in the same location, the distribution of the radiating pain did so with alterations in its distribution.
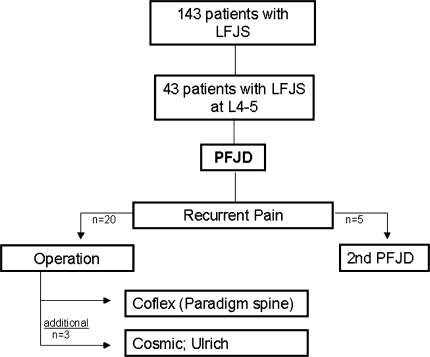
Owing to this recurrent pain within 3 months, 22 patients decided to have an operation and received the Coflex interspinous device. As mentioned above, two operated patients later developed a disc herniation at L5–S1 with sudden onset of sciatica and were excluded from this analysis. Thus, 20 surgical patients were evaluated and 21 patients did not receive any surgery (Fig. 3). Sixteen of these 21 non-surgery patients did not require further invasive therapy. Five patients decided to have a second PFJD because of recurrent pain 6–12 months after the first PFJD (Fig. 3). These patients were included and followed in the non-surgical group.
Fig. 3.
Patient selection for treatment of LFJS. All patients underwent percutaneous facet joint denervation (PFJD). Twenty patients with early recurrence of pain decided for surgery (plus another 2 who were excluded). Five patients with later recurrence of pain decided for a second PFJD (and remained categorized as non-surgical patients). Owing to recurring pain after surgery, three patients received additional screw-rod instrumentation
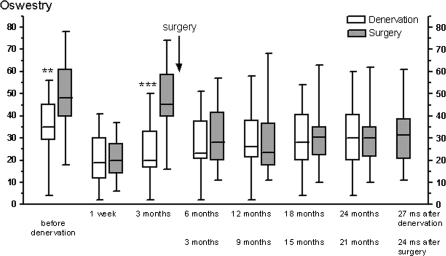
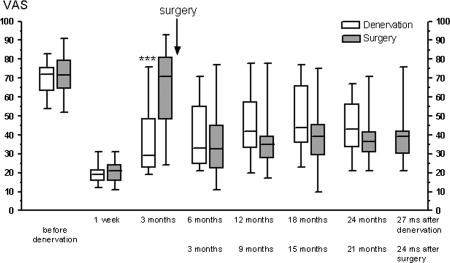
The patients who went on to have surgery had a significantly higher (P < 0.001) ODI at baseline before the initial PFJD than did the patients who never underwent surgery (Fig. 4). Surgical and non-surgical patients benefited significantly 7 days after surgery or PFJD, according to the ODI and VAS (Figs. 4, 5). After 24 months, the treated patients still benefited significantly according to the previously mentioned criteria, although when compared with the 1 week results in both groups, a significant deterioration could be observed (P < 0.027 according to ODI and VAS).
Fig. 4.
Course of functional disability according to the Oswestry disability index (ODI), separated into surgical and non-surgical patients. The later surgical patients received the interspinous implant soon after the 3 month follow-up after denervation
Fig. 5.
Course of pain in surgical and non-surgical patients according to a visual analog scale (VAS) separated into surgical and non-surgical patients. The later surgical patients received the interspinous implant soon after the 3-month follow-up after denervation
Nevertheless, defining success as a reduction of 50% or more in the ODI and VAS, only 9 of the 20 (45%) Coflex patients were successful on the ODI, and only 7 of 20 (35%) were successful on VAS 2 years after surgery. Using the criteria of 50% reduction in ODI or VAS, similar results were found in the non-surgical patients [8 of 21 (38%) according to ODI and 8 of 21 (38%) according to VAS].
After 24 months, the overall outcome according to Odom’s criteria showed similar outcomes in all treated patients (Table 2).
Table 2.
