Abstract
Low back pain (LBP) poses a significant problem to society. Although initial conservative therapy may be beneficial, persisting chronic LBP still frequently leads to expensive invasive intervention. A novel non-invasive therapy that focuses on discogenic LBP is Intervertebral Differential Dynamics Therapy® (IDD Therapy, North American Medical Corp. Reg U.S.). IDD Therapy consists of intermittent traction sessions in the Accu-SPINA device (Steadfast Corporation Ltd, Essex, UK), an FDA approved, class II medical device. The intervertebral disc and facet joints are unloaded through axial distraction, positioning and relaxation cycles. The purpose of this study is to investigate the effect of IDD Therapy when added to a standard graded activity program for chronic LBP patients. In a single blind, single centre, randomized controlled trial; 60 consecutive patients were assigned to either the SHAM or the IDD Therapy. All subjects received the standard conservative therapeutic care (graded activity) and 20 sessions in the Accu-SPINA device. The traction weight in the IDD Therapy was systematically increased until 50% of a person’s body weight plus 4.45 kg (10 lb) was reached. The SHAM group received a non-therapeutic traction weight of 4.45 kg in all sessions. The main outcome was assessed using a 100-mm visual analogue scale (VAS) for LBP. Secondary outcomes were VAS scores for leg pain, Oswestry Disability Index (ODI), Short-Form 36 (SF-36). All parameters were measured before and 2, 6 and 14 weeks after start of the treatment. Fear of (re)injury due to movement or activities (Tampa Scale for Kinesiophobia), coping strategies (Utrecht Coping List) and use of pain medication were recorded before and at 14 weeks. A repeated measures analysis was performed. The two groups were comparable at baseline in terms of demographic, clinical and psychological characteristics, indicating that the random allocation had succeeded. VAS low back pain improved significantly from 61 (±25) to 32 (±27) with the IDD protocol and 53 (±26) to 36 (±27) in the SHAM protocol. Moreover, leg pain, ODI and SF-36 scores improved significantly but in both groups. The use of pain medication decreased significantly, whereas scores for kinesiophobia and coping remained at the same non-pathological level. None of the parameters showed a difference between both protocols. Both treatment regimes had a significant beneficial effect on LBP, leg pain, functional status and quality of life after 14 weeks. The added axial, intermittent, mechanical traction of IDD Therapy to a standard graded activity program has been shown not to be effective.
Keywords: Low back pain, Traction, IDD therapy®, Non-invasive therapy, Randomized clinical trial
Introduction
Low back pain (LBP) poses a significant problem to society. In the Netherlands, the 1-year-period prevalence in the general population was 44% in 2003 [13]. Almost one-fourth of the employed population with LBP reported sickness leave in the past year [13]. LBP is associated with persistent or recurrent disability and absence from work, resulting in high costs for society [1, 9].
Low back pain is usually a benign condition that tends to resolve quickly. However, LBP can also be caused by pathological conditions such as lumbar disc degeneration [3]. Since disc degeneration might be caused by several conditions, its treatment is still a great challenge for therapists. Conservative therapies may be beneficial, but a variety of non-surgical treatment modalities also exists [18], for example graded activity. This is a physical exercise program based on operant-conditioning behavioural principles and it is proven to be effective in reducing the number of days of absence from work because of LBP [17]. Nevertheless, persistent chronic LBP still frequently leads to expensive surgical intervention. Due to the fact that there is still no consensus of the best therapy for LBP, any non-surgical therapy deserves investigation.
Non-invasive and probably cost-effective therapies that have received interest recently are traction-based therapies, as can be seen in the special issue of The Spine Journal [7]. However, reports of high-quality RCTs to evaluate traction therapy are scarce [5, 7]. For example, reported studies lacked a randomized comparison group [2, 19], had a retrospective design [10, 11, 15, 16], sample sizes were too small [6, 10, 11], heterogeneous patient groups were studied [3, 6, 19] or the authors were commercially related to the evaluated therapy [11, 16]. Moreover, within this particular field there is still controversy since various different traction techniques and corresponding protocols exist. In a total of ten RCTs a categorization of traction therapies was made based on temporal (sustained or intermittent) and force (focused or dispersed) variables [7], but the most effective or most appropriate intervention could not be determined [7]. A larger systematic review by Clarke et al. [5] (24 RCTs) concluded that for patients with LBP, who may or may not have sciatica, traction as a single treatment is no more effective than placebo, sham, no treatment or other treatments. For patients who do have sciatica, the evidence is inconsistent. A review of the efficacy of spinal decompression through motorized traction could also not change this conclusion [9]. In consequence, the studied literature provides more evidence against rather than for the use of traction therapy as the sole treatment for LBP.
