Abstract
The objective of the study was to develop a clinical prediction rule (CPR) to identify patients with neck pain likely to improve with cervical traction. The study design included prospective cohort of patients with neck pain referred to physical therapy. Development of a CPR will assist clinicians in classifying patients with neck pain likely to benefit from cervical traction. Eighty patients with neck pain received a standardized examination and then completed six sessions of intermittent cervical traction and cervical strengthening exercises twice weekly for 3 weeks. Patient outcome was classified at the end of treatment, based on perceived recovery according to the global rating of change. Patients who achieved a change ≥+6 (“A great deal better” or “A very great deal better”) were classified as having a successful outcome. Univariate analyses (t tests and chi-square) were conducted on historical and physical examination items to determine potential predictors of successful outcome. Variables with a significance level of P ≤ 0.15 were retained as potential prediction variables. Sensitivity, specificity and positive and negative likelihood ratios (LRs) were then calculated for all variables with a significant relationship with the reference criterion of successful outcome. Potential predictor variables were entered into a step-wise logistic regression model to determine the most accurate set of clinical examination items for prediction of treatment success. Sixty-eight patients (38 female) were included in data analysis of which 30 had a successful outcome. A CPR with five variables was identified: (1) patient reported peripheralization with lower cervical spine (C4–7) mobility testing; (2) positive shoulder abduction test; (3) age ≥55; (4) positive upper limb tension test A; and (5) positive neck distraction test. Having at least three out of five predictors present resulted in a +LR equal to 4.81 (95% CI = 2.17–11.4), increasing the likelihood of success with cervical traction from 44 to 79.2%. If at least four out of five variables were present, the +LR was equal to 23.1 (2.5–227.9), increasing the post-test probability of having improvement with cervical traction to 94.8%. This preliminary CPR provides the ability to a priori identify patients with neck pain likely to experience a dramatic response with cervical traction and exercise. Before the rule can be implemented in routine clinical practice, future studies are necessary to validate the rule. The CPR developed in this study may improve clinical decision-making by assisting clinicians in identifying patients with neck pain likely to benefit from cervical traction and exercise.
Keywords: Neck pain, Classification, Cervical traction
Introduction
Neck pain is a common occurrence and source of disability within the general population with a lifetime incidence as high as 54% [12, 14]. Over one-third of patients with neck pain will develop chronic symptoms lasting more than 6 months [4, 14], representing a serious health concern [13, 49]. Over 50% of patients with neck pain seen by a general practitioner are referred for physical therapy [3].
Cervical traction is an intervention that is frequently recommended for the treatment of patients with neck pain [60]. Despite its relatively common use [41], the efficacy of cervical traction has not been adequately studied [29]. Additionally, recent systematic reviews have not endorsed the use of mechanical traction for patients with neck pain; however, these reviews note the poor methodological quality of available research [25, 29, 50, 55].
The lack of evidence for cervical traction among patients with neck pain may be partly attributed to the inability of researchers to define the relevant sub-group of patients who are most likely to benefit from this treatment [19, 22]. Without the ability to match the right patient to a specific intervention, therapists are left with little evidence to guide their practice.
Clinical prediction rules (CPR) are commonly used in medical practice to improve decision-making by matching a treatment to a specific sub-group of patients. Once the CPR has been developed, it must be validated to determine its ability to improve decision-making, impact clinical practice, improve patient outcomes, and decrease costs. Sub-grouping methods show considerable promise in improving outcomes in patients with low back pain [5, 8, 22]. Recently, a CPR was developed for classifying patients with neck pain who respond best to thoracic spine manipulation [9].
Several authors have suggested clinical criteria for identifying patients with neck pain likely to respond to traction [6, 21, 48, 61]. Experts generally agree that traction is most appropriate for patients with neck and upper extremity symptoms, and signs of neurological compromise, for whom centralization of symptoms is a treatment goal [47]. Despite these theories, no decision-making strategies have been identified to help the clinician determine who will respond to cervical traction. The purpose of this study was to develop a CPR to identify patients with neck pain who are likely to benefit from traction based on a reference standard of patient-reported improvement.
Methods and materials
We conducted a prospective cohort study of patients with neck pain referred to physical therapy at Brooke Army Medical Center in San Antonio, Texas. Inclusion criteria required patients to be 18 years of age or older, with a primary complaint of neck pain with or without upper extremity symptoms, and a baseline neck disability index (NDI) score of 20% or greater. Exclusion criteria were as follows: identification of any medical red flags suggestive of a non-musculoskeletal etiology of symptoms, pregnancy, or any evidence of vascular compromise, central nervous system involvement or multiple-level neurological impairments. All patients reviewed and signed a consent form approved by the Institutional Review Board at Brooke Army Medical Center, San Antonio, Texas.
Therapists
Five physical therapists who were fellows in the US Army-Baylor University Post-professional Doctoral Program in Orthopaedic Manual Physical Therapy completed the examination and treatments. All therapists underwent a standardized training regimen which included studying a manual of operational procedures and viewing video clips demonstrating each examination and treatment procedure used in this study. Therapists then underwent a 2-h training session in which they practiced the examination and treatment protocol to ensure that all study procedures were performed in a standardized fashion. On average, participating therapists had 10.0 years (SD 5.61, range 4–17 years) of clinical experience.
Examination procedures
Patients provided demographic information and completed a variety of self-report measures, followed by a standardized history and physical examination at baseline. Self-report measures included a body diagram [61], numeric pain rating scale (NPRS) [35], the NDI [56], and fear-avoidance beliefs questionnaire (FABQ) [58]. Patients recorded the location of their symptoms on the body diagram.
