Abstract
This study assessed the ideal district of lateral radiograph in evaluation of transarticular screw placement in the lower cervical spine. To assess the ideal zone of lateral radiographs in determining the safe or hazardous locations of the screw tips during transarticular screw implantation in the lower cervical spine. Transarticular screw in the lower cervical spine had been used as an alternative technique to achieve posterior cervical spine stability. Injury to the spinal nerves caused by transarticular screws which are too long must be identified quickly to minimize the neurologic complication. No previous radiological study regarding evaluation of the transarticular screw placement using lateral radiographs has been reported. Twelve cervical spines were removed from embalmed cadavers. Four transarticular screw placements with Dalcanto’s technique under direct visualization, including placement of the screw tip staying the ventral cortex, 2, 4 and 6 mm over-penetration of the ventral cortex, were performed on each specimen. Following each placement, a lateral radiograph was taken. Each vertebral body was divided vertically into four equal zones, and another equal zone posterior to the posterior border of the vertebral body was defined as Zone pre-1. The numbers of screw tips seen in each zone were quantified for each placement. Partitions of χ2 method was used to evaluate the ideal zone on lateral radiograph for transarticular screw insertion. At C34 and C45, no significant difference was found between Zone pre-1 and Zone 1 (χ2 = 0.18, P > 0.50), while there was significant difference between Zones 1 and 2 (χ2 = 73.6, P < 0.005), as well as Zones 2 and 3 (χ2 = 13.2, P < 0.005). At C56 and C67, No significant difference was found between Zones 2 and 3 (χ2 = 0.25, P > 0.50), while there was significant difference between Zone pre-1 and Zone 1 (χ2 = 66.2, P < 0.005), as well as Zones 1 and 2 (χ2 = 10.5, P < 0.005). Ideal screw tip positions on lateral radiograph for transarticular screw by Dalcanto’s technique should be in Zone 1 at C34 and C45, in Zone pre-1 at C56 and C67. If the screw tip was in Zones 3 and 4, the safe rate will be decreased significantly and it might be too deep and be dangerous.
Keywords: Lower cervical spine, Transarticular screw placement, Cervical radiograph, Nerve root injury
Introduction
Transarticular screw in the lower cervical spine had been used as an alternative technique to achieve posterior cervical spine stability [3, 8]. As other techniques as lateral mass screw placement, there are high potential risk of injuring the adjacent neurovascular structures if the transarticular screws were too long. It must be identified quickly to minimize the neurologic complication. Although there were many studies on transarticular screw placement in the lower cervical spine, no previous radiological study regarding evaluation of the transarticular screw placement using lateral radiographs has been reported [3, 7, 8].
The most common concerns associated with transarticular screw placement is the damaging of the cervical spinal nerve caused by a too long or misplaced screw because the spinal nerve lies directly in the front of the lateral mass. Proper and prompt diagnosis of such placement may avoid a major complication to the patient. Usually, lateral radiographs or fluoroscopy are the most commonly used modality in evaluation of the screw positions during surgery. The purpose of this study was to assess the value of lateral radiographs in determining the safe or hazardous locations of the screw tips used in the transarticular screw insertion.
Materials and methods
Materials
Twelve cervical spines (six male, six female with an age range of 60–75 years) from C1 to T1 were harvested from embalmed cadavers in the Anatomy Department of Soochow University (China). The specimens were further stripped of all soft tissue on the posterior and lateral surfaces.
Placements of transarticular screws
Four transarticular screws were used at C34, C45, C56, and C67 per side on each specimen (one side after another). The screws trajectories were prepared by drilling according to the technique of Dalcanto’s (started 2 mm caudal to the midpoint of lateral mass and traveled 40° caudal and 20° lateral) [3]. AP and lateral fluoroscopy was used during drilling to prevent the trajectories being too steep or too flat. All screws were placed using fluoroscopic guidance to ensure proper placement. Once the screw paths were properly prepared, the specimen was fixed in a vice-like device and placed with no rotation. Under direct visualization, four screw placements related to depth were subsequently performed on each specimen, one screw which was inserted deeper and deeper. For the first screw placement, the tip of the screws did not protrude past the most ventral cortex of the lateral mass. The second, third and fourth screw placements were then carried out by advancing the screws so that the tips were situated 2.0, 4.0 and 6.0 mm anterior to the most ventral cortex of the lateral mass, respectively. Sliding caliper was used on the specimens by one radiologist to ensure the length of screw tips before the most ventral cortex.