A new non-invasive traction therapy that focuses on patients with discogenic LBP is Intervertebral Differential Dynamics Therapy® (IDD Therapy, North American Medical Corp. Reg U.S.). IDD Therapy consists of 20 traction sessions of approximately 25 min during 6 weeks in the Accu-SPINA device (Steadfast Corporation Ltd, Essex, UK). This device intends to unload the intervertebral disc and facet joint through axial distraction, positioning and relaxation cycles. According to the manufacturer of the Accu-SPINA, the hypothesis of the working mechanism is that a negative intradiscal pressure during distraction is created, which may increase nutrient flow into the disc. This cyclic mechanism of distraction could promote self healing in damaged tissues.
A small retrospective pilot study (n = 33) showed that a treatment of 20 sessions of distraction of the lumbar spine in the Accu-SPINA device, gave pain relief 1 year after the treatment completion to 76% of the patients with a herniated disc [16]. However, that study had several serious methodological flaws making the conclusions untrustworthy. In view of the potential importance of this new non-invasive therapy, we re-investigated this traction-system in a single blind randomized controlled trial. The purpose of the present study is to investigate the additional effect of IDD Therapy to a standard graded activity program for chronic LBP patients with symptomatic lumbar disc degeneration or bulging disc with no radicular pain, and no prior surgical treatment with dynamic stabilization, fusion or disc replacement.
Materials and methods
Study design
The efficacy of the IDD Therapy on the visual analogue scale (VAS) score of LBP was investigated in chronic LBP patients with symptomatic lumbar disc degeneration or bulging disc with no radicular pain, and no prior surgical treatment with dynamic stabilization, fusion or disc replacement. These patients did not suffer from medical conditions that required surgical spine interventions. The traction protocol whether IDD or SHAM was added to a standard graded activity program. Patients were recruited at the orthopaedic department of the Sint Maartenskliniek, Nijmegen. The study protocol was approved by the investigational review board of the hospital and the Medical Ethical Review Board of the region Arnhem–Nijmegen.
Subjects
An orthopaedic surgeon screened the patient’s file and existing X-rays to check if the patient was eligible for participation. The following inclusion criteria were used: (1) LBP for more than 3 months; (2) bulging disc; (3) lumbar degenerative disc disease; (4) place of residence within 25 km from the hospital. Exclusion criteria were (1) previous surgical treatment with dynamic stabilization, fusion or disc replacement; (2) radicular leg pain; (3) malignancy; (4) pregnancy; (5) osteoporosis. All participants provided written informed consent.
Randomization
Participants were blinded to the traction protocol to be given and assigned either to the IDD Therapy or SHAM Therapy. Randomization occurred through computer-generated random block lists. Numbered sealed envelopes were prepared and given to the physiotherapist. After the inclusion of a patient into the trial, the physiotherapist opened an envelope with a treatment code and was therefore not blinded for the assigned treatment. The allocated traction protocol was followed, and the envelope was returned to the trial coordinator with the patient’s study number. The trial coordinator had the key for the treatment being given. The traction therapy was given by the same physiotherapist during the patient’s entire course of treatments. Follow-up evaluation was performed by an independent physiotherapist and a research nurse, both of whom were blinded to the treatment. The patient was not informed about the intervention received until after the 14 weeks follow-up assessment, which was the primary endpoint of the study.
Protocol
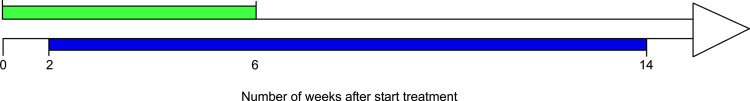
Both the IDD and the SHAM group started the treatment protocol with 20 traction sessions in the same Accu-SPINA device during 6 weeks, according to the protocol of the IDD Therapy. The standard graded activity program was added 2 weeks after start of the traction sessions in both groups. This program consisted of a 1-h training for 2 days per week during a total of 12 weeks (Fig. 1). Traction therapy was given separately of the graded activity training and always on a different day.
Fig. 1.
