Abstract
The effectiveness of physiotherapy after first-time lumbar disc surgery is still largely unknown. Studies in this field are heterogeneous and behavioural treatment principles have only been evaluated in one earlier study. The aim of this randomised study was to compare clinic-based physiotherapy with a behavioural approach to a home-based training programme regarding back disability, activity level, behavioural aspects, pain and global health measures. A total of 59 lumbar disc patients without any previous spine surgery or comorbidity participated in the study. Clinic-based physiotherapy with a behavioural approach was compared to home-based training 3 and 12 months after surgery. Additionally, the home training group was followed up 3 months after surgery by a structured telephone interview evaluating adherence to the exercise programme. Outcome measures were: Oswestry Disability Index (ODI), physical activity level, kinesiophobia, coping, pain, quality of life and patient satisfaction. Treatment compliance was high in both groups. There were no differences between the two groups regarding back pain disability measured by ODI 3 and 12 months after surgery. However, back pain reduction and increase in quality of life were significantly higher in the home-based training group. The patients in the clinic-based training group had significantly higher activity levels 12 months after surgery and were significantly more satisfied with physiotherapy care 3 months after surgery compared to the home-based training group. Rehabilitation after first-time lumbar disc surgery can be based on home training as long as the patients receive both careful instructions from a physiotherapist and strategies for active pain coping, and have access to the physiotherapist if questions regarding training arise. This might be a convenient treatment arrangement for most patients.
Keywords: Lumbar disc herniation, Surgery, Physiotherapy, Behavioural, Training
Introduction
Although lumbar disc surgery is the most common surgical treatment for disc herniation in patients with back and leg symptoms, there is still no consensus on rehabilitation guidelines [40].
Postoperative rehabilitation of these patients could be important for minimising complaints after surgery. According to a Cochrane review from 2002 [40], however, available studies in this field are very heterogeneous with regard to the type of exercise programmes as well as to the timing and duration of the intervention. Early [26] and intensive [4, 5, 10, 33] training has been shown to have positive effects on pain, functional status and return to work in the short term. Studies on the long-term effects of different exercise programmes are sparse. Ostelo et al. [40] suggested that there is strong evidence that there is no difference between intensive and mild exercise programmes on long-term follow-up. Since that review, several randomised controlled studies have been published on this topic [4, 11, 12, 15, 19, 24, 25, 52]. All add further support to early and active programmes, but the effect of different training programmes still tends to level out on long-term follow-up. Recently, however, Millisdotter and Stromqvist [37] have shown in a prospective controlled study that a specific stabilising programme might have benefits regarding disability 12 months after surgery when compared to routine care.
Manniche [33] and Kjellby-Wendt [25] emphasised that intensive training programmes confront patients with their fears and insecurities, thus implying a behavioural effect.
Behavioural treatment principles are successfully applied in the treatment of non-specific low back pain [42]. Even though the outcome of lumbar disc surgery seems to be influenced by behavioural and cognitive factors, such as passive pain coping and fear of movement [8, 9], behavioural treatment principles have only been evaluated in one study [41]. In this study, it was concluded that the behaviour-oriented principles did not offer any additional advantages to this patient group. Nevertheless, the authors of this study recommended that caregivers should convey a message of active pain coping and encourage patients to gradually resume normal daily activities, including returning to work.
According to earlier studies on patients with acute orthopaedic injuries [2], after arthroscopic orthopaedic surgery [7, 44], with non-specific low back pain [38] and after spinal surgery [34], home-based training is a feasible treatment. Regarding patients who had undergone lumbar disc surgery, home exercises have been compared to supervised exercise programmes in four studies [4, 15, 22, 52], the results of which are contradictory. Johannsen et al. [22] found these two treatment approaches almost equally effective regarding global health aspects, disability, pain and mobility. Yilmaz et al. [52], however, found supervised dynamic lumbar stabilisation training to be more beneficial than home-based training, which in turn was more effective than no training. This is a pattern that has also been reported in other studies [4, 15].
In summary, early and active training is beneficial for this patient group, as well as training programmes including exercises which aim to regain back muscle activity and trunk stability. A passive attitude towards pain seems to be an obstacle for recovery, however, behaviourally oriented programmes have only been evaluated in one previous study. In clinical practice it remains unclear whether minimal instructions regarding training and activity are sufficient, or if a further comprehensive programme led by a physiotherapist is more appropriate in rehabilitation after lumbar disc surgery.
The aim of the present study was to compare the effects of a regular, clinic-based, behaviour-oriented physiotherapy programme with a home-based exercise programme on disability, activity level, behavioural aspects such as kinesiophobia and coping, pain, global health measures and patient satisfaction.
Methods
Study design
This study was a randomised controlled prospective clinical trial with assessments before randomisation and 3 and 12 months after surgical treatment.
Participants
Patients were recruited from two neighbouring orthopaedic clinics in Sweden, one university hospital and one community hospital, between March 2003 and March 2005. Both clinics have catchment areas of about 250,000 inhabitants.
Patients were eligible for inclusion if they were scheduled for planned (not acute) first-time lumbar disc surgery, were between 18 and 60 years old, and had a lumbar disc herniation confirmed by MRI. All had incapacitating pain and physical signs of nerve root compression corresponding to the level of disc herniation. Criteria for exclusion were comorbidity influencing daily activities and not being fluent in the Swedish language.
