Abstract
The objective of the study was to provide an inventory of predictive instruments and their constituting parameters associated with return to work in patients with subacute (2–10 weeks pain duration) and chronic (10–24 weeks pain duration) non-specific low back pain (NSLBP). Data sources included systematic review in Medline, Embase, Cinahl, Central, PEDro, Psyndex, PsychInfo/PsycLit, and Sociofile up to September 2008, in reference lists of systematic reviews on risk factors, and of included studies. For the systematic review, two reviewers independently assessed study eligibility and quality, and extracted data. Disagreements were resolved by consensus. Risk factors were inventorised and grouped into a somatic and psychosocial domain. 23 studies reporting on subacute and 16 studies reporting on chronic patients were included. The studies on subacute patients reported on a total of 56 biomedical factors out of which 35 (63%) were modifiable and 61 psychosocial factors out of which 51 (84%) were modifiable. The corresponding values in studies on chronic patients were 44 biomedical [27 (62%) modifiable] and 61 [40 (66%) modifiable] respectively. Our data suggest that the interdisciplinary approach in patients at risk to develop persistent NSLBP is justified in both, the subacute and chronic disease stages. Psychosocial interventions might be more effective in subacute stages since a higher proportion of modifiable risk factors were identified in that group.
Keywords: Back pain, Occupational diseases, Return to work, Prognostic indicators, Systematic review
Background
Low-back pain is one of the most important reasons for GP visits in developed countries. In the UK, for example, low-back pain accounts for about 7 million GP visits annually [1]. Whereas the majority of low back pain patients recover without a specific intervention within a few weeks, only about 20% of the affected will remain on sick leave and about half of them will stay on prolonged sick leave or sustained restriction in function [2]. This small proportion of patients with persistent symptoms account for about 80% of the total costs of NSLBP [2].
From a clinical perspective it remains challenging to tailor the most appropriate therapies considering both, clinical outcome and costs. Guidelines suggest that patients at risk for delayed recovery should be identified early and receive a multifaceted therapy considering biological, psychological and social factors [3, 4]. These programmes aim to improve functional restoration and promote return to work. Various studies showed advantage of a biopsychosocial approach compared to an isolated biomedical approach [5, 6]. However, to our knowledge there has been no study investigating to what extent the biopsychosocial approach is superior to a psychosocial approach in patients with chronic NSLBP non-specific low back pain. Arguably, the biopsychosocial approach is only justified if biomedical risk factors still play a major role in patients with delayed recovery. We therefore performed two systematic reviews, one focusing on risk factors of patients with subacute NSLBP, and one focusing on risk factors of patients with chronic NSLBP. We aimed at categorising risk factors into a biomedical and a psychosocial domain and aimed at comparing the proportions in the subacute and chronic stage. The final aim was then to draw a conclusion regarding the usefulness of biomedical interventions in patients with chronic unspecific low back pain.
Methods
Identification of studies
We searched Medline (PubMed Version), Embase (Ovid interface), PsychINFO/PsychLIT, Cinahl, Central, PEDro, Psyndex, Sociofile from inception to October 2008. The full search algorithm is available on request.
In addition, we checked the reference lists of the included publications, relevant systematic reviews, relevant articles on the topic, guidelines, expert reports, and the ‘related articles’ query in Medline. We imposed no language restrictions. Health care professionals with sufficient knowledge of the given language assessed articles in other languages than English, e.g. German, French, Spanish or Italian.
Study selection
An epidemiologist and an information specialist defined the search strategy applying previously published rigorous methods [7]. Two reviewers screened the titles, keywords, and abstracts of all retrieved records. The agreement between reviewers for study selection was good (kappa = 0.73). We looked for prospective cohort studies reporting on biomedical and psychosocial factors related to return to work in patients suffering from subacute (2–10 weeks pain duration) or chronic (10–24 weeks pain duration) NSLBP. In the case of multiple publications on the same study population, all publications were retrieved to gather the most possible information. Two independent evaluators classified each factor as modifiable or not modifiable. In the event of disagreement consensus was reached between evaluators.
Data extraction
One reviewer extracted the salient features from each study using a data extraction form that was pre-tested using one of the included studies. A second reviewer double-checked the extraction form for discrepancies. From each study data regarding setting (e.g., year, country of origin), gender, mean age and number of participants were documented (Table 1).
Table 1.