Time line of the treatment protocol. The treatment started with the traction therapy whether the IDD or the SHAM protocol. This consisted of 20 half-hour sessions during the first 6 weeks of the treatment (green line). Two weeks after initiation started the standard therapeutic care (graded activity) and lasted 12 weeks (blue line). The graded activity program consisted of 1 h of training for 2 days per week
A traction session started with the participant being fitted in a pelvic and chest harness and placed in a supine position. The chest harness was attached and tightened to the table. Knees were flexed over a cushion and the pelvic harness was fixed to the tower that could be raised or lowered to give a focused angle optimal to the disc space being treated. The traction to be given in the IDD Therapy, was calculated as follows. On the first and second day of treatment, one-half of a person’s body weight minus 4.54 kg (10 lb) was given. Thereafter, the traction weight was systematically increased with 2.27 kg (5 lb) until 50% body weight plus 4.54 kg was reached. The SHAM group received a non-therapeutic traction weight of 4.54 kg (less than 10% body weight) in all sessions to assure a sensation similar to the intervention. The actual traction sessions were set at intervals of 60 s of distraction followed by 30 s of partial relaxation (intermittent traction). A total treatment session included 17 repetitions and lasted 25–30 min. Subjects were given five sessions per week for the first 2 weeks, three sessions per week for weeks 3–4 and the last 2 weeks two sessions per week. In addition to the traction, the Accu-SPINA device accomplished a massage, heat, blue relaxing light and music during the treatment sessions in both groups.
Measurements
At the baseline assessment subjects provided socio-demographic variables and historical information on prior experience, previous spinal surgery and the use of (pain) medication. The primary outcome was LBP assessed using a 100-mm VAS. Unbearable pain intensity was recorded as 100, and 0 indicated no pain at all. Secondary outcomes were VAS scores for leg pain, Oswestry Disability Index (ODI), and Short-Form 36 (SF-36). The ODI measures the effect of LBP on daily function in ten domains. The SF-36 assesses general quality of life in nine subscales. All these parameters were measured before treatment and after 2, 6 and 14 weeks following the start of the treatment.
Since chronic LBP was associated with cognitive and emotional factors [14] a psychological examination was completed at baseline. In this examination participants were interviewed and were asked to complete several questionnaires. The Tampa Scale for Kinesiophobia was used to asses fear of (re)injury due to movement or activities. Coping strategies were recorded with the Utrecht Coping List (UCL). These questionnaires were also measured at the 14 weeks follow-up assessment.
A change in use of pain medication was reported if a substantially decrease or increase, defined as a 50% change or greater in the amount of pain medication, was observed after 14 weeks compared to the used medication before treatment.
Power calculation
To detect a clinically relevant difference of 20 points (variability 29 points) on the VAS scale to be reached after 14 weeks for the IDD and SHAM protocol respectively, a sample size of 60 patients, 30 in each group is needed. This is a difference of 20% of the maximum score and can be detected with α = 0.05 and β = 0.20 (power = 0.80). Ultimately, 94 patients were assessed for eligibility, of which 13 patients refused to participate, 3 reasons were unknown and we reported 3 non-responders. Fifteen patients could not participate because of other reasons not related to the study (work or time-related).
Analysis
Baseline status of the groups was compared using two-tailed independent t tests and Chi-square tests or appropriate non-parametric alternatives. Analyses were performed carrying out the ‘intention-to-treat’ principle: all patients were included in the analysis of the group to which they had been randomized, regardless of any subsequent events. Between group differences on the outcome measures were examined using a repeated measures analysis. The within-subjects factor was ‘time’ with four levels. Traction ‘protocol’ whether IDD or SHAM was used as the between-subjects factor. In order to determine the effect of the traction protocol on the VAS score of LBP properly, the baseline score of VAS LBP was categorized and then used as a between-subjects factor in the analysis. The three subgroups were defined as follows: baseline VAS score 0–33, 34–66 and >66. The main interactions of interest were time × protocol, time × VAS_categorized and time × protocol × VAS_categorized.
A repeated measures analysis was also performed for VAS leg pain and the total scores of SF-36 and ODI, with the same factors ‘time’ and ‘protocol’. A paired samples t test was used to compare the UCL and Tampa scores at 0 and 14 weeks follow-up. The change in use of pain medication was calculated with a Wilcoxon signed-rank test. In all analyses the level of significance was set at P < 0.05. Data-analysis was performed using the statistical package of SPSS 12.0.1 for Windows.
Results
Patient characteristics
Sixty subjects were recruited, 31 randomized to the IDD and 29 to the SHAM protocol. All patients were known with lumbar back pain for at least 1 year and underwent one or more non-surgical treatment modalities before starting with the investigated treatment. Everyone had had physiotherapy and 23 patients in the IDD and 24 patients in the SHAM group also underwent other non-surgical therapies, such as exercise therapy (McKenzie or Cesar therapy), chiropractics or epidural/steroid injections.
