Abstract
Spinal cord injury (SCI) is a devastating condition for individual patients and costly for health care systems requiring significant long-term expenditures. Cytokine erythropoietin (EPO) is a glycoprotein mediating cytoprotection in a variety of tissues, including spinal cord, through activation of multiple signaling pathways. It has been reported that EPO exerts its beneficial effects by apoptosis blockage, reduction of inflammation, and restoration of vascular integrity. Neuronal regeneration has been also suggested. In the present review, the pathophysiology of SCI and the properties of endogenous or exogenously administered EPO are briefly described. Moreover, an attempt to present the current traumatic, ischemic and inflammatory animal models that mimic SCI is made. Currently, a clearly effective pharmacological treatment is lacking. It is highlighted that administration of EPO or other recently generated EPO analogues such as asialo-EPO and carbamylated-EPO demonstrate exceptional preclinical characteristics, rendering the evaluation of these tissue-protective agents imperative in human clinical trials.
Keywords: Animal models, Clinical trials, Erythropoietin, Neuroprotection, Spinal cord injury
Introduction
In about 2,500 BC, in the Edwin Smith papyrus, an Egyptian physician accurately described the clinical features of traumatic tetraplegia and revealed an awareness of the awful prognosis with the advice: “an ailment not to be treated.” Nowadays, the annual incidence of spinal cord injury (SCI) within the United Kingdom is about 10–15 per million of the population. Road traffic accidents account for 45% of the cases, while domestic and industrial ones for 34% [69]. In the United States, 11,000 new cases of SCI are reported each year, over half of which occur among individuals under 30 years of age [13]. Aside from the incalculable human pain, the cost of medical care for patients with SCI is estimated at over 4 billion dollars per year [51].
At present, an indisputably effective therapy for SCI is lacking. The sole standard therapeutic intervention for such patients is the synthetic glucocorticosteroid methylprednisolone sodium succinate (MPSS) [13]. Nonetheless, even this regimen has been called into question in recent years since it may have potentially deleterious effects on early mortality and morbidity [3].
Currently, various other pharmacological agents for limiting SCI consequences are under evaluation in animals and humans [9]. One of the most promising candidates is erythropoietin (EPO), a hematopoietic growth factor produced mainly by kidney and fetal liver, which stimulates proliferation and differentiation of erythroid precursor cell [45]. In addition, a recent clinical trial reported substantial improvement in outcome of stroke patients with non-hemorrhagic infarcts within the distribution of the middle cerebral artery treated with recombinant human EPO (rhEPO) intravenously within 8 h of the onset of symptoms [28]. SCI is believed to share many pathophysiological features with brain injury and recent studies in animal models indicate that EPO is very effective in enhancing neurological recovery after experimental SCI [18, 36, 43, 66].
The scope of this review is to bring forward the results of these studies and highlight the future development of non-hematopoietic EPO analogues with a safe pharmacological profile for use in the clinical practice. A brief description of the EPO glycoprotein and the currently available animal models to simulate SCI patterns is also attempted.
Erythropoietin
Historical background
It was in 1906 that Carnot and DeFlandre [16, 45] reported the presence of reticulocytosis in normal rabbits injected with plasma from anemic ones and thus postulated a humoral factor they named hemopoietin. The existence of this factor was confirmed by Hjort in 1936 [40], Krumdieck in 1943 [50] and Erslev in 1953 [31] but it was Bonsdorf and Jalavisto in 1948 [10] that first used the term erythropoietin. In 1950, Reissman [64] showed that hypoxia stimulated the erythropoietin production and a few years later kidney was reported to be the site of erythropoietin production [45]. In 1977, Miyake et al. [63] isolated EPO from the urine of anemic patients, and the identification of its amino acid sequence enabled scientists to synthesize EPO DNA probes for isolation and cloning of the EPO gene. The road for rhEPO production had opened [45].
Structure of EPO and EPO’s receptor
The gene encoding EPO occupies a 5.4-kb region [56] and is located on chromosome 7q11–q22 [76]. It contains five exons and four introns coding for the prohormone of 193 amino acids [41]. From the latter comes the mature glycoprotein hormone (EPO) which consists of 165 amino acids with a molecular weight of 30.4 kDa [52]. EPO presents a tertiary conformation analogous to that of interleukin-6, growth hormone and prolactin [6].
The receptor of EPO (EPO-R) belongs to the type I family of single-transmembrane cytokine receptors [45]. The corresponding gene is located on chromosome 19p with eight exons and seven introns, encoding a 507 amino acid peptide with a molecular weight of 66 kDa [77].
Production and site of action
In intrauterine life, EPO is produced by liver until late gestation, when a switch is gradually initiated from liver to kidneys [38]. The latter subsequently become the primary sites of EPO synthesis [45]. In these organs mRNA is expressed in interstitial cells of the peritubular capillary bed with fibroblast-like characteristics [55]. In addition, liver contributes to 10–15% of circulating plasma levels [32]. Minimal expression of EPO mRNA has also been demonstrated in the brain cortex, cerebellum, hippocampus, pituitary gland [68, 78], placenta [23], testes, spleen, and lung [70]. EPO is mainly crucial for the survival, proliferation, and differentiation in the erythrocytic lineage [45]. Yet, it is involved in other kinds of cells such as megakaryocytic [79] and neural ones [59] and in human bronchial tumors [47] as well. It is also thought to play a role in brain development [57].
Spinal cord injury
The response to SCI develops in two steps; the first being the injury itself leading to direct damage of the nervous tissue, while the second represents all the events that amplify the early primary lesion [33]. The experimental animal models that facilitate the understanding of SCI pathogenesis and the sequential phenomena observed in recent animal studies are presented in the following section.
Animal models
There are several animal models trying to mimic human SCI; the trauma, the ischemia and the inflammation models [13]. This categorization was based on the fact that SCI is seen as the result of ischemia, inflammation and apoptosis processes spreading away from the lesion as a function of time [61].
