Abstract
Psychological factors have been found to be of major importance for the transition from acute to chronic low back pain (CLBP). Although some evidence has been provided that depressive symptoms occur secondarily to CLBP, psychological treatment modules that specifically address depressive symptoms are not yet included in German inpatient rehabilitation programs. In this study, a standard rehabilitation program for patients with CLBP and depressive symptoms was compared to a standard rehabilitation, into which a cognitive-behavioral management training of depressive symptoms was integrated. Moreover, treatment effects of this multidisciplinary standard rehabilitation program delivered to patients with either no or only mild depressive symptoms were investigated. As a further aim of the present study, gender effects on rehabilitation outcomes were examined. Short-, mid-, and long-term effects on individual global improvement as well as pain-related, psychological, and work-related measures were evaluated among N = 199 consecutively admitted patients with CLBP, aged from 24 to 62 years. The standard rehabilitation program had no persisting effects on psychological outcomes among patients with no and mild depressive symptoms. Patients with moderate and severe depressive symptoms in the standard rehabilitation program did not benefit with clinical importance at the 6- and 12-month follow-up assessments, but did show clinically significant improvements in psychological outcome measures at the 6-month follow-up assessment when the supplemental psychological component was applied. Additionally, days of sick leave decreased in the intervention group in the mid-term when compared to the baseline. Females benefited more in mental health than males. However, due to regression effects at the 12-month follow-up assessment, booster sessions are highly recommended. The results presented here support the notion that a more adequately tailored rehabilitation program seems to improve rehabilitation success and prevent further development of CLBP among this high-risk subpopulation.
Keywords: Chronic low back pain, Depressive symptoms, Gender, Multidisciplinary inpatient orthopedic rehabilitation, Cognitive-behavioral management of depressive symptoms
Introduction
Low back pain is a complaint that is associated with a large financial burden for health care systems, predominantly due to increased indirect costs [1, 38, 42]. Additionally, a considerable risk of a transition from acute to chronic low back pain (CLBP) has been demonstrated, mainly affected by psychological and social factors [10, 21, 28, 33]. Regarding psychological factors, the significant impact of clinical and subclinical levels of anxiety and depression on the development of chronicity has been demonstrated [6, 21, 22, 28, 31]. Thereby, cognitive factors seem to particularly mediate the relationship of pain with functional and emotional adjustment [8, 20, 40].
Based on the widely accepted multidimensional concept of CLBP, multimodal and multidisciplinary rehabilitation programs have been designed. Many systematic reviews and meta-analytic studies support that compared to no-treatment, waiting list, and single biomedical treatments, multidisciplinary treatments provide greater beneficial effects if cognitive-behavioral components are integrated [3, 7, 11, 14, 24, 25, 27, 29, 37, 39]. Further studies lend support to the assumption that psychological factors are of greater importance for therapeutic success than other variables, such as medical findings or physical performance factors [8, 10, 43]. In particular, coping with pain and beliefs regarding the controllability of pain have been found to be prognostic factors [30, 35, 40]. Although favorable effects of cognitive-behavioral treatments on psychological outcome measures have been demonstrated, the impact on pain-related outcome measures seems to be diminished [39].
Mixed results were reported for the predictive validity of depressive symptoms for rehabilitation success [35, 41]. Patients with moderate and severe depressive symptoms benefited less from a standard multidisciplinary rehabilitation program compared to patients with no and mild depressive symptoms [23]. Interestingly, improvements in self-rated depressive symptoms and disability during inpatient multidisciplinary rehabilitation had a prognostic value [27]. Thus, it can be assumed that decreasing depressive symptoms would improve the rehabilitation outcome and would prevent further transition to CLBP.
Likewise, inconsistent findings were reported regarding the predictive validity of gender for rehabilitation success, with studies finding either no gender effects [35] or better rehabilitation outcomes among females [18, 19, 23].
Finally, mixed results regarding the persistence of treatment gains have been presented, showing stable treatment effects at follow-up assessments from at least 7 months to 13 years [2, 7, 18, 26] or slight regression effects on depressive symptoms, catastrophizing coping, and lumbar flexion tests at the 6- and 12-month follow-up assessments [27]. Van Tulder et al. [37] concluded that long-term effects of non-invasive treatment modalities on pain and function have not been supported by their systematic review, a conclusion that was confirmed recently for intensive group training [36].
The aim of this study was to evaluate effects of a cognitive-behavioral management training of depressive symptoms, integrated in a standard multidisciplinary inpatient rehabilitation program for patients with CLBP as well as moderate and severe depressive symptoms. Within this context, 1 year longitudinal rehabilitation effects of this newly developed program on a work-related measure as well as pain-related and psychological measures were compared to standard rehabilitation. It was expected that the newly developed program would elicit increased and stable improvements. Moreover, the standard rehabilitation program was also delivered to patients with no and mild depressive symptoms and was predicted to be effective among this subgroup. To further illuminate gender-specific rehabilitation effects, the study also focused on gender differences in rehabilitation outcome. Thus, based on the results of our study, more adequately tailored rehabilitation programs could be designed in order to improve rehabilitation outcomes.
Methods
Design
A three-factorial design with two between-subjects factors and one within-subjects factor was conducted. The first factor represented the treatment condition, with two control groups, both participating in a standard rehabilitation program, and one intervention group. The first control group consisted of patients with no and mild depressive symptoms (CG; n = 92) and the second control group of patients with moderate and severe depressive symptoms (CGdepr; n = 52). The patients assigned to the intervention group had moderate and severe depressive symptoms and took part in the standard rehabilitation program combined with a cognitive-behavioral management training of depressive symptoms (IGdepr; n = 55). Depressive symptoms were assessed by the General Depression Scale, being a self-report measure (ADS; [15]). The second, quasi-experimental, factor consisted of gender (male, n = 117 vs. female, n = 82). The third factor involved the within-subjects factor of time of assessment with four sample points; rehabilitation outcomes were evaluated prior to rehabilitation (t 1), immediately after rehabilitation (t 2), and 6 (t 4) and 12 months after rehabilitation (t 5). A follow-up measurement 3 months after discharge (t 3) was also carried out, but is not taken into consideration in the present analyses.
For the purpose of assignment, the ADS was administered by physicians (orthopaedists or rheumatologists) during patients’ initial physical examinations at the clinics. Patients were informed that the ADS would be used to determine their stress level and to tailor the rehabilitation program to their individual needs. Assignment was carried out by an independent doctoral student at the University of Bremen. Physicians and nursing staff at the clinics were blind to patients’ group assignments. Participants with no and low depressive symptoms were only treated with the standard rehabilitation program. A treatment of depressive symptoms among these participants seemed not to be indicated neither for conceptual reasons nor for economical reasons.
Participants with moderate and severe depressive symptoms were assigned to the control and intervention groups. In order to prevent conducting both treatment conditions simultaneously in a clinic and obscuring the internal validity of the study due to a loss of motivation in the control group, prior to the study time periods were fixed for each clinic, in which the control or experimental condition should be realized. Both participating clinics carried out both treatment conditions in alternating and reverse sequence. Thus, in order to control for seasonal effects, one clinic delivered the control condition, whilst the other conducted the experimental condition. In following trials, treatment conditions were changed in both clinics.
To orthogonalize the distribution of sample size in the design, 19 male participants assigned to the CG were excluded at random (χ 2 (df = 2) = 3.18, P = ns).
Participants
In total, 199 participants with CLBP were included in the study. Participants ranged in age from 24 to 62 years (M = 49.00, SD = 7.03). The mean pain duration was 13.00 years (SD = 9.25). Participants were recruited from two inpatient orthopedic rehabilitation clinics. The inclusion criteria were as follows: non-specific CLBP with at least six-month pain duration, ICD-10 diagnoses (M54.4, M54.5), age between 20 and 62 years, and fluency in the German language. The following exclusion criteria were applied to this study: specific etiology of back pain (surgery or accidents during 6 months prior to rehabilitation, somatic disorders such as radicular syndrome, neoplasms, osteoporosis, inflammatory diseases, fibromyalgia), pregnancy, other physical complications (acute infections, cardiovascular diseases, internal medical conditions), and mental disorders (psychosis, post-traumatic stress disorder).