Ultimately, 56 patients (93%) completed the 14-week follow-up evaluation. Three patients in the SHAM group failed to finish the graded activity program, two because of physical problems and one because of lost of motivation and heavy emotional cost. One patient in the IDD group could not finish the graded activity program due to logistical problems. Nevertheless, they all finished the traction sessions and a part of the graded activity program (complete data available until 6 weeks follow-up moment).
General socio-demographic characteristics and mean values (and standard deviations) for the scores of the VAS, ODI, SF-36, Tampa and UCL of both groups are given in Table 1. Evaluation of these variables showed no between-group differences at baseline since all P values >0.05, implying a successful randomization.
Table 1.
Participant’s general characteristics and baseline values of outcome measures
| Variable | IDD group (n = 31) | SHAM group (n = 29) | P valuef |
|---|---|---|---|
| Age (years)a | 42 (8.6) | 46 (9.7) | 0.115 |
| Gender (m:f) | 19:12 | 14:15 | 0.311 |
| Weight (kg)a | 79 (14.6) | 81 (14.5) | 0.646 |
| Height (cm)a | 176 (11.4) | 174 (8.8) | 0.626 |
| BMI (kg/m2)a | 25.7 (4.5) | 26.5 (3.5) | 0.318 |
| Smoker (yes:no) | 12:19 | 13:16 | 0.631 |
| Alcohol (yes:no) | 18:13 | 22:7 | 0.144 |
| Use of pain medication (yes:no) | 16:15 | 14:15 | 0.796 |
| Previous surgery (yes:no)b | 2:31 | 6:29 | 0.105 |
| Moderate activity (yes:no)c | 7:31 | 5:29 | 0.605 |
| Life event in last 2 years (yes:no) | 12:19 | 13:16 | 0.631 |
| Employed (yes:no) | 27:4 | 22:7 | 0.261 |
| Heavy physical work (yes:no)d | 13:14 | 13:9 | 0.398 |
| Baseline values outcome measures | |||
| VAS low back pain | 61 (24.6) | 53 (26.4) | 0.277 |
| ODI | 36 (15.7) | 33 (16.8) | 0.460 |
| Total score SF-36 | 52 (17.1) | 53 (18.1) | 0.702 |
| VAS right leg pain | 37 (28.3) | 33 (30.2) | 0.668 |
| VAS left leg pain | 27 (25.2) | 31 (28.5) | 0.514 |
| Tampa scoree | 39 (7.4) | 38 (7.8) | 0.704 |
aValues are mean ± SD
bSurgery for Hernia Nuclei Pulposa (HNP)
cNumber of moderate activity exceeds once a week
dNumber of those who were employed
eQuestionnaire completed by 54 participants (26 of the IDD group and 28 of the SHAM group)
f P values of two-tailed independent t tests, Chi-square tests or appropriate non-parametric tests for baseline between-group differences
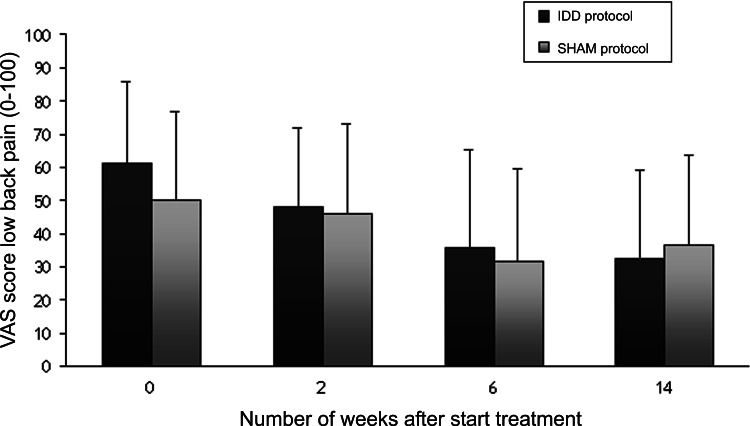
VAS score LBP
Fourteen weeks after start of the treatment the mean VAS score decreased to 32 (±26.8) in the IDD group and to 36 (±27.1) in the SHAM group, respectively (Fig. 2). This decrease was statistically significant (main effect of ‘time’, F 3,150 = 24.1, P < 0.001). However, no difference between the groups (F 1,50 = 0.156, P = 0.695) and no time × group interaction (F 3,150 = 1.34, P = 0.26) was detected. This implies that time has had more influence on the improvement in VAS score than the intervention itself. The three subgroups for the categorized VAS score (0–33, 34–66 and >67) consisted of 12, 22 and 22 patients, respectively. A significant between-subjects effect for this factor was observed (F 2,50 = 38.5, P < 0.001), possibly indicating that the categorized pre-treatment VAS score of LBP influences the VAS score after treatment. The non-significance of the interactions group × VAS_categorized and time × group × VAS_categorized indicated that this effect was similar in both groups. A contrast test of the variable ‘time’ (contrast: repeated) revealed a significant decrease in LBP between 0–2 weeks (P = 0.001) and 2–6 weeks (P < 0.001), regardless of the intervention.