Outcome according to Odom’s criteria of surgical and non-surgical patients
| 12 months | 24 months | |||
|---|---|---|---|---|
| Surgical | Non-surgical | Surgical | Non-surgical | |
| Excellent | 1 | 0 | 0 | 0 |
| Good | 12 | 6 | 4 | 2 |
| Fair | 6 | 12 | 14 | 16 |
| Poor | 1 | 3 | 2 | 3 |
Three surgical patients with a secondary poor outcome within 3 months after implantation of a Coflex device received an additional posterior semi-dynamic stabilization (Cosmic; Ulrich Medical; Ulm, Germany). The final outcome of these patients was good in two cases and fair in one case according to Odom’s criteria. These patients had a weight between 100 and 110 kg. No surgical- or device-related complications were observed.
Radiological outcomes
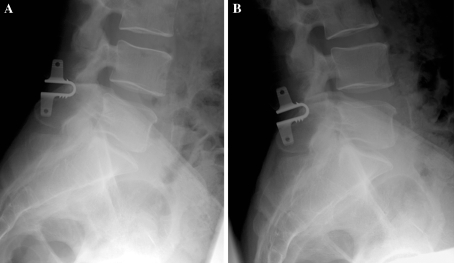
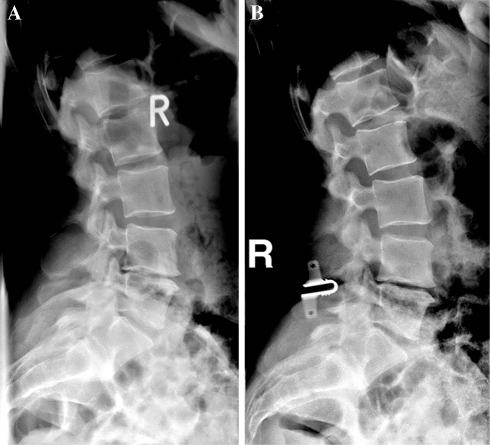
The interspinous devices allowed segmental movement in all of the operated cases (Fig. 6). The data analysis showed a significantly lower lordotic angle of the operated segment L4–5 (P < 0.0001) and a significantly higher lordotic angle of the adjacent level L3–4 (P < 0.032) in plain radiographs 2 years after the operation (Table 3; Fig. 7). Furthermore, the radiographic evaluation showed a significantly restricted ROM of the operated level L4–5 (P = 0.003) and elevated ROM of the adjacent segment L3–4 (P = 0.031) after Coflex implantation (Table 3). The lumbar ROM L1–5 was increased postoperatively (P = 0.006). The radiological evaluation according to Kellgren’s criteria revealed clear degenerative changes in the facet joints (2.95 ± 0.99) and the discs (2.88 ± 1.02) in all patients. These degenerative changes did not correlate with the clinical status (r < 0.29, P > 0.08).
Fig. 6.
Functional radiographs of a 56-year-old male patient. The interspinous distraction device still allows motion at the operated segment. a Flexion, b extension
Table 3.
a Mean lordosis angle in plain scans and b mean sagittal range of motion (ROM) in flexion–extension scans
| Pre-OP | 2 years | P value | |
|---|---|---|---|
| a Plain (°) mean ± SD | |||
| L1–5 (°) | 28.6 ± 11.5 | 27.8 ± 12.1 | 0.283 |
| L3–4 (°) | 6.4 ± 3.7 | 8.0 ± 3.5 | 0.032 |
| L4–5 (°) | 7.8 ± 3.1 | 5.7 ± 2.4 | <0.0001 |
| b ROM (°) mean ± SD | |||
| L1–5 (°) | 15.8 ± 10.4 | 21.1 ± 11.8 | 0.006 |
| L3–4 (°) | 2.0 ± 2.6 | 4.8 ± 4.2 | 0.031 |
| L4–5 (°) | 4.6 ± 2.8 | 2.6 ± 1.5 | 0.003 |
Fig. 7.