Radiographs preparation
Following each placement, a standard lateral radiograph was taken while the specimen was fixed in the stabilizing device in order to decrease position distortion. Philips X-ray radiograph machine and AGFA-CR digital processor was used by another radiologist to get these photographs, the X-ray tube focus on the central of C5 with one meter of focus film distance.
Districts classification of lateral radiograph
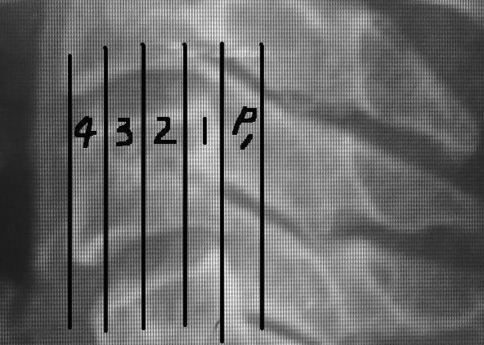
The positions of the screw tips on lateral radiographs were categorized with respect to the vertebral body at the level the screw protruded. Each vertebral body on lateral radiographs was divided vertically into four equal zones with Zone 1 being most posterior, and another equal zone posterior to the posterior border of the vertebral body was defined as Zone pre-1, the width was a quarter of which of the vertebral body (Fig. 1).
Fig. 1.
Illustration of districts classification of the vertebral body on the lateral view
Statistical analysis
The numbers of screw tips seen in each zone were quantified for each placement. The data were collected by two radiologists, respectively. And the average values were adopted as the real values for statistics (Figs. 2, 3, 4, 5). Groups 0 and 2 mm were added as “safe group”, 4 and 6 mm as “danger group”. The numbers of transarticular screw tips were quantified and documented due to the upper and the lower part of the lower cervical spine, respectively. The upper part of the lower cervical spine included C34 and C45, the lower part for C56 and C67. The data of “safe group” and “danger group” screws were recorded in varies districts at each part, respectively. Partitions of χ2 methods were performed comparing the data between varies districts. P < 0.007 indicated a significant difference.
Fig. 2.
Screws placed without penetrating the ventral cortex (0 mm). Lateral radiograph showing the screw tip positions in Zone 1 at C34, Pre-Zone 1 at C56
Fig. 3.
Screws placed with 2 mm over-penetrating the ventral cortex (2 mm). Lateral radiograph showing the screw tip positions in Zone 1 at C34, Zone 1 at C56
Fig. 4.
Screws placed with 4 mm over-penetrating the ventral cortex (4 mm). Lateral radiograph showing the screw tip positions in Zone 2 at C34, Zone 1 at C56
Fig. 5.
Screws placed with 6 mm over-penetrating the ventral cortex (6 mm). Lateral radiograph showing the screw tip positions in Zone 3 at C34, Zone 2 at C56
Results
Statistics about C34 and C45
The numbers of the screw tips on lateral radiographic projection for C34 and C45 are shown in Table 1. No significant difference was found between Zone pre-1 and Zone 1 (χ2 = 0.18, P > 0.50), while there was significant difference between Zones 1 and 2 (χ2 = 73.6, P < 0.005), as well as Zones 2 and 3 (χ2 = 13.2, P < 0.005).
Table 1.
