Abstract
Superiority of pedicle screws over hybrid/hook instrumentation or vice versa in the treatment of Lenke Type 1 and 2 adolescent idiopathic scoliosis (AIS) remains unresolved for moderate curves. Our objective was therefore to compare the assessment of pedicle screw and hybrid/hooks instrumentation with special attention to cosmesis and uninstrumented spine using novel assessment methods. We carried out a retrospective study of radiographs and clinical photos of 40 cases of thoracic AIS between 40° and 70° of Cobb angle Lenke Type 1 and 2, treated with either pedicle screws or hybrid/hooks. The cases were subjectively assessed by four spine surgeons (SRS Travelling Fellows) for radiographic and operative cosmetic result, shoulder balance, trunk shift, rib hump, and waist asymmetry. Instrumentation in the radiographs was obscured with only the non-instrumented part visible, and the surgeons were asked to guess the instrumentation being used. Eighty photographs of patients before and after surgery were assessed for cosmesis by ten non-medical judges for overall cosmetic score, shoulder balance, waist asymmetry, and shoulder blade prominence. Objective assessment of radiographs and clinical photos was performed for Cobb angle of instrumented and non-instrumented spine, global coronal and sagittal balance, number of unfused vertebrae, disc angulation, tilt of last instrumented vertebra, shoulder balance, waist asymmetry, rib prominence, and percent correction. SRS-24 questionnaire was used to measure health-related quality of life in patients. Subjective assessments by surgeons and non-medical judges showed no significant difference by instrumentation (P ≥ 0.05) for all variables. Out of the 160 guesses by surgeons of the cases with instrumentation blocked in the radiographs, they were unable to guess the instrumentation in 92% of the cases. Objective assessment of all variables and SRS-24 scores of all five domains showed no significant difference by instrumentation (P ≥ 0.05). In this first-ever conducted study in a blinded-fashion, we conclude that there is no significant difference between the pedicle screw and hybrid/hooks instrumentations used to treat AIS for Lenke Type 1 and 2 curves for moderate curves between 40° and 70°.
Keywords: Adolescent idiopathic scoliosis, Pedicle screws, Hybrid/hooks, Treatment outcomes for spine surgery
Introduction
There is today no consensus on the preferred instrumentation technique to use for the treatment of adolescent idiopathic scoliosis (AIS). In the last century, there have been several iterations in the corrective methods of progressive curves in AIS from non-segmental rod systems, to segmental hook fixation, to most recent all pedicle screw fixation. The use of hook instrumentation developed by Cotrel-Dubousset (CD) has long been considered gold standard for the treatment of AIS [26]. However, in 1995, Suk et al. [28] introduced the concept of using all pedicle screw instrumentation in AIS, which was originally developed for spinal trauma and tumors [30]. In the 2000s, there has been a surge in the use of pedicle screw instrumentation based in part by the reported advantages of pedicle screws in terms of enhanced correction and stabilization of spine [3, 9, 10, 19, 27, 29]. However, there have been conflicting reports in literature on the use of pedicle screws in spine surgery [18, 19, 21, 23, 25, 26]. Pedicle screw instrumentation could be technically demanding especially in AIS because of the small size of the pedicles and the proximity of the spinal cord in the concavity of the curve [18]. Although some studies have reported acceptable accuracy in placing screws without any neurological complication [18, 30] other studies found a rate of 10% of patients with misplaced pedicle screws [14].
Recent studies that compared pedicle screw instrumentation with hybrid type of fixation have reported significantly better results with all pedicle screw constructs [11–13, 16]. The higher cost of all pedicle screws however remains a concern. Storer et al. [26] in their study comparing pedicle screw and hybrid constructs reported that surgery using either constructs effectively corrects AIS. In addition, they stated that the extra expense incurred with pedicle screws may not be justified in the light of the fact that there is no significant difference in curve correction between the two constructs. Similar views were expressed by Winter et al. [33]. From our own training and experience, from Harrington instrumentation to Luque, CD, CD-like instrumentation followed by hybrid and more recently all pedicle screw constructs, our clinical impression has been that surgery with either constructs gave effective results. We also found that more implants did not necessarily provide better surgical outcomes in treating AIS. Similar observations were made by other researchers who reported that over correction of the main thoracic curve led to either a left shoulder elevation or a left coronal imbalance with maximum correction [1].
It is important to mention that all the comparative studies pertaining to pedicle screws and hybrids/hooks focused on the surgical correction of Cobb angle. Cobb angle is itself limited as it is a single-plane measure of spinal alignment [24]. However, spine surgeons continue to focus on percent correction of the Cobb angle, which so far has no scientific evidence to be considered as “better end result” [33]. Moreover, in our own experience over 15 years in AIS surgery, it has increasingly become clear that the surgical result should be judged not on the instrumented spine, but on the non-instrumented mobile spine, as the former is not functional anymore. This opinion is shared by many deformities surgeons [4, 5, 8, 15]. In addition, the number of fused vertebra, the overall balance of the spine, the alignment of the unfused spine, cosmesis, and patient satisfaction should also be taken into consideration [2].
