Abstract
Lumbar spinal fusion is advancing with minimally invasive techniques, bone graft alternatives, and new implants. This has resulted in significant reductions of operative time, duration of hospitalization, and higher success in fusion rates. However, costs have increased as many new technologies are expensive. This study was carried out to investigate the clinical outcomes and fusion rates of a low implant load construct of unilateral pedicle screws and a translaminar screw in transforaminal lumbar interbody fusion (TLIF) which reduced the cost of the posterior implants by almost 50%. Nineteen consecutive patients who underwent single level TLIF with this construct were included in the study. Sixteen patients had a TLIF allograft interbody spacer placed, while in three a polyetheretherketone (PEEK) cage was used. Follow-up ranged from 15 to 54 months with a mean of 32 months. A clinical and radiographic evaluation was carried out preoperatively and at multiple time points following surgery. An overall improvement in Oswestry scores and visual analogue scales for leg and back pain (VAS) was observed. Three patients underwent revision surgery due to recurrence of back pain. All patients showed radiographic evidence of fusion from 9 to 26 months (mean 19) following surgery. This study suggests that unilateral pedicle screws and a contralateral translaminar screw are a cheaper and viable option for single level lumbar fusion.
Keywords: Translaminar screw, Transforaminal interbody fusion, Allograft, Polyetheretherketone cage
Introduction
Lumbar spinal fusion is a commonly performed surgical procedure. It is used in a variety of spinal pathologies including degenerative disease, trauma, spondylolisthesis and deformities. A mechanically stable spine provides an ideal environment for the formation of a fusion mass. The stiffness of the spine increases 2.4 times following use of instrumentation [9, 10]. Though the degree of stability required for spinal fusion is unknown, increased stiffness of the spine improves fusion rates, and lowers the chances of nonunion at the graft site. Instrumented spinal fusion also allows early ambulation with minimal requirement of a post operative external immobilizer.
The first attempt at spinal fusion with internal fixation was reported in 1891 [9] with the use of a wiring technique. Currently, pedicle screws are frequently used to provide spinal stability till the formation of a fusion mass. Their use for the last two decades points towards their efficacy and consistency in outcomes. Concerns have been raised regarding the extensive paraspinal muscle retraction required for their insertion, and the consequent increased infection rates and muscle injury [13]. Also improperly placed screws may cause neural and vascular damage.
Researchers have been attempting to fuse the spine with minimally invasive techniques and reduced implant load. Significant reductions of operative time, duration of hospitalization and costs have been cited as benefits of these techniques [19]. Studies of comparison of unilateral versus bilateral posterior constructs using pedicle screws have shown equal fusion rates; however, unilateral instrumentation has not been recommended for long fusions [12, 18]. Many authors have reported decreased spine stiffness following unilateral instrumentation [8, 18]. As a means of providing suitable spine stiffness with minimal implant load, the combination of unilateral pedicle screw instrumentation with a contralateral translaminar screw is under increased investigation.
Translaminar screws as a means of spinal fixation were first described in 1948 [14].Over the years they were modified by other researchers [5]. The present day screw is a long screw that enters the spinous process on one side and fixes the contralateral facet joint after traversing the lamina [15].
Results in several biomechanical studies have shown that the strength of bilateral pedicle screws and unilateral pedicle screws with a translaminar screw construct are similar [6, 18]. However, reports on the clinical outcomes with the translaminar screw are few in literature [11, 20]. Hence, a study was undertaken to investigate the clinical outcomes and fusion rates of a unilateral pedicle screw construct supplemented with a translaminar screw in transforaminal lumbar interbody fusion (TLIF). We also evaluated the cost differential of a bilateral pedicle screw system and unilateral pedicle screws with a translaminar screw.