Trauma models
These models employ techniques of transection, compression and, contusion. In transection, spinal cord (SC) is cut at various degrees [48], but since the majority of human SCI is associated with SC compression, this method does not seem suitable for evaluating treatment options. Yet, it is also supported that such dismission of transaction models is inappropriate because these models allow a much clearer analysis of the cellular effects of trauma, and also of the effects of the potential therapies, since they are much less complex. Compression is carried out by means of a modified aneurismal clip, forceps or applying weight on exposed SC [4, 19, 36]. Contusion is caused by either displacing SC or hitting it with a dropped weight (steel rod) and is characterized by more extensive damage [11, 33, 37, 43, 62, 74, 75]. The squeezing of the nerve roots has also been reported, usually in the lumbar region using forceps and leading to allodynia [66].
Ischemia models
Transient occlusion of the aorta with a clip or forceps results in temporary block in SC blood flow. This complication was adequately demonstrated in heart surgery operations. The primary targets of damage due to the inducted ischemia are motor neurons in the ventral horn of SC [18, 68].
Inflammation models
Inflammation as a result of autoimmune disease has been also studied. Experimental autoimmune encephalitis (EAE) is a good example [1]. This disease is induced in animals by immunization against myelin basic protein or myelin oligodendrocyte glycoprotein [15]. Symptoms range from ataxia to death and multiple doses of pharmaceutical treatment are needed as opposed to blunt trauma which is treated with a single dose [13].
Pathophysiology and pathology of SCI
The primary damage to the SC may injure or even kill neurons, axons and blood vessels at the site of injury, leading to vasoconstriction, hemorrhage, and ischemia [72]. The primary injury is followed by a cascade of secondary damage including fluid-electrolyte imbalance, regional blood flow alterations, calcium-mediated cellular injury, free radical generation, glutamate-induced excitoxicity, disturbances in mitochondrion function, pro-inflammatory cytokine production and apoptotic cell death. Inflammatory cells such as neutrophils, macrophages, and resident microglia are attracted by the dead cells and further amplify injury by releasing pro-inflammatory cytokines at the site of injury [61]. As a result, these secondary mechanisms damage SC tissue that was otherwise spared during the initial insult [72].
In SCI an attempt to limit the spread of cellular damage is represented by the creation of a safe zone (penumbra) by triggering nervous cells surrounding the focal lesion [30]. A delayed and widespread oligodendrocyte apoptosis and demyelination of long spinal tracts in the white matter follows [27]. This time delay in oligodendrocytic cell death offers an opportunity for pharmacological intervention improving clinical outcome and rendering EPO an important factor in determining the size of the penumbra [13].
During the weeks following trauma, the site of SCI is characterized by disrupted axons and a cystic cavity encased within a glial scar. Intact tissue surrounding the lesion is found in variable amounts. It is in this intact tissue that neurons are found either uninjured or with part of their myelin sheaths lost. These neurons have the potential to regenerate axons. Nonetheless, axonal regeneration frequently fails for two reasons; first, elements within the lesion environment inhibit axonal growth and second, neurons of the central nervous system themselves exhibit a weak intrinsic ability to regenerate axons after trauma [3, 13].
EPO in SCI
Erythropoietin and EPO-R have been documented to play important roles in SCI. This is the case for both endogenous and exogenously administered EPO [38]. The proposed mechanisms of action and some implications regarding human trials are discussed hereby.
Endogenous EPO
Under normal conditions, EPO seems to contribute to the development of the nervous system. Many studies have proven the expression of EPO and EPO-R in neurons and glial cells in fetal SC [42] and others suggested that even after birth the SC expresses molecules in a cell type specific manner consistent with a paracrine–autocrine role, with the ligand located close to its target [13]. Researchers demonstrated EPO-R localization on capillaries within the white matter and on bodies and proximal dendrites of motor neurons of the ventral horn surrounded by a dense plexus of EPO-immunoreactive fibers [18, 66].
Of great clinical importance is also the expression of EPO after SCI. This expression is part of the physiological response to hypoxia. EPO has been shown not only to protect neuronal cells in vitro from apoptosis induced by hypoxia, but also from excitotoxins and glucose deprivation [13, 17]. Evidence suggested the positive effect of EPO even in the prevention of radiation-induced SCI [2]. Interestingly, Bemaudin et al. [7] reported that within the penumbra surrounding ischemic brain lesions, cells expressed increased levels of EPO and EPO-R. EPO-R upregulation occurred first in neurons and endothelial cells of the microcirculation, and was followed by an increase in EPO expression by astrocytes and neurons as well. Thereafter a phenomenon of delayed preconditioning is believed to occur, that is an augmentative resistance to future stressful stimuli [25]. EPO, by inhibiting apoptosis, reduces the inflammatory response, and this in turn reduces secondary injury [14]. Yet, the expression of EPO in the penumbra is limited by the long latency for EPO production and pro-inflammatory cytokines directly inhibiting EPO production, thus rendering cell death ineluctable [60].
Exogenously administered EPO
The aforementioned problems are surpassed with the administration of exogenous rhEPO which has been suggested to produce substantial neuroprotection in animal models of traumatic SCI [4, 11, 19, 33, 36, 37, 39, 43, 44, 62, 74, 75], spinal nerve root crush injury [66], transient SC ischemia [18, 68], and SC inflammation in EAE [1]. The principal findings of the above studies are shown in Table 1.
Table 1.