The NPRS was used to record the patients’ level of pain. The FABQ was used to quantify the patients’ beliefs about the influence of work and activity on their neck pain [23, 32, 58], and the NDI was used to capture the patients perceived level of disability due to their neck pain [56]. Both the FABQ and the NDI have been shown to be reliable and valid [7, 23].
The historical examination included questions regarding the mode of onset, nature and location of symptoms, aggravating and relieving factors, and prior history of neck pain. The physical examination included a neurological screen [46], postural assessment [40], cervical range of motion measurements and symptoms response [44], assessment of the length [46] and strength [40] of the muscles of the upper quarter, and endurance of the deep neck flexor (DNF) muscles [26]. The amount of motion and symptom response was recorded for segmental mobility testing [45, 46] of the cervical and thoracic spine (C2–T4). The physical examination also included several special tests typically performed in the examination of patients with neck pain, including the Spurling test [54], Quadrant test (also called Spurling’s B) [57, 59], cervical distraction test [59], and the upper limb tension test A [17]. Specific operational definitions for all tests used and criteria defining a positive test are included in Appendix A.
Intervention
Based on the purpose of the study, all patients received a standardized treatment regimen regardless of the results of the clinical examination [33]. Patients received a treatment combination of both cervical traction and active exercise 2–3 times per week for a total of six treatments over a 3-week period. Patients were also advised to maintain their normal activity level as long as it did not exacerbate their pain. The first treatment session was performed on the day of the initial examination unless a pregnancy test was required, then patients were scheduled within 1–2 days to begin their first traction treatment. A follow-up examination was completed on the last visit. Patients completed a daily exercise log to record compliance with the home exercise program.
Cervical traction
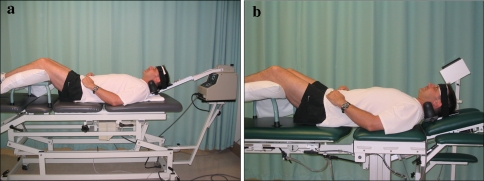
Intermittent mechanical traction was performed using one of two traction units: the Chattanooga Triton Traction Table (Fig. 1a) and the Saunders 3D Active Trac Table (Fig. 1b). Both traction units were calibrated before the research study began.
Fig. 1.
a Chattanooga Triton Traction Table model MP-1/TRE-24 and b Saunders3D Active Trac Table
Traction was performed with the patient in supine with the legs supported comfortably on a padded stool. The angle of pull was set to 24° of flexion if the patient had full cervical flexion active range of motion; otherwise it was set to 15°. The on/off cycle was set to 60 s of pull force and 20 s of relaxation force. Traction force during the off time was set to 50% of pull force. The initial pull force was set to 10–12 pounds (approximate weight of the patient’s head), then incrementally adjusted upwards within the first treatment session to optimally reduce the patient’s symptoms. In general, patients were instructed that the force should feel “moderately strong to strong” without increasing symptoms. Force of pull was incrementally adjusted on subsequent sessions as well, based on the patient’s tolerance to previous traction treatments and the symptom response. A maximum pull force of 40 lbs was set. Each session lasted approximately 15 min. The average force of pull for this study was 23.2 lbs ± 5.6 lbs (range 12–38 lbs). There was no statistical difference in force of pull between those who had success with traction and those who did not.
Exercise
An active exercise intervention was included as part of the overall treatment program because it is frequently used clinically to treat patients with neck pain [38, 39, 52, 62, 63]. There is growing evidence that patients with neck pain have weakness and/or motor control difficulties in facilitating the DNF muscles [37, 53, 56]. One high quality RCT also suggests that an active exercise program consisting of DNF training and postural exercise is beneficial for improvement in neck pain, headache frequency and intensity [38].
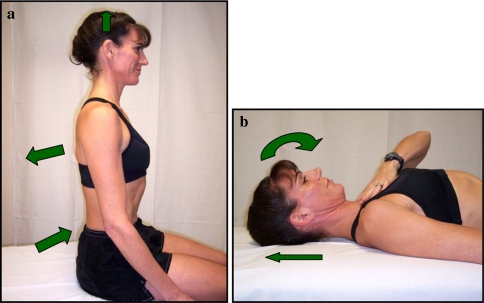
Based on this evidence, all patients were instructed in two exercises following the initial traction treatment: a seated posture exercise (Fig. 2a) and a supine DNF strengthening exercise (Fig. 2b). Both exercises were performed in the clinic and then daily as part of a home exercise program. Patients performed the seated posture exercise in sitting with the spine in a natural lumbar lordosis. The patients retracted and adducted their scapulas and gently elongated their cervical spines to achieve a neutral upright postural position [38]. Patients were instructed to hold this position for at least 10 s and complete this exercise 2 times per h. For the supine DNF strengthening exercise, patients were instructed to perform a slow and controlled craniocervical flexion motion without contracting the large, superficial muscles of the neck. Patients held each contraction for 10 s and performed ten repetitions twice daily.
Fig. 2.
a Seated posture exercise and b supine deep neck flexor exercise
The global rating of change (GROC) served as the reference criterion for establishing a successful outcome. The GROC is a 15-point global rating scale ranging from −7 (“A very great deal worse”) to zero (“About the same”) to +7 (“A very great deal better”) [34]. Intermittent descriptors of worsening or improving symptoms are assigned values from −1 to −6 and +1 to +6, respectively [42, 43]. It has been reported that scores of +4 and +5 are indicative of moderate changes in patient status and scores of +6 and +7 indicate large changes in patient status [34]. It was determined a priori that patients who rated their perceived recovery on the GROC as “A great deal better” or “A very great deal better” (i.e., a score of +6 or greater), at the post-treatment examination were categorized as a success. A high threshold for defining “success” was established to maximize the likelihood that the clinical outcome could be attributable to the intervention as opposed to the passage of time. Patients whose scores on the GROC did not exceed the +6 cut off at the post-treatment examination were categorized as having a non-successful outcome.