To appropriately address clinical outcomes or effects of the surgical treatments, various aspects of outcome assessment should be considered. The major objective of this study therefore, is to compare all pedicle screw constructs with hybrid/hook instrumentation for radiographic and cosmesis outcomes for AIS run of the mill cases (40–70°) of Lenke Type 1 and 2, using novel outcome assessment methods.
Methods
Study design
This is a retrospective comparative outcomes study of prospectively collected surgical cases of AIS. We compared surgical outcomes of patients with thoracic idiopathic scoliosis of Lenke Type 1 and 2, treated with pedicle screw and hybrid/hooks instrumentation using novel assessment methods.
Study participants
Cases for this study were obtained from our online electronic database of surgical cases of AIS Scolisoft®. The following query was used: Age above 10 years, right thoracic AIS Lenke Type 1 and 2; Cobb angle 40–70°; underwent posterior surgery alone. This returned 52 cases. We discarded 12 cases that had poor documentation such as missing clinical photograph, missing one x-rays such as side bending or lateral x-rays and or intermediate cases between hybrid and all pedicle screw. Cases where we did not have a minimum of 6 months follow-up of complete iconographic documentation were not included. We were therefore left with two groups of 20 patients.
Pedicle screw instrumentation (Fig. 1) is defined as a construct having each individual vertebra instrumented with at least one pedicle screw (to the exception of one or two vertebrae). Hybrid instrumentation is defined as constructs instrumented with pedicle screws for the bottom of the construct, and pedicle or laminar hooks above in the thoracic spine (Fig. 2).
Fig. 1.

Sample radiograph of pedicle screw instrumentation
Fig. 2.
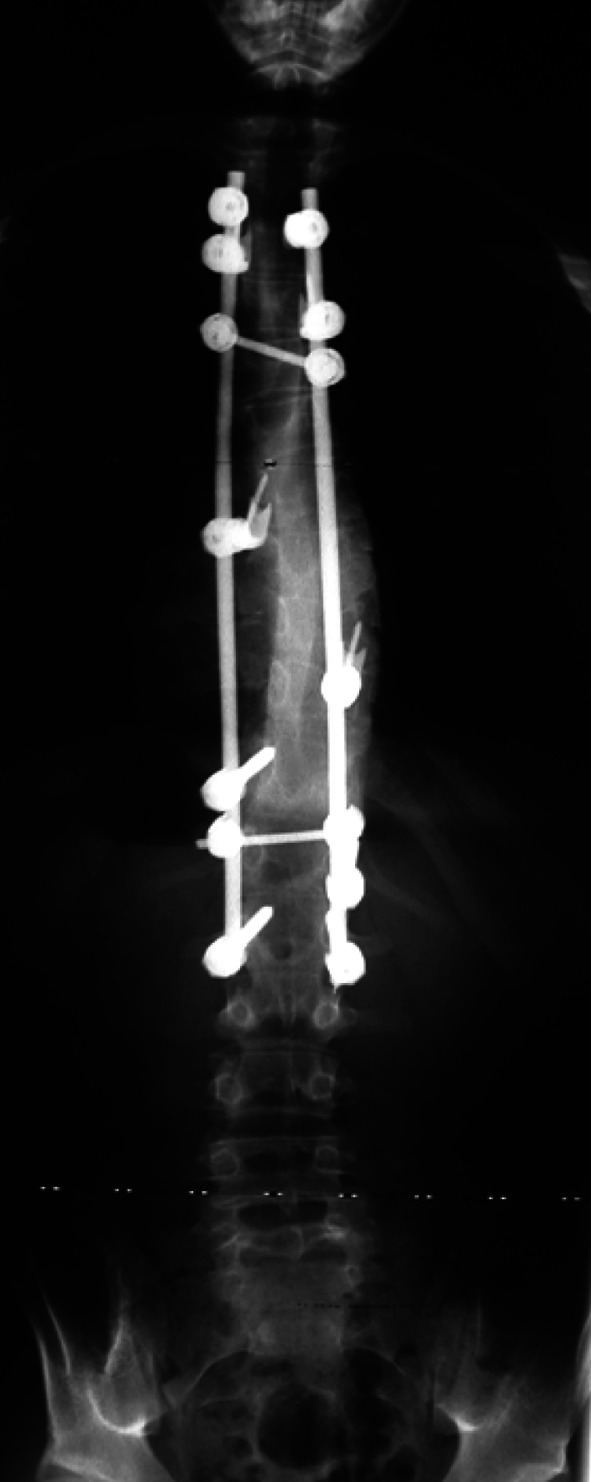
Sample radiographs of hybrid/hooks instrumentation
Case assessments
Cases were subjectively assessed by:
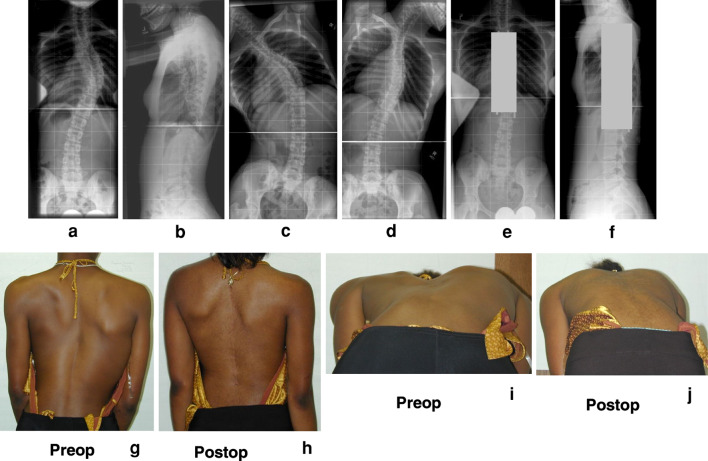
Four spinal deformity surgeons (Scoliosis Research Society Travelling Fellows) who were not involved in the surgical treatment of any of the cases in this study. The surgeons were given standing coronal and sagittal plane radiographs of each case taken before and after surgery along with preoperative right and left side bending films; and clinical photographs of posterior and rib views before and after surgery (Fig. 3). Variables assessed on x-rays and clinical photographs respectively were: overall radiographic result, radiographic result of unfused spine, operative cosmetic results, shoulder balance, trunk shift, rib hump, and waist asymmetry. The surgeons were asked to score these variables on a scale of 1–10. The instrumented part of the spine was obscured by blocking it on the postoperative coronal and sagittal radiographs using Microsoft Paint Program (version 5.1., Microsoft, WA, USA). The surgeons were asked to guess the instrumentation type used in the blocked radiographs (Fig. 3e, f).