Animal models evaluating exogenously administered EPO
| Study | Model | Method | Findings |
|---|---|---|---|
| King et al. [48] | Hemisection injury (rats) | SC hemisection extending from the midline to the lateral edge of SC at T10/T11 level | Three days post-injury: both EPO and CEPO reduced the size of lesion, the number of apoptotic nuclei around lesion, the number of axons expressing the injury marker β-amyloid precursor protein |
| Administration of EPO and CEPO intraperitoneally 30 min and 24 h after injury | Both compounds increased Schwann cell infiltration into the lesion site | ||
| None of them had any effect on macrophage infiltration within either the lesion site or surrounding intact tissue | |||
| Gorio et al. [36] | Compression—contusion injury (rodents) | Employment of modified aneurysm clip | At 28 days treated animals exhibited substantially superior clinical outcome |
| Impaction with a steel rod | Compression model: improvement 12 h after treatment | ||
| Administration of rhEPO via an intraperitoneal injection immediately after injury | Contusion model: myelinated axons appeared histologically normal—no apoptotic oligodendrocytes in the region of the fasciculus cuneatus—reduction in the number of inflammatory cells in and around the site of injury | ||
| Arishima et al. [4] | Compression injury (rats) | Induction of injury by the static load technique | Decrease of apoptotic neurons and oligodendrocytes as early as 6 h after SCI |
| Administration of EPO intraperitoneally 15 min and 24 h after compression | Decrease of active caspase-3 immunoreactive cells | ||
| Cetin et al. [19] | Compression injury (rats) | Employment of aneurysm clip at T3 level | Significant decrease of ischemic damage |
| Administration of rhEPO intraperitoneally 5 min after injury | Best neurological, functional and histopathological recovery was documented with the combined administration of rhEPO and MPSS | ||
| Comparison with MPSS | |||
| Fumagalli et al. [33] | Contusion injury (rats) | Impaction with a steel rod at T9 level | Three days after injury: only EPO up-regulated the NGF gene expression both caudally and rostrally to the lesion site enhancing the regenerative process |
| Administration of rhEPO via an intraperitoneal injection within 30 min after injury | |||
| Investigation of NGF expression | Seven days after injury: both EPO and MPSS enhanced NGF mRNA levels at the epicenter of the lesion | ||
| Comparison with MPSS | |||
| Okutan et al. [62] | Contusion injury (rats) | Impaction with a steel rod | Increase of MPO and caspase-3 activity after SCI |
| Administration of rhEPO via an intraperitoneal injection immediately after injury | Decrease of MPO and caspase-3 activity in animals treated either by rhEPO or MPSS | ||
| Significant early functional recovery | |||
| Determination of MPO and caspase-3 activity | EPO presented substantial anti-apoptotic and anti-inflammatory effects | ||
| Comparison with MPSS | |||
| Vitellaro-Zuccarello et al. [75] | Contusion injury (rats) | Impaction with a steel rod | Attenuation of astrogliosis |
| Administration of rhEPO via an intraperitoneal injection 30 min after injury | Influence on the expression of aquaporin 4 (astrocytic water channel) with beneficial effect for the resolution of edema | ||
| Investigation of chronic (1 month) EPO-mediated effects | |||
| Vitellaro-Zuccarello et al. [74] | Contusion injury (rats) | Impaction with a steel rod | Better preservation of myelin in the ventral white matter |
| Administration of rhEPO via an intraperitoneal injection 30 min after injury | Generation of new myelinating oligodendrocytes | ||
| Increased density of the serotonergic plexus around motor neurons (sparing of fiber tracts) | |||
| Investigation of: myelin preservation, activation of oligodendrocyte progenitors, ventral horn density of serotonergic plexus | |||
| Boran et al. [11] | Contusion injury (rats) | Steel bullet dropped through a tube onto the dorsal surface of SC | Enhancement of neurological recovery |
| Administration of rhEPO intraperitoneally within 60 min after SCI | EPO provided better results than MPSS | ||
| Comparison with MPSS | |||
| Gorio et al. [37] | Contusion injury (rats) | Impaction with steel rod | Both EPO and MPSS suppressed proinflammatory cytokines |
| Administration of EPO intravenously | Only EPO was associated with reduced microglial infiltration, attenuated scar formation and sustained neurological improvement in 1 month | ||
| Comparison with MPSS | Co-administration of MPSS antagonized the protective effects of EPO | ||
| Kaptanoglu et al. [43] | Contusion injury (rodents) | Impaction with a steel rod | Preservation of the SC ultrastructure as determined by electron microscope |
| Intraperitoneal administration of rhEPO | RhEPO and MPSS gave similar results | ||
| Comparison with MPSS | EPO was more effective than MPSS in inhibiting SCI-induced lipid peroxidation | ||
| Sekiguchi et al. [66] | Nerve root crush injury (rats) | L5 dorsal root ganglia exposed and the nerves crushed with forceps | Although EPO was not initially protective, it significantly increased the recovery rate from mechanical allodynia after 7 days |
| Administration of rhEPO subcutaneously 1 day before injury and daily after that | 50% of ipsilateral hindpaws in untreated animals demonstrated allodynia, but only 12.5% of animals treated with rhEPO | ||
| Sönmez et al. [68] | Transient ischemia (rats) | Inflation of balloon below the branching point of left subsclavian artery | Attenuation of neuronal injury |
| Administration of rhEPO intravenously immediately after the onset of reperfusion | Potentiation of the expression of transcription factor pCREB in anterior horn of SC | ||
| Celik et al. [18] | Transient ischemia (rabbits) | Infrarenal aorta exposed and non-traumatically occluded | Significant amelioration in neurological damage within 1 h of treatment |
| Lack of histological evidence of injury | |||
| Treatment with rhEPO intravenously immediately after the release of occlusion | Motor neurons negative for TUNEL labeling (a marker of apoptosis) | ||
| Agnello et al. [1] | Inflammation in EAE (rats) | Induction of the disease by immunization with MBP | Delay of onset of EAE |
| Administration of rhEPO intraperitoneally daily from day 3 after immunization with MBP | Reduced inflammation and glial activation/proliferation | ||
| Clinical effects maintained without further EPO administration for at least 2 months |
NGF nerve growth factor, MPO myeloperoxidase, MBP myelin basic protein
Mechanisms of action
Erythropoietin has been shown to bind to a receptor complex that includes the EPO-R and the β common receptor, a receptor subunit of interleukin (IL)-3, IL-5 and granulocyte macrophage (GM) colony stimulating factor receptors [48]. The exact mechanisms by which EPO exhibits its neuroprotective effects are not fully understood. Yet, apoptosis blockage, reduction of inflammation, and restoration of vascular integrity, among others, have all been implicated as possible mechanisms [13, 29, 67].