Plain radiograph of a 39-year-old female patient with monosegmental degenerative changes at L4–5. a Preoperative. b After implantation of a Coflex interspinous device. The patient responded with a significant pain relief to the FJI and PFJD, so following our diagnostic algorithm, a discography was not performed despite radiological signs of a DDD
Discussion
The presented study shows a 2-year follow-up of 41 patients with LFJS at L4–5 that underwent PFJD. While five patients with recurrent pain opted for additional PFJD, 20 patients underwent a subsequent implantation of an interspinous device. The clinical outcome improved significantly in the surgically treated patients, but it did not differ compared with patients receiving PFJD only after 24 months. Radiological evaluation could show a restricted ROM of the operated and an elevated ROM of the adjacent segment.
Facet joint denervation
The role of PFJD in the long-term treatment of low back pain caused by the facet joints remains controversial. In a prospective randomized study in 70 patients without previous back surgery, PFJD had no significant effect on VAS or ODI at 4 or 12 weeks [25]. However, other prospective randomized studies on PFJD for LFJS have reported a pain reduction in at least 50% in 46–87% of the patients at the 1-year follow-up [9, 49, 50]. In contrast to the study by Leclaire et al. [25] patients’ selection for a PFJD in the latter studies consisted of a pain relief of more than 50% following medial branch block or FJI performed by the study teams themselves.
In the present study, 98% of all patients had a pain relief greater than 50% at the 7-day follow-up; whereas, only 44% of all patients had this much pain relief at the 3 months of follow-up. The present study selected patients by the same criteria as in the studies just mentioned (i.e. substantial reduction of VAS score after FJI), so our relatively low rate of pain reduction 3 months after PFJD might be explained by the high portion of patients with previous back surgery (40%). Studies including patients with previous back surgery have reported only approximately 40% improvement after PFJD [29, 35, 36, 38]. A suboptimal anatomic placement of the radiofrequency needles resulting in ineffective PFJD is another possible explanation [3, 25].
A double-blind control-block to verify the diagnosis of LFJS [30, 31] was not performed, but we view the positive FJI and subsequent beneficial PFJD as a highly indicative sign that LFJS was present and as strong evidence against the possibility of a placebo effect during FJI.
On the basis of the results of the past literature and present study, PFJD appears to be an effective and safe method to treat LFJS [8, 9, 49, 50]. Complications, such as transient dysaesthesia, numbness, or neuritis are rare [9, 49, 50].
Fusion surgery
When compared with PFJD, the role of surgery in the treatment of low back pain remains even more controversial [52]. A significant improvement of low back pain after spinal fusion could not be verified by a review of the Cochrane database [16]. Nevertheless, the differentiated diagnosis of the origin of low back pain by FJI was considered as helpful to achieve substantial clinical improvement by stabilizing surgery [32]. Fusion techniques to treat low back pain possibly related to the facet joints were performed and evaluated in two prospective [11, 32] and two retrospective studies [12, 19]. However, the differentiation of low back pain [19] was not clear and not intended in these studies. FJI was used as a predictor of surgical outcome, but not to make a clear diagnosis of an LFJS.
Recent studies on stabilizing pedicle screw surgery have reported a low rate of complications [2, 54], but still, fusion surgery might accelerate degeneration of the adjacent segments [24, 26, 41]. Interspinous devices might be an alternative in the surgical treatment of degenerative lumbar disease.
Interspinous devices
Distraction of the spinous processes leads to a stretching of the ligamentum flavum (thus widening the spinal canal) and opening of the neuroforamina. Furthermore, it decreases the facet joint loading [53]; so, besides spinal canal stenosis, it might also be possible to treat low back pain originating from the facet joints by distracting the spinous processes.