The numbers of the transarticular screw tips at C34 and C45 on lateral X-ray projection
| Character districts | Deep of placement | Safe rate (%) | |||||
|---|---|---|---|---|---|---|---|
| Safe group (mm) | Danger group (mm) | ||||||
| 0 | 2 | Total | 4 | 6 | Total | ||
| Pre-1 | 6 | 0 | 6 | 0 | 0 | 0 | 100 |
| 1 | 42 | 26 | 68 | 2 | 0 | 2 | 97.1 |
| 2 | 0 | 22 | 22 | 36 | 20 | 56 | 28.2 |
| 3 | 0 | 0 | 0 | 10 | 28 | 38 | 0 |
| 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 48 | 48 | 96 | 48 | 48 | 96 | – |
No significant difference was found between Zone pre-1 and Zone 1 (P > 0.50), while there was significant difference between Zones 1 and 2 (P < 0.005), as well as Zones 2 and 3 (P < 0.005)
Statistics about C56 and C67
The numbers of the screw tips for C56 and C67 are shown in Table 2. No significant difference was found between Zones 2 and 3 (χ2 = 0.25, P > 0.50), while there was significant difference between Zone pre-1 and Zone 1 (χ2 = 66.2, P < 0.005), as well as Zones 1 and 2 (χ2 = 10.5, P < 0.005).
Table 2.
The numbers of the transarticular screw tips at C56 and C67 on lateral X-ray projection
| Character districts | Deep of placement | Safe rate (%) | |||||
|---|---|---|---|---|---|---|---|
| Safe group (mm) | Danger group (mm) | ||||||
| 0 | 2 | Total | 4 | 6 | Total | ||
| Pre-1 | 36 | 26 | 62 | 0 | 0 | 0 | 100 |
| 1 | 12 | 20 | 32 | 40 | 20 | 60 | 34.8 |
| 2 | 0 | 2 | 2 | 8 | 24 | 32 | 5.9 |
| 3 | 0 | 0 | 0 | 0 | 4 | 4 | 0 |
| 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 48 | 48 | 96 | 48 | 48 | 96 | – |
No significant difference was found between Zone 2 and Zone 3 (P > 0.50), while there was significant difference between Zone pre-1 and Zone 1 (P < 0.005), as well as Zones 1 and 2(P < 0.005)
Discussion
Theoretically, complications associated with transarticular screw placement in the lower cervical spine may include violation of the spinal cord, vertebral artery, spinal nerve by either a misplaced or over-penetrated screw. There would be no risks of injuring the spinal cord and vertebral artery as long as screws are directed laterally to the parasagittal plane [3, 4]. Also, no incidence of spinal cord or vertebral artery injury has been reported in clinical practice of transarticular screw insertion [8]. Although few articles based on the neural complications of transarticular screw insertion, it seems that, even in experienced hands, injury to the spinal nerve was the main complication of the procedure when the screw was inserted too deep. In regard to lateral mass screw placement, several recommendations have been made to avoid or minimize neural complications, including a thorough knowledge of morphology of the lateral mass and surrounding anatomy, careful evaluation of preoperative CT scans on the individual basis, correct identification of the screw entrance point, placement of drill bits or screws in the lateral orientation, selection of screws in proper length by using an adjustable drill guide and measuring drill length, and using oblique projection radiograph to check the position of the screw tip in relation to the intervertebral foramen [1, 5, 6, 9]. Unfortunately, there remains a great chance of violating the spinal nerve during the transarticular screw insertion, even with screw placement visualized under fluoroscopy [6]. Fluoroscopy is a commonly used radiological modality during surgery. The lateral view provided by fluoroscopy is perhaps the most convenient projection to direct each screw insertion or check the screw position after screw insertion. This projection will show the screw trajectory in the sagittal plane. However, its value in determining the screw length has not been assessed. If we can detect an over-penetrated screw using lateral projection radiographs, the chance of spinal nerve injury or postoperative radiculopathy may be minimized, and a second surgery for revision of the screw placement may be avoided.