Materials and methods
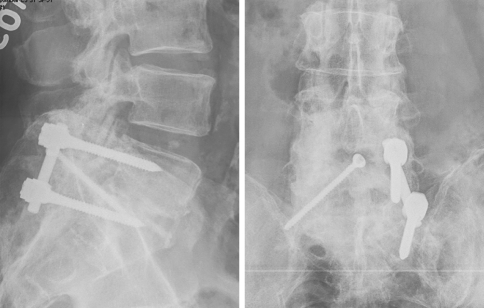
From March 2003 to February 2006 19 patients underwent transforaminal lumbar interbody fusion using a unilateral pedicle screw construct, and contra lateral translaminar screw fixation (Fig. 1). For 14 patients this was their first surgery at that level and the indication for surgery was chronic low back pain, with degenerative disc disease and unilateral radicular complaints. The remaining five patients had previous discectomy with ongoing leg and back pain, and had signs and symptoms consistent with instability at that segment. There were 12 males and 7 females in the study. The age ranged from 28 to 66 years with an average age of 45 years. The translaminar screw was used at the L4–L5 level in ten patients. In seven patients the L5–S1 level and in two the L3–L4 level were fixed with this device. TLIF allograft interbody spacer (MTF, Edison, NJ) was placed in 16 patients while in 3 patients a polyetheretherketone (PEEK) cage (Medtronic Sofamor Danek, Memphis, TN) was used. All cages were filled with autograft. A supplementary posterior fusion was also carried out on the side of the translaminar screw in all patients. Eleven patients had the translaminar fixation on the left side, and in eight patients it was on the right.
Fig. 1.
a, b Radiograph of anteroposterior and lateral views of unilateral pedicle screws and a translaminar screw
Twelve patients of the 14 previously unoperated patients were single level disc disease. Of the remaining two patients, one patient had a non-contiguous two level disc herniation at L3–4 and T11–12. Both sites were decompressed and fused and the translaminar screw was used only at the lumbar fusion site. In the other patient a hybrid construct was used in two level disc disease. Pedicle screws were used at L4, L5 and S1 on the right and at L5–S1 on the left side. The L4–L5 level on the left was fixed with a translaminar screw.
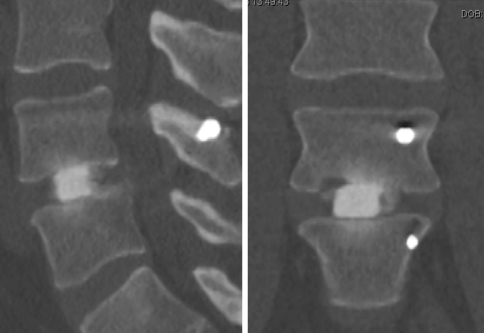
Follow-up ranged from 15 to 54 months with a mean of 32 months. Patients were evaluated using the Oswestry disability index (ODI), Visual analogue scale (VAS) for leg and back pain, and a pain diagram. Postoperative visits were scheduled at 2, 6, 12 and 24 weeks and at 1 and 2 years after the surgery. A record of their most recent follow-up was also included in the study. A clinical and radiological examination (Fig. 2) was conducted at every follow-up visit. CT scan was done for evaluation of fusion when a clinical or radiographic exam aroused a suspicion of nonunion (Fig. 3).
Fig. 2.
Radiographic progress of L5–S1 fusion at 18 months
Fig. 3.
CT-scan evaluation of fusion at 12 months
Technique
The patient is placed prone on a Kambin frame. Access to the spinal segment undergoing fusion is achieved using a standard midline approach. A Synframe (Synthes Spine, Paoli, PA, USA) is used for a stable operative field. It is a ring shaped retractor system [1] fixed to the operating table with arms. One side of the spine is exposed, and the locations for pedicle screw entry are prepared. This is the side of radicular complaints or the side which is preferred by the surgeon when there is only back pain. Pedicle screws are placed first followed by decompression of the facet complex and neural structures and placement of a TLIF graft. We observed that compressing the unilateral pedicle screw construct often leads to scoliosis on that side. Further, posterior compression is required to restore lordosis prior to placement of the translaminar screw as no further lordosis is possible once the screw has been placed in the facet. For this purpose, we used an 18-gauge stainless steel wire which is passed around the two spinous processes at the level of the fusion to maintain the coronal and saggital alignment of the spine. The contralateral or translaminar screw side is then exposed. This includes exposure of the lamina of the superior vertebra, inferior vertebra and facet. The area is then decorticated and the facet capsule removed. The 18-gauge wire is then tightened until adequate compression is achieved on both sides of the midline. The wire also helps to restore the segmental lordosis. The pedicle screws are then locked using a rod and caps followed by placement of the translaminar screw.