Regarding the use of different interspinous implants in the clinical setting, controversial results depending on the device used and the indications exist [13, 22, 23, 43, 51, 56]. Some studies have shown that the implantation of interspinous devices in case of spinal canal stenosis or DDD had improved low back pain back [23, 43, 56], whereas in other studies these implants failed to show similar positive outcomes [22, 51]. The positive effect regarding low back pain in some of these studies might be related to a facet joint release.
In the present study, all of the operated patients with diagnosed LFJS at the level L4–5 profited substantially from interspinous distraction. These findings support the theory that in case of a singe level LFJS facet joint unloading can lead to a pain reduction. However, more than 24 months of follow-up period, a significant deterioration could be observed. The reason for the recurrence of pain is not quite clear. The patients suffered from a degenerative disease of the lumbar spine that can progress. We did not perform an infiltration of the facet joints at L4–5 at the 2-year follow-up. Thus, it is unclear whether the pain recurrence originates from the LFJS at L4–5 or from other causes as DDD or facet pain at adjacent levels. Furthermore, even if an LFJS is reconfirmed at the same level, the question arises what consequence the increase of pain should have. Should the patients undergo PFJD again or further surgery as fusion or dynamic screw-rod instrumentation? We would favor PFJD again as first treatment modality in these cases, because it is less invasive. Furthermore, the surgery required an anesthesiological team, two nurses in the operative room, hospitalization for at least 3 days, avoidance of heavy labor for at least 4 weeks (associated with loss of income in many cases during this period). The denervated patients were treated with the aid of one nurse at the outpatient department and could immediately return to normal activity. The costs for the insurances are about 23-fold higher for the operated patients. This reflects some of the socioeconomic costs comparing both procedures.
A further possibility of pain recurrence is the failure of the interspinous implant to maintain facet joint unloading for a longer period. In our study, three patients had an early secondary deterioration after Coflex implantation and received a semi-dynamic screw-rod instrumentation (Cosmic) that improved the pain again. All of them had a body weight of more than 100 kg. This might demonstrate that the total weight of the patient and duration of load have a major impact on the function of the device to unload the facet joints.
Radiological presentation
Distraction of the spinous processes by the interspinous device could lead to a non-lordotic alignment of the operated segment and thereby also influence the alignment of other spinal segments. The present study shows that the operated segment loses 2.1° of lordosis, while the adjacent segment gains 1.6° of lordosis. In a study using the DIAM interspinous device [22], a slight loss of lordosis of 2° was found in the operated segment on postoperative images. The moderate increase in lordosis in the superior adjacent segment found in the present study is probably a compensation for the kyphotic change in the operated segment.
Restriction of motion at the operated level by the interspinous device might lead to hypermobility of the adjacent segments. Radiographic evaluation of patients implanted with the Coflex device showed a significantly decreased ROM at the index level without effect on adjacent level ROM [23]. Biomechanical studies also support the finding that interspinous devices (Coflex, X-Stop) restrict ROM at the operated level without affecting the facet joint loading or disc pressure at adjacent levels [14, 48, 53]. Our data also showed a significant reduction in mobility at the operated segment. The postoperative increase in adjacent level ROM of 2.8° in the present study was significant, but with 4.8° was still in the physiological range. The ROM of the lumbar spine L1–5 also increased significantly by 5.3° in our study. Thus, our data are consistent with other studies showing no evidence of hypermobility of the adjacent level.
Conclusions
Facet joint infiltration is an appropriate way to detect and treat LFJS. The standard therapy should be a PFJD.
The implantation of an interspinous Coflex device in case of recurrent facet joint pain succeeds to unload the facet joints and to improve facet joint pain in clinical short- and mid-term settings, but it does not show any advantage over PFJD. Furthermore, considering the efforts and costs of surgery for this indication, a PJFD should be repeated in case of recurrent pain, before surgery is considered. The current Coflex device does not seem to be suitable for heavy patients.
Acknowledgments
We thank Dr. Nidal Toman, MD, and Mr. Sina Alavi for technical support. We would also like to thank Michael Hanna, PhD (Mercury Medical Research and Writing, New York) for editing the manuscript.