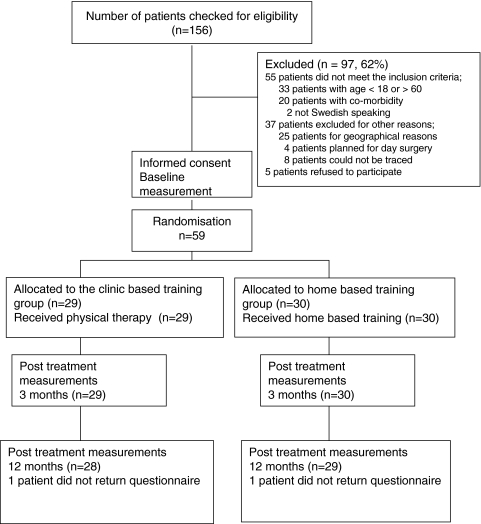
The operation lists of the two departments were searched for eligible patients. Out of 253 patients who were scheduled for lumbar disc surgery, 83 had an acute operation and 14 a reoperation, leaving 156 who were checked for eligibility. A total of 59 patients finally met all inclusion criteria and gave their informed consent to participate (Fig. 1). A total of 41 patients (69%) were recruited from the community hospital and 18 patients (31%) from the university hospital. Twenty patients from the community hospital were randomised to the clinic-based group and 21 patients to the home-based group. Corresponding numbers for the university hospital were nine (clinic based) and nine (home based). The most common reasons for exclusion were age over 60 years (n = 33), comorbidity (n = 20) and geographic (n = 25).
Fig. 1.
Patient flow through the study
The patients were consecutively randomised to clinic-based training or home-based training during their postoperative stay in hospital. Randomisation was done from a computer-generated random list in blocks of four, stratified by hospital, and distributed in numbered, concealed envelopes by the physiotherapists at the respective orthopaedic departments. These physiotherapists neither took part in the later follow-up (3 weeks after surgery) nor the later treatment of the patients.
A total of 29 patients were randomised to the clinic-based training group and 30 to the home-based training group (Fig. 1).
Demographic data of the study group are presented in Table 1.
Table 1.
Characteristics of the two study groups at baseline and P values for comparisons between groups
| Clinic-based training group n = 29 |
Home-based training group n = 30 |
||||
|---|---|---|---|---|---|
| Interquartile range | Interquartile range | P value | |||
| Age in years (median) | 43 | 35–47 | 38 | 31–43 | 0.016 |
| Gender: women/men (number) | 12/17 | 12/18 | 0.914 | ||
| Duration of symptoms before surgery, months (median) | 10 | 6–24 | 6 | 4–17 | 0.150 |
| Patients on sick leave (number) | 15 | 20 | 0.243 | ||
| Length of sick leave, months (median) | 6 | 4–14 | 4 | 2–7 | 0.132 |
| Smokers (number) | 7 | 6 | 0.701 | ||
| Work load (number) | |||||
| Heavy | 9 | 7 | |||
| Moderate | 10 | 11 | |||
| Light | 7 | 11 | |||
| Unemployed | 3 | 1 | 0.354 | ||
Values are medians and interquartile range
The study was approved by the Regional Ethics Committee in Uppsala.
All patients were surgically treated with a standard lumbar discectomy using microsurgical technique with magnifying glasses but without microscope.
The levels of disc herniation were similarly distributed in the two groups: 15 patients in each group at the level of L5–S1, 14 patients in the clinic-based training group and 12 in the home training group at L4–L5. In the home training group, one patient had a disc herniation located at L3–L4, and two patients at L2–L3.
Initial physiotherapy 0–3 weeks after surgery for both treatment groups
All patients in both groups received oral and written information about postoperative training by a physiotherapist in the ward. Exercise started the first day after surgery and comprised stabilisation of the trunk by activation of the deep abdominal muscles [39], back and hip mobility, and activation of the back, abdominal and buttock muscles, as well as instructions about how to get out of bed. Additionally, the patients received a written exercise programme which they were instructed to follow at least once a day. The patients were given no sitting restrictions and were encouraged to increase their daily activities gradually and to take daily walks.
Patients in both groups were followed up by the same physiotherapist 3 weeks after surgery. For the home-based training group this was the only physiotherapy visit. At this follow-up visit all patients were clinically examined and given a new training programme which they were recommended to do daily. The importance of physical activity for the healing process was emphasised. The programme comprised back and hip mobility, trunk stability, strengthening of back, abdominal and leg muscles, and stretching of back, hamstring, quadriceps femoris and calf muscles. The patients were recommended to continue, and gradually extend, their daily walks and return to their normal daily routines and work as soon as possible. They were given no restrictions apart from heavy lifting during the first 3 months after surgery.
After this visit, the patients followed one of the two treatment groups, the clinic-based or the home-based training group.
The clinic-based training group
Patients who were randomised to the clinic-based training group visited the physiotherapy department once a week for 8 weeks, starting at the first follow-up visit 3 weeks after surgery and continuing until 11 weeks after surgery. They worked on their exercises under supervision by the physiotherapist alongside their daily home programme and were recommended to gradually resume normal daily activities. The physiotherapy was influenced by a behavioural operant approach including graded activity with positive reinforcement of healthy behaviour, aiming to reduce fear and avoidant behaviour [16, 17, 29, 30, 41, 50]. The exercise programme comprised back and hip mobility, trunk stability and strengthening of back, abdominal and leg muscles. Exercises with weight resistance were gradually added and increased. The programme also comprised general condition training by treadmill walking, stretching of back, hamstring, quadriceps femoris and calf muscles as well as a short relaxation. The patients also had the opportunity to discuss questions and thoughts about their condition at every visit. Active coping styles were encouraged and patients with residual pain were recommended to continue with their daily walks and home programme regardless. If a patient showed signs of passive pain coping, barriers to activity were identified and discussed and alternatives to painful exercises were given. The importance of future regular physical training was continuously emphasised and the patients were requested to establish goals for future regular weekly physical activity.
The home-based training group
Patients randomised to the home-based training group were informed and instructed at the above described occasion 3 weeks after surgery. They were recommended to gradually increase the number of repetitions of the exercises. No additional instructions were given to this group. Future regular physical activity was encouraged. After this visit, the patients continued to train on their own. They had the possibility of contacting the physiotherapist if they had questions concerning their training programme.