The study was conducted with the approval of the Institutional Review Board of the University of Bremen. All participants were informed by a clinic physician and a patient information sheet about the study aims, following a multidimensional concept of pain and investigating pain experiences, coping with pain, and pain-related impairment in daily life. Moreover, after the assignment based on the ADS, it was explained to possible participants of the IGdepr that the supplemental program was designed to address their higher stress level, which also had been detected by the ADS. All patients were asked to give their written informed consent within 2 days after the physical consultation and prior to the start of the interventions.
Baseline characteristics of participants for each treatment condition and both genders are summarized in Table 1. Female participants as well as participants with depressive symptoms (CGdepr, IGdepr) scored higher on mental health. Furthermore, they showed higher frequencies of unemployment, stage of chronicity III of the MPSS, clinical depression, and somatization. Compared to male participants, slightly more female participants took in antidepressants during the last 4 weeks.
Table 1.
Baseline characteristics of participants by different treatment condition and gender
| Variable | CG (n = 92) | CGdepr (n = 54) | IGdepr (n = 55) | Males (n = 117) | Females (n = 82) |
|---|---|---|---|---|---|
| Socio-demographic data | |||||
| Age (year) (mean ± SD) | 48.65 ± 7.52 | 49.21 ± 7.51 | 49.32 ± 5.60 | 48.34 ± 6.92 | 49.86 ± 7.14 |
| BMI (kg/m2) (mean ± SD) | 28.91 ± 5.38 | 29.31 ± 6.23 | 29.82 ± 6.26 | 28.57 ± 4.96 | 30.29 ± 6.83 |
| Gender, females no. (%) | 32 (34.8%) | 23 (44.2%) | 27 (49.1%) | 0 (0.0%) | 82 (100.0%) |
| Married no. (%) | 63 (70.0%) | 39 (81.3%) | 35 (64.8%) | 79 (69.9%) | 58 (73.4%) |
| Educational level (%) | |||||
| Low | 68.9% | 70.8% | 61.8% | 68.1% | 66.3% |
| Middle | 21.1% | 16.7% | 27.3% | 22.1% | 21.3% |
| High | 2.2% | 8.3% | 1.8% | 1.8% | 1.3% |
| Work-related data | |||||
| Employed no. (%) | 82 (91.1%) | 42 (87.5%) | 44 (80.0%) | 102 (90.3%) | 66 (82.5%) |
| Duration of unemployment no. (%) | |||||
| More than 1 year | 5 (5.6%) | 5 (10.4%) | 7 (13.0%) | 6 (5.3%) | 11 (13.9%) |
| Days of sick leave due to pain in the last 3 months no. (%) | |||||
| More than 2 weeks | 31 (35.6%) | 12 (26.7%) | 23 (44.2%) | 44 (39.3%) | 22 (30.6%) |
| Application for early retirement no. (%) | 1 (1.1%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (1.3%) |
| Pain history | |||||
| Pain duration (year) (mean ± SD) | 12.74 ± 9.44 | 13.96 ± 10.16 | 12.38 ± 7.79 | 13.04 ± 9.66 | 12.94 ± 8.68 |
| Pain locations (mean ± SD) | 3.71 ± 2.09 | 4.73 ± 2.71 | 4.74 ± 2.69 | 3.67 ± 2.13 | 5.12 ± 2.70 |
| Average pain intensity (mean ± SD) | 5.30 ± 1.88 | 5.43 ± 2.00 | 5.84 ± 2.01 | 5.42 ± 1.80 | 5.56 ± 2.16 |
| Stage of chronicity (MPSS) no. (%) | |||||
| I | 51 (56.7%) | 21 (41.2%) | 23 (42.6%) | 62 (54.4%) | 33 (40.7%) |
| II | 35 (38.9%) | 25 (49.0%) | 25 (46.3%) | 50 (43.9%) | 35 (43.2%) |
| III | 4 (4.4%) | 5 (9.8%) | 6 (11.1%) | 2 (1.8%) | 13 (16.0%) |
| Psychological status | |||||
| Clinical depression (ADS) no. (%) | 0 (0.0%) | 20 (38.5%) | 24 (43.6%) | 21 (17.9%) | 23 (28.0%) |
| Clinical anxiety (HADS-D) no. (%) | 0 (0.0%) | 18 (34.6%) | 17 (31.5%) | 18 (15.5%) | 17 (20.7%) |
| Clinical somatization (SCL-90-R) no. (%) | 41 (45.6%) | 37 (71.2%) | 40 (83.3%) | 63 (56.3%) | 55 (70.5%) |
| Physical health status (SF-12) (mean ± SD) | 35.20 ± 8.86 | 35.85 ± 8.58 | 33.72 ± 9.31 | 34.75 ± 8.37 | 35.28 ± 9.66 |
| Mental health status (SF-12) (mean ± SD) | 54.85 ± 7.37 | 41.60 ± 10.08 | 41.97 ± 9.44 | 50.41 ± 9.80 | 44.12 ± 11.30 |
| Taking antidepressants in the last 4 weeks no. (%) | 1 (1.1%) | 2 (3.9%) | 4 (8.2%) | 2 (1.8%) | 5 (6.5%) |
MPSS Mainz pain staging system, ADS general depression scale, HADS-D hospital anxiety and depression scale, SCL-90-R symptom checklist revised version, SF-12 short-form health survey; response ranges: average pain intensity (0–10), health status (0–100)
Treatment conditions
All participants were treated with the standard rehabilitation program, which consisted of a multimodal and multidisciplinary treatment and followed a bio-psycho-social therapeutic approach. Besides medical and physiotherapeutic interventions, a cognitive-behavioral pain management was integrated. Additionally, a cognitive-behavioral management training of depressive symptoms was administered to the intervention group. Both treatments were conducted during inpatient orthopedic rehabilitation lasting 3–4 weeks.
Cognitive-behavioral pain management and cognitive-behavioral management of depressive symptoms each consisted of 60 min sessions and were carried out in closed intervention groups of eight patients. The cognitive-behavioral training sessions of the IGdepr were carried out in alternating order, starting with a cognitive-behavioral pain management session and followed by a session of cognitive-behavioral management of depressive symptoms to consolidate contents of the pain management training. Sessions of relaxation training were delivered to open groups of 12–16 patients. All psychological interventions were conducted by clinical psychologists.
Standard rehabilitation program
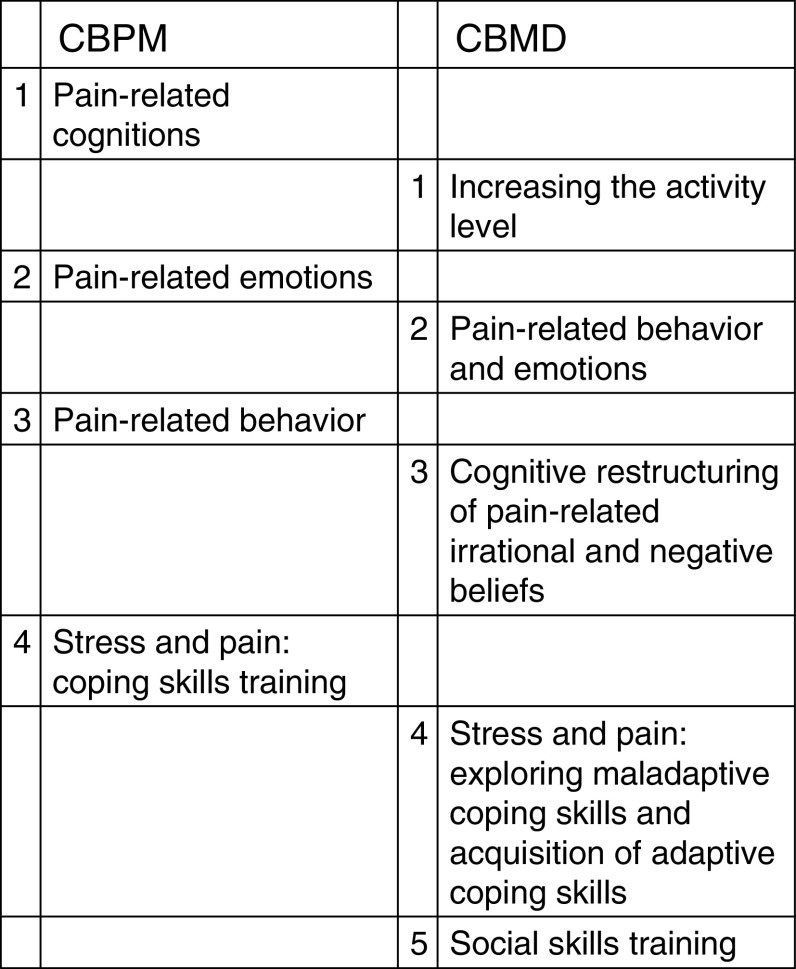
In addition to pharmacotherapy, this standard rehabilitation program consisted of 21.5–26.5 treatment hours per week and incorporated diverse evidence-based modules, such as exercise training (individual and group physiotherapy, pool training), individually adapted medical training therapy, cognitive-behavioral pain management (4 × 60 min sessions), progressive muscle relaxation (6 sessions; 1 × 50 min introduction, 5 × 30 min exercising), and psycho-education (approximately 5 group discussions per week; for evidence-based health care in CLBP, see e.g., [37]). The cognitive-behavioral pain management training was aimed to increase patients’ understanding of a multidimensional concept of pain. Thus, knowledge about chronic pain and pain-eliciting and pain-exacerbating cognitions, emotions, and behavioral patterns were identified. Moreover, in order to promote patients’ self-management competencies and self-efficacy expectations, participants learned skills to manage pain and stress (Fig. 1). The first three sessions focused on the relationship of pain perception with positive and negative thoughts (session 1), with positive and negative emotions (session 2), and with positive and negative behavioral patterns (session 3). In the fourth session, the association of stress and pain perception was discussed and adaptive coping strategies were learned. In addition, an enjoyment exercise was practiced, focusing on the experience of diverse tastes.