References
- 1.Andersen KH, Mosdal C, Vaernet K. Percutaneous radiofrequency facet denervation in low-back and extremity pain. Acta Neurochir (Wien) 1987;87(1–2):48–51. doi: 10.1007/BF02076015. [DOI] [PubMed] [Google Scholar]
- 2.Blumenthal S, McAfee PC, Guyer RD, Hochschuler SH, Geisler FH, Holt RT, Garcia R, Jr, Regan JJ, Ohnmeiss DD. A prospective, randomized, multicenter Food and Drug Administration investigational device exemptions study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part I: evaluation of clinical outcomes. Spine. 2005;30(14):1565–1575. doi: 10.1097/01.brs.0000170587.32676.0e. [DOI] [PubMed] [Google Scholar]
- 3.Bogduk N, Macintosh J, Marsland A. Technical limitations to the efficacy of radiofrequency neurotomy for spinal pain. Neurosurgery. 1987;20(4):529–535. doi: 10.1097/00006123-198704000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Bough B, Thakore J, Davies M, Dowling F. Degeneration of the lumbar facet joints: arthrography and pathology. J Bone Joint Surg (Br) 1990;72:275–276. doi: 10.1302/0301-620X.72B2.2138157. [DOI] [PubMed] [Google Scholar]
- 5.Cavanaugh JM, Ozaktay AC, Yamashita HT, King AI. Lumbar facet pain: biomechanics, neuroanatomy and neurophysiology. J Biomech. 1996;29(9):1117–1129. doi: 10.1016/0021-9290(96)00023-1. [DOI] [PubMed] [Google Scholar]
- 6.Christie SD, Song JK, Fessler RG. Dynamic interspinous process technology. Spine. 2005;30(16 Suppl):S73–S78. doi: 10.1097/01.brs.0000174532.58468.6c. [DOI] [PubMed] [Google Scholar]
- 7.Cobb JR (1948) In: Edwards JW (ed) Outlines for the study of scoliosis: instructional course lecture, vol 5. American Academy of Orthopedic Surgeons, Ann Arbor, pp 261–275
- 8.Cohen SP, Raja SN. Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology. 2007;106:591–614. doi: 10.1097/00000542-200703000-00024. [DOI] [PubMed] [Google Scholar]
- 9.Dreyfuss P, Halbrook B, Pauza K, Joshi A, McLarty J, Bogduk N. Efficacy and validity of radiofrequency neurotomy for chronic lumbar zygapophysial joint pain. Spine. 2000;25:1270–1277. doi: 10.1097/00007632-200005150-00012. [DOI] [PubMed] [Google Scholar]
- 10.Eisenstein SM, Parry CR. The lumbar facet arthrosis syndrome: clinical presentation and articular surface changes. J Bone Joint Surg Br. 1987;69(1):3–7. doi: 10.1302/0301-620X.69B1.2950102. [DOI] [PubMed] [Google Scholar]
- 11.Esses SI, Botsford DJ, Kostuik JP. The role of external spinal skeletal fixation in the assessment of low-back disorders. Spine. 1989;14:594–601. doi: 10.1097/00007632-198906000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Esses SI, Moro JK. The value of facet joint blocks in patient selection for lumbar fusion. Spine. 1993;18(2):185–190. doi: 10.1097/00007632-199302000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Floman Y, Millgram MA, Smorgick Y, Rand N, Ashkenazi E. Failure of the Wallis interspinous implant to lower the incidence of recurrent lumbar disc herniations in patients undergoing primary disc excision. J Spinal Disord Tech. 2007;20(5):337–341. doi: 10.1097/BSD.0b013e318030a81d. [DOI] [PubMed] [Google Scholar]
- 14.Fuchs PD, Lindsey DP, Hsu KY, Zucherman JF, Yerby SA. The use of an interspinous implant in conjunction with a graded facetectomy procedure. Spine. 2005;30(11):1266–1272. doi: 10.1097/01.brs.0000164152.32734.d2. [DOI] [PubMed] [Google Scholar]