Outcome measures
Before 1–2 weeks of admission to the orthopaedic clinic for surgery, all patients were sent a questionnaire (described below) to be completed and returned on arrival at the hospital.
After 3 and 12 months of surgery, another questionnaire was sent for the evaluation of outcome measures (described below).
The 3-month follow-up took place 1–2 weeks after the clinic-based training group had finished their treatment programme.
In addition, all patients in the home-based training group were contacted by telephone 3 months after surgery by a physiotherapist unknown to the patient, and a structured interview was performed. The interview contained questions about adherence to the exercise programme.
The questionnaires to be answered preoperatively and 3 and 12 months after surgery included questions regarding:
Back pain-related disability, assessed with the Oswestry disability questionnaire [13] which was the primary outcome variable. This scale has been reported to be reliable and have sufficient width to detect improvement or worsening in individuals with low back pain [6]. An advantage of this self-reported questionnaire is that it captures the patient’s own perception of his/her back problem, which might be of greater relevance in assessing outcome after treatment than so-called objective measures of impairment [14]. Previous studies, though, have shown a high correlation between subjective and objective measures of disability [35].
Thelevel of physical training and possible walking distance.
Kinesiophobia, evaluated by a modification of the Tampa Scale of Kinesiophobia (TSK), with a possible score distribution from a low of 12, indicating no kinesiophobia, to a high of 48, indicating maximal kinesiophobia [36, 51]. Five questions from the TSK were omitted since these were considered to be inappropriate for this patient group.
Coping strategies, assessed by the subscales of self-statement and catastrophising from the Coping Strategies Questionnaire (CSQ). The dimensions self-statement and catastrophising each contain six questions, ranging from a possible low score of 0 to a high of 36 on each dimension.
A coping self-statement means telling oneself that one can cope with pain, no matter how bad it gets, e.g. “I tell myself to be brave and carry on despite the pain”.
Catastrophising means negative self-statements and an exaggerated negative orientation towards pain, e.g. “It is terrible and I feel it is never going to get any better”.
Higher scores indicate more self-statement and more pain catastrophising, respectively [28, 45].
The intensity of back and leg pain, using visual analogue scales (VAS).
Generic health-related quality of life, measured by EuroQol [3] and SF-36 [47, 49].
Patient satisfaction regarding physiotherapy care, measured by two separate questions 3 months after surgery. Question one: “In your own view, did you receive enough help from the physiotherapist after your back operation?” Possible answers were “No, I received too little help”, or “Yes, I received enough help.” Question two: “Would you recommend the physiotherapy you received to a friend who is going to be treated by disc surgery?” Possible answers were “Yes” or “No”.
Therapies given by other caregivers, evaluated by separate questions at 3-month follow-up. The first question was “Have you been treated by caregiver/s other than those within the hospital since you had your back operation?” Possible answers were “Yes” or “No”. For patients who answered yes there was an attendant question regarding which caregiver they had visited and how many times.
In addition, the patients reported orally whether their leg pain was better, unchanged/worse (dichotomous data) 3 weeks after surgery compared to before the intervention started.
Statistics
A power analysis, carried out prior to the study, showed that a total of 50 patients, 25 in each group, was needed to detect a clinically significant mean score difference of eight points in the ODI (SD = 10) with 80% power. To allow for possible drop-outs we decided to include 30 patients in each group, making a total of 60 patients.
Since most data were ordinal and not normally distributed, the median was used as measure of location and the interquartile range (q1–q3) as measure of dispersion.
The Mann–Whitney rank sum test was used to compare differences between the two groups regarding changes over time.
Differences of proportions were analysed using chi-square statistics and Fisher’s exact test.
Since the average age of the clinic-based group was 5 years higher than that of the home training group, we ran a linear multiple regression analysis to adjust for age. Group affiliation and age acted as independent variables and pain (leg and back pain), disability (ODI) and quality of life (EuroQol5D, EuroQol VAS) as dependent variables.
According to the intention-to-treat principle, the two patients who underwent repeated surgery (1 from each treatment group) during the first postoperative period were included in the data analysis. We performed a separate analysis without these two patients and found only minor differences concerning group median values. Moreover these differences did not influence any of the outcome variables.
A two-sided P value less than 0.05 was considered to be significant.
Results
Demographic data for the two study groups are presented in Table 1. The median age in the clinic-based training group was 43 years (range 30–59), which was significantly higher than the home-based training group with a median of 38 years (range 25–57). As adjustments for age had little effect on the results for outcome variables, we present only the crude differences between the groups.
Participation
All patients answered the 3-month follow-up questionnaire. One patient in each group did not answer the 12-month questionnaire despite repeated reminders.
One patient in the clinic-based training group had another disc herniation at the same level and was reoperated 9 months after the first operation. One patient in the home-based training group had a postoperative discitis and was treated surgically with lumbar fusion 11 months after the primary operation.
Leg pain before and 3 weeks after surgery
After 3 weeks of surgery, 24/29 patients (83%) in the clinic-based group reported less leg pain in comparison to before surgery and five patients reported unchanged/worse leg pain. The corresponding number of patients in the home-based training group was 27/30 patients (90%) reporting no pain and three patients reporting unchanged or worse leg pain. When these proportions were compared there was no significant difference between the two groups (P = 0.472).
During the first 3 months after surgery, 6/30 patients (20%) in the home-based training group contacted the physiotherapist, a total of 13 telephone calls. They all had questions and concerns about residual leg or back pain and two of them also had queries about the intensity of training. These six patients had slightly but not significantly higher median scores for kinesiophobia (36/32) and catastrophising (17/13) and slightly but not significantly lower median scores for coping self-statement (19/21) compared to the other patients in the home-based training group.
Differences between groups
Comparisons of differences between the two groups at baseline and the different time points are presented in Tables 2 and 3.
Table 2.