Apoptosis blockage
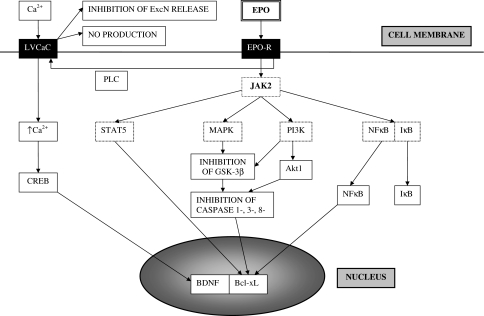
In vitro, EPO protects neurons from cell death induced by hypoxia and a variety of other agents, including excitotoxins and glucose deprivation [13]. In vivo, following a crush injury of a spinal nerve root, EPO prevented apoptosis in dorsal root ganglion neurons [49, 66], while in a transient SC ischemia model, there was no detectable apoptotic pattern (no TUNEL labeling present) in ventral horn motor neurons [18]. The preventive effect of EPO on SC cell apoptosis was also demonstrated in a compression model in rats [4]. In confirmation, studies suggested an absence of inflammatory cells probably due to inhibition of apoptosis and of caspase-1, which constitutes a member of the inflammation process. Moreover, several pathways may be responsible for EPO’s antiapoptotic effects. Research implies the activation of Janus kinase-2 (Jak2) and signal transducer and activator of transcription-5, which in turn induce survival proteins such as Bcl-xL [13, 24]. Phosphatidylinositol-3 kinase (PI3K) is also activated in the UT-7 leukemia cell line, where it recruits protein kinase B (Akt) [44]. This PI3K-Akt pathway results in Bcl-xL upregulation [54] and mediates antiapoptotic signaling through platelet-derived growth factor by employing Nuclear Factor-κΒ (NF-κB) after the inhibition of the inhibitor of κB [45, 65]. In addition, Jak2 activates Ras-mitogen-activated protein-kinases (MAPKs) which in turn inhibit the glycogen-synthase kinase 3β (GSK3β) leading to inhibition of caspase activation [12, 22]. Finally, phospholipase (PLC) is involved in the modulation of the activity of low-voltage calcium channels (LVCaC), thereby augmenting nitric oxide (NO) production and reducing the release of excitatory neurotransmitters [12, 35]. Moreover, brain-derived neurotrophic factor’s expression is induced by activation of these LVCaC and recruitment of the Ca2+-sensitive transcription factor Ca2+/cAMP-response element-binding protein [5]. The intracellular signal transduction pathways activated by the EPO-R are presented in Fig. 1.
Fig. 1.
Intracellular signaling events activated by the EPO-R [5, 12, 22, 35]
Reduction of inflammation
Although MPSS and ganglioside GMl do not reduce the infiltration of neutrophils after SCI [71], EPO seems to achieve such a reduction [1, 36]. The anti-inflammatory effects of EPO could not be explained by antagonism of inflammatory cytokines but rather by an antiapoptotic effect on neurons. More precisely, neurons that were exposed to trimethyltin, an apoptosis inducing toxin, released factors that stimulated tumor necrosis factor (TNF) production by glial cells. EPO inhibited this TNF production [73]. Other studies [8] demonstrated that NF-kB was up-regulated after SCI by macrophages, endothelial cells, and neurons and EPO has been suggested to engage both the NF-κB and the Jak2 pathway [45]. In conclusion, cross-talk appears to exist between antiapoptotic and anti-inflammatory actions of EPO [13, 26].
Restoration of vascular integrity
Erythropoietin has been found to antagonize the apoptosis of endothelial cells through activation of Aktl and mitochondrial modulation of cysteine proteases [21], stimulate mitogenesis and support angiogenesis against VEGF-induced permeability for improving tissue oxygenation [13] and strengthen the tight junctions of endothelial cells [13, 58].
Other mechanisms
Erythropoietin’s beneficial effects are due to limitation of damage following SCI and enhancement of neuronal regeneration. Activation of the EPO confers a variety of phenomena; reduction of calcium influx upon depolarization and synaptic vesicle release of neurotoxic glutamate [46]; increase of astrocyte production of glutathione peroxidase [34]; reduction of lipid peroxidation by-products [43]. Neural stem cells present in SC proliferate to form spheres of undifferentiated cells that produce neurons, astrocytes, and oligodendrocytes [13]. Cultured stem cells when exposed to EPO produced two to threefold more neurons [67]. Thus, EPO might contribute to recovery after SCI by increasing the number of new neurons [13].
Human trials
Anemia encountered in patients with renal failure, cancer and surgery has been successfully and safely treated with rhEPO [45]. Results of studies in animal models indicated the effectiveness of treatment with rhEPO in SCI [1, 18, 36, 43, 66], even if when rhEPO was administered up to 24 h after the initial SCI. However, the time of rhEPO administration seems to be correlated with the necessary number of doses, that is when rhEPO was provided immediately after SCI, one dose was enough for amelioration of neurological outcome. On the other hand, in case of delay of treatment with subsequent multiple pathways’ activation, multiple doses were more effective [13].
The question of demonstrating similar results in humans should be now addressed. For example, an intriguing finding in recent studies was that MPSS was not as effective as rhEPO in SCI animal models [43]. In contradistinction, MPSS has been reported to have some effect when administered within 8 h after SCI in humans, but is associated with a worse outcome when administered later [30].
A major concern expressed by clinicians is that besides the tissue protective effects, EPO demonstrates also hematopoietic activity, increasing the risk for thrombosis after the administration of multiple doses of this glycoprotein. Several EPO analogues have been brought into light as an attempt to address this concern. There are two key concepts in their production; plasma half-life and interaction with different receptors [13, 39].
To start with, administration of short-lived asialo-erythropoietin (asialo-EPO), generated by total enzymatic desialylation of EPO [48], was protective in animal models of stroke, SCI and peripheral neuropathy without increasing erythrocyte mass [39]. In addition, asialo-EPO was as effective as rhEPO in normalizing motor function after SCI using an aneurysm clip model [29]. These findings confirmed the formulated hypothesis that a short-lived EPO could initiate neuroprotection but not survive long enough to stimulate erythropoiesis [13].
While asialo-EPO binds to the same receptor as EPO, carbamylated EPO (CEPO) and other EPO mutants do not bind to this receptor. This property confers loss of hematopoietic activity in human cell cultures or upon chronic dosing in animal models [13]. CEPO’s neuroprotective functions were demonstrated in two animal models of SCI. In the first model of SC compression, neuroprotection was documented even when the first dose was given with a delay of 2 or 3 days after injury. In the second model of mice immunized with myelin oligodendrocyte glycoprotein to induce EAE, amelioration of neurological dysfunction was also observed [53].