- 15.Ghormley RK. Low back pain with special reference to the articular facets with presentation of an operative procedure. J Am Med Assoc. 1933;101:1773–1777. [Google Scholar]
- 16.Gibson JN, Grant IC, Waddel G. The Cochrane review of surgery for lumbar disc prolapses and degenerative lumbar spondylosis. Spine. 1999;24:1820–1832. doi: 10.1097/00007632-199909010-00012. [DOI] [PubMed] [Google Scholar]
- 17.Goldwaite JE. The lumbosacral articulation: an explanation of many cases of lumbago, sciatia, and paraplegia. Boston Med Surg J. 1911;164:365–372. [Google Scholar]
- 18.Hirsch C, Inglemark B, Miller M. The anatomical basis for low back pain. Acta Orthop Scand. 1963;33:1–17. doi: 10.3109/17453676308999829. [DOI] [PubMed] [Google Scholar]
- 19.Jackson RP. The facet syndrome: myth or reality? Clin Orthop Relat Res. 1992;279:110–121. [PubMed] [Google Scholar]
- 20.Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kettler A, Drumm J, Heuer F, Haeussler K, Mack C, Claes L, Wilke HJ. Can a modified interspinous spacer prevent instability in axial rotation and lateral bending? A biomechanical in vitro study resulting in a new idea. Clin Biomech (Bristol, Avon) 2008;23(2):242–247. doi: 10.1016/j.clinbiomech.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 22.Kim KA, McDonald M, Pik JHT, Khoureir P, Wang MY. Dynamic intraspinous spacer technology for posterior stabilization: case–control study on the safety, sagittal angulation, and pain outcome at 1-year follow-up evaluation. Neurosurg Focus. 2007;22(1):E7. [PubMed] [Google Scholar]
- 23.Kong DS, Kim ES, Eoh W. One-year outcome evaluation after interspinous implantation for degenerative spinal stenosis with segmental instability. J Korean Med Sci. 2007;22:330–335. doi: 10.3346/jkms.2007.22.2.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kumar MN, Jacquot F, Hall H. Long-term follow-up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J. 2001;10:309–313. doi: 10.1007/s005860000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leclaire R, Fortin L, Lambert R, Bergeron YM, Rossignol M. Radiofrequency facet joint denervation in the treatment of low back pain: a placebo controlled clinical trial to assess efficacy. Spine. 2001;26:1411–1417. doi: 10.1097/00007632-200107010-00003. [DOI] [PubMed] [Google Scholar]
- 26.Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine. 1988;13:375–377. doi: 10.1097/00007632-198803000-00029. [DOI] [PubMed] [Google Scholar]
- 27.Lewinnek GE, Warfield CA (1986) Facet joint degeneration as a cause of low back pain. Clin Orthop Relat Res (213):216–22 [PubMed]
- 28.Lippitt AB. The facet joint and its role in spine pain: management with facet joint injections. Spine. 1984;9:746–750. doi: 10.1097/00007632-198410000-00016. [DOI] [PubMed] [Google Scholar]
- 29.Lora J, Long DM. So-called facet denervation in the management of intractable back pain. Spine. 1976;1:121–126. doi: 10.1097/00007632-197606000-00006. [DOI] [Google Scholar]