Fig. 1.
Overview on the treatment elements of the cognitive-behavioral pain management (CBPM) and the cognitive-behavioral management of depressive symptoms (CBMD)
Cognitive-behavioral management of depressive symptoms
This supplemental program included five 60 min sessions aimed to provide information on the relationship of somatic, emotional, cognitive, and behavioral depressive symptoms with pain perception. Thus, the following elements of a treatment of depressive symptoms were incorporated: enhancement of the activity level, cognitive restructuring, and social skills training (Fig. 1). Furthermore, behavioral expression of pain and the role of significant others in the maintenance of pain behavior were discussed (session 2). Based on the preceding session of the cognitive-behavioral pain management, cognitive and behavioral skills to cope with daily stressors and pain as well as emotion-regulating strategies to manage stressors and pain were further improved in the fourth session. Additionally, maladaptive coping strategies were explored and adaptive coping skills were practiced.
Measures
At the baseline assessment, socio-demographic information, work-related parameters, and physical data were collected. Furthermore, stage of chronicity was assessed at the pre-treatment assessment by a physician using the Mainz Pain Staging System (MPSS; [12; cf. 13]). Moreover, in accordance with a bio-psycho-social approach and in line with the recommendations of Turk et al. [34], the following outcome measures were assessed.
Work-related measure
Patients reported their days of sick leave over the prior 3 months.
Individual global improvement
Subjective rehabilitation success was rated on a 6-point Likert scale of a single item and recoded (1 = ‘very good’ to 6 = ‘insufficient’).
Pain-related measures
The current number of pain sites was reported in answer to an open question. Average pain intensity over the prior 2 weeks was evaluated on an 11-point Likert scale, ranging from ‘no pain’ (0) to ‘pain as bad as could be’ (10).
Psychological measures
Depressive symptoms over the prior week were assessed by a German version of the CES-D, the ADS [16], consisting of 20 items with 4-point numerical scales (0 = ‘seldom’ to 3 = ‘mostly’; response range: 0–60). Sum scores ≥24 were clinically significant. Anxiety over the prior week was measured by the German version of the Hospital Anxiety and Depression Scale (HADS-D Anxiety; [17]), operationalized by seven items with 4-point numerical scales (0 = ‘not at all’ to 3 = ‘mostly’; response range: 0–21). Sum scores ≥11 were clinically significant. Somatization related to the prior week was measured by the 12-item subscale of the German version of the Symptom Checklist (SCL-R; [9]). Items were evaluated on 5-point Likert scales (0 = ‘not at all’ to 4 = ‘strongly’; response range: 0–48). T-scores ≥60 were clinically significant. Generic health functioning was assessed by a German short version of the short-form health survey (SF-36; [4]). Physical and mental health status during the prior 2 weeks were assessed using six items each. Both subtest scores were transformed into a 0–100 scale.
Reliability and validity of the psychosocial self-report measures used have been proven to be good.
Procedure
All pain-related and psychological measures were assessed at all four sample points. Days of sick leave were measured at the pre-treatment, 6-month follow-up, and 12-month follow-up assessments. Subjective rehabilitation success was estimated at the post-treatment, 6-month, and 12-month follow-up assessments. Questionnaires at the pre- and post-treatment assessments were completed at the rehabilitation clinics in groups supervised by trained nursing staff, whereas data for the follow-up assessments were collected by postal inquiry.
Statistical analyses
Missing values
Due to missing values across all four sample points, sample sizes were reduced to the following: days of sick leave: N = 151, subjective rehabilitation success: N = 191, pain sites: N = 182, average pain intensity: N = 185, anxiety: N = 196, and SF-12, health functioning: N = 177.
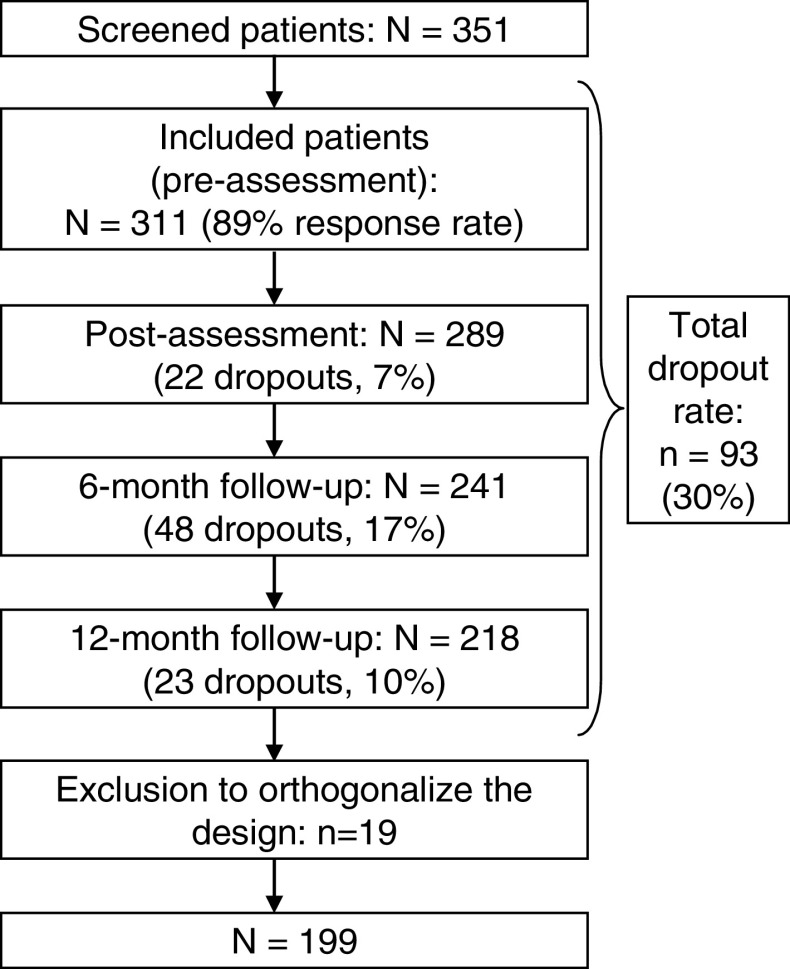
Attrition rates
In total, 351 participants were asked during the physical interview at the pre-treatment assessment to participate in the study (Fig. 2). Forty participants refused to take part in the study, from whom no further information was available (response rate: 89%). Only 22 participants (7%) dropped out during the inpatient rehabilitation. All of these participants had to leave the clinic at an earlier stage due to personal reasons. At the 6-month follow-up, 48 participants (17%), and at the 12-month follow-up, 23 participants (9%) discontinued their participation. Eight drop-out patients (one to two patients of the six experimental groups) participated in the 12-month assessment, but did not complete the questionnaires at one of the preceding sample points. These patients were excluded, as results of multivariate analyses of variance with repeated measurement (MANOVAR) on psychological outcomes at the pre-, post-, and 12-month follow-up assessments did not differ if analyses were carried out with and without these eight patients. In total, 30% of participants dropped out through the study.