Epilogue
Compounds employed in the evaluation of SCI treatment include MPSS, tirilazad mesylate, naloxone, GM-1 ganglioside, lazaroids, free radical scavengers, and various receptor antagonists, all of which attempt to limit secondary damage [3, 43]. Recently, research has focused on rhEPO and its non-erythropoietic derivatives (when several doses are under consideration) investigating their antiapoptotic, and anti-inflammatory functions as well as their role in restoring vascular integrity [38, 53]. Moreover, researchers suggested a contribution of EPO to neurons regeneration [67]. The remarkable safety profile of rhEPO therapy in anemia and the demonstration of rhEPO and its analogues’ broad neuroprotective effects in animal models should encourage the design of clinical trials to assess the efficacy of therapy of these proteins on isolated SCI [45].
Clinical evaluation end points should include besides quality of life assessment, motor, sensory and autonomic function [13]. Finally, the employment of the EPO 3′ untranslated region as a specific system for hypoxia-inducible gene therapy of several neurological disorders including SCI shows that a new era of innovative therapeutical approaches in SCI has emerged [20].
Conflict of interest statement
None.
References
- 1.Agnello D, Bigini P, Villa P, Mennini T, Cerami A, Brines ML, et al. Erythropoietin exerts an anti-inflammatory effect on the CNS in a model of experimental autoimmune encephalomyelitis. Brain Res. 2002;952:128–134. doi: 10.1016/S0006-8993(02)03239-0. [DOI] [PubMed] [Google Scholar]
- 2.Akyurek S. The effect of erythropoietin in the prevention of radiation-induced spinal cord damage. Med Hypotheses. 2007;68:238–239. doi: 10.1016/j.mehy.2006.05.040. [DOI] [PubMed] [Google Scholar]
- 3.American Association of Neurological Surgeons Pharmacological therapy after acute cervical spinal cord injury. Neurosurgery. 2002;50:S63–S72. doi: 10.1097/00006123-200203001-00013. [DOI] [PubMed] [Google Scholar]
- 4.Arishima Y, Setoguchi T, Yamaura I, Yone K, Komiya S. Preventive effect of erythropoietin on spinal cord cell apoptosis following acute traumatic injury in rats. Spine. 2006;31:2432–2438. doi: 10.1097/01.brs.0000239124.41410.7a. [DOI] [PubMed] [Google Scholar]
- 5.Bartesaghi S, Marinovich M, Corsini E, Galli CL, Viviani B. Erythropoietin: a novel neuroprotective cytokine. Neurotoxicology. 2005;26:923–928. doi: 10.1016/j.neuro.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 6.Bazan JF. Haemopoietic receptors and helical cytokines. Immunol Today. 1990;11:350–354. doi: 10.1016/0167-5699(90)90139-Z. [DOI] [PubMed] [Google Scholar]
- 7.Bernaudin M, Marti HH, Roussel S, Divoux D, Nouvelot A, Mackenzie ET, et al. A potential role for erythropoietin in focal permanent cerebral ischemia in mice. J Cereb Blood Flow Metab. 1999;19:643–651. doi: 10.1097/00004647-199906000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Bethea JR, Castro M, Keane RW, Lee TT, Dietrich WD, Yezierski RP. Traumatic spinal cord injury induces nuclear factor-kappaB activation. J Neurosci. 1998;18:3251–3260. doi: 10.1523/JNEUROSCI.18-09-03251.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blight AR, Zimber MP. Acute spinal cord injury: pharmacotherapy and drug development perspectives. Curr Opin Investig Drugs. 2001;2:801–808. [PubMed] [Google Scholar]
- 10.Bonsdorf E, Jalavisto E. A humoral mechanism in anoxic erythrocytosis. Acta Physiol Scand. 1948;16:150–170. doi: 10.1111/j.1748-1716.1948.tb00535.x. [DOI] [Google Scholar]
- 11.Boran BO, Colak A, Kutlay M. Erythropoietin enhances neurological recovery after experimental spinal cord injury. Restor Neurol Neurosci. 2005;23:341–345. [PubMed] [Google Scholar]
- 12.Brines M, Cerami A. Emerging biological roles for erythropoietin in the nervous system. Natl Rev. 2005;6:484–494. doi: 10.1038/nrn1687. [DOI] [PubMed] [Google Scholar]
- 13.Brines M, Cerami A. Erythropoietin in spinal cord injury. In: Höke A, editor. Erythropoietin and the nervous system. Novel therapeutic options for neuroprotection. New York: Springer; 2006. pp. 147–164. [Google Scholar]
- 14.Brines ML, Ghezzi P, Keenan S, Agnello D, Lanerolle NC, Cerami C, et al. Erythropoietin crosses the blood-brain barrier to protect against experimental brain injury. Proc Natl Acad Sci USA. 2000;97:10526–10531. doi: 10.1073/pnas.97.19.10526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burkhardt H, Kalden JR. Animal models of autoimmune diseases. Rheumatol Int. 1997;17:91–99. doi: 10.1007/s002960050015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carnot C, DeFlandre C. Sur l’ activité hémopoiétique du sérum au cours de la régénération du sang. CR Acad Sci Paris. 1906;143:432–435. [Google Scholar]
- 17.Castillo M, Yan E, Walker DW. Expression of erythropoietin and its receptor in the brain of late-gestation fetal sheep, and responses to asphyxia caused by umbilical cord occlusion. Dev Neurosci. 2005;27:220–227. doi: 10.1159/000085995. [DOI] [PubMed] [Google Scholar]