- 30.Lord SM, Barnsley L, Bogduk N. The utility of comparative local anesthetic blocks versus placebo-controlled blocks for the diagnosis of cervical zygapophysial joint pain. Clin J Pain. 1995;11:208–213. doi: 10.1097/00002508-199509000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Lord SM, Barnsley L, Wallis BJ, McDonald GJ, Bogduk N. Percutaneous radio-frequency neurotomy for chronic cervical zygapophyseal-joint pain. N Engl J Med. 1996;335(23):1721–1726. doi: 10.1056/NEJM199612053352302. [DOI] [PubMed] [Google Scholar]
- 32.Lovely TJ, Rastogi P. The value of provocative facet blocking as a predictor of success in lumbar spine fusion. J Spinal Disord. 1997;10:512–517. doi: 10.1097/00002517-199712000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Lynch MC, Taylor JF. Facet joint injection for low back pain: a clinical study. J Bone Joint Surg. 1986;68:138–141. doi: 10.1302/0301-620X.68B1.2934398. [DOI] [PubMed] [Google Scholar]
- 34.Maigne R, Le Corre F, Judet H. Low back pain of dorse-lumbar origin: surgical treatment of posterior articular capsule excision (author’s transl) Nouv Presse Med. 1978;7(7):565–568. [PubMed] [Google Scholar]
- 35.McCulloch JA, Organ LW. Percutaneous radiofrequency lumbar rhizolysis. Can Med Assoc J. 1977;116:30–32. [PMC free article] [PubMed] [Google Scholar]
- 36.North RB, Han M, Zahurak M, Kidd DH. Radiofrequency lumbar facet denervation: analysis of prognostic factors. Pain. 1994;57:77–83. doi: 10.1016/0304-3959(94)90110-4. [DOI] [PubMed] [Google Scholar]
- 37.Phillips FM, Voronov LI, Gaitanis IN, Carandang G, Havey RM, Patwardhan AG. Biomechanics of posterior dynamic stabilizing device (DIAM) after facetectomy and discectomy. Spine J. 2006;6(6):714–722. doi: 10.1016/j.spinee.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 38.Privat JM, Bouvier JP, Benezech J (1980) Facet syndrome: pathologie articulaire posterieure et sciatique. In: Simon L (ed) La Sciatique et le Nerf Sciatique, Masson, Paris, pp 182–189
- 39.Rashbaum RF. Radiofrequency facet denervation: a treatment alternative in refractory low back pain with or without sciatica. Orthop Clin N Am. 1983;14:569–575. [PubMed] [Google Scholar]
- 40.Rees WES. Multiple bilateral subcutaneous rhizolysis of segmental nerves in the treatment of the intervertebral disc syndrome. Ann Gen Pract. 1971;26:126–127. [Google Scholar]
- 41.Schlegel JD, Smith JA, Schleusener RL. Lumbar motion segment pathology adjacent to thoracolumbar, lumbar and lumbosacral fusions. Spine. 1996;21:970–981. doi: 10.1097/00007632-199604150-00013. [DOI] [PubMed] [Google Scholar]
- 42.Schofferman J, Kine G. Effectiveness of repeated radiofrequency neurotomy for lumbar facet pain. Spine. 2004;29:2471–2473. doi: 10.1097/01.brs.0000143170.47345.44. [DOI] [PubMed] [Google Scholar]
- 43.Sénégas J. Mechanical supplementation by non-rigid fixation in degenerative intervertebral lumbar segments: the Wallis system. Eur Spine J. 2002;11(Suppl 2):164–169. doi: 10.1007/s00586-002-0423-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shealy CN. The role of the spinal facets in back and sciatic pain. Headache. 1974;14:101–110. doi: 10.1111/j.1526-4610.1974.hed1402101.x. [DOI] [PubMed] [Google Scholar]
- 45.Shealy CN. Percutaneous radiofrequency denervation of spinal facets: treatment for chronic back pain and sciatica. J Neurosurg. 1975;43:448–451. doi: 10.3171/jns.1975.43.4.0448. [DOI] [PubMed] [Google Scholar]
- 46.Shealy CN. Facet denervation in the management of back and sciatic pain. Clin Orthop Relat Res. 1976;115:157–164. [PubMed] [Google Scholar]