Ten non-medical judges who volunteered to participate in the study to perform the assessments were asked to rate cosmesis in patient photographs taken before and after surgery for each patient. The judges included lay persons from different professions, education level, economic status, gender, and race. They were in no way involved in any aspect of spine treatment of the cases used in this study and none of them had a medical background. They were educated in detail about normal and scoliotic back with the help of a diagram of scoliosis back, along with photographs of a typical scoliosis patient. The photographs were thoroughly shuffled so that the scoring of the post surgery photographs are not influenced by the pre surgery and vice versa (Fig. 4). Study coordinator spent 20 min with each non-medical judge to educate them in detail about the study and the variables to be assessed. The non-medical judges were told not to consider the postoperative scars on the back for overall cosmetic scoring. Variables assessed by non-medical judges include, overall cosmetic score, shoulder balance, overall balance, waist asymmetry, and shoulder blade prominence. All scoring by non-medical judges was done on a scale of 0–10 (0 = worst, 10 = excellent).
Fig. 3.
Sample portfolio of a case consisting of radiographs and clinical photographs of patients before and after surgery of patients instrumented with hybrid/hooks or pedicle screws, which were given to spinal deformity surgeons for evaluation. a Anterior–posterior (AP) view radiograph before surgery. b Sagittal view radiographs before surgery. c Left side bending radiograph. d Right side bending radiograph. e AP view radiograph after surgery with instrumentation blocked. f Sagittal view radiograph after surgery with instrumentation blocked. g Posterior view clinical photo of patient before surgery. h Posterior view clinical photo of patient after surgery. i Rib view of patient before surgery. j Rib view of patient after surgery
Fig. 4.
Sample of clinical photographs of patients before and after surgery with pedicle screw or hybrid/hook instrumentation that were given to non-medical judges to rate on a scale of 0–10. These photographs represent 8 of the total 80 given to the judges. Note that the pre and post surgical photographs are not arranged in a contiguous manner, but at random, as given to the non-medical judges
Objective assessment
Objective assessment of radiographs and photographs was done by a Spine Fellow who was not involved in any of the surgeries performed on the cases used in this study. Variables assessed include: Radiographic: Cobb angle measurement of the spine before and after surgery (in degrees), Cobb angle of instrumented and uninstrumented spine (in degrees), number of fused vertebrae, global coronal balance (mm), global sagittal balance (mm), tilt of last vertebra (LIV) (in degrees), and disc angulation (in degrees); Cosmesis: trunk shift (mm), shoulder balance (mm), waist line asymmetry (mm), and rib prominence (in degrees).
Health-related quality of life
Health-related quality of life (HRQOL) was assessed with SRS-24 questionnaire. The SRS-24 scores from the two instrumentation groups were compared for overall score and for the five domains (pain, function, self-esteem, mental health, and satisfaction).
Statistical analysis
Data was analyzed using the SPSS (version 15.0, SAS Institute Inc., Cary, NC, USA). Distribution of variables is given as mean, standard deviation and ranges.