Fig. 2.
Schematic diagram of sample sizes prior to, immediately after, 6 months after, and 12 months after rehabilitation
Dropout analyses
χ 2 tests revealed that the dropout rates at the three sample points were not significantly different between the three treatment groups (post: χ 2 (df = 2) = 1.18, P = ns; 6-month follow-up: χ 2 (df = 2) = 3.88, P = ns; 12-month follow-up: χ 2 (df = 2) = 1.13, P = ns). Further analyses of pre-treatment assessment scores, comparing the remaining 199 participants with the 93 participants who dropped out, suggested that the groups did not differ in socio-demographic measures, employment status, days of sick leave, or MPSS. In contrast, t tests indicated that participants who dropped out scored lower on mental health and higher on anxiety. However, post hoc t tests confirmed that participants who had dropped out of the CGdepr and IGdepr did not differ in the psychosocial status at the pre-assessment.
Parametric procedures
As analyses of variance performed on baseline scores revealed that the two treatment conditions did not differ significantly in outcome measures, controlling for baseline scores by analysis of covariance was not indicated. To investigate rehabilitation effects on both pain-related measures and the psychological outcomes of depressive symptoms, anxiety, and somatization, two-way univariate analyses of variance with repeated measurements (ANOVARs) were conducted. The between-subjects factors consisted of ‘treatment condition’ (CG vs. CGdepr vs. IGdepr) and ‘gender’ (male vs. female); the within-subjects factor ‘time’ was comprised of the four sample points (pre-treatment, post-treatment, 6-month follow-up, and 12-month follow-up). For health-related quality of life, a two-way MANOVAR was performed first. To locate effects on the two subscales of health functioning, subsequent univariate analyses of variance with repeated measurements (ANOVARs) were carried out. The two-way univariate ANOVAR for the subjective rehabilitation success was performed with the following sample points: post-treatment, and 6-month and 12-month follow-up assessments. To control for possible heterogeneous variance-covariance matrices, Greenhouse-Geisser corrections were used. To identify dependent and independent mean differences, mean comparisons by Bonferroni were conducted. The significance level was not adjusted as the tests served to generate hypotheses. All results were based on two-tailed tests using P < 0.05. Interaction effects with time were interpreted to focus on results with content validity. To explore treatment effects on physical and pain-related outcome measures, pairwise comparisons for physical health and average pain intensity were performed post hoc.
All treatment effects for both groups with moderate and high depressive symptoms (CGdepr, IGdepr) were replicated by 2 × 2 × 4 ANOVARs and a MANOVAR, when the CG was excluded from the factor “treatment condition”. To generate hypotheses regarding the needs of treatment of participants with no and low depressive symptoms, this treatment condition was included in the present analyses.
To evaluate the clinical significance of rehabilitation effects, within-group effect sizes were calculated using Cohen’s d [5], subtracting each assessment sample mean (post, 6-, and 12-month follow-up) from its preceding assessment sample mean and dividing by the standard deviation of the preceding assessment (e.g., ES = (M pre − M post)/SDPre). Selected between-group effect sizes were also calculated by subtracting the mean of the control group from the mean of the intervention group and dividing by the pooled standard deviation of both groups. Effect sizes with d = 0.20 were considered to be small, d = 0.50 medium, and d = 0.80 large.
Non-parametric procedures
To examine rehabilitation effects on the days of sick leave over the prior 3 months, Wilcoxon sign-rank tests with the comparison of the three sample points (pre-treatment and 6 and 12 months after rehabilitation) were carried out separately for males in the CG, females in the CG, males in the CGdepr, females in the CGdepr, males in the IGdepr, and females in the IGdepr. For simplicity, means and standard deviations are depicted in Table 6 instead of mean ranks.
Table 6.
Means (M), standard deviations (SD) and results of Wilcoxon sign-rank tests for days of sick leave
| CG | CGdepr | IGdepr | CG | CGdepr | IGdepr | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| t 1 | t 4 | t 5 | t 1 | t 4 | t 5 | t 1 | t 4 | t 5 | t 1 – t 4 | t 1 – t 5 | t 4 – t 5 | t 1 – t 4 | t 1 – t 5 | t 4 – t 5 | t 1 – t 4 | t 1 – t 5 | t 4 – t 5 | ||
| Male | |||||||||||||||||||
| M | 25.41 | 5.47 | 7.72 | 23.73 | 11.07 | 11.38 | 34.25 | 11.93 | 9.76 | Z | −3.78 | −3.83 | −0.89 | −1.57 | −1.88 | −0.41 | −2.65 | −1.71 | −0.95 |
| SD | 35.69 | 15.53 | 21.19 | 30.35 | 24.85 | 29.16 | 38.33 | 24.36 | 19.05 | P | <0.001 | <0.001 | 0.375 | 0.116 | 0.060 | 0.686 | 0.008 | 0.088 | 0.341 |
| Female | |||||||||||||||||||
| M | 22.03 | 12.94 | 12.91 | 19.82 | 7.74 | 5.55 | 25.76 | 11.41 | 11.36 | Z | −1.76 | −1.55 | −0.71 | −1.11 | −2.25 | −0.93 | −2.08 | −1.70 | −0.32 |
| SD | 30.39 | 25.68 | 26.20 | 31.45 | 20.96 | 20.03 | 38.44 | 26.94 | 26.40 | P | 0.078 | 0.121 | 0.477 | 0.226 | 0.025 | 0.352 | 0.037 | 0.089 | 0.752 |
CG control group with mild depressive symptoms, CG depr control group with moderate and severe depressive symptoms, IG depr intervention group with moderate and severe depressive symptoms. t 1 = pre, t 4 = 6 months after, t 5 = 12 months after rehabilitation
Results
Effects of treatment condition, gender, and time on psychosocial outcome measures
MANOVAR and ANOVAR results for the psychological and pain-related measures as well as subjective rehabilitation success are presented in Tables 2 and 3. In the two-way MANOVAR for generic health functioning, the simple interaction of treatment condition by time was statistically significant. Thus, post hoc derived ANOVAR results were interpreted.
Table 2.