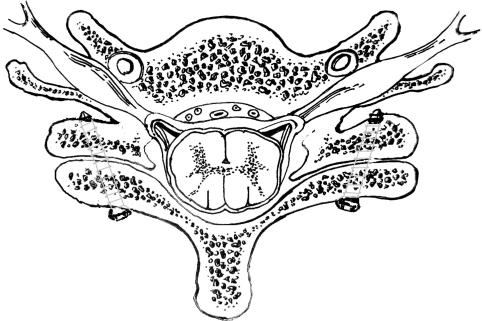
In the present study, we thought that the posterior border of the vertebral body is a well visible landmark on lateral radiograph. It is possible to predict whether a screw is placed too deeply if one can determine the radiographic relationships of various screw placements to the posterior border of the vertebral body. Takayasu et al. [8] considered that one pitch (about 2 mm) penetrating beyond the most ventral cortex would be safe during implantation of transarticular screws. We also found the out point of the transarticular screw by technique of Dalcanto’s in current study was between the posterior tubercle of the transverse process and the corresponding anterior cortex of the lateral mass. There was no involvement of anterior and posterior branches of cervical nerve root during transarticular screw insertion in our study when the screw tips penetrating within 2 mm. However, it was dangerous when the screw tip beyond more than 4 mm, as it would penetrate the posterior tubercle of the transverse process, enter the inferior part of neuro-foramen and involve the anterior branch of cervical nerve root (Figs. 6, 7). And clinically, it will be usually defined as safe and suitable if the screw tips over the contrary cortex within 2 mm. So 0 and 2 mm groups were assumed as “safe group”, while 4 and 6 mm as “danger group” in our study.
Fig. 6.
The out point of the transarticular screw is between the posterior tubercle of the transverse process and the corresponding anterior cortex of the lateral mass, where anterior and posterior branches of cervical nerve root would not be involved
Fig. 7.
Axial view of the transarticular screws. The tip of transarticular screw would penetrate the posterior tubercle of the transverse process, enter the inferior part of neuro-foramen and involve the anterior branch of cervical nerve root, if it were implanted too deep
The difference of the upper and the lower part of the lower cervical spine had been reported [2]. From the lateral radiographs of the lower cervical spine, the difference can be observed between the upper part (C3–C5) and the lower part (C5–C7). It seems that the most ventral cortex of the upper facets (C34 and C45) of the lower cervical spine was more anterior than that of the lower facets (C56 and C67) on the lateral radiographs. This is the reason why we documented the data according to the upper and lower part of the lower cervical spine.
Evaluation of lateral radiographs taken on the screw placements at C34 and C45 revealed that there were 97.1% of screw tips in “safe group” in Zone 1, while none in Zones 3 and 4. And there were 97.9% of screw tip in “danger group” in Zones 2 and 3. This observation suggested that the screw length is proper and safe if the tip of a screw placed at C34 and C45 is located in Zone 1. In contrast, the screw is most likely over-penetrated if found in Zones 3 and 4. However, it was difficult to judge if a screw tip located in Zone 2 was too long because 22 (45.8%) of 48 screw tips seen in Zone 2 were over-penetrating the ventral cortex of the lateral mass by only 2 mm, while 56 (58.3%) of 96 screw tips over-penetrating by 4–6 mm. Although the value of percentage of the safe rate was higher in Zone pre-1 (100%) than Zone 1(97.1%), the difference was not significant according to our statistic analysis. According to our study, there were only six screw tips (12.5%) in 0 mm group, and none in other groups in Zone pre-1. It means if one screw tip was found in Zone pre-1, there might be only small possibility that the screw tip reached the most ventral cortex, while more did not even get the ventral cortex. Thus Zone 1 should be ideal district for proper transarticular screws at C34 and C45.
At C56 and C67, there were 64.6% screw tips in “safe group” in Zone pre-1, while none in Zone 3 and Zone 4. There were 95.8% screw tips in “danger group” in Zones 1 and 2. The safe rate was 100% in Zone pre-1, 34.8% in Zone 1, 5.9% in Zone 2, 0% in Zones 3 and 4. There was significant difference between Zone pre-1 and Zone 1. This observation suggested that the screw length is proper and safe if the tip of a screw placed at C56 and C67 is located in Zone pre-1. In contrast, the screw is most likely over-penetrated if found in Zone 2. It might be too deep if one screw tip was found in Zones 3 and 4. However, it was difficult to judge if a screw tip located in Zone 1 was too long because 20 (41.7%) of 48 screw tips seen in Zone 1 were over-penetrating the ventral cortex of the lateral mass by only 2 mm, while 60 (62.5%) of 96 screw tips over-penetrating by 4–6 mm.