The translaminar screw is inserted using a stab incision approximately 8 cm lateral to the midline on the side of the pedicle screw construct. This facilitates the entry of a long 3.2-mm drill to the base of the superior spinous process. The drill is centered and placed in line with the contra lateral lamina, and advanced to the opposite facet joint. During passage of the drill, care is taken to remain within the cortical confines of the lamina. A suitable length (usually 46–60 mm) 4.5-mm cortical screw is then passed for fixation, traversing through the lamina and facet joints and terminating at the base of the transverse process (Fig. 1). Accurate placement of the screw is confirmed using the C arm. The stainless steel wire is then removed prior to closure of the wound.
Results
Clinical
Oswestry scores
Preoperative Oswestry scores ranged from 40 to 86 with a mean of 57. At the latest follow-up the range was 2–40 with a mean of 20.
Back pain
The preoperative back pain score ranged from 3.6 to 10 with a mean of 6.6. It ranged from 1 to 6 with a mean of 3.6 at the latest follow-up.
Leg pain
Leg pain scores of 9.7–1.0 were recorded preoperatively with a mean of 5.4. The scores improved to a range of 4–1 with a mean of 2 at latest follow-up.
Radiographic
Radiographic measurements were made by two independent observers on the electronic public access computer system (EPACS, Stentor, USA). All patients showed radiographic evidence of fusion from 9 to 26 months (mean 19) following surgery. There was no case of nonunion in our study. The criteria we used for fusion included radiographic loss of allograft endplates, end of progression of subsidence and stabilization of symptoms clinically on the Oswestry index and VAS pain scales.
Revision surgery
Three patients reported recurrence of radicular pain in the lower extremity after decompression and fusion using a unilateral pedicle screw with contra lateral translaminar screw. They were re-operated and the fusion site was explored. In all three patients solid fusion was observed with scar tissue formation in the area of the exiting nerve root. Following implant removal, decompression of the nerve roots was performed along with extensive scar excision leading to resolution of symptoms.
Cost
An evaluation of the cost of implants showed that the use of unilateral pedicle screws with a translaminar screw for single level fusion cut the cost by nearly half. This construct cost $1340 as against the bilateral pedicle screw system which is priced at $2600.
Discussion
A variety of techniques have been developed for lumbar spinal fusion. Interbody fusion has become widely popular since it provides a large surface area for fusion with the graft under compression. Anterior column load sharing, restoration of sagittal contour and decompression of neural foramen are some of its other advantages. This technique has also proven to be effective in discogenic back pain. Interbody fusion can be carried out through the anterior or posterior approach. Though high fusion rates have been reported with the anterior approach, the possibility of iliac vessel injury and retrograde ejaculation cannot be overlooked [3, 16, 17]. Further, studies have recommended that anterior lumbar interbody fusion (ALIF) be supplemented with posterior instrumentation for higher fusion rates [21].
The TLIF procedure allows a single point access for interbody fusion and posterior instrumentation. It preserves the anterior longitudinal ligament and a major portion of the posterior ligament complex with minimal compromise of spinal stability. However, following TLIF the spine needs to be instrumented, since studies have shown that mechanically stable spines have a greater chance of fusion [2, 7]. In an attempt to increase the stability of the spine, the volume of instrumentation has often been disproportionately increased. This may lead to injury to muscles, ligaments, and adjacent facet joints causing impaired fusion. [11]
With the advent of minimally invasive techniques to achieve spinal fusion, it has become essential to use minimal instrumentation without compromising on the final stiffness of the spine. Lesser soft tissue dissection allows for early recovery and rehabilitation of the patient. It leads to less postoperative pain, reduced surgical time and less blood loss [4, 5]. These advantages can be obtained with the use of a unilateral pedicle screw, and contralateral translaminar screw construct. The rate of neurological deficit and cerebrospinal fluid leakage during translaminar screw insertion is reported to be one half to one quarter that associated with pedicle screws [20]. Wound infection rates, among cases of translaminar screws are also described as being one tenth that of pedicle screws [20]
The use of unilateral pedicle screws and a translaminar screw allows fusion to be done with little muscle stripping often associated with posterolateral fusion. Yet it accomplishes a 270° fusion with interbody and posterior fusion of the contralateral posterior spinal elements. However, the procedure has limited application due to the requirement of at least one viable lamina, and we found it to be indicated in only 19 patients in a several year period. The ideal indication would be a patient with unilateral radicular complaints requiring a single level spinal fusion. We excluded any patients with bilateral symptoms in this study, as it was our premise that bilateral decompression may make it difficult to pass the translaminar screw. It would also change the way we performed the posterior fusion between the facets, laminae and spinous processes only on the side stabilized with the translaminar screw. This limited the number of patients who qualified for the procedure. Expansion of the indications to include multiple level fusions and partially decompressed laminas will entail further studies.