Summary of MANOVAR and ANOVAR results for main effects of ‘treatment condition (TC)’, ‘gender (G)’, and ‘time (T)’ and interaction effects on psychological outcome measures
| Variable | Factors | ||||||
|---|---|---|---|---|---|---|---|
| TC | G | TC × G | T | TC × T | G × T | TC × G × T | |
| Depressive symptoms | |||||||
| df 1,2 | 2, 193 | 1, 193 | 2, 193 | 2.6, 495.9 | 5.1, 495.9 | 2.6, 495.9 | 5.1, 495.9 |
| F | 73.21 | 5.68 | 3.03 | 23.93 | 7.77 | 1.60 | 0.59 |
| P | <0.001 | 0.018 | 0.051 | <0.001 | <0.001 | 0.196 | 0.712 |
| η 2 | 0.431 | 0.029 | 0.030 | 0.110 | 0.074 | 0.008 | 0.006 |
| Anxiety | |||||||
| df 1,2 | 2, 190 | 1, 190 | 2, 190 | 2.6, 487.7 | 5.1, 487.7 | 2.6, 487.7 | 5.1, 487.7 |
| F | 61.42 | 2.59 | 0.60 | 33.51 | 4.46 | 2.60 | 1.19 |
| P | <0.001 | 0.109 | 0.553 | <0.001 | <0.001 | 0.061 | 0.314 |
| η 2 | 0.393 | 0.013 | 0.006 | 0.150 | 0.045 | 0.013 | 0.012 |
| Somatization | |||||||
| df 1,2 | 2, 193 | 1, 193 | 2, 193 | 2.4, 465.2 | 4.8, 465.2 | 2.4, 465.2 | 4.8, 465.2 |
| F | 23.35 | 8.54 | 0.64 | 15.33 | 1.63 | 2.37 | 0.65 |
| P | <0.001 | 0.004 | 0.527 | <0.001 | 0.154 | 0.083 | 0.660 |
| η 2 | 0.195 | 0.042 | 0.007 | 0.074 | 0.017 | 0.012 | 0.007 |
| SF-12 | |||||||
| df 1,2 | 4, 340 | 2, 170 | 4, 340 | 6, 1024 | 12, 1024 | 6, 1024 | 12, 1024 |
| F | 24.33 | 2.22 | 1.46 | 21.10 | 3.56 | 2.71 | 1.59 |
| P | <0.001 | 0.111 | 0.214 | <0.001 | <0.001 | 0.013 | 0.089 |
| η 2 | 0.223 | 0.025 | 0.017 | 0.110 | 0.040 | 0.016 | 0.018 |
| Physical health | |||||||
| df 1,2 | 2, 171 | 1, 171 | 2, 171 | 2.6, 442.6 | 5.2, 442.6 | 2.6, 442.6 | 5.2, 442.6 |
| F | 2.53 | 0.27 | 0.45 | 11.65 | 0.52 | 0.74 | 1.12 |
| P | 0.083 | 0.601 | 0.636 | <0.001 | 0.766 | 0.508 | 0.348 |
| η 2 | 0.029 | 0.002 | 0.005 | 0.064 | 0.006 | 0.004 | 0.013 |
| Mental health | |||||||
| df 1,2 | 2, 171 | 1, 171 | 2, 171 | 2.7, 461.9 | 5.4, 461.9 | 2.7, 461.9 | 5.4, 461.9 |
| F | 54.06 | 4.46 | 2.09 | 32.01 | 6.76 | 4.78 | 2.06 |
| P | <0.001 | 0.036 | 0.126 | <0.001 | <0.001 | 0.004 | 0.063 |
| η 2 | 0.387 | 0.025 | 0.024 | 0.158 | 0.073 | 0.027 | 0.024 |
df 1,2 degrees of freedom
Table 3.
Summary of MANOVAR and ANOVAR results for main effects of ‘treatment condition (TC)’, ‘gender (G)’, and ‘time (T)’ and interaction effects on pain-related outcome measures and subjective rehabilitation success
| Variable | Factors | ||||||
|---|---|---|---|---|---|---|---|
| TC | G | TC × G | T | TC × T | G × T | TC × G × T | |
| Average pain intensity | |||||||
| df 1,2 | 2, 179 | 1, 179 | 2, 179 | 2.9, 515.3 | 5.8, 515.3 | 2.9, 515.3 | 5.8, 515.3 |
| F | 6.30 | 2.44 | 0.47 | 19.71 | 0.95 | 0.42 | 1.52 |
| P | 0.002 | 0.296 | 0.626 | <0.001 | 0.459 | 0.732 | 0.172 |
| η 2 | 0.066 | 0.006 | 0.005 | 0.099 | 0.010 | 0.002 | 0.017 |
| Pain sites | |||||||
| df 1,2 | 2, 176 | 1, 176 | 2, 176 | 2.7, 480.7 | 5.5, 480.7 | 2.7, 480.7 | 5.2, 480.7 |
| F | 4.13 | 16.43 | 1.60 | 9.85 | 0.85 | 2.32 | 1.80 |
| P | 0.018 | <0.001 | 0.205 | <0.001 | 0.522 | 0.080 | 0.104 |
| η 2 | 0.045 | 0.085 | 0.018 | 0.053 | 0.010 | 0.013 | 0.020 |
| Subjective rehabilitation success | |||||||
| df 1,2 | 2, 185 | 1, 185 | 2, 185 | 1.9, 355.9 | 3.8, 355.9 | 1.9, 355.9 | 3.8, 355.9 |
| F | 0.61 | 0.55 | 0.15 | 7.78 | 1.59 | 0.45 | 1.46 |
| P | 0.545 | 0.461 | 0.858 | 0.001 | 0.180 | 0.630 | 0.216 |
| η 2 | 0.007 | 0.003 | 0.002 | 0.040 | 0.017 | 0.002 | 0.016 |
df 1,2 degrees of freedom
Treatment condition by time
Univariate ANOVARs yielded a simple interaction effect for depressive symptoms (Table 2). As shown in Table 4, patients with moderate and severe depressive symptoms benefited from both treatment conditions in the short-term. Unexpectedly, patients of the CG showed a negative rehabilitation effect during both follow-up assessments; depressive symptoms were increased in the CG at the 6- and 12-month follow-up assessments compared to baseline. The rehabilitation effect in the CGdepr did not persist to follow-up assessments. In contrast, statistically and clinically significant mid- and long-term effects were found in the IGdepr. Regarding between-group comparisons, depressive symptoms in the IGdepr were significantly lower at the 6-month follow-up assessment than in the CGdepr (P = 0.025, d between = −0.44).
Table 4.
Means (M), standard deviations (SD), within-group effect sizes (ES), and pairwise comparisons (P values) for the significant interactions ‘treatment condition’ and ‘time’ for selected psychosocial outcome measures
| Variable | CG | CGdepr | IGdepr | CG | CGdepr | IGdepr | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| t 1 | t 2 | t 4 | t 5 | t 1 | t 2 | t 4 | t 5 | t 1 | t 2 | t 4 | t 5 | t 1 – t 2 | t 1 – t 4 | t 1 – t 5 | t 1 – t 2 | t 1 – t 4 | t 1 – t 5 | t 1 – t 2 | t 1 – t 4 | t 1 – t 5 | ||
| Depressive symptoms | ||||||||||||||||||||||
| M | 9.29 | 7.75 | 13.28 | 11.43 | 23.41 | 16.17 | 22.07 | 22.06 | 24.40 | 16.61 | 17.80 | 20.43 | ES | 0.24 | −0.61 | −0.33 | 1.15 | 0.21 | 0.22 | 1.25 | 1.06 | 0.64 |
| SD | 6.55 | 7.44 | 10.24 | 9.19 | 6.28 | 7.14 | 9.82 | 8.82 | 6.24 | 7.09 | 9.76 | 8.76 | P | 0.062 | <0.001 | 0.019 | <0.001 | 0.331 | 0.243 | <0.001 | <0.001 | <0.001 |
| Anxiety | ||||||||||||||||||||||
| M | 4.61 | 2.90 | 4.87 | 4.22 | 9.48 | 6.10 | 8.82 | 8.41 | 9.61 | 6.44 | 6.93 | 8.37 | ES | 0.54 | −0.08 | 0.12 | 1.11 | 0.22 | 0.35 | 1.05 | 0.89 | 0.41 |
| SD | 3.18 | 3.22 | 3.94 | 3.50 | 3.04 | 3.07 | 3.77 | 3.35 | 3.02 | 3.06 | 3.75 | 3.33 | P | <0.001 | 0.538 | 0.267 | <0.001 | 0.223 | 0.014 | <0.001 | <0.001 | 0.004 |
| Physical health | ||||||||||||||||||||||
| M | 35.18 | 40.94 | 39.75 | 38.58 | 35.89 | 40.10 | 37.42 | 37.92 | 33.33 | 37.59 | 35.61 | 36.06 | ES | −0.60 | −0.47 | −0.35 | −0.46 | −0.17 | −0.22 | −0.47 | −0.25 | −0.30 |
| SD | 9.63 | 9.20 | 10.85 | 10.21 | 9.12 | 8.71 | 10.27 | 9.67 | 9.06 | 8.65 | 10.20 | 9.61 | P | <0.001 | 0.001 | 0.002 | <0.001 | 0.358 | 0.116 | <0.001 | 0.191 | 0.044 |
| Mental health | ||||||||||||||||||||||
| M | 54.49 | 58.52 | 52.08 | 53.41 | 40.95 | 52.82 | 43.54 | 42.97 | 41.30 | 47.93 | 48.42 | 41.56 | ES | −0.45 | 0.27 | 0.12 | −1.41 | −0.31 | −0.24 | −0.79 | −0.85 | −0.03 |
| SD | 8.90 | 7.59 | 11.47 | 9.71 | 8.43 | 7.18 | 10.86 | 9.19 | 8.37 | 7.13 | 10.78 | 9.13 | P | <0.001 | 0.095 | 0.375 | <0.001 | 0.138 | 0.175 | <0.001 | <0.001 | 0.871 |
| Average pain intensity | ||||||||||||||||||||||
| M | 5.21 | 3.58 | 4.14 | 4.17 | 5.41 | 4.39 | 5.03 | 5.10 | 5.86 | 4.19 | 5.19 | 5.39 | ES | 0.80 | 0.53 | 0.51 | 0.52 | 0.20 | 0.16 | 0.85 | 0.34 | 0.24 |
| SD | 2.04 | 2.15 | 2.23 | 2.41 | 1.96 | 2.07 | 2.15 | 2.31 | 1.95 | 2.06 | 2.14 | 2.30 | P | <0.001 | <0.001 | <0.001 | 0.001 | 0.274 | 0.363 | <0.001 | 0.064 | 0.178 |
CG control group with mild depressive symptoms, CG depr control group with moderate and severe depressive symptoms, IG depr intervention group with moderate and severe depressive symptoms. t 1 = pre, t 2 = post, t 4 = 6 months after, t 5 = 12 months after rehabilitation
A significant simple interaction effect was also observed for anxiety. All patients showed significantly improved anxiety levels immediately after rehabilitation. The favorable short-term effects of the CG evened out at the follow-up assessments, and thus, anxiety scores at the 6- and 12-month follow-up assessments were not different from the baseline scores. A regression effect was also found in the CGdepr at the 6-month follow-up assessment. At the 12-month follow-up assessment, anxiety scores were significantly improved in comparison with the baseline. In contrast, anxiety levels of the IGdepr were statistically and clinically significantly improved at both follow-up assessments. Furthermore, the IGdepr reported significantly less anxiety than the CGdepr at the 6-month follow-up assessment (P = 0.010, d between = −0.50).