Fig. 2.
Mean VAS scores (±SD) of low back pain in the IDD group and the SHAM group. The effect of time was statistically significant (P < 0.05)
In both groups some patients did not complete the graded activity program, therefore we studied a ‘worst-case’, ‘best-case’ and ‘last observation carrying forward’ scenario. The VAS score of LBP at 14 weeks was imputed with 0 (=unbearable pain = ’worst-case’) or 100 (=no pain at all = ’best-case’), or the VAS score at 6 weeks was duplicated to be imputed at 14 weeks (‘last observation carrying forward’). After completion of the imputation, similar analyses were performed. No differences between the groups were found. In the ‘worst-case’ and ‘last observation carrying forward’ scenario the interaction time × VAS_categorized became significant (P = 0.017 and 0.029, respectively). The similar results for these analyses, despite the interaction effect, compared to the primary analysis indicated that the drop-outs had not affected the validity of the results and therefore the probability of a Type II error (false negative) decreased.
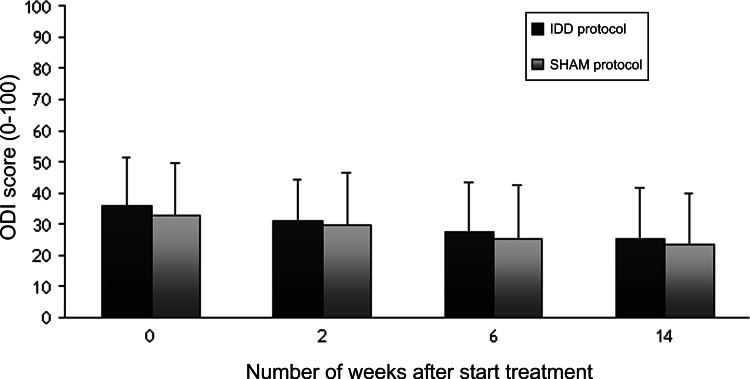
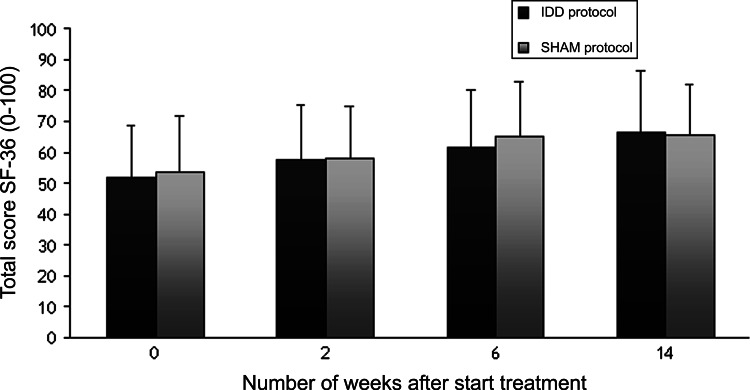
Secondary outcome measures
Scores for the ODI, SF-36 and VAS leg pain showed a significant improvement during the treatment in the IDD and the SHAM group. However, the differences between the groups were very small and not statistically significant. Functional status improved regardless of the traction protocol (main effect of ‘time’, F 3,159 = 13.2, P < 0.001), which was displayed by a decrease of the ODI score (Fig. 3). Further, the total score of the SF-36 increased significantly (main effect of ‘time’, F 3,1224 = 23.7, P < 0.001), which implied an improvement in the health-related quality of life regardless of the protocol subjected to (Fig. 4).
Fig. 3.
Functional status, as measured with the ODI, in the IDD group and the SHAM group. The effect of time was statistically significant (P < 0.05)
Fig. 4.