In contrast to other studies which identified predictor variables for treatment success [19, 28], we elected to use the patient’s perceived recovery rather than a region-specific disability measure such as the NDI to judge a patient’s success. The GROC is considered to be a valid reference standard for identifying clinically important change [2, 18, 31], and the NDI has been criticized for not being sufficiently responsive to capture small, but clinically important, changes in disability [30]. In addition, perceived recovery has previously been used in trials of patients with neck pain and has shown to be responsive to physical therapy management programs [30, 43].
Data analysis
At the end of treatment, patients were dichotomized as having experienced either a successful or unsuccessful outcome based on their self-reported GROC score. Patients who achieved a change greater than or equal to +6 (“A great deal better” or “A very great deal better”) were classified as having successful outcomes. The mean NDI and NPRS change scores [and 95% confidence intervals (CIs)] were calculated for both groups and analyzed using an independent t test to validate that a difference existed between groups based on the GROC reference criterion.
Individual variables from the self-report measures and the history and physical examination were tested for univariate relationship with the GROC reference criterion using independent-samples t tests for continuous variables and chi-square tests for categorical variables. Variables with a significance level of P ≤ 0.15 were retained as potential prediction variables [20]. This significance level was selected to decrease the likelihood that potentially meaningful predictor variables would be overlooked.
For continuous variables with a significant univariate relationship, sensitivity and specificity values were calculated for all possible cutoff points and then plotted as a receiver operator characteristic (ROC) curve [16]. The point on the curve nearest the upper left-hand corner represented the value with the best diagnostic accuracy, and this point was selected as the cutoff defining a positive test [16]. Sensitivity, specificity, and positive and negative likelihood ratios (LRs) were then calculated for variables with a significant relationship with the reference criterion of successful outcome. Potential predictor variables were entered into a step-wise logistic regression model to determine the most accurate set of variables for prediction of treatment success. Variables retained in the regression model were used to form the most parsimonious combination of predictors for identifying patients with neck pain likely to benefit from cervical spine traction and exercise.
Results
Between January 2006 and April 2007, 80 subjects were recruited for the study. Twelve subjects did not complete the study for various reasons, thus their data were excluded. Therefore, 68 patients (38 female) were included in the data analysis.
Subject demographics and initial baseline variables from the patient history and self-report measures for the entire sample as well as for the successful outcome and non-successful outcome groups are presented in Table 1. Thirty patients (44%) were categorized as having achieved successful outcomes, and 38 subjects were categorized as having achieved non-successful outcomes. Analysis of NPRS and NDI change scores revealed that the successful outcome group experienced significantly greater improvements (P < 0.001) in pain (NPRS change score = 2.2, 95% CI = 1.2–3.2) and disability (NDI change score = 12.5, 95% CI = 6.2–18.7) over the non-successful group.
Table 1.
Demographics and baseline characteristics of subjects
| Variable | All subjects | Success with cervical traction | Failure to improve with cervical traction |
|---|---|---|---|
| Age, mean (SD) | 47.8 (10.7) | 49.9 (10.94) | 46.1 (10.28) |
| NPRS, mean (SD) | 4.55 (2.05) | 5.13 (2.27) | 4.09 (1.79) |
| Body mass index (kg/m2), mean (SD) | 28.13 (4.64) | 29.85 (4.50) | 26.95 (4.61) |
| Current smoker (%) | 47.1% | 22.1% | 25.0% |
| History of neck pain (%) | 30% | 29.4% | 64.7% |
| Missed any work for neck pain (%) | 25.0% | 14.7% | 10.3% |
| NDI (%), mean (SD) | 33.1 (12.7) | 34.9 (16.1) | 31.7 (9.2) |
| FABQPA, mean (SD) | 13.99 (7.25) | 14.67 (6.30) | 13.45 (7.95) |
| FABQW, mean (SD) | 14.31 (10.2) | 13.0 (10.8) | 15.32 (9.76) |
| Mean duration of symptoms (days) | 292.4 (678.5) | 374.1 (867.9) | 228.0 (483.3) |
NPRS numeric pain rating scale, GROC global rating of change, NDI neck disability index, FABQPA fear avoidance belief/physical activity, FABQW fear avoidance belief/work subscale
The 15 potential predictor variables (Table 2) that exhibited a significance level of less than or equal to 0.15 were entered into the logistic regression. The cutoff values determined by the ROC curves were 28.4 for BMI, 55 years for age, 55° for cervical flexion, 40° for cervical side bending, and 60° for cervical rotation, both to the symptomatic side. Accuracy statistics for all 15 variables with 95% CIs are shown in Table 2. The positive LRs ranged from 0.66 to 4.43, with the strongest predictor being age ≥55 years.
Table 3.
The five variables forming the clinical prediction rule and the number of subjects in each group at each level
| Number of predictors present | Success with cervical traction (% of pts) | Non-success with cervical traction (% of pts) | Total patients (% of pts) |
|---|---|---|---|
| ≥4 | 9 (13.2) | 0 | 9 (13.2) |
| ≥3 | 10 (14.7) | 5 (7.4) | 15 (22.1) |
| ≥2 | 6 (8.8) | 17 (25) | 23 (33.8) |
| ≥1 | 4 (5.8) | 10 (14.7) | 14 (20.6) |
| 0 | 1 (1.5) | 6 (8.8) | 7 (10.3) |
Age ≥55
Positive shoulder abduction test
Positive ULTT A
Symptom peripheralization with central posterior–anterior motion testing at lower cervical (C4–7) spine
Positive neck distraction test
Table 2.