- 47.Staender M, Maerz U, Tonn JC, Steude U. Computerized tomography-guided kryorhizotomy in 76 patients with lumbar facet joint syndrome. J Neurosurg Spine. 2005;3(6):444–449. doi: 10.3171/spi.2005.3.6.0444. [DOI] [PubMed] [Google Scholar]
- 48.Tsai KJ, Murakami H, Lowery GL, Hutton WC. A biomechanical evaluation of an interspinous device (Coflex) used to stabilize the lumbar spine. J Surg Orthop Adv. 2006;15(3):167–172. [PubMed] [Google Scholar]
- 49.Kleef M, Barendse GA, Kessels A, Voets HM, Weber WE, Lange S. Randomized trial of radiofrequency lumbar facet denervation for chronic low back pain. Spine. 1999;24:1937–1942. doi: 10.1097/00007632-199909150-00013. [DOI] [PubMed] [Google Scholar]
- 50.Wijk RM, Geurts JW, Wynne HJ, Hammink E, Buskens E, Lousberg R, Knape JT, Groen GJ. Radiofrequency denervation of lumbar facet joints in the treatment of chronic low back pain: a randomized, double-blind, sham lesion controlled trial. Clin J Pain. 2005;21:335–344. doi: 10.1097/01.ajp.0000120792.69705.c9. [DOI] [PubMed] [Google Scholar]
- 51.Verhoof OJ, Bron JL, Wapstra FH, Royen BJ. High failure rate of the interspinous distraction device (X-Stop) for the treatment of lumbar spinal stenosis caused by degenerative spondylolisthesis. Eur Spine J. 2008;17(2):188–192. doi: 10.1007/s00586-007-0492-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Weiner BK. Interspinous process decompression system (X STOP) device affords superior outcomes and equal safety to nonoperative therapy. Spine. 2005;30(24):2846–2847. doi: 10.1097/01.brs.0000192198.13867.69. [DOI] [PubMed] [Google Scholar]
- 53.Wiseman CM, Lindsey DP, Fredrick AD, Yerby SA. The effect of an interspinous process implant on facet loading during extension. Spine. 2005;30(8):903–907. doi: 10.1097/01.brs.0000158876.51771.f8. [DOI] [PubMed] [Google Scholar]
- 54.Zigler J, Delamarter R, Spivak JM, Linovitz RJ, Danielson GO, 3rd, Haider TT, Cammisa F, Zuchermann J, Balderston R, Kitchel S, Foley K, Watkins R, Bradford D, Yue J, Yuan H, Herkowitz H, Geiger D, Bendo J, Peppers T, Sachs B, Girardi F, Kropf M, Goldstein J. Results of the prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential fusion for the treatment of 1-level degenerative disc disease. Spine. 2007;32(11):1155–1162. doi: 10.1097/BRS.0b013e318054e377. [DOI] [PubMed] [Google Scholar]
- 55.Zucherman JF, Hsu KY, Hartjen CA, Mehalic TF, Implicito DA, Martin MJ, Johnson DR, 2nd, Skidmore GA, Vessa PP, Dwyer JW, Puccio S, Cauthen JC, Ozuna RM. A prospective randomized multi-center study for the treatment of lumbar spinal stenosis with the X STOP interspinous implant: 1-year results. Eur Spine J. 2004;13(1):22–31. doi: 10.1007/s00586-003-0581-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zucherman JF, Hsu KY, Hartjen CA, Mehalic TF, Implicito DA, Martin MJ, Johnson DR, 2nd, Skidmore GA, Vessa PP, Dwyer JW, Puccio S, Cauthen JC, Ozuna RM. A multicenter, prospective, randomized trial evaluating the X STOP interspinous process decompression system for the treatment of neurogenic intermittent claudication: two-year follow-up results. Spine. 2005;30(12):1351–1358. doi: 10.1097/01.brs.0000166618.42749.d1. [DOI] [PubMed] [Google Scholar]