Paired sample t test was done to study the difference in the mean values for each variable between pre and post surgery scores. Analysis of variance (ANOVA) was used to find differences in all the variables assessed between the two instrumentation types. Statistical significance was set at P < 0.05.
Results
The study sample consisted of 40 patients (20 pedicle screw group—Group 1; 20 hybrid group—Group 2). Both groups had very similar characteristics: There were in total 32 females and 8 males, with a mean age of 14.6 (11.0–29.0) [mean age in Group 1 was 15.0 years (12.0–29.0 years) and Group 2 was 14.2 years (11.0–22.0 years)]. Percentage of females to males in Group 1 was 73.7 vs 26.4%, and 78.6 vs 21.4% in Group 2. Both the groups had both Lenke Type 1 and 2 cases. Group 1 had 18 cases of Lenke Type 1 and two of Lenke Type 2. Group 2 had 15 cases of Lenke Type 1 and 5 cases of Lenke Type 2 cases. The mean Cobb angle in Group 1 was 49° and in Group 2, 53.0°. Mean side bending angle was for the Group 1 27.8 ± 12.7° and for the Group 2 31.2 ± 14.1°. The average follow-up of our cases was 1.7 years (range 6 months to 7 years). Both groups had similar number of vertebrae fused (10.4 for Group 1 and 10.1 numbers of fused vertebrae for Group 2). All surgeries had been performed by senior spinal deformity surgeons not involved in the assessment.
Medical experts subjective assessment
Seven outcome variables (overall radiographic result, radiographic result of unfused spine, operative cosmetic results, shoulder balance, trunk shift, rib hump, and waist asymmetry) were subjectively assessed by four spinal deformity surgeons. Table 1 shows the mean, standard deviation and range values of the seven variables along with ANOVA results (P value). Subjective assessment by medical experts showed that there is a significant inter observer variability in their scoring for all the variables assessed (>0.01) except operative cosmetic result (P = 0.146). This indicates that the spine surgeons agree with each other on the operative cosmetic results.
Table 1.
Results of assessment by medical experts
| Outcome | Pedicle screw—Group 1 | Hybrid—Group 2 | P value (ANOVA by procedure) | P value (ANOVA by judge–interobserver agreement) |
|---|---|---|---|---|
| Radiographic result | 7.0 ± 1.48 | 7.6 ± 1.5 | 0.724* | <0.01 |
| Unfused spine | 7.05 ± 1.5 | 7.3 ± 1.4 | 0.983* | <0.01 |
| Operative cosmetic result | 7.35 ± 1.3 | 7.95 ± 1.3 | 0.573* | 0.146* |
| Shoulder balance | 7.15 ± 1.5 | 7.7 ± 1.5 | 0.478* | <0.01 |
| Trunk shift | 7.4 ± 1.5 | 8.2 ± 1.2 | 0.541* | <0.01 |
| Rib hump | 6.4 ± 1.9 | 6.1 ± 3.5 | 0.609* | <0.01 |
| Waist asymmetry | 7.2 ± 1.3 | 7.7 ± 1.37 | 0.746* | <0.01 |
* Non-significant: In the case of interobserver agreement, non-significant (P = 0.146) indicates that there is an agreement between the judges on the operative cosmetic result
Analysis of variance by instrumentation type of the seven variables showed no significant difference between the two procedures (P ≥ 0.05). Overall, statistical analysis showed that the medical experts were not able to discriminate between the two instrumentation types through their subjective evaluations of any of the seven variables.
Guessing of instrumentation type by medical experts
Out of 160 guesses of the type of instrumentation used for the cases, the medical experts could not guess the instrumentation 74% of the times, made incorrect guesses 18% of the time and correct guesses, only 8% of the times. Total percentage that the judges could not guess or made the wrong guess as to the type of instrumentation was 92%.
Non-medical subjective assessment
Paired sample t test showed significant difference between pre and post surgery scores for all variables (Table 2) for both types of instrumentations. This indicates that the non-medical judges were able to perceive the change after surgery in all variables assessed despite the fact that the pre and post surgery clinical photos were given completely shuffled to the judges for scoring. Based on the mean values of the pre and post surgery scores for all variables assessed, there is in general an improvement with treatment with both types of instrumentation (between 1.4 and 2.4 difference on the scale 1–10). ANOVA showed significant inter-rater variability in scoring for all variables (P ≤ 0.01). However, ANOVA of the scores by instrumentation type did not show statistically significant difference for any of the variables, except shoulder balance before surgery (P = 0.006). However, post surgically, there is not significant difference between the two instrumentation types for shoulder balance (P = 0.171). Overall, statistical analysis showed that non-medical judges who reviewed 80 clinical photographs each were unable to discriminate between the two instrumentation types through any of the variables.
Table 2.