Sensitivity, specificity, and likelihood ratios for variables with a significant univariate relationship with responding favorably to intermittent cervical traction
| Variable | Sensitivity | Specificity | P value | Positive likelihood ratio | Negative likelihood ratio |
|---|---|---|---|---|---|
| Neck distraction test | 0.83 (0.66–0.93) | 0.50 (0.35–0.65) | 0.004 | 1.67 (1.18–2.45) | 0.33 (0.14–0.73) |
| Pain with MMT | 0.63 (0.46–0.78) | 0.71 (0.55–0.83) | 0.005 | 2.19 (1.27–3.92) | 0.52 (0.30–0.82) |
| Body mass index ≥28.4 | 0.67 (0.49–0.81) | 0.68 (0.53–0.81) | 0.006 | 2.11 (1.26–3.66) | 0.49 (0.27–0.81) |
| Frequency of past episodes | 0.70 (0.48–0.85) | 0.67 (0.47–0.82) | 0.026 | 2.10 (1.15–4.08) | 0.45 (0.21–0.87) |
| Symptoms distal to shoulder | 0.67 (0.49–0.81) | 0.58 (0.42–0.72) | 0.044 | 1.58 (1.01–2.53) | 0.58 (0.32–0.99) |
| Shoulder abduction test | 0.33 (0.19–0.51) | 0.87 (0.73–0.94) | 0.046 | 2.53 (1.01–6.50) | 0.77 (0.55–1.00) |
| Headaches | 0.43 (0.27–0.61) | 0.55 (0.40–0.70) | 0.073 | 0.97 (0.56–1.65) | 1.02 (0.65–1.57) |
| Diminished strength | 0.43 (0.27–0.61) | 0.76 (0.61–0.87) | 0.085 | 1.83 (0.92–3.69) | 0.74 (0.50–1.04) |
| Peripheralization with PA C4–7 | 0.37 (0.22–0.54) | 0.82 (0.67–0.91) | 0.090 | 1.99 (0.90–4.47) | 0.78 (0.54–1.04) |
| Ipsilateral rotation <60° | 0.43 (0.27–0.61) | 0.66 (0.50–0.79) | 0.090 | 1.27 (0.69–2.31) | 0.86 (0.57–1.26) |
| Patient reported neck stiffness | 0.43 (0.27–0.61) | 0.34 (0.21–0.50) | 0.104 | 0.66 (0.40–1.02) | 1.65 (0.97–2.88) |
| Flexion AROM <55° | 0.60 (0.42–0.75) | 0.55 (0.40–0.70) | 0.117 | 1.34 (0.84–2.14) | 0.72 (0.42–1.19) |
| Positive ULTT A | 0.80 (0.63–0.90) | 0.37 (0.23–0.53) | 0.130 | 1.27 (0.93–1.75) | 0.54 (0.23–1.18) |
| Age ≥55 | 0.47 (0.30–0.64) | 0.89 (0.76–0.96) | 0.150 | 4.43 (1.74–11.89) | 0.60 (0.40–0.81) |
| Ipsilateral sidebending <40° | 0.73 (0.56–0.86) | 0.45 (0.30-0.60) | 0.150 | 1.33 (0.92–1.93) | 0.60 (0.29–1.14) |
The following five variables were retained in the final regression model: (1) patient reported peripheralization with lower cervical spine (C4–7) mobility testing; (2) positive shoulder abduction test; (3) age ≥55; (4) positive upper limb tension test A; and (5) positive neck distraction test. The five variables forming the CPR and the number of subjects in each group at each level are shown in Table 3.
Accuracy statistics were calculated based on the number of predictors present (Table 4). The pretest probability for the likelihood of having a successful outcome was 44% (30 out of 68 patients). Having at least three out of five predictors present resulted in a +LR equal to 4.81 (95% CI = 2.17–11.4), increasing the likelihood of success with cervical traction from 44 to 79.2%. If at least four out of five variables were present, the +LR was equal to 23.1 (2.5–227.9), increasing the post-test probability of having improvement with cervical traction to 94.8%. There were no patients meeting at least 4/5 criteria who experienced a non-successful outcome, thus the +LR could not be calculated because the equation resulted in a zero for the denominator. Therefore, 0.5 was added to this cell in the table to avoid division by zero error and permit calculation of the +LR [59].
Table 4.
Combination of predictor variables and associated accuracy statistics with 95% confidence intervals
| Number of predictors present | Sensitivity | Specificity | Positive likelihood ratio | Negative likelihood ratio | Probability of success with cervical traction (%) |
|---|---|---|---|---|---|
| ≥4 | 0.30 (0.17–0.48) | 1.0 (0.91–1.0) | 23.1 (2.50–227.90) | 0.71 (0.53–0.85) | 94.8 |
| ≥3 | 0.63 (0.46–0.78) | 0.87 (0.73–0.94) | 4.81 (2.17–11.4) | 0.42 (0.25–0.65) | 79.2 |
| ≥2 | 0.30 (0.17–0.48) | 0.97 (0.87–1.00) | 1.44 (1.05–2.03) | 0.40 (0.16–0.90) | 53.2 |
| ≤1 | 0.07 (0.02–0.21) | 0.97 (0.87–1.00) | 1.15 (0.97–1.4) | 0.21 (0.03–1.23) | 47.6 |
The probability of successful outcome after cervical traction is calculated using the positive likelihood ratios and assumes 44% of patients will have a favorable outcome after cervical traction treatment regardless of the number of predictors present. Accuracy statistics with 95% confidence intervals for individual variables for predicting success with cervical traction
Discussion
The purpose of this study was to improve decision-making for patients with neck pain by identifying the sub-group of patients likely to benefit from cervical traction and exercise. The pretest probability of success with cervical traction was 44%. We elected to report the positive LR because the purpose of this study was to determine the change in probability that patients are likely to experience a successful outcome when they satisfy the rule’s criteria [7]. If a patient exhibited four out of five criteria, the post-test probability of success increased to 94.8%. However, having at least three out of five predictors present still resulted in a post-test probability of 79.2%, thus having three out of five predictors appears to be the optimal threshold for decision-making. Conversely, having fewer than two predictors present might indicate a sub-group who would preferentially benefit from a different intervention. For example, if the patient only had one of the predictor variables, the post-test probability of benefitting from cervical traction and exercise is only 47.6%, which is less than chance.