Health-related quality of life, as measured with the SF-36, in the IDD group and the SHAM group. Only the effect of time was statistically significant (P < 0.05), indicating an improvement after 14 weeks regardless of traction protocol
Since we could not detect a difference in the VAS score between the left and right leg, we calculated the mean VAS score for leg pain. As displayed by this score, leg pain decreased during the treatment (main effect of time F 3,156 = 10.5, P < 0.001) in the IDD group from 31 (±21.3) to 17 (±17.5) and from 29 (±26.5) to 22 (± 24.5) in the SHAM group, respectively. Furthermore, during the treatment patients in both groups were highly satisfied, as measured with a VAS score for satisfaction in which completely satisfied was recorded as 100 and not satisfied as 0. A median VAS score of at least 70 points was observed for both groups during all follow-up moments.
The coping style and level of kinesiophobia, as measured with the UCL and Tampa scale, did not show an improvement at the end of treatment. Moreover, no difference between the groups could be detected.
Nine patients in the IDD group and five patients in the SHAM group reported a change in their use of pain medication. All those patients reported a decrease, which was significant in both groups (P = 0.003 and 0.025 in the IDD and SHAM group, respectively).
Post hoc power analysis
To control the validity of our assumptions, we calculated the post hoc power of the main analysis. This analysis showed that a minimal difference of 8.6 points for the VAS score for LBP would have been detectable with this sample size (n = 60) and F value (0.156). The minimum sample size required to detect the observed difference (1.7 points on a 100-point scale, with a standard error of 4.3) was n = 1,499. However, it is questionable if the minimum detectable difference would be of any clinical significance. Moreover, since the worst-case scenario did not change the results, it may be concluded that the probability of a Type II error (a false negative) was close to zero.
Discussion
The purpose of this study was to investigate the additional effect of IDD Therapy to a standard graded activity program for LBP, in patients with symptomatic lumbar disc degeneration. IDD Therapy consisted of a traction protocol in the Accu-SPINA device, while the control group received a SHAM Therapy in the same device. Our main finding is that there was no difference between the IDD Therapy and the SHAM Therapy 14 weeks after start of the treatment neither for the primary outcome, a 100-point VAS scale for LBP, nor for the secondary outcomes, i.e. SF-36 and ODI. Nevertheless, the participants in both groups reported a significant improvement in LBP, leg pain, daily function (ODI) and general health perception (SF-36). Furthermore, the fear of (re)injury due to movement or activities, as measured with the Tampa scale, and coping strategies, as measured with the UCL, did not change after treatment. Finally, a decrease in the use of pain medication was reported in both groups.
A constant point of discussion in recent reviews [5, 7] is the low quality of the selected studies and insufficient homogeneity between trials, making a meta-analysis impossible. It was emphasized that most available studies have several methodological problems, thus potentially biased results. For example, heterogeneous patient groups were used or sample sizes were too small to detect a clinically significant difference. As a consequence, a comparison of our results with previous studies is difficult. Nevertheless, the results of the current study seem to support the conclusions of recent reviews [5, 7], in which no uniform evidence of the efficacy for traction therapy as a treatment for LBP was reported. However, it should be stressed that in this study the IDD Therapy was used as an add on therapy to the standard graded activity program. We could confirm the finding that traction appears to be a safe, non-invasive treatment since no adverse events were reported [7].
Our results were in contrast with previous methodologically flawed studies that reported on IDD Therapy [11, 15, 16]. A preliminary study reported that decompression of the lumbar spine in a proto-type of the Accu-SPINA device yielded good to excellent results and relieved pain in 86% of the patients with a pathology of a ruptured lumbar intervertebral disc and in 75% of those with facet arthrosis [15]. These percentages, however, were based on very small sample sizes of 14 and 8 patients, respectively. A retrospective pilot study, in which the authors declared to have a proprietary interest in IDD Therapy, noted an improvement in pain score of 4.46 on a 10-point scale [16]. A second low-quality retrospective study yielded success rates of 79 and 92 % in patients with lumbar back pain and surgical candidates, respectively, in which success was defined as a 50% decrease or greater in pain [11]. They also suggested that IDD Therapy not only decreased pain, but also alleviated the depression associated with pain [11]. Since depression affected reported pain prior to treatment, it is questionable whether the reported improvement was solely due to the IDD Therapy or to more or less psychological aspects of the treatment.