Results of ANOVA of subjective scores by non-medical judges by procedure
| Outcome | Pedicle screw—Group 1 | Hybrid—Group 2 | P value ANOVA by procedure | P value of paired t test comparing pre and post scores | |||
|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | ||
| Overall cosmetic score | 5.4 ± 1.6 | 7.8 ± 1.2 | 5.5 ± 1.9 | 7.6 ± 1.2 | 0.643* | 0.148* | <0.01 |
| Shoulder balance | 6.3 ± 1.7 | 7.6 ± 1.63 | 5.8 ± 2.0 | 7.4 ± 1.6 | 0.009 | 0.189* | <0.01 |
| Overall balance | 5.4 ± 1.7 | 7.4 ± 1.5 | 5.1 ± 2.0 | 7.5 ± 1.5 | 0.197* | 0.722* | <0.01 |
| Waistline asymmetry | 5.4 ± 1.8 | 7.3 ± 1.7 | 5.3 ± 2.0 | 7.3 ± 1.6 | 0.513* | 0.908* | <0.01 |
| Shoulder blade prominence | 5.2 ± 1.8 | 7.3 ± 1.7 | 4.9 ± 2.1 | 7.0 ± 1.6 | 0.056* | 0.075* | <0.01 |
* No statistically significant difference
Objective assessment of spinal deformity variables
Paired sample t test showed that there was a significant difference between all deformity variables for both groups before and after surgery. However, there was no difference in any of the variables studied between the two groups by procedure (Table 3).
Table 3.
Results of objective assessment
| Outcome | Pedicle screw—Group 1 (mean/SD) | Hybrid/hooks—Group 2 (mean/SD) | P value ANOVA by procedure |
|---|---|---|---|
| Global coronal balance (post) (mm) | 3.8 ± 3.4 | 3.0 ± 2.7 | 0.417* |
| Global sagittal balance (post) mm | 7.6 ± 5.0 | 11.5 ± 7.6 | 0.06* |
| Tilt LIV (degrees) | 5.05 ± 5.2 | 3.7 ± 0.8 | 0.34* |
| # Unfused vertebra | 3.6 ± 0.94 | 3.7 ± 0.8 | 0.72* |
| Disc angulation (degrees) | 2.4 ± 3.7 | 4.2 ± 4.2 | 0.15* |
| Trunk shift (mm) | |||
| Pre | 2.4 ± 1.82 | 3.9 ± 2.9 | 0.06* |
| Post | 1.3 ± 1.5 | 1.9 ± 1.8 | 0.2* |
| Cobb angle thoracic (degrees) | |||
| Pre | 49.3 ± 8.7 | 52.3 ± 9.8 | 0.18* |
| Post | 14.2 ± 6.7 | 12.7 ± 8.6 | 0.53* |
| Cobb angle lumbar (degrees) | |||
| Pre | 30 ± 7.4 | 32.6 ± 10.5 | 0.36* |
| Post | 8.3 ± 7.3 | 9.3 ± 7.9 | 0.66* |
| Shoulder balance (ratio: right and left shoulder) | |||
| Pre | 0.09 ± 0.17 | 0.15 ± 0.13 | 0.20* |
| Post | 0.01 ± 0.12 | 0.10 ± 0.14 | 0.94* |
| Waist asymmetry (ratio: right and left) | |||
| Pre | 0.06 ± 0.42 | 0.14 ± 0.5 | 0.22* |
| Post | 0.16 ± 0.34 | 0.03 ± 0.5 | 0.61* |
| Rib prominence (degrees) | |||
| Pre | 9.6 ± 3.4 | 7.47 ± 5.1 | 0.39* |
| Post | 7.6 ± 3.0 | 7.35 ± 4.5 | 0.37* |
* No statistical significance
SRS-24 scores
SRS-24 scores analysis showed no significant difference between pedicle screw group and hybrid/hook group for any of the domains: function (4.3 vs 4.2; P = 0.54); pain (4.6 vs 4.1; P = 0.50); self image (4.5 vs 4.4; P = 0.140); mental health (4.6 vs 4.0; P = 0.56); satisfaction (4.7 vs 4.5; P = 0.22).
Discussion
The etymological meaning of orthopedics derives from Greek: Ortho = straight, paedics = children. Therefore, intuitively in spine surgery, we have labored under the assumption that straighter is better. To achieve a straight spine in AIS, there have been several efforts through development of surgical techniques and implants. In the process, it was assumed that more the number of implants used in the surgical treatment, the better for achieving a straight spine. However, so far this has not been demonstrated to translate into improved outcomes. In the 2000s, one of the implants that has gained popularity among spine surgeons in the treatment of AIS is the pedicle screw over the established hook or hybrid system. This is based on the reported advantages of enhanced correction and stabilization of the spine with pedicle screws. However, in a recent evidence-based evaluation of literature on pedicle screw constructs in the treatment of AIS, Mulpuri et al. [21] reported weak evidence to show that the pedicle screw constructs are superior in improving curve correction and stabilization of the curve. Moreover, the evidence regarding advantage of all pedicle screw constructs remains limited to case series, biomechanical studies and expert opinions [21].