One of the initial judgment’s of a CPR’s validity is whether the predictors that emerge have biologic plausibility for their inclusion [7]. In clinical studies reporting success with cervical traction, patient populations included those with cervical radiculopathy or compressive myelopathy [1, 6, 36, 48, 51]. Several preliminary studies attempting to identify the sub-group of patients with neck pain like to benefit from traction have included patients with distal symptoms who demonstrate signs of nerve root compression [10, 21]. A diagnostic test study has also demonstrated that patients with cervical radiculopathy are represented by patients with clinical signs and symptoms associated with nerve root compression [59]. Of the five predictor variables that were retained in the final rule from this study, four of the predictors appear to have a relationship to cervical nerve root compression. This supports the notion that patients presenting with signs of nerve root compression may represent the sub-group of patients most likely to benefit from cervical traction. Peripheralization of symptoms with lower cervical spine mobility testing and a positive ULTT A may indicate adverse mechanical compression on neural structures, whereas relief of symptoms during the neck distraction test and shoulder abduction test would demonstrate relief of neural compression or tension.
Significant variability exists in the dosing parameters utilized in cervical traction studies, which may account for the lack of conclusive evidence that traction is an effective intervention for patients with neck pain. The parameters used were based on a review of the literature and consultation with experienced clinicians and researchers. One parameter which had the greatest variability was force of pull. Forces as little as 5 lbs [11, 15] and as much as 40 lbs [24] have been utilized with varying results. We chose to pull at a force that was designed to optimally centralize and/or reduce the patient’s symptoms. Many previous studies demonstrating benefit for cervical traction have utilized forces of at least 20 pounds [27, 36, 64]. Therefore, we started the dose at 10–12 pounds, then incrementally adjusted it upwards within and between treatment sessions to optimally centralize and/or reduce the patient’s symptoms. Future studies should investigate the optimal dosing of traction, both in the amount of force utilized and the frequency of visits.
One of the limitations of this initial study is that no comparison group was utilized. Therefore, we cannot be assured that patients were responding specifically to cervical traction and exercise rather than the passage of time. However, the predictors that emerged in this rule are not typically thought to be associated with a favorable natural history, and in fact are commonly associated with chronicity [4, 12, 14]. We also utilized a high threshold in our definition of a successful outcome. This protected against the possibility that the patients’ responses could be attributed to the passage of time. Future research should validate whether the same criteria emerge in a different population and utilize a comparison group to verify that these criteria are specifically associated with a response to cervical traction and exercise.
Conclusion
This preliminary CPR provides the ability to a priori identify the sub-group of patients with neck pain likely to benefit from cervical traction and exercise, which has the potential to improve decision-making in clinical practice. The results of this study represent the initial step in the development of a prediction rule. Future studies are needed to validate the rule and determine its impact on clinical practice patterns, patient outcomes, and costs.
Conflict of interest statement
We affirm that we have no financial affiliation (including research funding) or involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript, except as disclosed in an attachment and cited in the manuscript. Any other conflict of interest (i.e., personal associations or involvement as a director, officer, or expert witness) is also disclosed in an attachment. The Saunders Group, Inc. loaned the investigative team use of a 3D ActiveTrac table for this study. The company played no role in the design, conduct, or reporting of the study or in the decision to submit the manuscript for publication.
Appendix A
Table 5
Table 5.
Operational definitions for special tests used in the study
| Test | Performance | Criteria for positive test |
|---|---|---|
| Adson’s maneuver | Patient is seated. Examiner locates the patient’s radial pulse with the elbow extended. Patient then rotates head toward test shoulder and extends head/neck. Examiner then externally rotates and extends the patient’s shoulder as the patient takes a deep breath and holds it | Reproduction of symptoms in tested UE with diminished or absent pulse |
| Cervical rotation lateral flexion (CRLF) test | Patient is seated. The examiner passively and maximally rotates head away from the side being tested. In this position, the cervical spine is flexed, bringing the ear toward the sternum | If flexion is restricted compared to the opposite side then the test is positive for a hypomobile first rib |
| Spurling A | Patient is seated. The examiner passively side bends the patient’s head toward the symptomatic side and then applies approximately 7 kg of overpressure to the patient’s head | Reproduction of patient symptoms |
| Quadrant test (Spurling B) | Patient is seated. The examiner passively side bends and rotates the patient’s head toward the symptomatic side and then induces cervical extension. Next, approximately 7 kg of overpressure is applied to the patient’s head | Reproduction of patient symptoms |
| Neck distraction test | Patient lies supine and the neck comfortably positioned. The examiner securely grasps the patient’s head under the occipit and chin and gradually applies an axial traction force up to approximately 30 pounds | Reduction or elimination of symptoms |
| Valsalva maneuver | Patient is seated and instructed to take a deep breath and hold the breath while attempting to exhale over a 2–3-s period with gradually increasing force | Reproduction of patient symptoms |
| Upper limb tension test A | With the patient supine, the examiner sequentially introduces the following movements to the symptomatic upper extremity: a. Scapular depression b. Shoulder abduction c. Forearm supination d. Wrist and finger extension e. Shoulder external rotation f. Elbow extension g. Contralateral then ipsilateral cervical side bending |
Reproduction of patient’s symptoms |
| Shoulder abduction test | While sitting, the patient is instructed to place the hand of the affected extremity on the head in order to support the extremity in the scapular plane | Alleviation of patient symptoms |
Footnotes
This study was approved by the Institutional Review Board at Brooke Army Medical Center, Fort Sam Houston, Texas. The opinions and assertions contained herein are the private views of the authors and are not to be construed as official as reflecting the views of the Department of the Army, Department of the Air Force, Department of the Navy, or the Department of Defense.