Unilateral compression using the pedicle screws causes undesirable scoliosis. In an attempt to avoid scoliosis and restore lordosis intraoperatively, we developed an interspinous wiring technique for compression at the site of fusion so as to evenly distribute the compressive forces on the vertebral column. Prior to settling for the cerclage interspinous wire, we had used an AO large fragment reduction forceps and other compression devices which did not work as well.
It has been established that unilateral constructs may also lead to increased rates of hardware failure. Presence of coupled motions due to asymmetry and inability to provide enough rigidity are drawbacks of unilateral internal fixation. Further, considerable off-axis motion was detected in the unilateral pedicle screw construct causing significant reduction of stiffness [5]. Seven fresh frozen human cadaveric specimens were tested in random construct order in flexion/extension, lateral bending, and axial rotation using ±5.0 Nm torques and 50 N axial compressive loads. The authors concluded that in flexion/extension, lateral bending, and axial rotation, there were no measurable differences in either stiffness or range of motion between the standard bilateral pedicle screw, and the construct of unilateral pedicle screw and translaminar screw after TLIF. The unilateral pedicle screw construct provided only half of the improvement in stiffness compared with bilateral or translaminar screw constructs and allowed for significant off-axis rotational motions, which could be detrimental to stability and the promotion for fusion [16].
Conclusion
The purpose of instrumentation is to provide stability to the spine till fusion occurs. It is clear from this study that the construct of unilateral pedicle screw with a contralateral translaminar screw achieved this goal successfully in single level fusion with a reduced implant cost. There was no case of implant failure in our study, and patients improved clinically as evidenced by superior Oswestry and pain scores. This study suggests that unilateral pedicle screws and a contra lateral translaminar screw are a stable construct and a less expensive option for single level lumbar fusion.
References
- 1.Aebi M, Steffen T (2000) Synframe: a preliminary report. Eur spine J 9(suppl 1): S44–S50 1 [DOI] [PMC free article] [PubMed]
- 2.Ames CP, Acosta FL, Jr, Chi J, Iyengar J, Muiru W, Acaroglu E, Puttlitz CM. Biomechanical comparison of posterior lumbar interbody fusion and transforaminal lumbar interbody fusion performed at 1 and 2 levels. Spine. 2005;30(19):E562–E566. doi: 10.1097/01.brs.0000180505.80347.b1. [DOI] [PubMed] [Google Scholar]
- 3.Beaubien BP, Derincek A, Lew WD, Wood KB. In vitro, biomechanical comparison of an anterior lumbar interbody fusion with an anteriorly placed, low-profile lumbar plate and posteriorly placed pedicle screws or translaminar screws. Spine. 2005;30(16):1846–1851. doi: 10.1097/01.brs.0000174275.95104.12. [DOI] [PubMed] [Google Scholar]
- 4.Beringer WF, Mobasser JP. Unilateral pedicle screw instrumentation for minimally invasive transforaminal lumbar interbody fusion. Neurosurg Focus. 2006;20(3):E4. [PubMed] [Google Scholar]
- 5.Best NM, Sasso RC. Efficacy of translaminar facet screw fixation in circumferential interbody fusions as compared to pedicle screw fixation. J Spinal Disord Tech. 2006;19(2):98–103. doi: 10.1097/01.bsd.0000179244.76244.5e. [DOI] [PubMed] [Google Scholar]