Assessment of outcome of surgery on cases of AIS can be looked at in three different ways: First, from the cosmesis point of view. Cosmesis by definition is preservation, restoration, and enhancement of appearance and surgery for idiopathic scoliosis is in part considered an operation with cosmetic implications [22]. In fact, in a recent study on the importance of physical deformity in AIS, severity of the deformity was found to be the most important clinical consideration for surgical treatment [7]. In the present study cosmesis was evaluated through subjective evaluations by medical experts and non-medical judges of cosmetic appearance in clinical photographs taken before and after surgery. Although cosmesis is a spectrum with wide inter-rater variability, our study showed that overall, neither the medical nor non-medical judges could differentiate between pedicle screw and hybrid instrumentation in their evaluation of cosmesis in this study.
Second, from the classic radiographic approach, which employs measuring variables such as Cobb angle correction, apical vertebral translation, and tilt of last instrumented vertebra. Using these variables, it has been statistically demonstrated in some studies that thoracic pedicle screw instrumentation provides better Cobb angle correction than hybrid/hook instrumentation. [16, 17, 27, 29]. Other studies including the present one did not obtain similar results [20, 26, 32]. The discrepancy in the results may have to do with series that dealt with bigger and stiffer curves and due to the different philosophies in curve correction held by spine surgeons.
Obviously comparison of two different techniques (hybrid/pedicle screw) done by the same surgeon may give different results especially if the goal is to maximize Cobb angle correction. In the present study, we looked at run of the mill cases (40–70° curves) of AIS Lenke Type 1 and 2 with average Cobb angle of 50°. Objective assessment in our study showed that there is no statistically significant difference between the two instrumentation for all variables assessed. Other studies looking at stiffer curves of more than 70° have shown the superiority of pedicle screw fixation in terms of correction [6], that obviates the need of anterior release in most cases.
Lastly, we employed HRQOL assessments to evaluate surgical outcomes, as more recent studies on the treatment of AIS focused on patient-related outcomes like SRS-24 HRQOL questionnaire responses in addition to objective variables to define successful outcome [31]. To date, no study has shown that there is any statistically significant difference in the SRS-24 scores between hybrid/hooks and all pedicle screw instrumentation [13, 21]. Our study similarly did not show any significant difference between the two instrumentations for any of the domains.
In addition, the present study employed novel outcome assessment methods whereby spine surgeons blinded to the type of instrumentation used judged not only the effect of procedure on the non-instrumented part, but overall cosmetic effect as well. We thought that if we were to ask the judges to view the cases knowing what type of instrumentation used, they would probably introduce bias in their judgment. Also, our study focused on the non-instrumented part of the spine that remains functional and is important throughout follow-up. Hence, the fate of the non-instrumented part of the spine and overall balance of the patient should be more important for the spine surgeon than the strict Cobb angle correction. Assessment of non-instrumented part of the spine in this study showed no significant difference between the two procedures, and this is the first study to our knowledge to look at the outcome of surgery from this angle.
There are several limitations to this study. One major limitation of this study is the minimum 6 months follow-up period that we have used to compare the two groups as opposed to the established minimum of 2 years follow-up. Our mean follow-up is however 1.7 years and previous studies have shown that even at 2 years follow-up, there is no real clinically relevant difference in the correction of the angular parameters between hybrid and pedicle screw constructs [5, 20]. Second limitation is the small sample size in this study for each group. Larger groups of patient may have shown statistical difference between the two groups. However our two groups were very similar in age, curve characteristics, Cobb angle, curve flexibility and numbers of vertebrae being fused, and we purposely looked at the clear cut cases of hybrid and pedicle screw. The lack of difference observed between the two techniques is partly explained by the fact that these curves were all moderate and flexible. Another limitation is related to the fact that these cases have been operated by different spine surgeons and hence a lack of homogeneity in the group treated. All the surgeons were however senior spinal deformity surgeons who had extensive experience in both techniques. At last, it was not possible to track back the type of rods that had been used (flexible or stiff rod) as well as the type of correction maneuver that had been used for correction (rod rotation vs translation, vs cantilever). However for these moderate curves we do not think it is as important as for larger and stiffer curve. The focus and goal of our study was to report and demonstrate the use of novel subjective assessment methods of surgical outcomes in AIS that is totally blinded.
Conclusion
In this first ever conducted study in a blinded fashion using novel assessment methods, we found no difference in the functional, patient-related, and cosmetic assessment when treating AIS of Lenke Type 1 and 2 moderate curves between 40° and 70° with either hybrid/hooks or pedicle screw instrumentation. Economic and safety factors may have a role in deciding one instrumentation over the other in view of such equivalent assessment.
Acknowledgement
This study was funded by a research grant from Synthes Spine.
Contributor Information
Vincent Arlet, Phone: +1-434-2430266, Email: va3e@hscmail.mcc.virginia.edu.