Summary of the included studies
| Dionne | Dionne | Dionne | Faber | Hagen | Heymans | Heymans | Hunt | Loisel | Lötters | Öhlund | Okurowski | Pransky | Prkachin | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Category | SA | SA | SA | SA | SA | SA | SA | SA | SA | SA | SA | SA | SA | SA |
| Year | 2005 | 2007 | 2007 | 2006 | 2005 | 2006 | 2007 | 2002 | 2002 | 2006 | 1996 | 2003 | 2006 | 2007 |
| Country of origin | Can | Can | Can | Ned | Nor | Ned | Ned | Can | Can | Ned | Swe | USA | USA | USA |
| Number of participants | 1,007 | 369 | 491 | 103 | 257 | 299 | 628 | 192 | 104 | 129 | 101 | 986 | 494 | 192 |
| Gender (% males) | 59 | 0 | 100 | 76 | 52 | 79 | 79 | 73 | 54 | 70 | 70 | 74 | 78 | 72 |
| Mean age | 39 | 39 | 39 | NR | 41 | 40 | 41 | 41 | 40 | 43 | 41 | 36 | 37 | 40 |
| Total number of risk factors | 111 | 111 | 111 | 19 | 30 | 27 | 22 | 17 | 5 | 39 | 5 | 22 | 22 | 11 |
| Not significant | 104 | 104 | 96 | 16 | 21 | 21 | 17 | 15 | 2 | 36 | 1 | 18 | 13 | 7 |
| Significant | 7 | 7 | 15 | 3 | 9 | 6 | 5 | 2 | 3 | 3 | 4 | 4 | 9 | 4 |
| Biomedical modifiable | 2 | 1 | 3 | 1 | 4 | 2 | 1 | 0 | 3 | 2 | 1 | 0 | 1 | 1 |
| Biomedical non-modifiable | 2 | 1 | 5 | 2 | 1 | 0 | 2 | 1 | 0 | 0 | 0 | 1 | 3 | 0 |
| Psychosocial modifiable | 3 | 2 | 4 | 0 | 3 | 4 | 2 | 1 | 0 | 1 | 3 | 3 | 3 | 3 |
| Psychosocial non-modifiable | 0 | 3 | 3 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 |
| Shaw | Schultz | Schultz | Soucy | Truchon | Turner | Turner | Van der Weide | Van der Weide | Weber | Bloch | Bloch | Bloch | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Category | SA | SA | SA | SA | SA | SA | SA | SA | SA | SA | CH | CH | CH |
| Year | 2007 | 2004 | 2005 | 2006 | 2005 | 2006 | 2008 | 1998 | 1998 | 1998 | 2000 | 2000 | 2000 |
| Country of origin | USA | USA | USA | Can | Can | USA | USA | Ned | Ned | Ger | Den | Ger | Isr |
| Number of participants | 140 | 192 | 111 | 437 | 439 | 1,068 | 1,885 | 120 | 59 | 662 | 494 | 295 | 289 |
| Gender (% males) | 100 | 72 | 62 | 57 | 56 | 69 | 68 | 33 | 39 | 67 | 46 | 64 | 74 |
| Mean age | 30 | 40 | 41 | 39 | 39 | 39 | 39 | 39 | 38 | 48 | 41 | 49 | 39 |
| Total number of risk factors | 21 | 49 | 49 | 16 | 12 | 13 | 62 | 19 | 19 | 10 | 43 | 43 | 38 |
| Not significant | 19 | 46 | 47 | 13 | 8 | 11 | 53 | 15 | 16 | 6 | 33 | 35 | 30 |
| Significant | 2 | 3 | 2 | 3 | 4 | 2 | 9 | 4 | 3 | 4 | 10 | 8 | 8 |
| Biomedical modifiable | 2 | 1 | 0 | 0 | 1 | 0 | 5 | 1 | 2 | 1 | 2 | 1 | 1 |
| Biomedical non-modifiable | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 2 | 0 |
| Psychosocial modifiable | 0 | 2 | 2 | 2 | 2 | 2 | 3 | 3 | 1 | 2 | 4 | 3 | 4 |
| Psychosocial non-modifiable | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 3 | 2 | 3 |
| Bloch | Bloch | Bloch | Bradisch | Halldorsen | Halldorsen | Hannson | Indahl | Indahl | Lancourt | Storheim | Van der Giezen | Weber | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Category | CH | CH | CH | CH | CH | CH | CH | CH | CH | CH | CH | CH | CH |
| Year | 2000 | 2000 | 2000 | 1998 | 1998 | 1998 | 2000 | 1995 | 1998 | 1992 | 2005 | 2000 | 1998 |
| Country of origin | Ned | Swe | USA | Can | Nor | Nor | a | Nor | Nor | USA | Nor | Ned | Ger |
| Number of participants | 392 | 455 | 413 | 120 | 260 | 76 | a | 975 | 245 | 79 | 93 | 298 | 257 |
| Gender (% males) | 61 | 39 | 44 | 76 | 64 | 51 | a | 61 | 64 | NR | c | NR | 70 |
| Mean age | 40 | 44 | 42 | b | 41 | 42 | a | NR | 41 | NR | ~40 | 39 | d |
| Total number of risk factors | 42 | 41 | 39 | 1 | 23 | 28 | 19 | 3 | 28 | 34 | 42 | 36 | 24 |
| Not significant | 30 | 33 | 31 | 1 | 16 | 24 | 2 | 1 | 25 | 25 | 39 | 31 | 21 |
| Significant | 12 | 8 | 8 | 0 | 7 | 4 | 17 | 2 | 3 | 9 | 3 | 5 | 3 |
| Biomedical modifiable | 3 | 4 | 3 | 0 | 2 | 0 | 4 | 0 | 0 | 2 | 2 | 2 | 1 |
| Biomedical non-modifiable | 2 | 1 | 1 | 0 | 3 | 0 | 4 | 1 | 0 | 1 | 0 | 1 | 0 |
| Psychosocial modifiable | 5 | 2 | 2 | 0 | 1 | 1 | 9 | 1 | 1 | 3 | 1 | 1 | 2 |
| Psychosocial non-modifiable | 2 | 1 | 2 | 0 | 1 | 1 | 0 | 0 | 2 | 3 | 0 | 1 | 0 |
SA subacute, CH chronic, Can Canada, Den Denmark, Ger Germany, Isr Israel, Ned Nederlands, Nor Norway, Swe Sweden, NR not reported
aHansson [36]: Denmark: N = 494, 46% male, mean age 41; Germany: N = 295, 64% male, age = 49; Israel: N = 289, 74% male, age = 39; Netherlands: N = 392, 61% male, age = 40; Sweden: N = 455, 39% male, age = 44; USA: N = 413, 56% male, age = 42
bBradish [33]: Group non-specific 35.3, Group degenerative 45.5
cStorheim [40]: 32% in NRTW, 52% in RTW
dWeber [42]: 47 Group RTW, 52 Group nRTW
Assessment of study quality
One reviewer assessed the methodological quality of each included study. Based on existing recommendations [8] we developed a quality assessment form (see “Appendix”). Items were either rated as yes, no, partially or not known.