Median preoperative values for the two treatment groups
| Preoperative value | After 3 months, postintervention | After 12 months, postintervention | ||||||
|---|---|---|---|---|---|---|---|---|
| Clinic-based training group | Home-based training group | Clinic-based training group | Home-based training group | P value | Clinic-based training group | Home-based training group | P value | |
| ODI (0–100) | ||||||||
| Median | 38 | 39 | 16 | 14 | 0.49 | 15 | 6 | 0.09 |
| Median for difference (interquartile range) | −20 (−5, −36) | −20 (−13, −36) | −23 (−9, −38) | −32 (−17, −42) | ||||
| Back pain VAS (0–100) | ||||||||
| Median | 70 | 70 | 23 | 14 | 0.33 | 34 | 9 | 0.04 |
| Median for difference (interquartile range) | −31 (−11, −69) | −42 (−25, −61) | −19 (−10, −43) | −45 (−13, −73) | ||||
| Leg pain VAS (0–100) | ||||||||
| Median | 75 | 70 | 18 | 7 | 0.34 | 23 | 5 | 0.06 |
| Median for difference (interquartile range) | −32 (−14, −71) | −53 (−23, −77) | −23 (−11, −67) | −58 (−32, −80) | ||||
| TSK (12–48) | ||||||||
| Median | 31 | 33 | 20 | 22 | 0.34 | 20 | 24 | 0.96 |
| Median for difference (interquartile range) | −10 (−5, −16) | −9 (−4, −11) | −7 (−2, −15) | −10 (−3, −14) | ||||
| CSQ Self-statement (0–36) | ||||||||
| Median | 19 | 21 | 21 | 24 | 0.29 | 19 | 19 | 0.34 |
| Median for difference (interquartile range) | 2 (−4, 6) | 4 (−2, 8) | 1 (−3, 5) | 1 (−4, 3) | ||||
| CSQ Catastrophising (0–36) | ||||||||
| Median | 15 | 13 | 7 | 3 | 0.37 | 8 | 10 | 0.39 |
| Median for difference (interquartile range) | −6 (−1, −12) | −9 (−2, −14) | −7 (0, −10) | −5 (5, −15) | ||||
| EuroQol 5D (−0.594−1) | ||||||||
| Median | 0.19 | 0.33 | 0.76 | 0.76 | 0.91 | 0.70 | 0.80 | 0.35 |
| Median for difference (interquartile range) | 0.24 (0.06, 0.76) | 0.27 (0.11, 0.64) | 0.36 (0.04, 0.63) | 0.48 (0.11, 0.74) | ||||
| EuroQol VAS (0–100) | ||||||||
| Median | 50 | 49 | 80 | 80 | 0.580 | 70 | 70 | 0.03 |
| Median for difference (interquartile range) | 23 (10, 43) | 32 (12, 49) | 13 (0.8, 33) | 30 (15, 55) | ||||
Medians of outcome scores, and medians for differences and interquartile range for differences, for the two treatment groups at the different time points. P values for comparisons of differences between the two treatment groups, 3 and 12 months after disc surgery
Table 3.
Maximum walking distance for each treatment group at the different time points and P values for comparisons of differences between the groups
| Walking distance | Before surgery | 3 months after surgery | 12 months after surgery | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Clinic-based training group | Home-based training group | P value | Clinic-based training group | Home-based training group | P value | Clinic-based training group | Home-based training group | P value | |
| <100 m | 7 | 6 | 1 | – | – | – | |||
| 100–500 m | 5 | 9 | 3 | 1 | 2 | 1 | |||
| 0.5–1 km | 6 | 4 | 1 | 2 | 3 | 2 | |||
| >1 km | 11 | 11 | 0.874 | 24 | 27 | 0.365 | 23 | 26 | 0.412 |
| No data | 1 | 1 | |||||||
Postintervention follow-up, 0–3 months after surgery
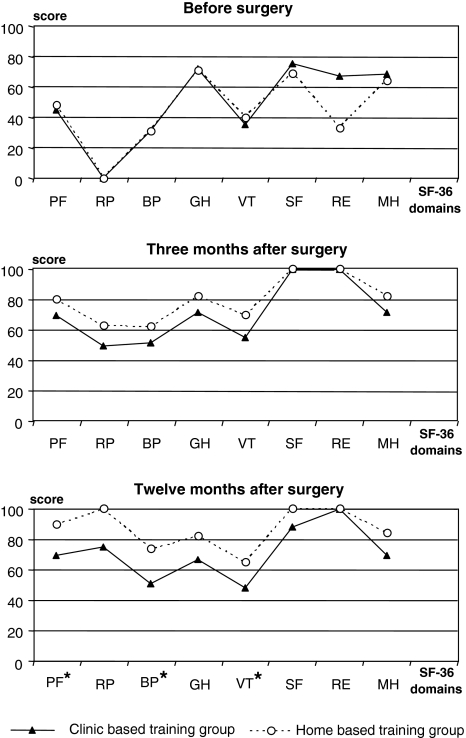
The first follow-up was scheduled 1–2 weeks after the clinic-based training was finished, 3 months after surgery (Tables 2, 3; Fig. 2).
Fig. 2.
SF-36 scores before and 3 and 12 months after surgery for the clinic-based training group and the home-based training group. Asterisks indicate a significant difference between the two groups. PF Physical function, RP role physical, BP bodily pain, GH general health, VT vitality, SF social functioning, RE role emotional, MH mental health
No significant differences between the two groups were found regarding ODI, level of physical training, maximum walking distance, kinesiophobia, coping, pain or quality of life.
Compliance and patient satisfaction
All but 4/29 patients (14%) adhered to the eight planned visits in the clinic-based training group. These four patients had seven, four, four and two visits, respectively.
The patients in the home-based training group were contacted by telephone 3 months after surgery and all reported they had understood the exercises well and knew how to accomplish the home programme. Most patients, 25/30 (86%), thought they had got on well with their exercises at home, while 4/30 (14%) were dissatisfied with their home training.