Usually, fluoroscopic images are used at the time of surgery to assess screw position. As we all known, the posterior cortex of vertebral body is clearer than the anterior edge of facet in fluoroscopic views. And the districts of cervical vertebrae according to the posterior edge of the vertebral body can decrease dramatically the effect of the magnification factors. The methods used in this study were simple and reproducible. The conclusion from current study provided important references for the surgery of implantation of transarticular screw in the lower cervical spine in which fluoroscopy will be used to evaluate the depth of screw, although the lateral radiographs have some difference with fluoroscopic views.
Finally, it should be pointed out that this study was done with 0 degree of rotation and that these results are only applicable when the X-ray beam passes symmetrically through both lateral masses (standard lateral views). The rotation of the spine would have affect on the relationship of a penetrated screw and the posterior cortex of the vertebral body. Additionally, it is not only the length but also the direction of the transarticular screw will determinate the potential risk of neural injury. Obviously, a screw inserted straight forward puts the neurovascular structures much more in danger than a screw inserted with 20° divergence which was introduced in current study. It should be emphasized that the different pa angle cannot be detected only on the lateral radiograph. Thus, the safety zones in our study should be limited only in correct usage of Dalcanto’s technique, in which the transarticular screws be implanted with 20° divergence. If in the post-operative period there is a suspicion of a radicular problem then a lateral radiograph used with an apparently properly placed screw may be insufficient and CT must be used to see the real reason. Thus, further studies should be necessary for theses points.
In summary, ideal screw tip positions on lateral radiograph for transarticular screw by Dalcanto’s technique should be in Zone 1 at C34 and C45, in Zone pre-1 at C56 and C67. If the screw tip was in Zone 3 or 4, the safe rate will be decreased significantly and it might be too deep and be dangerous.
Acknowledgments
The authors deeply thank Chao Chen from Department of exhibition service of Ningbo Museum of Art of China for his help to draw Figs. 6 and 7.
References
- 1.An HS, Gordin R, Renner K. Anatomic considerations for plate-screw fixation of the cervical spine. Spine. 1991;16:S548–S551. doi: 10.1097/00007632-199110001-00019. [DOI] [PubMed] [Google Scholar]
- 2.Barrey C, Mertens P, Jund J et al (2005) Quantitative anatomic evaluation of cervical lateral mass fixation with a comparison of the Roy-Camille and the Magerl screw techniques. Spine 6:E140–E147 [DOI] [PubMed]
- 3.Dalcanto RA, Lieberman I, Inceoglu S, et al. Biomechanical comparison of transarticular facet screws to lateral mass plates in two-level instrumentations of the cervical spine. Spine. 2005;8:897–902. doi: 10.1097/01.brs.0000158937.64577.25. [DOI] [PubMed] [Google Scholar]
- 4.Ebraheim NA, Xu R, Yeasting RA. The location of the vertebral artery foramen and its relationship to posterior lateral mass screw fixation. Spine. 1996;21:1291–1295. doi: 10.1097/00007632-199606010-00002. [DOI] [PubMed] [Google Scholar]
- 5.Graham AW, Swank ML, Kinard RE, et al. Posterior cervical arthrodesis and stabilization with a lateral mass plate: Clinical and computed tomographic evaluation of lateral mass screw placement and associated complications. Spine. 1996;21:323–329. doi: 10.1097/00007632-199602010-00014. [DOI] [PubMed] [Google Scholar]
- 6.Heller JG, Silcox H, Sutterlin CE. Complications of posterior cervical plating. Spine. 1995;20:2442–2448. doi: 10.1097/00007632-199511001-00013. [DOI] [PubMed] [Google Scholar]
- 7.Klekamp JW, Ugbo JL, Heller JG, et al. Cervical transfacet versus lateral mass screws: a biomechanical comparison. J Spinal Disord. 2000;13:515–518. doi: 10.1097/00002517-200012000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Takayasu M, Hara M, Yamauchi K, et al. Transarticular screw fixation in the middle and lower cervical spine Technical note. J Neurosurg. 2003;99:132–136. doi: 10.3171/spi.2003.99.1.0132. [DOI] [PubMed] [Google Scholar]
- 9.Xu R, Robke J, Ebraheim NA, et al. Evaluation of cervical posterior lateral mass screw placement by oblique radiographs. Spine. 1996;21:696–701. doi: 10.1097/00007632-199603150-00007. [DOI] [PubMed] [Google Scholar]