In contrast to the previous studies [11, 15, 16], we did not test IDD Therapy as a single treatment, but added it to a standard graded activity program. A graded activity program is aimed at changing the individual’s perception of his/her medical condition and is focused on abilities rather than the disabilities [17]. It is likely that telling participants their pain was benign and providing experiences that supported that message resulted in a reduction of the use of pain medication, as seen in our study. Previous literature concluded that graded activity was not effective in pain reduction or functional status but solely in reducing the number of days absent from work: the general principle of the program [17]. We could not confirm this finding, since we did not report the exact absence from work. Nevertheless, our results supported the finding that the addition of traction to a standard physiotherapy program did not produce significantly better results [4].
The principal strength of the presented study is that, to our knowledge, it is to date the first single blind, single centre, randomized controlled trial that investigated the efficacy of IDD Therapy in patients with lumbar disc degeneration. Another strength is that our study population was homogenous and comparable to the total population of patients with chronic LBP without radicular leg pain since the ODI, SF-36, Tampa and UCL scores did not differ from published norms for patients with chronic LBP [8, 12]. Thus, the selection bias of the orthopaedic surgeons was limited, moreover since less than 14% of the subjects refused to participate. Furthermore, each patient’s X-rays of the lumbar spine were screened to exclude patients with contraindications for traction therapy, such as osteoporosis or malignancy. Finally, we selected patients with chronic LBP (>3 months) to limit the chance of spontaneous recovery.
Our study was limited by some factors. First, blinding of the treating physiotherapists was impossible due to the character of the traction therapy. However, because an independent physiotherapist and a research nurse both of whom were blinded conducted the follow-up evaluation, information bias was avoided. Secondly, the protocol recommends 20 intermittent sessions, with a full 13 min of joint mobilization. This protocol was based solely on the experience of the manufacturer. It remains uncertain if this is the optimal protocol for traction therapy in the Accu-SPINA device, since the degree that subject positioning and temporal or force characteristics of the protocol could influence the results is not known [5, 7]. Nevertheless, the traction to be given in the IDD and SHAM protocols was substantially different (up to 50% body weight vs. less than 10% body weight) that one would expect a detectable difference in clinical outcome. Moreover, high-dose traction (30–50% of body weight) is thought to be most effective for axial traction [7]. Finally, there was a drop-out rate of approximately 7%. However, the drop-outs were equally spread between the groups and a worst-case and best-case scenario showed that these did not influence the results.
Despite the fact that no difference could be found between IDD Therapy and the SHAM therapy, added to standard graded activity, a significant decrease in LBP and leg pain and an increase in functional status and quality of life was found in both groups. These significant improvements were remarkable, and we believe some of it may be due to the standard graded activity program, but also partly due to the attention received during the 20 treatment sessions in the Accu-SPINA device. The added axial, intermittent, mechanical traction of IDD Therapy has shown not to be effective.
We emphasize the need for properly designed RCTs to evaluate specific new non-surgical therapies that are being marketed to the public. Future studies on traction therapy should focus on different patient groups and other parameters of traction, for example subject positioning and temporal or force characteristics, in order to clarify the use of traction in chronic LBP. Practitioners using such therapies should reconsider their treatment protocols, because based on this study traction has probably no place at all in the treatment of chronic LBP.
Acknowledgments
We would like to thank the Steadfast Corporation Ltd (1 Bourne Court, Essex, UK) for enable us to make use of the Accu-SPINA device. Steadfast Corporation Ltd had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation and review of the manuscript.