- 6.Deguchi M, Cheng BC, Sato K, Matsuyama Y, Zdeblick TA. Biomechanical evaluation of translaminar facet joint fixation. A comparative study of poly-l-lactide pins, screws, and pedicle fixation. Spine. 1998;23(12):1307–1312. doi: 10.1097/00007632-199806150-00003. [DOI] [PubMed] [Google Scholar]
- 7.Fischgrund JS, Mackay M, Herkowitz HN, Brower R, Montgomery DM, Kurz LT. 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine. 1997;22(24):2807–2812. doi: 10.1097/00007632-199712150-00003. [DOI] [PubMed] [Google Scholar]
- 8.Goel VK, Lim TH, Gwon J, Chen JY, Winterbottom JM, Park JB, Weinstein JN, Ahn JY. Effects of rigidity of an internal fixation device. A comprehensive biomechanical investigation. Spine. 1991;16(3 Suppl):S155–S156. doi: 10.1097/00007632-199103001-00023. [DOI] [PubMed] [Google Scholar]
- 9.Grob D, Humke T. Translaminar screw fixation in the lumbar spine: technique, indications, results. Eur Spine J. 1998;7(3):178. doi: 10.1007/s005860050053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heggeness MH, Esssess SI. Translaminar facet joint screw fixation for lumbar and lumbosacral fusion. A clinical and biomechanical study. Spine. 1991;16(Suppl 6):S266–S269. doi: 10.1097/00007632-199106001-00018. [DOI] [PubMed] [Google Scholar]
- 11.Jang JS, Lee SH. Minimally invasive transforaminal lumbar interbody fusion with ipsilateral pedicle screw and contralateral facet screw fixation. J Neurosurg Spine. 2005;3(3):218–223. doi: 10.3171/spi.2005.3.3.0218. [DOI] [PubMed] [Google Scholar]
- 12.Kabins MB, Weinstein JN, Spratt KF, Found EM, Goel VK, Woody J, Sayre HA. Isolated L4–L5 fusions using the variable screw placement system: unilateral versus bilateral. J Spinal Disord. 1992;5(1):39–49. doi: 10.1097/00002517-199203000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery: (1996) A histologic and enzymatic analysis. Spine 21(8):941–944. doi:10.1097/00007632-199604150-00007 [DOI] [PubMed]
- 14.King D. Internal fixation of lumbosacral fusion. J Bone Joint Surg Am. 1948;30:560–565. [PubMed] [Google Scholar]
- 15.Magerl FP. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop Relat Res. 1984;189:125–41. [PubMed] [Google Scholar]
- 16.Sasso RC, Best NM, Mummaneni PV, Reilly TM, Hussain SM. Analysis of operative complications in a series of 471 anterior lumbar interbody fusion procedures. Spine. 2005;30(6):670–674. doi: 10.1097/01.brs.0000155423.18218.75. [DOI] [PubMed] [Google Scholar]
- 17.Sasso RC, Kenneth Burkus J, LeHuec JC. Retrograde ejaculation after anterior lumbar interbody fusion: transperitoneal versus retroperitoneal exposure. Spine. 2003;28(10):1023–1026. doi: 10.1097/00007632-200305150-00013. [DOI] [PubMed] [Google Scholar]
- 18.Slucky AV, Brodke DS, Bachus KN, Droge JA, Braun JT. Less invasive posterior fixation method following transforaminal lumbar interbody fusion: a biomechanical analysis. Spine J. 2006;6(1):78–85. doi: 10.1016/j.spinee.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 19.Suk KS, Lee HM, Kim NH, Ha JW. Unilateral versus bilateral pedicle screw fixation in lumbar spinal fusion. Spine. 2000;25(14):1843–1847. doi: 10.1097/00007632-200007150-00017. [DOI] [PubMed] [Google Scholar]
- 20.Tuli J, Tuli S, Eichler ME, Woodard EJ. A comparison of long-term outcomes of translaminar facet screw fixation and pedicle screw fixation: a prospective study. J Neurosurg Spine. 2007;7(3):287–292. doi: 10.3171/SPI-07/09/287. [DOI] [PubMed] [Google Scholar]
- 21.Wang JM, Kim DJ, Yun YH. Posterior pedicular screw instrumentation and anterior interbody fusion in adult lumbar spondylolysis or grade I spondylolisthesis with segmental instability. J Spinal Disord. 1996;9(2):83–88. doi: 10.1097/00002517-199604000-00001. [DOI] [PubMed] [Google Scholar]