The subsequent ANOVARs for the physical and mental components of health-related quality of life revealed a significant interaction effect for mental health. Again, all three treatment groups benefited substantially from the rehabilitation in the short run. Regression effects were found in the CG and the CGdepr at both follow-up assessments; thus, follow-up assessment scores of psychological well-being did not differ from the baseline scores. In contrast, in the IGdepr, psychological well-being was significantly improved 6 months after discharge, with an effect size of d within = 0.85. Moreover, patients in the IGdepr scored significantly higher on psychological well-being than patients in the CGdepr at the 6-month follow-up assessment (P = 0.030, d between = 0.45). However, at the post-treatment assessment, patients in the IGdepr scored significantly lower on psychological well-being than patients in the CGdepr (P = 0.001, d between = −0.68).
Post hoc calculated within-group effect sizes for SF-12 physical health and average pain intensity indicated that the CG improved in physical health and average pain intensity across all three sample points compared to baseline measures with medium to large effect sizes. The CGdepr did not show persisting rehabilitation effects on either physical outcome measure at the follow-up assessments. The IGdepr did show improved physical health at the 12-month follow-up assessment, but no persistent treatment effects on average pain intensity.
Gender by time
Gender-specific rehabilitation effects were ascertained by a twofold ANOVAR for mental health. As shown in Table 5, both genders benefited significantly from the rehabilitation in the short run. The short-term effect size for females was large, but for males moderate. In males, the favorable short-term effect did not indicate persistency. Unexpectedly, males showed a negative treatment effect at the 12-month follow-up assessment. In contrast, females did show significantly improved psychological functioning at both follow-up assessments compared to baseline. However, the genders did not differ at the follow-up assessments.
Table 5.
Means (M), standard deviations (SD), within-group effect sizes (ES), and pairwise comparisons (P values) for the significant simple interaction ‘gender’ and ‘time’ for mental health
| Variable | Male | Female | Male | Female | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| t 1 | t 2 | t 4 | t 5 | t 1 | t 2 | t 4 | t 5 | t 1 − t 2 | t 1 − t 4 | t 1 −t 5 | t 1 − t 2 | t 1 − t 4 | t 1 – t 5 | ||
| Mental health | |||||||||||||||
| M | 48.43 | 52.90 | 49.07 | 46.26 | 42.74 | 53.28 | 46.97 | 45.69 | ES | −0.50 | −0.07 | 0.24 | −1.25 | −0.50 | −0.35 |
| SD | 9.01 | 7.67 | 11.61 | 9.83 | 8.40 | 7.15 | 10.82 | 9.16 | P | <0.001 | 0.619 | 0.049 | <0.001 | 0.004 | 0.017 |
t 1 = pre, t 2 = post, t 4 = 6 months after, t 5 = 12 months after rehabilitation
Treatment and gender-specific effects on days of sick leave
Wilcoxon sign-rank tests yielded that males in the CG showed significantly decreased days of sick leave at both follow-up assessments, whereas no significant reduction could be observed among females in the CG (Table 6). Males in the CGdepr did not show beneficial effects, but females showed reduced days of sick leave at the 12-month follow-up assessment. Both genders in IGdepr improved in days of sick leave at the 6-month follow-up assessment.
Discussion
Since prior research has provided evidence that psychological problems or manifest psychiatric disorders augment chronicity of pain [6, 21, 22, 28, 31] and impair the rehabilitation outcome [23, 41], we designed a cognitive-behavioral management training of depressive symptoms for participants with moderate and severe depressive symptoms to improve treatment outcomes in this high-risk subpopulation. An inpatient program was initiated, as patients with CLBP in Germany are used to be treated in rehabilitation clinics far from home. However, few current outpatient programs were designed, adapting inpatient programs. These programs seem to be more accepted by patients who show a higher stage of chronicity and are more occupied at home. Short-, mid-, and long-term effects on individual global improvement as well as pain-related, psychosocial, and work-related measures were evaluated among 199 consecutively admitted patients with CLBP aged from 24 to 62 years. The newly developed inpatient orthopedic rehabilitation program for patients with moderate and severe depressive symptoms was compared to a multidisciplinary standard rehabilitation program without the additional psychological component in participants with moderate and severe depressive symptoms. Additionally, effects of the standard rehabilitation were examined in patients with no and mild depressive symptoms. Finally, in order to identify factors moderating the effectiveness of our rehabilitation program, gender-specific effects on the rehabilitation outcome were investigated. These moderating factors could be acknowledged in future conceptualizations of rehabilitation programs.
All patients benefited statistically and clinically significantly from all three treatment conditions in psychological and pain-related outcome measures in the short run. Compared to the within-group effect size of ES = 0.77 reported by Pfingsten et al. [27], the effect size of the CG was substantially lower, but effect sizes of both groups with moderate and severe depressive symptoms were substantially larger. Overall, the medium to large within-effect sizes in the present study are in line with previous results [7, 14, 24, 25, 39].
Treatment-dependent mid- and long-term rehabilitation effects
Mid- and long-term rehabilitation effects were substantially influenced by treatment condition and gender. The results of ANOVARs indicated that patients in the CG did not show stable treatment gains in anxiety and mental health. These non-significant courses at the follow-up assessments might be due to a floor effect. However, unfavorable mid- and long-term effects on depressive symptoms have been found. This might be attributed to the accelerated chronicity over the course of the disease, which is generally associated with increased depressive symptoms; a regression analysis showed that higher depressive symptoms 6 months after rehabilitation were predicted by a higher stage of chronicity and mental health prior to rehabilitation [15]. Although the levels of depressive symptoms were substantially below the clinical cut-off score, this unexpected finding points to the assumption that for this subgroup a preventive intervention with low-intensity management of depressive symptoms might also be recommended. Nevertheless, this adverse effect was only shown in depressive symptoms; post hoc calculated analysis supports that the patients benefited persistently in physical health and average pain intensity from the multidisciplinary standard rehabilitation program.
Patients in the CGdepr showed non-significant or clinically non-relevant improvements in psychological outcome measures at both follow-up assessments. Hence, patients with moderate and severe depressive symptoms who participated in the multidisciplinary standard rehabilitation without the supplemental psychological component did not benefit. These results are in line with a pilot study, suggesting insufficient rehabilitation success in psychosocial outcome measures among this subgroup, which is affected by considerable strain [23].