Most patients, 24/30 (83%), had trained 3–7 times per week, 2/30 (7%) once a week or occasionally and 3/30 (10%) had not undertaken the home programme at all. These three patients’ median values for back and leg pain were higher than those of the other patients in the home-based training group (back pain 68, leg pain 38, compared to back pain 18, leg pain 10). All three patients reported, however, that they had less pain 3 weeks after surgery compared with preoperative pain levels.
Three months after surgery 28/29 patients (97%) in the clinic-based training group and 20/30 patients (67%) in the home-based training group reported that they had received sufficient help from the physiotherapist. This difference between the groups was significant (P = 0.023).
Significantly more patients in the clinic-based training group than in the home-based training group would recommend the treatment they had been provided to other patients 27/29 (93%) versus 21/30 (70%), (P = 0.023).
Treatment by other health care providers
During the first 3 months after surgery, 4/30 patients (13%) in the home-based training group visited another caregiver. Two patients visited a chiropractor, a masseur and another physiotherapist, and two patients visited a masseur only, whereas only one patient (3%) in the physiotherapy group visited another caregiver, a chiropractor.
Long-term comparison (0–12 months)
The second follow-up was carried out 12 months after surgery (Tables 2, 3; Fig. 2).
Disability
There were no significant differences between the two treatment groups regarding ODI at 12-month follow-up (Table 2).
Level of physical training
After 12 months of surgery, all patients in the clinic-based training group, 28/28 (100%), reported that they trained regularly, compared with 23/29 (79%) patients in the home-based training group. This difference was significant (P = 0.019).
Maximum walking distance did not differ significantly between the two groups (Table 3).
Kinesiophobia and coping
There were no significant differences between the two treatment groups regarding kinesiophobia and coping at 12-month follow-up.
Pain
The home-based training group had a reduction of back pain from 70 mm at baseline to 9 mm at 12-month follow-up, whereas the corresponding reduction in the clinic-based training group was from 70 to 34 mm. This difference was statistically significant (P = 0.040).
Moreover, the home-based training group had a reduction of leg pain from median 70 mm at baseline to median 5 mm at 12-month follow-up, while the reduction in the clinic-based training group was from 75 to 23 mm. This difference was not quite statistically significant (P = 0.062) (Table 2).
Quality of life
Quality of life as measured by EuroQol VAS increased significantly more in the home-based training group (from 49 to 85 mm) compared to the clinic-based training group (from 50 to 70 mm) (Table 2). This difference between the groups was also reflected in the dimensions physical function, bodily pain and vitality within the SF-36 questionnaire (Fig. 2).
Discussion
The main finding in this study was that there was no difference between the outcome of clinic-based training with regular scheduled visits to a physiotherapist and home-based training regarding back pain-specific functional status 3 and 12 months after first-time disc surgery. Back pain reduction and quality of life were significantly better in the home-based training group 1 year after surgery. However, those patients who followed the regular, multidimensional physiotherapy programme had a significantly higher compliance rate for future regular physical activity and were significantly more satisfied with the help they had received from the physiotherapist.
Figure 1 shows that 62% (n = 97) of the 156 patients who were initially checked for eligibility were excluded from participation in this study. The main reasons for this were age over 60 years (34%), geographic (26%) or comorbidities (21%). Patients over 60 years were excluded since they are expected to have more pronounced degenerative changes [23]. Comorbidities are also likely to be more common among older patients. This was an exclusion criterion, as it is known to significantly influence most aspects of health [18]. We feared that concurrent diagnoses could constitute an obstacle for recovery and for the ability to fulfil the prescribed training, thereby decreasing compliance.
Both hospitals have geographically extensive catchment areas. Patients who lived far from the hospital, had difficulties to get there, and/or already had an established physiotherapist contact in their home area were not included in the study (26%), as we considered the risk for drop-out and lack of compliance to be too high.
Patients with lumbar disc herniation are often regarded as a homogenous group. For rehabilitation, however, it is important to acknowledge its heterogeneity. It is reasonable to assume that different subgroups would need different kinds of postoperative care.
It should be noted that the results of this study are only valid for a selected subgroup of patients undergoing first-time elective lumbar disc surgery, comprising individuals aged from 18 to 60 years without comorbidities. This subgroup comprised about 38% of the patients who were undergoing first-time lumbar disc surgery in the two Swedish hospitals.
In clinical physiotherapy practice, this is a considerable number of patients, and a large amount of time and costs can be saved if rehabilitation for these patients delivers a message of active coping and instructions about the subsequent home-based training.
Depending on patient selection and definitions, the success rate of surgery ranges from 60 to 90% [1, 20, 27, 31, 32, 43]. In this study, both groups had a pronounced treatment effect 12 months after surgery, with a mean decrease of 24.6 (SD 20.5) in ODI scores for the whole sample: from a mean of 39.6 preoperatively to a mean of 15.1 at 12-month follow-up. The home-based training group had low median ODI values 12 months after surgery (ODI 6) as well as low median levels of leg (VAS 5) and back pain (VAS 9). In a study on a similar group by Häkkinen and co-workers [21], the corresponding mean ODI value was 19. In the Swedish spine register, based on 1,021 disc patients surgically treated during 2003, the corresponding mean levels of leg and back pain at 12-month follow-up were 23 and 26, respectively [46]. The excellent results of the home-based training group were unexpected and contrasting to previous studies, but in those, the control groups had a less active or no exercise programme, and compliance with the prescribed home training was not reported [4, 15, 52].
Finding the appropriate balance in physical exercise is important after lumbar disc surgery. The higher physical activity in the clinic-based training group might have been too intense for some patients and could thereby have contributed to more back pain in this group at 12-month follow-up.
Another explanation for the lower back pain score in the home-based training group could be the home-based training arrangement, which with little postoperative treatment indirectly encourages the patients to return to normal life habits, possibly influencing pain perception positively.