- 18.Celik M, Gokmen N, Erbayraktar S, Akhisaroglu M, Konakc S, Ulukus C, et al. Erythropoietin prevents motor neuron apoptosis and neurologic disability in experimental spinal cord ischemic injury. Proc Natl Acad Sci USA. 2002;99:2258–2263. doi: 10.1073/pnas.042693799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cetin A, Nas K, Bãyãkbayram H, Ceviz A, Olmez G. The effects of systemically administered methylprednisolone and recombinant human erythropoietin after acute spinal cord compressive injury in rats. Eur Spine J. 2006;15:1539–1544. doi: 10.1007/s00586-006-0091-2. [DOI] [PubMed] [Google Scholar]
- 20.Choi BH, Ha Y, Ahn CH, Huang X, Kim JM, Park SR, et al. A hypoxia-inducible gene expression system using erythropoietin 3’ untranslated region for the gene therapy of rat spinal cord injury. Neurosci Lett. 2007;412:118–122. doi: 10.1016/j.neulet.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 21.Chong ZZ, Kang JQ, Maiese K. Erythropoietin is a novel vascular protectant through activation of Aktl and mitochondrial modulation of cysteine proteases. Circulation. 2002;106:2973–2979. doi: 10.1161/01.CIR.0000039103.58920.1F. [DOI] [PubMed] [Google Scholar]
- 22.Chong ZZ, Kang JQ, Maiese K. Hematopoietic factor erythropoietin fosters neuroprotection through novel signal transduction cascades. J Cereb Blood Flow Metab. 2002;22:503–514. doi: 10.1097/00004647-200205000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Conrad KP, Benyo DF, Westerhausen-Larsen A, Miles TM. Expression of erythropoietin by the human placenta. FASEB J. 1996;10:760–766. doi: 10.1096/fasebj.10.7.8635693. [DOI] [PubMed] [Google Scholar]
- 24.Copeland NG, Gilbert DJ, Schindler C, Zhong Z, Wen Z, Darnell JE, Jr, et al. Distribution of the mammalian Stat gene family in mouse chromosomes. Genomics. 1995;29:225–228. doi: 10.1006/geno.1995.1235. [DOI] [PubMed] [Google Scholar]
- 25.Dawson TM. Preconditioning-mediated neuroprotection through erythropoietin? Lancet. 2002;359:96–101. doi: 10.1016/S0140-6736(02)07335-X. [DOI] [PubMed] [Google Scholar]
- 26.Digicaylioglu M, Lipton SA. Erythropoietin-mediated neuroprotection involves cross-talk between Jak2 and NF-kappaB signalling cascades. Nature. 2001;412:641–647. doi: 10.1038/35088074. [DOI] [PubMed] [Google Scholar]
- 27.Dong H, Fazzaro A, Xiang C, Korsmeyer SJ, Jacquin MF, McDonald JW. Enhanced oligodendrocyte survival after spinal cord injury in Bax-deficient mice and mice with delayed Wallerian degeneration. J Neurosci. 2003;23:8682–8691. doi: 10.1523/JNEUROSCI.23-25-08682.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ehrenreich H, Hasselblatt M, Dembowski C, Cepek L, Lewzuk P, Stiefel M, et al. Erythropoietin therapy for acute stroke is both safe and beneficial. Mol Med. 2002;8:495–505. [PMC free article] [PubMed] [Google Scholar]
- 29.Erbayraktar S, Grasso G, Sfacteria A, Xie QW, Colerman T, Kreilgaard M, et al. Asialoerythropoietin is a nonerythropoietic cytokine with broad neuroprotective activity in vivo. Proc Natl Acad Sci USA. 2003;100:6741–6746. doi: 10.1073/pnas.1031753100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Erbayraktar S, Yilmaz O, Gokmen N, Brines M. Erythropoietin is a multifunctional tissue-protective cytokine. Curr Hematol Rep. 2003;2:465–470. [PubMed] [Google Scholar]
- 31.Erslev A. Humoral regulation of red cell production. Blood. 1953;8:349–357. [PubMed] [Google Scholar]
- 32.Erslev AJ, Caro J, Kansu E, Silver R. Renal and extrarenal erythropoietin production in anemic rats. Br J Haematol. 1980;45:65–72. doi: 10.1111/j.1365-2141.1980.tb03811.x. [DOI] [PubMed] [Google Scholar]
- 33.Fumagalli F, Madaschi L, Brenna P, Caffino L, Marfia G, Di Giulio AM, et al. Single exposure to erythropoietin modulates Nerve Growth Factor expression in the spinal cord following traumatic injury: comparison with methylprednisolone. Eur J Pharmacol. 2008;578:19–27. doi: 10.1016/j.ejphar.2007.09.021. [DOI] [PubMed] [Google Scholar]
- 34.Genc S, Akhisaroglu M, Kuralay F, Genc K. Erythropoietin restores glutathione peroxidase activity in l-methyl-4-phenyl-l, 2, 5, 6-tetrahydropyridine-induced neurotoxicity in C57BL mice and stimulates murine astroglial glutathione peroxidase production in vitro. Neurosci Lett. 2002;321:73–76. doi: 10.1016/S0304-3940(02)00041-1. [DOI] [PubMed] [Google Scholar]
- 35.Genc S, Koroglu TF, Genc K. Erythropoietin and the nervous system. Brain Res. 2004;1000:19–31. doi: 10.1016/j.brainres.2003.12.037. [DOI] [PubMed] [Google Scholar]
- 36.Gorio A, Gokmen N, Erbayraktar S, Yilmaz O, Madaschi L, Cichetti C, et al. Recombinant human erythropoietin counteracts secondary injury and markedly enhances neurological recovery from experimental spinal cord trauma. Proc Natl Acad Sci USA. 2002;99:9450–9455. doi: 10.1073/pnas.142287899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gorio A, Madaschi L, Stefano Di, Carelli S, Di Giulio AM, Biasi S, Coleman T, Cerami A, Brines M. Methylprednisolone neutralises the beneficial effects of erythropoietin in experimental spinal cord injury. Proc Natl Acad Sci USA. 2005;102:16379–16384. doi: 10.1073/pnas.0508479102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grasso G, Sfacteria A, Passalaqua M, Morabito A, Buemi M, Macri B, et al. Erythropoietin and erythropoietin receptor expression after experimental spinal cord injury encourages therapy by exogenous erythropoietin. Neurosurgery. 2005;56:821–827. doi: 10.1227/01.NEU.0000156493.00904.7E. [DOI] [PubMed] [Google Scholar]