Contributor Information
Nicole H. Raney, Phone: +1-210-6676192, Email: Sanantoniogirl1@hotmail.com
Evan J. Petersen, Email: evan.petersen@amedd.army.mil
Tracy A. Smith, Email: tracy.alexandra.smith@gmail.com
James E. Cowan, Email: James.cowan@navsoc.socom.mil
Daniel G. Rendeiro, Email: Daniel.rendeiro@amedd.army.mil
Gail D. Deyle, Email: gdeyle@satx.rr.com
John D. Childs, Email: childsjd@gmail.com
References
- 1.Abdulwahab SS, Sabbahi M. Neck retractions, cervical root decompression, and radicular pain. J Orthop Sports Phys Ther. 2000;30:4–9. doi: 10.2519/jospt.2000.30.1.4. [DOI] [PubMed] [Google Scholar]
- 2.Bolton JE. Sensitivity and specificity of outcome measures in patients with neck pain: detecting clinically significant improvement. Spine. 2004;29:2410–2417. doi: 10.1097/01.brs.0000143080.74061.25. [DOI] [PubMed] [Google Scholar]
- 3.Borghouts J, Janssen H, Koes B, Muris J, Metsemakers J, Bouter L. The management of chronic neck pain in general practice. A retrospective study. Scand J Prim Health Care. 1999;17:215–220. doi: 10.1080/028134399750002430. [DOI] [PubMed] [Google Scholar]
- 4.Bovim G, Schrader H, Sand T. Neck pain in the general population. Spine. 1994;19:1307–1309. doi: 10.1097/00007632-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Brennan GP, Fritz JM, Hunter SJ, Thackeray A, Delitto A, Erhard RE. Identifying subgroups of patients with acute/subacute “nonspecific” low back pain: results of a randomized clinical trial. Spine. 2006;31:623–631. doi: 10.1097/01.brs.0000202807.72292.a8. [DOI] [PubMed] [Google Scholar]
- 6.Browder DA, Erhard RE, Piva SR. Intermittent cervical traction and thoracic manipulation for management of mild cervical compressive myelopathy attributed to cervical herniated disc: a case series. J Orthop Sports Phys Ther. 2004;34:701–712. doi: 10.2519/jospt.2004.34.11.701. [DOI] [PubMed] [Google Scholar]
- 7.Childs JD, Cleland JA. Development and application of clinical prediction rules to improve decision making in physical therapist practice. Phys Ther. 2006;86:122–131. doi: 10.1093/ptj/86.1.122. [DOI] [PubMed] [Google Scholar]
- 8.Childs JD, Fritz JM, Flynn TW, Irrgang JJ, Johnson KK, Majkowski GR, Delitto A. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med. 2004;141:920–928. doi: 10.7326/0003-4819-141-12-200412210-00008. [DOI] [PubMed] [Google Scholar]
- 9.Cleland JA, Childs JD, Fritz JM, Whitman JM, Eberhart SL. Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: use of thoracic spine manipulation, exercise, and patient education. Phys Ther. 2007;87:9–23. doi: 10.2522/ptj.20060155. [DOI] [PubMed] [Google Scholar]
- 10.Cleland JA, Fritz JM, Whitman JM, Heath R. Predictors of short-term outcome in people with a clinical diagnosis of cervical radiculopathy. Phys Ther. 2007;87:1619–1632. doi: 10.2522/ptj.20060155. [DOI] [PubMed] [Google Scholar]
- 11.Constantoyannis C, Konstantinou D, Kourtopoulos H, Papadakis N. Intermittent cervical traction for cervical radiculopathy caused by large-volume herniated disks. J Manip Physiol Ther. 2002;25:188–192. doi: 10.1067/mmt.2001.123356. [DOI] [PubMed] [Google Scholar]
- 12.Cote P, Cassidy JD, Carroll L. The factors associated with neck pain and its related disability in the Saskatchewan population. Spine. 2000;25:1109–1117. doi: 10.1097/00007632-200005010-00012. [DOI] [PubMed] [Google Scholar]
- 13.Cote P, Cassidy JD, Carroll L. The epidemiology of neck pain: what we have learned from our population-based studies. J Can Chiropract Assoc. 2003;47:284–290. [Google Scholar]
- 14.Cote P, Cassidy JD, Carroll LJ, Kristman V. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain. 2004;112:267–273. doi: 10.1016/j.pain.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Crue BL, Todd EM. The importance of flexion in cervical halter traction. Bull Los Angel Neuro Soc. 1965;30:95–98. [PubMed] [Google Scholar]
- 16.Deyo RA, Centor RM. Assessing the responsiveness of functional scales to clinical change: an analogy to diagnostic test performance. J Chronic Dis. 1986;39:897–906. doi: 10.1016/0021-9681(86)90038-X. [DOI] [PubMed] [Google Scholar]
- 17.Elvey RL (1994) The investigation of arm pain: signs of adverse responses to the physical examination of the brachial plexus and related tissues. In: Boyling JD, Palastanga N (eds) Grieve’s modern manual therapy, 2nd edn. Churchill Livingstone, New York
- 18.Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 19.Flynn T, Fritz J, Whitman J, Wainner R, Magel J, Rendeiro D, Butler B, Garber M, Allison S. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine. 2002;27:2835–2843. doi: 10.1097/00007632-200212150-00021. [DOI] [PubMed] [Google Scholar]