The primary aim after surgery, besides pain reduction, is the return to a normal activity level as soon as possible and the prevention of future recurrent back and/or leg pain. As the physiotherapist in this study had the opportunity to adjust the exercises for patients in the clinic-based training group, these patients were able to accomplish the programme despite residual pain. This may provide an explanation for their significantly higher level of regular physical training at 12-month follow-up despite higher levels of back pain in the clinic-based group. The behavioural support for this group, with the possibility to identify and discuss problems impeding physical activities, may have promoted subsequent physical activity.
The same physiotherapist met all patients, and instructions on physical activity were the same for both groups. Even though behavioural support was minimal in the home-based training group, the similarity of the two treatment approaches probably contributed to the small differences between the two groups.
In the home-based training group, the physiotherapist was contacted by 20% of patients within the first three months after surgery. Almost every patient who called had queries about residual pain, indicating that this is a subject patients need to be informed about. When home-based training is offered, it might be beneficial therefore to include a brief educational intervention as well.
In earlier studies, evaluating treatments aiming at the minimisation of psychosocial barriers to the rehabilitation progress, it was concluded that the behavioural intervention was most effective in patients who had pronounced kinesiophobia and passive pain coping strategies [17, 48]. In accordance with these studies, programmes with behaviour-oriented principles might be of advantage for selected patients who have pronounced kinesiophobia and passive pain coping, but not necessarily for all patients. Identifying patients at risk and developing effective treatment programmes for them are challenging future research tasks.
The study was randomised but the sample was quite small and the significantly higher level of back pain 12 months after surgery in the clinic-based training group might be explained by some confounding factor unevenly and randomly distributed over the groups. This is indicated by the fact that the significant differences between the groups occurred when the physiotherapy intervention was actually over, between 3 and 12 months after surgery. It is, however, unlikely that the intervention itself is responsible for the differences seen after 12 months.
In our power analysis we used an expected SD of 10 points for the ODI, the main outcome variable. However, the standard deviation of the ODI 3 months after surgery was 14 points, which means that we underestimated the ODI variation. Since the differences were far from being significant though we do not think this lack of power of the study sample affects the interpretation of our results.
One shortcoming of the study was the lack of more sensitive pain ratings 3 weeks after surgery, when we only had dichotomous data. The groups were small and the power analysis did not include various potential confounders. We can therefore not rule out the presence of influential factors other than our intervention. However, the absence of any difference in pain ratings 3 weeks after surgery suggests that the operative results did not differ between the two groups.
Clinical implications
Rehabilitation after first-time disc surgery for patients without comorbidities can be based on training instructions and home training. This requires that patients receive careful instructions from a physiotherapist, a message of active pain coping and access to the physiotherapist if questions arise concerning their training. This might be a convenient treatment arrangement for most patients.
Conclusions
The results of behaviour-oriented clinic-based physiotherapy did not differ from home training regarding back pain-specific functional status 3 and 12 months after first-time disc surgery, but back pain reduction and the increase in quality of life were significantly higher in the home-based training group.
The patients who completed the regular, multidimensional clinic-based physiotherapy programme were more motivated to continue regular physical activity and were significantly more satisfied with physiotherapy care despite more persistent back pain.
Acknowledgments
This research was supported by grants from the County Council of Västmanland (Västmanlands läns Landsting) to Ann-Christin Johansson. The protocol has been examined and approved by the Ethics Committee at the Faculty of Medicine at Uppsala University.
References
- 1.Barrios C, Ahmed M, Arrotegui JI, Bjornsson A. Clinical factors predicting outcome after surgery for herniated lumbar discs: an epedemiological multivariate analysis. J Spinal Disord. 1990;3:205–209. doi: 10.1097/00002517-199009000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Bassett SF, Prapavessis H. Home-based physical therapy intervention with adherence-enhancing strategies versus clinic-based management for patients with ankle sprains. Phys Ther. 2007;87:1132–1143. doi: 10.2522/ptj.20060260. [DOI] [PubMed] [Google Scholar]
- 3.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 4.Choi G, Pai-Raiturker P, Kim MJ, Dai Jin C, Chae YS, Lee YS. The effect of early isolated lumbar extension exercise program for patients with herniated disc undergoing lumbar discectomy. Neurosurgery. 2005;57:764–772. doi: 10.1227/01.NEU.0000175858.80925.38. [DOI] [PubMed] [Google Scholar]