- 39.Grasso G, Sfacteria A, Erbayraktar S, Passalacqua M, Meli F, Gokmen N, et al. Amelioration of spinal cord compressive injury by pharmacological preconditioning with erythropoietin and a nonerythropoietic erythropoietin derivative. J Neurosurg Spine. 2006;4:310–318. doi: 10.3171/spi.2006.4.4.310. [DOI] [PubMed] [Google Scholar]
- 40.Hjort E. Reticulocyte increase after injection of anemic serum. Nor Mag Laegevidensk. 1936;97:270–277. [Google Scholar]
- 41.Jelkmann W. Erythropoietin: structure, control of production, and function. Physiol Rev. 1992;72:449–489. doi: 10.1152/physrev.1992.72.2.449. [DOI] [PubMed] [Google Scholar]
- 42.Juul SE, Yachnis AT, Rojiani AM, Christensen RD. Immunohistochemical localization of erythropoietin and its receptor in the developing human brain. Pediatr Dev Pathol. 1999;2:148–158. doi: 10.1007/s100249900103. [DOI] [PubMed] [Google Scholar]
- 43.Kaptanoglu E, Solaroglu I, Okutan O, Surucu HS, Akbiyik F, Beskonakli E. Erythropoietin exerts neuroprotection after acute spinal cord injury in rats: effect on lipid peroxidation and early ultrastructural findings. Neurosurg Rev. 2004;21:113–120. doi: 10.1007/s10143-003-0300-y. [DOI] [PubMed] [Google Scholar]
- 44.Kashii Y, Uchida M, Kirito K, Tanaka M, Nishijima K, Toshima M, et al. A member of Forkhead family transcription factor, FKHRLl, is one of the downstream molecules of phosphatidylinositol 3-kinase-Akt activation pathway in erythropoietin signal transduction. Blood. 2000;96:941–949. [PubMed] [Google Scholar]
- 45.45. Kasper C (2003) Erythropoietin. In: Thomson AW, Lotze MT (eds) The cytokine handbook. vol I. 4th edn. Elsevier, London, pp 149–166
- 46.Kawakami M, Sekiguchi M, Sato K, Kozaki S, Takahashi M. Erythropoietin receptor-mediated inhibition of exocytotic glutamate release confers neuroprotection during chemical ischemia. J Biol Chem. 2001;276:39469–39475. doi: 10.1074/jbc.M105832200. [DOI] [PubMed] [Google Scholar]
- 47.Kayser K, Gabius HJ. Analysis of expression of erythropoietin-binding sites in human lung carcinoma by the biotinylated ligand. Zentralbl Pathol. 1992;138:266–271. [PubMed] [Google Scholar]
- 48.King VR, Averill SA, Hewazy D, Priestley JV, Torup L, Michael-Titus AT. Erythropoietin and carbamylated erythropoietin are neuroprotective following spinal cord hemisection in the rat. Eur J Neurosci. 2007;26:90–100. doi: 10.1111/j.1460-9568.2007.05635.x. [DOI] [PubMed] [Google Scholar]
- 49.Knabe W, Sirén AL, Ehrenreich H, Kuhn HJ. Expression patterns of erythropoietin and its receptor in the developing spinal cord and dorsal root ganglia. Anat Embryol (Berl) 2005;210:209–219. doi: 10.1007/s00429-005-0019-3. [DOI] [PubMed] [Google Scholar]
- 50.Krumdieck N. Erythropoietic substance in the serum of anemic animals. Proc Soc Exp Biol Med. 1943;54:14–17. [Google Scholar]
- 51.Kwon BK, Borisoff JF, Tetzlaff W. Molecular targets for therapeutic intervention after spinal cord injury. Mol Interv. 2002;2:244–258. doi: 10.1124/mi.2.4.244. [DOI] [PubMed] [Google Scholar]
- 52.Lai PH, Everett R, Wang FF, Arakawa T, Goldwasser E. Structural characterization of human erythropoietin. J Biol Chem. 1986;261:3116–3121. [PubMed] [Google Scholar]
- 53.Leist M, Ghezzi P, Grasso G, Bianchi R, Villa P, Fratelli M, et al. Erythropoietin-derived tissue-protective cytokines that do not bind to the classical erythropoietin receptor. Science. 2004;305:239–242. doi: 10.1126/science.1098313. [DOI] [PubMed] [Google Scholar]
- 54.Leverrier Y, Thomas J, Mathieu AL, Low W, Blanquier B, Marvel J. Role of PI3-kinase in Bcl-X induction and apoptosis inhibition mediated by IL-3 or IGF-1 in Baf-3 cells. Cell Death Differ. 1999;6:290–296. doi: 10.1038/sj.cdd.4400492. [DOI] [PubMed] [Google Scholar]
- 55.Liapis H, Roby J, Birkland TP, Davila RM, Ritter D, Parks WC. In situ hybridization of human erythropoietin in pre- and post-natal kidneys. Pediatr Pathol Lab Med. 1995;15:875–883. doi: 10.3109/15513819509027024. [DOI] [PubMed] [Google Scholar]
- 56.Lin FK, Suggs S, Lin CH, Browne JK, Smalling R, Egrie JC, et al. Cloning and expression of the human erythropoietin gene. Proc Natl Acad Sci USA. 1985;82:7580–7584. doi: 10.1073/pnas.82.22.7580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liu ZY, Chin K, Noguchi CT. Tissue specific expression of human erythropoietin receptor in transgenic mice. Dev Biol. 1994;166:159–169. doi: 10.1006/dbio.1994.1304. [DOI] [PubMed] [Google Scholar]
- 58.Martinez-Estrada OM, Rodriguez-Millan E, Gonzalez-De Vicente E, Reina M, Vilaro S, Fabre M. Erythropoietin protects the in vitro blood-brain barrier against VEGF-induced permeability. Eur J Neurosci. 2003;18:2538–2544. doi: 10.1046/j.1460-9568.2003.02987.x. [DOI] [PubMed] [Google Scholar]