Jean Albert Ouellet, Phone: +1-514-4124464, FAX: +1-514-4124353, Email: jaouellet@hotmail.com.
Jeffrey Shilt, Phone: +1-208-3678506, Email: jeffshilt@sarmc.org.
Francis H. Shen, Phone: +1-434-2430291, Email: fhs2q@virginia.edu
Kirkham Wood, Phone: +1-617-7248636, Email: kbwood@partners.org.
Donald Chan, Phone: +1-434-2430266, Email: dc4k@virginia.edu.
John Hicks, Phone: +1-434-2430266, Email: jmh8rc@virginia.edu.
Ernesto Bersusky, Email: ebersusky@arnet.com.ar.
Vasantha Reddi, Phone: +1-434-2435382, FAX: +1-434-2435387, Email: vr8n@virginia.edu.
References
- 1.Arlet V, Marchesi D, Papin P, Aebi M. Decompensation following scoliosis surgery: treatment by decreasing the correction of the main thoracic curve or “letting the spine go”. Eur Spine J. 2000;9(2):156–160. doi: 10.1007/s005860050227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arlet V, Reddi V. Adolescent idiopathic scoliosis: Lenke Type I–VI case studies. Neurosurg Clin N Am. 2007;18(2):1–24. doi: 10.1016/j.nec.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Barr SH, Schuette AM, Emans JB. Lumbar pedicle screws versus hooks. Results in double major curve in adolescent idiopathic scoliosis. Spine. 1997;22(12):1369–1379. doi: 10.1097/00007632-199706150-00016. [DOI] [PubMed] [Google Scholar]
- 4.Betz RR, Harms J, Clements DH, III, et al. Comparison of anterior and posterior instrumentation for correction of adolescent idiopathic scoliosis. Spine. 1997;24:225–239. doi: 10.1097/00007632-199902010-00007. [DOI] [PubMed] [Google Scholar]
- 5.Di Silvestre M, Bakaloudis G, Lolli F, Vommaro F, Martikos K, Parisini P. Posterior fusion only for thoracic adolescent idiopathic scoliosis of more than 80°: pedicle screws versus hybrid instrumentation. Eur Spine J. 2008;17(10):1336–1349. doi: 10.1007/s00586-008-0731-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dobbs MB, Lenke LG, Bridwell KH (2005) Comparison of combined anterior/posterior fusion alone for the treatment of adolescent idiopathic scoliosis curves greater than 90 degrees. Book of abstracts. Scoliosis Research Society 40th annual meeting, October 2005, Miami, pp 44–45
- 7.Donaldson S, Hedden D, Stephens D, Alman B, Howard A, Narayanan U, Wright JG. Surgeon reliability in rating physical deformity in adolescent idiopathic scoliosis. Spine. 2007;32(3):363–367. doi: 10.1097/01.brs.0000253605.71168.2e. [DOI] [PubMed] [Google Scholar]
- 8.Ginsburg HH, Goldstein L, Haake PW et al (1995) Long term study of back pain in postoperative idiopathic scoliosis: longterm follow-up phase IV. Paper presented at Scoliosis Research Society 30th annual meeting, Ashville
- 9.Halm H, Niemeyer T, Link T, Liljenqvist U. Segmental pedicle screw instrumentation in idiopathic thoracic and lumbar scoliosis. Eur Spine J. 2000;9:119–197. doi: 10.1007/s005860000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hamil CL, Lenke LG, Bridwell KH, et al. The use of pedicle screw fixation to improve correction of lumbar spine of patients with idiopathic scoliosis: is it warranted? Spine. 1996;21:1241–1249. doi: 10.1097/00007632-199605150-00020. [DOI] [PubMed] [Google Scholar]
- 11.Karatoprack O, Unay K, Tezer M, Oztuk C, Aydogan M, Mirzanil C. Comparative analysis of pedicle screw versus hybrid instrumentation in adolescent idiopathic scoliosis surgery. Int Orthop. 2008;32(4):523–528. doi: 10.1007/s00264-007-0359-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim YJ, Lenke LH, Bridwell KH, et al. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine. 2004;25(4):415–419. doi: 10.1097/01.brs.0000109983.12113.9b. [DOI] [PubMed] [Google Scholar]
- 13.Kim YJ, Lenke LG, Kim J, Bridwell KH, Cho SK, et al. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2006;31(3):291–298. doi: 10.1097/01.brs.0000197865.20803.d4. [DOI] [PubMed] [Google Scholar]
- 14.Kuklo TR, Potter BK, Lenke LG, Polly DW, Jr, et al. Surgical revision rates of hooks versus hybrid versus screws versus combined anteroposterior spinal fusion for adolescent idiopathic scoliosis. Spine. 2007;16(10):1604–1614. doi: 10.1007/s00586-007-0431-x. [DOI] [PubMed] [Google Scholar]
- 15.Lenke LG, Bridwell KH, Baldus C, et al. Ability of Cotrel-Dubousset instrumentation to preserve distal lumbar segments in adolescent idiopathic scoliosis. J Spinal Disord. 1993;6:339–350. doi: 10.1097/00002517-199306040-00008. [DOI] [PubMed] [Google Scholar]