In contrast, within-group effect sizes for psychological outcome measures among patients in the IGdepr were enhanced compared to the effect sizes in the CGdepr. Thus, short-term treatment gains in levels of depressive symptoms and anxiety were maintained until the 6-month follow-up assessment, showing large effect sizes (depression: d within: 1.1, anxiety: d within: 0.89). However, these short- and mid-term improvements underwent slight regression effects at the 12-month follow-up assessment. Additionally, favorable short-term effects on mental health persisted to the 6-month follow-up assessment, but could not be maintained in the long-term. On the one hand, these results confirm our expectation that our newly developed standard rehabilitation program with a cognitive-behavioral management for depressive symptoms enhances rehabilitation success and reduces important risk factors for a further development of chronicity among this subgroup. However, slight regressions lend support to the assumption that after-care programs should be applied to stabilize short- and mid-term treatment gains.
Moreover, in agreement with prior results and our expectations, the cognitive-behavioral module revealed beneficial persisting effects primarily on psychological outcome measures, but not on pain-related measures [39]. However, patients who dropped out from all three conditions showed an increased anxiety and decreased mental health. Thus, our results are generally restricted to patients with less psychological strain. As both treatment conditions with participants with moderate and severe depressive symptoms who dropped out did not differ in the psychosocial status at pre-assessment, it can be assumed that the effect of our intervention was not overestimated.
Gender-specific mid- and long-term rehabilitation effects
Consistent with our preceding study, females benefited more from treatments than males [23]. Females showed persistent improvements in mental health at both follow-up assessments. In contrast, males improved in the short-term only, but scored lower on mental health at the 12-month follow-up assessment than at the pre-treatment assessment. However, gender-specific treatment effects in the present study were limited to mental health, which might be partly attributed to the impact of the new program, inducing some beneficial rehabilitation effects among males. In sum, to maintain their substantial short- and mid-term improvements, gender effects strengthen the assumption that booster sessions might be indicated for both genders, but especially for males.
The greater benefit among females in the present study is similar to former results provided by Jensen [19], showing greater improvements among females 18 months after a multidisciplinary standard rehabilitation program with a cognitive-behavioral treatment. The authors suggested that the gender difference may be due to the fact that compared to males, females had a greater need for the specific coping strategies or a more efficient employment of these strategies [19, p.76]. However, given the adverse effects on mental health at the 12-month follow-up assessment among males, it can be assumed that the standard rehabilitation with a cognitive-behavioral management of pain facilitates dealing with emotional, cognitive, and somatic aspects associated with pain. Reports from our psychologists support the idea that these aspects were unfamiliar to males. Similarly, Teuber et al. [32] emphasized that sick-role behavior is more compatible with the feminine gender role than with the masculine gender role. Thus, future conceptualizations of psychological treatments for inpatient orthopedic rehabilitation among males should take this aspect into account to enable greater benefits from rehabilitation among males.
Mid- and long-term rehabilitation effects dependent on treatment condition and gender
Slightly better outcomes for males and females in the intervention group at the mid-term were suggested by non-parametric analyses on days of sick leave. In addition, in the CGdepr, females showed a significant reduction in sick leave, but males did not benefit from the standard rehabilitation program. This finding is in line with prior results from Jensen et al. [18, 19] which showed that cognitive-behavioral therapy was more effective 18 months after rehabilitation among females and decreased related costs 3 years after rehabilitation by about €137.509 per female participant due to reduced sick leave.
General conclusions
Although results of the present study have to be interpreted cautiously due to the non-randomized procedure, beneficial short- and mid-term rehabilitation effects on psychological outcome measures of the inpatient standard rehabilitation program with a cognitive-behavioral management training of depressive symptoms for patients with CLBP and depressive symptoms were supported. In line with Sullivan [31, p. 12], it can be stated that these treatment modules, which are aimed at improving depressive symptoms, ‘deserve serious consideration as an integral component of chronic pain rehabilitation’. However, the attenuated increase in mental health from the pre- to post-treatment assessment suggests that more strain might be generated by the more intensive treatment during inpatient rehabilitation. Future studies should investigate if other non-effective elements could be reduced to counteract these adverse effects. Moreover, future studies should address the question of the cost-effectiveness of the newly developed program, which includes five more psychological sessions. We found significant differences between the both treatment groups with moderate and severe depressive symptoms in depressive symptoms, anxiety, and mental health in the mid-term. Furthermore, days of sick leave were reduced in the intervention group but not in the control group in the mid-term. Thus, a main source for increased indirect costs in patients with CLBP [38] might be improved and thus cover the costs of the additional psychological treatment.
In addition, a gender-dependent rehabilitation effect on mental health suggests taking gender-specific aspects into account for the conceptualization of psychological interventions in CLBP. Finally, regression effects support that booster sessions during the first year after rehabilitation [18, 19] or fading out sessions [2] might be highly recommended; this has been realized in these studies with considerable long-term effects. Apart from this, our newly developed program seems to be an effective avenue to enable rehabilitation success in patients with CLBP and depressive symptoms and prevent further development of chronicity in this high-risk subpopulation.
Acknowledgments
This study was sponsored by the German Pension Insurance Company Oldenburg-Bremen.
References
- 1.Andersson G. Epidemiological features of chronic low-back pain. Lancet. 1999;354:581–585. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 2.Bendix AF, Bendix T, Haestrup C, Busch E. A prospective, randomized 5-year follow-up study of functional restoration in chronic low back pain patients. Eur Spine J. 1998;7:111–119. doi: 10.1007/s005860050040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buchner M, Neubauer E, Zahlten-Hingurange A, Schiltenwolf M. The influence of the grade of chronicity on the outcome of multidisciplinary therapy for chronic low back pain. Spine. 2007;32:3060–3066. doi: 10.1097/BRS.0b013e31815cde5a. [DOI] [PubMed] [Google Scholar]
- 4.Bullinger M, Kirchberger I. SF-36 Fragebogen zum Gesundheitszustand. SF-12 Kurzversion des SF-36 [SF-12. German short version of the SF-36] Göttingen: Hogrefe; 1998. [Google Scholar]
- 5.Cohen J. Statistical power for the behavioural sciences. New York: Academic Press; 1977. [Google Scholar]
- 6.Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain-associated depression: antecedent or consequence of chronic pain? A review. Clin J Pain. 1997;13:116–137. doi: 10.1097/00002508-199706000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Flor H, Fydrich T, Turk DC. Efficacy of multidisciplinary pain treatment centers: a meta-analysis review. Pain. 1992;49:221–230. doi: 10.1016/0304-3959(92)90145-2. [DOI] [PubMed] [Google Scholar]
- 8.Flor H, Turk DC. Chronic back pain and rheumatoid arthritis: predicting pain and disability from cognitive variables. J Behav Med. 1988;11:251–265. doi: 10.1007/BF00844431. [DOI] [PubMed] [Google Scholar]
- 9.Franke G. SCL-90-R . Die Symptom Checkliste von Derogatis—Deutsche Version [the symptom checklist—German version] Göttingen: Beltz; 1995. [Google Scholar]