- 20.Freedman D. A note on screening regression equations. Am Stat. 1983;37:152–155. doi: 10.2307/2685877. [DOI] [Google Scholar]
- 21.Fritz JM, Brennan GP. Preliminary examination of a proposed treatment-based classification system for patients receiving physical therapy interventions for neck pain. Phys Ther. 2007;87:513–524. doi: 10.2522/ptj.20060101. [DOI] [PubMed] [Google Scholar]
- 22.Fritz JM, Delitto A, Erhard RE. Comparison of classification-based physical therapy with therapy based on clinical practice guidelines for patients with acute low back pain: a randomized clinical trial. Spine. 2003;28:1363–1371. doi: 10.1097/00007632-200307010-00003. [DOI] [PubMed] [Google Scholar]
- 23.George SZ, Fritz JM, Erhard RE. A comparison of fear-avoidance beliefs in patients with lumbar spine pain and cervical spine pain. Spine. 2001;26:2139–2145. doi: 10.1097/00007632-200110010-00019. [DOI] [PubMed] [Google Scholar]
- 24.Goldie I, Landquist A. Evaluation of the effects of different forms of physiotherapy in cervical pain. Scand J Rehabil Med. 1970;2:117–121. [PubMed] [Google Scholar]
- 25.Graham N, Gross AR, Goldsmith C. Mechanical traction for mechanical neck disorders: a systematic review. J Rehabil Med. 2006;38:145–152. doi: 10.1080/16501970600583029. [DOI] [PubMed] [Google Scholar]
- 26.Harris KD, Heer DM, Roy TC, Santos DM, Whitman JM, Wainner RS. Reliability of a measurement of neck flexor muscle endurance. Phys Ther. 2005;85:1349–1355. [PubMed] [Google Scholar]
- 27.Harris PR. Cervical traction. Review of literature and treatment guidelines. Phys Ther. 1977;57:910–914. doi: 10.1093/ptj/57.8.910. [DOI] [PubMed] [Google Scholar]
- 28.Hicks GE, Fritz JM, Delitto A, McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil. 2005;86:1753–1762. doi: 10.1016/j.apmr.2005.03.033. [DOI] [PubMed] [Google Scholar]
- 29.Hoving JL, Gross AR, Gasner D, Kay T, Kennedy C, Hondras MA, Haines T, Bouter LM. A critical appraisal of review articles on the effectiveness of conservative treatment for neck pain. Spine. 2001;26:196–205. doi: 10.1097/00007632-200101150-00015. [DOI] [PubMed] [Google Scholar]
- 30.Hoving JL, Koes BW, Vet HC, Windt DA, Assendelft WJ, Mameren H, Deville WL, Pool JJ, Scholten RJ, Bouter LM. Manual therapy, physical therapy, or continued care by a general practitioner for patients with neck pain. A randomized, controlled trial. Ann Intern Med. 2002;136:713–722. doi: 10.7326/0003-4819-136-10-200205210-00006. [DOI] [PubMed] [Google Scholar]
- 31.Hurst H, Bolton J. Assessing the clinical significance of change scores recorded on subjective outcome measures. J Manip Physiol Ther. 2004;27:26–35. doi: 10.1016/j.jmpt.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 32.Jacob T, Baras M, Zeev A, Epstein L. Low back pain: reliability of a set of pain measurement tools. Arch Phys Med Rehabil. 2001;82:735–742. doi: 10.1053/apmr.2001.22623. [DOI] [PubMed] [Google Scholar]
- 33.Jaeschke R, Guyatt GH, Sackett DL. Users’ guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The evidence-based medicine working group. JAMA. 1994;271:703–707. doi: 10.1001/jama.271.9.703. [DOI] [PubMed] [Google Scholar]
- 34.Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10:407–415. doi: 10.1016/0197-2456(89)90005-6. [DOI] [PubMed] [Google Scholar]
- 35.Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994;58:387–392. doi: 10.1016/0304-3959(94)90133-3. [DOI] [PubMed] [Google Scholar]
- 36.Joghataei MT, Arab AM, Khaksar H. The effect of cervical traction combined with conventional therapy on grip strength on patients with cervical radiculopathy. Clin Rehabil. 2004;18:879–887. doi: 10.1191/0269215504cr828oa. [DOI] [PubMed] [Google Scholar]
- 37.Jull G, Kristjansson E, Dall’Alba P. Impairment in the cervical flexors: a comparison of whiplash and insidious onset neck pain patients. Man Ther. 2004;9:89–94. doi: 10.1016/S1356-689X(03)00086-9. [DOI] [PubMed] [Google Scholar]
- 38.Jull G, Trott P, Potter H, Zito G, Niere K, Shirley D, Emberson J, Marschner I, Richardson C. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine. 2002;27:1835–1843. doi: 10.1097/00007632-200209010-00004. [DOI] [PubMed] [Google Scholar]
- 39.Kay TM, Gross A, Goldsmith C, Santaguida PL, Hoving J, Bronfort G (2005) Exercises for mechanical neck disorders. Cochrane Database Syst Rev CD004250 [DOI] [PubMed]
- 40.Kendall FME, Provance PG. Muscles: testing and function. Baltimore: Williams and Wilkins; 1993. [Google Scholar]
- 41.Klaber HG, Moffett JA, Hughes GI, Griffeths P. An investigation of the effects of cervical traction. Part 1: clinical effectiveness. Clin Rehabil. 1990;4:205–211. doi: 10.1177/026921559000400304. [DOI] [Google Scholar]