- 5.Danielsen J, Johnsen R, Kibsgaard S. Early, aggresive exercise for postoperative rehabilitation after discectomy. Spine. 2000;25:1015–1020. doi: 10.1097/00007632-200004150-00017. [DOI] [PubMed] [Google Scholar]
- 6.Davidson M, Keating JL. A comparison of five low back disability questionnaires: reliability and responsiveness. Phys Ther. 2002;82:8–24. doi: 10.1093/ptj/82.1.8. [DOI] [PubMed] [Google Scholar]
- 7.Carlo MS, Sell KE. The effects of the number and frequency of physical therapy treatments on selected outcomes of treatment in patients with anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1997;26:332–339. doi: 10.2519/jospt.1997.26.6.332. [DOI] [PubMed] [Google Scholar]
- 8.Boer J, Oosendorp R, Beems T, Munneke M, AW E. Continued disability and pain after lumbar disc surgery: the role of cognitive-behavioural factors. Pain. 2006;123:45–52. doi: 10.1016/j.pain.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 9.Boer JJ, Oostendorp RA, Beems T, Munneke M, Evers AW. Reduced work capacity after lumbar disc surgery: the role of cognitive-behavioral and work-related risk factors. Pain. 2006;126:72–78. doi: 10.1016/j.pain.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 10.Doland P, Greenfield K, Nelson RJ, Nelson IW. Can exercise therapy improve the outcome of microdiscectomy? Spine. 2000;25:1523–1532. doi: 10.1097/00007632-200006150-00011. [DOI] [PubMed] [Google Scholar]
- 11.Donaldson BL, Shipton EA, Inglis G, Rivett D, Frampton C. Comparison of usual surgical advice versus a nonaggravating six-month gym-based exercise rehabilitation program post-lumbar discectomy: results at one-year follow-up. Spine J. 2006;6:357–363. doi: 10.1016/j.spinee.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 12.Erdogmus CB, Resch KL, Sabitzer R, Muller H, Nuhr M, Schoggl A, Posch M, Osterode W, Ungersbock K, Ebenbichler GR. Physiotherapy-based rehabilitation following disc herniation operation: results of a randomized clinical trial. Spine. 2007;32:2041–2049. doi: 10.1097/BRS.0b013e318145a386. [DOI] [PubMed] [Google Scholar]
- 13.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 14.Fairbank JC, Pynsent PB. The Oswestry disability index. Spine. 2000;25:2940–2952. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 15.Filiz M, Cakmak A, Ozcan E. The effectiveness of exercise programmes after lumbar disc surgery: a randomized controlled study. Clin Rehabil. 2005;19:4–11. doi: 10.1191/0269215505cr836oa. [DOI] [PubMed] [Google Scholar]
- 16.Fordyce WE. Behavioral methods for chronic pain and illness. St Louis: Mosby; 1976. [Google Scholar]
- 17.George SZ, Fritz JM, Bialosky JE, Donald DA. The effect of a fear-avoidance-based physical therapy intervention for patients with acute low back pain: results of a randomized clinical trial. Spine. 2003;28:2551–2560. doi: 10.1097/01.BRS.0000096677.84605.A2. [DOI] [PubMed] [Google Scholar]
- 18.Gijsen R, Hoeymans N, Schellevis FG, Ruwaard D, Satariano WA, Bos GA. Causes and consequences of comorbidity: a review. J Clin Epidemiol. 2001;54:661–674. doi: 10.1016/S0895-4356(00)00363-2. [DOI] [PubMed] [Google Scholar]
- 19.Hakkinen A, Ylinen J, Kautiainen H, Tarvainen U, Kiviranta I. Effects of home strength training and stretching versus stretching alone after lumbar disk surgery: a randomized study with a 1-year follow-up. Arch Phys Med Rehabil. 2005;86:865–870. doi: 10.1016/j.apmr.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 20.Hurme M, Alaranta H. Factors predicting the results of surgery for lumbar intervertebral disc herniation. Spine. 1987;12:933–938. doi: 10.1097/00007632-198711000-00016. [DOI] [PubMed] [Google Scholar]
- 21.Häkkinen A, Kautiainen H, Jarvenpaa S, Arkela-Kautiainen M, Ylinen J. Changes in the total Oswestry Index and its items in females and males pre- and post-surgery for lumbar disc herniation: a 1-year follow up. Eur Spine J. 2006;16:347–352. doi: 10.1007/s00586-006-0187-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johannsen F, Remvig L, Kryger P, Beck P, Lybeck K, Larsen LH, Warming S, Dreyer V. Supervised endurance exercise training compared to home training after first lumbar diskectomy: a clinical trial. Clin Exp Rheumatol. 1994;12:609–614. [PubMed] [Google Scholar]
- 23.Jönsson B, Strömqvist B. Influence of age on symptoms and signs in lumbar disc herniation. Eur Spine J. 1995;4:202–205. doi: 10.1007/BF00303410. [DOI] [PubMed] [Google Scholar]
- 24.Kjellby-Wendt G, Carlsson SG, Styf J. Results of early active rehabilitation 5–7 years after surgical treatment for lumbar disc herniation. J Spinal Disord Tech. 2002;15:404–409. doi: 10.1097/00024720-200210000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Kjellby-Wendt G, Styf J, Carlsson SG. Early active rehabilitation after surgery for lumbar disc herniation: a prospective, randomized study of psychometric assessment in 50 patients. Acta Orthop Scand. 2001;72:518–524. doi: 10.1080/000164701753532871. [DOI] [PubMed] [Google Scholar]
- 26.Kjellby-Wendt G, Styyf J. Early active training after lumbar discectomy. A prospective, randomized, and controlled study. Spine. 1998;23:2345–2351. doi: 10.1097/00007632-199811010-00019. [DOI] [PubMed] [Google Scholar]
- 27.Korres DS, Loupassis G, Stamos K. Results of lumbar discectomy: a study using 15 different evaluation methods. Eur Spine J. 1992;1:20–24. doi: 10.1007/BF00302137. [DOI] [PubMed] [Google Scholar]
- 28.Lawson K, Reesor KA, Keefe FJ, Turner JA. Dimensions of pain-related cognitive coping: cross-validation of the factor structure of the Coping Strategy Questionnaire. Pain. 1990;43:195–204. doi: 10.1016/0304-3959(90)91073-R. [DOI] [PubMed] [Google Scholar]