- 59.Masuda S, Nagao M, Takahata K, Konishi Y, Gallyas F, Jr, Tabira T, et al. Functional erythropoietin receptor of the cells with neural characteristic. Comparison with receptor properties of erythroid cells. J Biol Chem. 1993;268:11208–11216. [PubMed] [Google Scholar]
- 60.Nagai A, Nakagawa E, Choi HB, Hatori K, Kobayashi S, Kim SU. Erythropoietin and erythropoietin receptors in human CNS neurons, astrocytes, microglia, and oligodendrocytes grown in culture. J Neuropathol Exp Neurol. 2001;60:386–392. doi: 10.1093/jnen/60.4.386. [DOI] [PubMed] [Google Scholar]
- 61.Norenberg MD, Smith J, Marcillo A. The pathology of human spinal cord injury: defining the problems. J Neurotrauma. 2004;21:429–440. doi: 10.1089/089771504323004575. [DOI] [PubMed] [Google Scholar]
- 62.Okutan O, Solaroglu I, Beskonakli E, Taskin Y. Recombinant human erythropoietin decreases myeloperoxidase and caspase-3 activity and improves early functional results after spinal cord injury in rats. J Clin Neurosci. 2007;14:364–368. doi: 10.1016/j.jocn.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 63.Powell JS, Berkner KL, Lebo RV, Adamson JW. Human erythropoietin gene: high level expression in stably transfected mammalian cells and chromosome localization. Proc Natl Acad Sci USA. 1986;83:6465–6459. doi: 10.1073/pnas.83.17.6465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Reissmann KR. Studies on the mechanism of erythropoietic stimulation in parabiotic rats during hypoxia. Blood. 1950;5:372–380. [PubMed] [Google Scholar]
- 65.Romashkova JA, Makarov SS. NF-kappaB is a target of AKT in anti-apoptotic PDGF signalling. Nature. 1999;401:86–90. doi: 10.1038/43474. [DOI] [PubMed] [Google Scholar]
- 66.Sekiguchi Y, Kikuchi S, Myers RR, Campna WM. ISSLS prize winner: Erythropoietin inhibits spinal neuronal apoptosis and pain following nerve root crush. Spine. 2003;28:2577–2584. doi: 10.1097/01.BRS.0000096674.12519.12. [DOI] [PubMed] [Google Scholar]
- 67.Shingo T, Sorokan ST, Shimazaki T, Weiss S. Erythropoietin regulates the in vitro and in vivo production of neuronal progenitors by mammalian forebrain neural stem cells. J Neurosci. 2001;21:9733–9743. doi: 10.1523/JNEUROSCI.21-24-09733.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sönmez A, Kabakçi B, Vardar E, Gürel D, Sönmez U, Orhan YT, et al. Erythropoietin attenuates neuronal injury and potentiates the expression of pCREB in anterior horn after transient spinal cord ischemia in rats. Surg Neurol. 2007;68:297–303. doi: 10.1016/j.surneu.2006.11.045. [DOI] [PubMed] [Google Scholar]
- 69.Swain A, Grundy D. At the accident. In: Grundy D, Swain A, editors. ABC of spinal cord injury. 4. London: BMJ Books; 2002. p. 1. [Google Scholar]
- 70.Tan CC, Eckard KU, Ratcliffe PJ. Organ distribution of erythropoietin messenger RNA in normal and uremic rats. Kidney Int. 1991;40:69–76. doi: 10.1038/ki.1991.181. [DOI] [PubMed] [Google Scholar]
- 71.Taoka Y, Okajima K. Role of leukocytes in spinal cord injury in rats. J Neurotrauma. 2000;17:219–229. doi: 10.1089/neu.2000.17.219. [DOI] [PubMed] [Google Scholar]
- 72.Tator CH. Update on the pathophysiology and pathology of acute spinal cord injury. Brain Pathol. 1995;5:407–413. doi: 10.1111/j.1750-3639.1995.tb00619.x. [DOI] [PubMed] [Google Scholar]
- 73.Villa P, Bigini P, Mennini T, Agnello D, Laragione T, Cagnotto A, et al. Erythropoietin selectively attenuates cytokine production and inflammation in cerebral ischemia by targeting neuronal apoptosis. J Exp Med. 2003;198:971–975. doi: 10.1084/jem.20021067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vitellaro-Zuccarello L, Mazzetti S, Madaschi L, Bosisio P, Gorio A, Biasi S. Erythropoietin-mediated preservation of the white matter in rat spinal cord injury. Neuroscience. 2007;144:865–877. doi: 10.1016/j.neuroscience.2006.10.023. [DOI] [PubMed] [Google Scholar]
- 75.75. Vitellaro-Zuccarello L, Mazzetti S, Madaschi L, Bosisio P, Fontana E, Gorio A et al (2008) Chronic erythropoietin-mediated effects on the expression of astrocyte markers in a rat model of contusive spinal cord injury. Neuroscience. doi:10.1016/j.neuroscience.2007.11.004 [DOI] [PubMed]
- 76.Watkins PC, Eddy R, Hoffman N, Stanislovitis P, Beck AK, Galli J, et al. Regional assignment of the erythropoietin gene to human chromosome region 7pter-q22. Cytogenet Cell Genet. 1986;42:214–218. doi: 10.1159/000132281. [DOI] [PubMed] [Google Scholar]
- 77.Winkelmann JC, Penny LA, Deaven LL, Forget BG, Jenkins RB. The gene for the human erythropoietin receptor: analysis of the coding sequence and assignment to chromosome 19p. Blood. 1990;76:24–30. [PubMed] [Google Scholar]
- 78.Yamaji R, Okada T, Moriya M, Naito M, Tsuruo T, Miyatake K, et al. Brain capillary endothelial cells express two forms of erythropoietin receptor mRNA. Eur J Biochem. 1996;239:495–500. doi: 10.1111/j.1432-1033.1996.0494u.x. [DOI] [PubMed] [Google Scholar]
- 79.Yoshida T, Ishida Y, Sasaki H, Inoue T, Kaku K, Kaneko T. Expression of high affinity binding sites for erythropoietin on L8057 cells, a mouse megakaryoblastic cell line, associated with cell differentiation. Am J Hematol. 1992;39:32–38. doi: 10.1002/ajh.2830390108. [DOI] [PubMed] [Google Scholar]