- 10.Gatchel RJ. Comorbidity of chronic pain and mental health disorders: the biopsychosocial perspective. Am Psychol. 2004;59:795–805. doi: 10.1037/0003-066X.59.8.795. [DOI] [PubMed] [Google Scholar]
- 11.Gatchel RJ, Rollings KH. Evidence-informed management of chronic back pain with cognitive behavioral therapy. Spine J. 2008;8:40–44. doi: 10.1016/j.spinee.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gerbershagen HU. Das Mainzer Stadienkonzept des Schmerzes [Mainz Pain Staging System] In: Klingler D, Morawetz R, Thoden U, Zimmermann M, editors. Antidepressiva als Analgetika. Wien: Arachne; 1996. pp. 71–95. [Google Scholar]
- 13.Gerbershagen HJ, Özgur E, Straub K, Dagtekin O, Gerbershagen K, Petzke F, Heidenreich A, Lehmann KA, Sabatowski R. Prevalence, severity, and chronicity of pain and general health-related quality of life in patients with localized prostate cancer. Eur J Pain. 2008;12:339–350. doi: 10.1016/j.ejpain.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 14.Guzmán J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ. 2001;322:1511–1516. doi: 10.1136/bmj.322.7301.1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hampel P, Moergel M. Schmerzchronifizierung bei Rückenschmerzpatienten in der stationären Rehabilitation—Zur Validität des Mainzer Stadienmodells der Schmerzchronifizierung [staging of pain among patients with chronic low back pain in the inpatient rehabilitation—validity of the Mainz Pain Staging System] Schmerz. 2009;23:154–165. doi: 10.1007/s00482-008-0743-8. [DOI] [PubMed] [Google Scholar]
- 16.Hautzinger M, Bailer M. Allgemeine Depressionsskala (ADS). Die deutsche Version des CES-D. Manual [German version of the CES-D] Weinheim: Beltz Test; 1993. [Google Scholar]
- 17.Herrmann-Lingen CH, Buss U, Snaith RP. HADS-D Hospital anxiety and depression scale—Deutsche Version [HADS-D Hospital anxiety and depression scale—German version] 2. Bern: Huber; 2005. [Google Scholar]
- 18.Jensen IB, Bergström G, Ljungquist T, Bodin L. A 3-year follow-up of a multidisciplinary rehabilitation programme for back and neck pain. Pain. 2005;115:273–283. doi: 10.1016/j.pain.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 19.Jensen IB, Bergström G, Ljungquist T, Bodin L, Nygren AL. A randomized controlled component analysis of a behavioral medicine rehabilitation program for chronic spinal pain: are the effects dependent on gender? Pain. 2001;91:65–78. doi: 10.1016/S0304-3959(00)00420-6. [DOI] [PubMed] [Google Scholar]
- 20.Koleck M, Mazaux JM, Rascle N, Bruchon-Schweitzer M. Psycho-social factors and coping strategies as predictors of chronic evolution and quality of life in patients with low back pain: a prospective study. Eur J Pain. 2006;10:1–11. doi: 10.1016/j.ejpain.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 21.Linton SJ. A review of psychological risk factors in back and neck pain. Spine. 2000;25:1148–1156. doi: 10.1097/00007632-200005010-00017. [DOI] [PubMed] [Google Scholar]
- 22.Magni G, Moreschi C, Rigatti-Luchini S, Mersky H. Prospective study on the relationship between depression symptoms and chronic musculoskeletal pain. Pain. 1994;56:289–297. doi: 10.1016/0304-3959(94)90167-8. [DOI] [PubMed] [Google Scholar]
- 23.Mohr B, Gräf T, Forster M, Krohn-Grimberghe B, Kurzeja R, Mantel F, Thomsen M, Hampel P. Der Einfluss von Depressivität und Geschlecht auf den Rehabilitationserfolg bei chronischem Rückenschmerz [Influence of depressive symptoms and gender in chronic low back pain rehabilitation outcome: a pilot study] Rehabilitation. 2008;47:284–298. doi: 10.1055/s-2008-1076708. [DOI] [PubMed] [Google Scholar]
- 24.Morley S, Ecclestone C, Williams A. Systematic review and meta-analysis of randomized controlled trials of cognitive behavior therapy and behavior therapy for chronic pain in adults, excluding headache. Pain. 1999;80:1–13. doi: 10.1016/S0304-3959(98)00255-3. [DOI] [PubMed] [Google Scholar]
- 25.Ostelo RWJG, van Tulder MW, Vlaeyen JWS, Linton SJ, Morley SJ, Assendelft WJJ (2008) Behavioural treatment for chronic low-back pain (Review). The Cochrane Library (2):CD002014. doi:10.1002/14651858.CD002014.pub2 [DOI] [PubMed]
- 26.Patrick LE, Altmaier EM, Found E. Long-term outcomes in multidisciplinary treatment of chronic low back pain. Results of a 13-year follow-up. Spine. 2004;29:850–855. doi: 10.1097/00007632-200404150-00006. [DOI] [PubMed] [Google Scholar]
- 27.Pfingsten M, Hildebrandt J, Leibing E, Franz C, Saur P. Effectiveness of a multimodal treatment program for chronic low-back pain. Pain. 1997;73:77–85. doi: 10.1016/S0304-3959(97)00083-3. [DOI] [PubMed] [Google Scholar]
- 28.Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine. 2002;27:109–120. doi: 10.1097/00007632-200203010-00017. [DOI] [PubMed] [Google Scholar]
- 29.Scascighini L, Toma V, Dober-Spielmann S, Sprott H. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatol. 2008;47:670–678. doi: 10.1093/rheumatology/ken021. [DOI] [PubMed] [Google Scholar]
- 30.Spinhoven P, ter Kuile M, Kole-Snijders AMJ, Hutten Mansfeld M, den Ouden DJ, Vlaeyen JWS. Catastrophizing and internal pain control as mediators of outcome in the multidisciplinary treatment of chronic low back pain. Eur J Pain. 2004;8:211–219. doi: 10.1016/j.ejpain.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 31.Sullivan MJ, Ressor K, Mikail S, Fisher R. The treatment in chronic low back pain: review and recommendations. Pain. 1992;50:5–13. doi: 10.1016/0304-3959(92)90107-M. [DOI] [PubMed] [Google Scholar]
- 32.Teuber N, Thiele A, Eberhardt B. Geschlechtsrolle und Schmerzerleben [A questionnaire study of the relationship between gender and chronic pain] Schmerz. 2006;20:307–313. doi: 10.1007/s00482-005-0436-5. [DOI] [PubMed] [Google Scholar]
- 33.Turk DC, Flor H. Etiological theories and treatments for chronic back pain. II: psychological models and interventions. Pain. 1984;19:209–233. doi: 10.1016/0304-3959(84)90001-0. [DOI] [PubMed] [Google Scholar]
- 34.Turk DS, Dworkin RH, Allen RR, Bellamy N, Brandenburg N, Carr DB, Cleeland C, Dionne R. Core outcome domains for chronic pain clinical trials: IMMPACT recommendations. Pain. 2003;106:337–345. doi: 10.1016/j.pain.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 35.van der Hulst M, Vollenbroek-Hutten MMR, Ijzerman MJ. A systematic review of sociodemographic, physical, and psychological predictors of multidisciplinary rehabilitation or, back school treatment outcome in patients with chronic low back pain. Spine. 2005;30:813–825. doi: 10.1097/01.brs.0000157414.47713.78. [DOI] [PubMed] [Google Scholar]
- 36.van der Roer N, van Tulder MW, Barendse J, Knol D, van Mechelen W, de Vet H. Intensive group training protocol versus guideline physiotherapy for patients with chronic low back pain: a randomised controlled trial. Eur Spine J. 2008;17:1193–1200. doi: 10.1007/s00586-008-0718-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van Tulder MW, Koes B, Malmvaara A. Outcome of non-invasive treatment modalities on back pain. An evidence-based review. Eur Spine J. 2006;15:S64–S81. doi: 10.1007/s00586-005-1048-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Tulder MW, Koes BW, Bouter LM. A cost-of-illness study of back pain in the Netherlands. Pain. 1995;62:233–240. doi: 10.1016/0304-3959(94)00272-G. [DOI] [PubMed] [Google Scholar]
- 39.van Tulder MW, Ostelo R, Vlaeyen JWS, Linton SJ, Morley SJ, Assendelft WJJ. Behavioral treatment for chronic low back pain. A systematic review within the framework of the Cochrane Back Review Group. Spine. 2000;26:270–281. doi: 10.1097/00007632-200102010-00012. [DOI] [PubMed] [Google Scholar]
- 40.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A fear-avoidance beliefs questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low-back pain and disability. Pain. 1993;52:157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 41.Watson PJ, Booker CK, Moores L, Main CJ. Returning the chronically unemployed with low back pain to employment. Eur J Pain. 2004;8:359–369. doi: 10.1016/j.ejpain.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 42.Wenig CM, Schmidt CO, Kohlmann T, Schweikert B. Costs of back pain in Germany. Eur J Pain. 2009;13:280–286. doi: 10.1016/j.ejpain.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 43.Wessels T, van Tulder M, Sigl T, Ewert T, Limm H, Stucki G. What predicts outcome in non-operative treatments of chronic low back pain? A systematic review. Eur Spine J. 2006;15:1633–1644. doi: 10.1007/s00586-006-0073-4. [DOI] [PubMed] [Google Scholar]