- 16.Lenke LG, O’Brien MF, Lehman RA, et al. Accuracy and efficacy of thoracic pedicle screws in curves more than 90 degrees. Spine. 2005;30(2):222–226. doi: 10.1097/01.brs.0000150482.26918.d8. [DOI] [PubMed] [Google Scholar]
- 17.Lenke LG, Kuklo TR, Ondra S, David PW. Rationale behind the current state-of-the-art treatment of scoliosis (in the pedicle screw era) Spine. 2008;33(10):1051–1054. doi: 10.1097/BRS.0b013e31816f2865. [DOI] [PubMed] [Google Scholar]
- 18.Liljenqvist U, Allkemper T, Hackenberg L, Link T, Steinbeck J, Halm H. Analysis of the vertebral morpohology in idiopathic scoliosis with magnetic resonance imaging using multiplanar reconstruction. J Bone Joint Surg Am. 2002;84:359–368. doi: 10.2106/00004623-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Liljenqvist U, Lepsien V, Hackenber L, Niemeyer T, Halm H. Comparative analysis of pedicle screws and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J. 2002;11:336–343. doi: 10.1007/s00586-002-0415-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lowenstein JE, Matsumoto H, Vitale MG, et al. Coronal and sagittal plane correction in adolescent idiopathic scoliosis: a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine. 2007;32(4):448–452. doi: 10.1097/01.brs.0000255030.78293.fd. [DOI] [PubMed] [Google Scholar]
- 21.Mulpuri K, Angeliki P, Reilly CW. Evidence-based medicine analysis of all pedicle screw constructs in adolescent idiopathic scoliosis. Spine. 2007;32(19):S109–S114. doi: 10.1097/BRS.0b013e318134eaa3. [DOI] [PubMed] [Google Scholar]
- 22.Negrini S, Grivas TB, Kotuicki T, et al. Why do we treat adolescent idiopathic scoliosis? What we want to obtain, avoid for our patients. SOSORT 2005. Consensus paper. Scoliosis. 2006;1:4. doi: 10.1186/1748-7161-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Papin P, Arlet V, Marchesi D, Rosenblatt B, Aebi M. Unusual presentation of spinal cord compression related to misplaced pedicle screws in thoracic scoliosis. Eur Spine J. 1999;8:156–160. doi: 10.1007/s005860050147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Potter BK, Kuklo TR, Lenke LG. Radiographic outcomes of anterior spinal fusion versus posterior spinal fusion for treatment of Lenke Type 1 adolescent idiopathic scoliosis curves. Spine. 2002;30:1859. doi: 10.1097/01.brs.0000174118.72916.96. [DOI] [PubMed] [Google Scholar]
- 25.Schlenzka D. Reviewer’s comment. Eur Spine J. 1999;8:160. doi: 10.1007/s005860050148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Storer SK, Vitale MG, Hyman J, et al. Correction of adolescent idiopathic scoliosis using thoracic pedicle screw fixation versus hook constructs. J Pediatr Orthop. 2005;25(4):415–419. doi: 10.1097/01.mph.0000165134.38120.87. [DOI] [PubMed] [Google Scholar]
- 27.Suk SI, Lee CK, Min HJ, Cho KH, Oh JH. Comparison of Cotrel-Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop. 1994;18:341–346. doi: 10.1007/BF00187077. [DOI] [PubMed] [Google Scholar]
- 28.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20(12):1399–1405. [PubMed] [Google Scholar]
- 29.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation to improve correction in the lumbar spine of patients with idiopathic scoliosis. Is it warranted? Spine. 1995;21:1241–1249. [Google Scholar]
- 30.Suk SI, Lee SM, Chung ER, Kim JH, Kim SS. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up. Spine. 2005;30(14):102–109. doi: 10.1097/01.brs.0000169452.50705.61. [DOI] [PubMed] [Google Scholar]
- 31.Upasani V, Caltoum C, Potacharapon M, et al. Adolescent idiopathic scoliosis patients report increased pain after five years compared with two years after surgical treatment. Spine. 2008;33(10):1107–1112. doi: 10.1097/BRS.0b013e31816f2849. [DOI] [PubMed] [Google Scholar]
- 32.Vora V, Crawford A, Babekhir N, et al. A pedicle screw construct gives an enhanced posterior correction of adolescent idiopathic scoliosis when compared with other constructs: myth or reality. Spine. 2007;32(17):1869–1874. doi: 10.1097/BRS.0b013e318108b912. [DOI] [PubMed] [Google Scholar]
- 33.Winter RB, Lonstein JE, Denis F. How much correction is enough? Spine. 2007;32(24):2641–2643. doi: 10.1097/BRS.0b013e31815a5207. [DOI] [PubMed] [Google Scholar]