- 42.Koes BW, Bouter LM, Mameren H, Essers AH, Verstegen GM, Hofhuizen DM, Houben JP, Knipschild PG. The effectiveness of manual therapy, physiotherapy, and treatment by the general practitioner for nonspecific back and neck complaints. A randomized clinical trial. Spine. 1992;17:28–35. doi: 10.1097/00007632-199201000-00005. [DOI] [PubMed] [Google Scholar]
- 43.Koes BW, Bouter LM, Mameren H, Essers AH, Verstegen GM, Hofhuizen DM, Houben JP, Knipschild PG. Randomised clinical trial of manipulative therapy and physiotherapy for persistent back and neck complaints: results of one year follow up. BMJ. 1992;304:601–605. doi: 10.1136/bmj.304.6827.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maitland G. Vertebral manipulation. Oxford: Butterworth & Heinemann; 2001. [Google Scholar]
- 45.Maitland G, Hengeveld E, Banks K. Maintland’s vertebral manipulation. Oxford: Butterworth-Heinemann; 2000. [Google Scholar]
- 46.Orthopaedic manual physical therapy management of the cervical-thoracic spine and ribcage. San Antonio: Manipulations Inc.; 2000. [Google Scholar]
- 47.McKenzie R. Cervical and thoracic spine: mechanical diagnosis and therapy. Minneapolis: Orthopaedic Physical Therapy Products; 1990. [Google Scholar]
- 48.Moeti P, Marchetti G. Clinical outcome from mechanical intermittent cervical traction for the treatment of cervical radiculopathy: a case series. J Orthop Sports Phys Ther. 2001;31:207–213. doi: 10.2519/jospt.2001.31.4.207. [DOI] [PubMed] [Google Scholar]
- 49.Palmer KT, Walker-Bone K, Griffin MJ, Syddall H, Pannett B, Coggon D, Cooper C. Prevalence and occupational associations of neck pain in the British population. Scand J Work Environ Health. 2001;27:49–56. doi: 10.5271/sjweh.586. [DOI] [PubMed] [Google Scholar]
- 50.Peake N, Harte A. The effectiveness of cervical traction. Phys Ther Rev. 2005;10:217–229. doi: 10.1179/108331905X68547. [DOI] [Google Scholar]
- 51.Saal JS, Saal JA, Yurth EF. Nonoperative management of herniated cervical intervertebral disc with radiculopathy. Spine. 1996;21:1877–1883. doi: 10.1097/00007632-199608150-00008. [DOI] [PubMed] [Google Scholar]
- 52.Sarig-Bahat H. Evidence for exercise therapy in mechanical neck disorders. Man Ther. 2003;8:10–20. doi: 10.1054/math.2002.0480. [DOI] [PubMed] [Google Scholar]
- 53.Silverman JL, Rodriquez AA, Agre JC. Quantitative cervical flexor strength in healthy subjects and in subjects with mechanical neck pain. Arch Phys Med Rehabil. 1991;72:679–681. [PubMed] [Google Scholar]
- 54.Spurling RGSW. Lateral rupture of the cervical intervertebral discs: a common cause of shoulder and arm pain. Surg Gynecol Obstet. 1944;78:350–358. [Google Scholar]
- 55.Heijden GJ, Beurskens AJ, Koes BW, Assendelft WJ, Vet HC, Bouter LM. The efficacy of traction for back and neck pain: a systematic, blinded review of randomized clinical trial methods. Phys Ther. 1995;75:93–104. doi: 10.1093/ptj/75.2.93. [DOI] [PubMed] [Google Scholar]
- 56.Vernon H, Mior S. The neck disability index: a study of reliability and validity. J Manip Physiol Ther. 1991;14:409–415. [PubMed] [Google Scholar]
- 57.Viikari-Juntura E. Interexaminer reliability of observations in physical examinations of the neck. Phys Ther. 1987;67:1526–1532. doi: 10.1093/ptj/67.10.1526. [DOI] [PubMed] [Google Scholar]
- 58.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A fear-avoidance beliefs questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 59.Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine. 2003;28:52–62. doi: 10.1097/00007632-200301010-00014. [DOI] [PubMed] [Google Scholar]
- 60.Wainner RS, Gill H. Diagnosis and nonoperative management of cervical radiculopathy. J Orthop Sports Phys Ther. 2000;30:728–744. doi: 10.2519/jospt.2000.30.12.728. [DOI] [PubMed] [Google Scholar]
- 61.Werneke M, Hart DL, Cook D. A descriptive study of the centralization phenomenon. A prospective analysis. Spine. 1999;24:676–683. doi: 10.1097/00007632-199904010-00012. [DOI] [PubMed] [Google Scholar]
- 62.Ylinen J, Hakkinen A, Nykanen M, Kautiainen H, Takala EP. Neck muscle training in the treatment of chronic neck pain: a three-year follow-up study. Eura Medicophys. 2007;43:161–169. [PubMed] [Google Scholar]
- 63.Ylinen J, Takala EP, Nykanen M, Hakkinen A, Malkia E, Pohjolainen T, Karppi SL, Kautiainen H, Airaksinen O. Active neck muscle training in the treatment of chronic neck pain in women: a randomized controlled trial. JAMA. 2003;289:2509–2516. doi: 10.1001/jama.289.19.2509. [DOI] [PubMed] [Google Scholar]
- 64.Zylbergold RS, Piper MC. Cervical spine disorders. A comparison of three types of traction. Spine. 1985;10:867–871. doi: 10.1097/00007632-198512000-00001. [DOI] [PubMed] [Google Scholar]