References
- 1.Anema JR, Steenstra IA, Bongers PM, et al. Multidisciplinary rehabilitation for subacute low back pain: graded activity or workplace intervention or both? A randomized controlled trial. Spine. 2007;32:291–298. doi: 10.1097/01.brs.0000253604.90039.ad. [DOI] [PubMed] [Google Scholar]
- 2.Beattie PF, Nelson RM, Michener LA, et al. Outcomes after a prone lumbar traction protocol for patients with activity-limiting low back pain: a prospective case series study. Arch Phys Med Rehabil. 2008;89:269–274. doi: 10.1016/j.apmr.2007.06.778. [DOI] [PubMed] [Google Scholar]
- 3.Beurskens AJ, de Vet HC, Koke AJ, et al. Efficacy of traction for nonspecific low back pain: 12-week and 6-month results of a randomized clinical trial. Spine. 1997;22:2756–2762. doi: 10.1097/00007632-199712010-00011. [DOI] [PubMed] [Google Scholar]
- 4.Borman P, Keskin D, Bodur H. The efficacy of lumbar traction in the management of patients with low back pain. Rheumatol Int. 2003;23:82–86. doi: 10.1007/s00296-002-0249-0. [DOI] [PubMed] [Google Scholar]
- 5.Clarke J, van Tulder M, Blomberg S, et al. Traction for low back pain with or without sciatica: an updated systematic review within the framework of the Cochrane collaboration. Spine. 2006;31:1591–1599. doi: 10.1097/01.brs.0000222043.09835.72. [DOI] [PubMed] [Google Scholar]
- 6.Fritz JM, Lindsay W, Matheson JW, et al. Is there a subgroup of patients with low back pain likely to benefit from mechanical traction? Results of a randomized clinical trial and subgrouping analysis. Spine. 2007;32:E793–E800. doi: 10.1097/BRS.0b013e31815d001a. [DOI] [PubMed] [Google Scholar]
- 7.Gay RE, Brault JS. Evidence-informed management of chronic low back pain with traction therapy. Spine J. 2008;8:234–242. doi: 10.1016/j.spinee.2007.10.025. [DOI] [PubMed] [Google Scholar]
- 8.Grotle M, Brox JI, Vollestad NK. Concurrent comparison of responsiveness in pain and functional status measurements used for patients with low back pain. Spine. 2004;29:E492–E501. doi: 10.1097/01.brs.0000143664.02702.0b. [DOI] [PubMed] [Google Scholar]
- 9.Macario A, Pergolizzi JV. Systematic literature review of spinal decompression via motorized traction for chronic discogenic low back pain. Pain Pract. 2006;6:171–178. doi: 10.1111/j.1533-2500.2006.00082.x. [DOI] [PubMed] [Google Scholar]
- 10.Macario A, Richmond C, Auster M, et al. Treatment of 94 outpatients with chronic discogenic low back pain with the DRX9000: a retrospective chart review. Pain Pract. 2008;8:11–17. doi: 10.1111/j.1533-2500.2007.00167.x. [DOI] [PubMed] [Google Scholar]
- 11.McClure D, Farris B (2006) Intervertebral Differential Dynamics Therapy—a new direction for the initial treatment of low back pain. Eur Musculoskeletal Rev 1:45–47 (Ref Type: Report)
- 12.Ostelo RW, Swinkels-Meewisse IJ, Knol DL, et al. Assessing pain and pain-related fear in acute low back pain: what is the smallest detectable change? Int J Behav Med. 2007;14:242–248. doi: 10.1007/BF03002999. [DOI] [PubMed] [Google Scholar]
- 13.Picavet HS, Schouten JS. Musculoskeletal pain in the Netherlands: prevalences, consequences and risk groups, the DMC(3)-study. Pain. 2003;102:167–178. doi: 10.1016/s0304-3959(02)00372-x. [DOI] [PubMed] [Google Scholar]
- 14.Picavet HS, Vlaeyen JW, Schouten JS. Pain catastrophizing and kinesiophobia: predictors of chronic low back pain. Am J Epidemiol. 2002;156:1028–1034. doi: 10.1093/aje/kwf136. [DOI] [PubMed] [Google Scholar]
- 15.Shealy CN, Borgmeyer V. Decompression, reduction, and stabilization of the lumbar spine: a cost-effective treatment for lumbosacral pain. Am J Pain Manage. 1997;7:663–665. [Google Scholar]
- 16.Shealy CN, Koladia N, Wesemann MM. Long-term effect analysis of IDD therapy in low back pain: a retrospective clinical pilot study. Am J Pain Manage. 2005;15:93–97. [Google Scholar]
- 17.Staal JB, Hlobil H, Twisk JW, et al. Graded activity for low back pain in occupational health care: a randomized, controlled trial. Ann Intern Med. 2004;140:77–84. doi: 10.7326/0003-4819-140-2-200401200-00007. [DOI] [PubMed] [Google Scholar]
- 18.van Tulder MW, Koes BW, Bouter LM. Conservative treatment of acute and chronic nonspecific low back pain. A systematic review of randomized controlled trials of the most common interventions. Spine. 1997;22:2128–2156. doi: 10.1097/00007632-199709150-00012. [DOI] [PubMed] [Google Scholar]
- 19.Werners R, Pynsent PB, Bulstrode CJ. Randomized trial comparing interferential therapy with motorized lumbar traction and massage in the management of low back pain in a primary care setting. Spine. 1999;24:1579–1584. doi: 10.1097/00007632-199908010-00012. [DOI] [PubMed] [Google Scholar]