- 29.Lindstrom I, Ohlund C, Nachemson A. Physical performance, pain, pain behavior and subjective disability in patients with subacute low back pain. Scand J Rehabil Med. 1995;27:153–160. [PubMed] [Google Scholar]
- 30.Lindstrom I, Öhlund C, Eek C, Wallin L, Peterson LE, Fordyce WE, Nachemson AL. The effect of graded activity on patients with subacute low back pain. Phys Ther. 1992;72:279–293. doi: 10.1093/ptj/72.4.279. [DOI] [PubMed] [Google Scholar]
- 31.Manniche C, Asmussen KH, Vinterberg H, Rose Hansen EB, Kramhoft J, Jordan A. Analysis of preoperative prognostic factors in first-time surgery for lumbar disc herniation, including Finneson’s and modified Sprengler’s score systems. Dan Med Bull. 1994;41:110–115. [PubMed] [Google Scholar]
- 32.Manniche C, Asmussen KH, Vinterberg H, Rose Hansen EB, Kramhoft J, Jordan A. Back pain, sciatica and disability following first time conventional haemilaminectomy for lumbar disc herniation. Use of “Low Back Pain Rating Scale” as a postal questionnaire. Dan Med Bull. 1994;41:103–106. [PubMed] [Google Scholar]
- 33.Manniche C, Skall H, Braendholt B, Christensen B, Christophersen L, Ellegaard B, Heilbuth A, Ingerslev M, Jorgensen O, Larsen E, Lorentzen L, Nielsen C, Nielsen H, Windelin M. Clinical trial of postoperative dynamic back exercises after first lumbar discectomy. Spine. 1993;18:92–97. doi: 10.1097/00007632-199301000-00014. [DOI] [PubMed] [Google Scholar]
- 34.Mannion AF, Denzler R, Dvorak J, Muntener M, Grob D. A randomised controlled trial of post-operative rehabilitation after surgical decompression of the lumbar spine. Eur Spine J. 2007;16:1101–1117. doi: 10.1007/s00586-007-0399-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mannion AF, Dvorak J, Muntener M, Grob D. A prospective study of the interrelationship between subjective and objective measures of disability before and 2 months after lumbar decompression surgery for disc herniation. Eur Spine J. 2005;14:454–465. doi: 10.1007/s00586-004-0787-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Miller RP, Kori SH, Todd DD (1991) The Tampa Scale. Unpublished Report, Tampa, FL
- 37.Millisdotter M, Stromqvist B. Early neuromuscular customized training after surgery for lumbar disc herniation: a prospective controlled study. Eur Spine J. 2007;16:19–26. doi: 10.1007/s00586-005-0044-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moore JE, Korff M, Cherkin D, Saunders K, Lorig K. A randomized trial of a cognitive-behavioral program for enhancing back pain self care in a primary care setting. Pain. 2000;88:145–153. doi: 10.1016/S0304-3959(00)00314-6. [DOI] [PubMed] [Google Scholar]
- 39.O’Sullivan PB, Twomey LT, Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylosis or spondylolisthesis. Spine. 1997;22:2959–2967. doi: 10.1097/00007632-199712150-00020. [DOI] [PubMed] [Google Scholar]
- 40.Ostelo RJ, de Vet HCW, Wadell G, Kerckhoffs MR, Leffers P, van Tulder MW (2002) Rehabilitation after lumbar disc surgery. Cochrane Database Syst Rev [DOI] [PubMed]
- 41.Ostelo RWJG, Vet HCW, Wadell G, Kerckhoffs MR, Lefflers P, Tulder M. Rehabilitation following first-time lumbar disc surgery. Spine. 2003;28:209–218. doi: 10.1097/00007632-200302010-00003. [DOI] [PubMed] [Google Scholar]
- 42.Ostelo RWJG, van Tulder MW, Vlaeyen JWS, Linton SJ, Morley SJ, Assendelft WJJ (2005) Behavioural treatment for chronic low-back-pain. Cochrane Database Syst Rev [DOI] [PubMed]
- 43.Pappas CTE, Harrington T, Sonntag VKH. Outcome analysis in 654 surgically treated lumbar disc herniations. Neurosurgery. 1992;30:862–866. doi: 10.1097/00006123-199206000-00007. [DOI] [PubMed] [Google Scholar]
- 44.Roddey TS, Olson SL, Gartsman GM, Hanten WP, Cook KF. A randomized controlled trial comparing 2 instructional approaches to home exercise instruction following arthroscopic full-thickness rotator cuff repair surgery. J Orthop Sports Phys Ther. 2002;32:548–559. doi: 10.2519/jospt.2002.32.11.548. [DOI] [PubMed] [Google Scholar]
- 45.Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- 46.Stromqvist B, Fritzell P, Hagg O, Jonsson B. One-year report from the Swedish National Spine Register. Swedish Society of Spinal Surgeons. Acta Orthop Suppl. 2005;76:1–24. doi: 10.1080/17453690510041950. [DOI] [PubMed] [Google Scholar]
- 47.Sullivan M, Karlsson J, Ware JE (1994) Hälsoenkät SF-36. Svensk manual och tolkningsguide (SF-36 Health survey, Swedish Manual and Interpretation Guide), Sahlgrenska University Hospital, Göteborg. Göteborgs Universitet
- 48.Sullivan MJ, Adams H, Rhodenizer T, Stanish WD. A psychosocial risk factor-targeted intervention for the prevention of chronic pain and disability following whiplash injury. Phys Ther. 2006;86:8–18. doi: 10.1093/ptj/86.1.8. [DOI] [PubMed] [Google Scholar]
- 49.Ware JEJ, Sherbourne CD. The MOS 36-item Short-Form health survey (SF-36). 1. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 50.Vlaeyen JW, Haazen IW, Schuerman JA, Kole-Snijders AM, Eek H. Behavioural rehabilitation of chronic low back pain: comparison of an operant treatment, an operant-cognitive treatment and an operant-respondent treatment. Br J Clin Psychol. 1995;34:95–118. doi: 10.1111/j.2044-8260.1995.tb01443.x. [DOI] [PubMed] [Google Scholar]
- 51.Vlaeyen JW, Kole-Snijders AM, Boeren RG, Eek H. Fear of movement/(re) injury in chronic low back pain and its relation to behavioural performance. Pain. 1995;62:363–372. doi: 10.1016/0304-3959(94)00279-N. [DOI] [PubMed] [Google Scholar]
- 52.Yilmaz F, Yilmaz A, Merdol F, Parlar D, Sahin F, Kuran B. Efficacy of dynamic lumbar stabilization exercise in lumbar microdiscectomy. J Rehabil Med. 2003;35:163–167. doi: 10.1080/16501970306125. [DOI] [PubMed] [Google Scholar]