Results
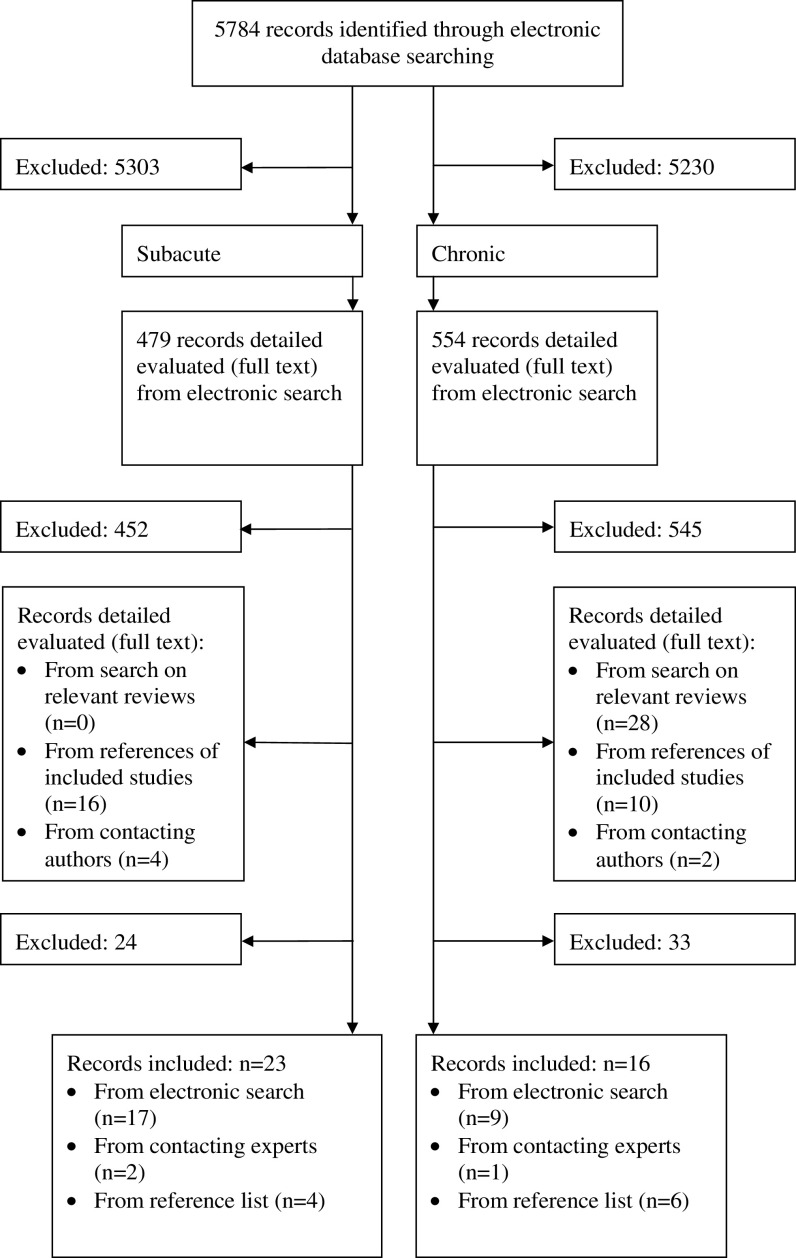
Through our search we retrieved 5,784 records from which 479 records appeared to be potentially relevant for subacute patients and 554 records for chronic patients. Full text assessment resulted in exclusion of 452 articles reporting on subacute patients and 545 articles reporting on chronic patients. Finally, we included 23 studies assessing 59–1,885 subacute patients [9–31] and 16 studies assessing 76–945 chronic patients [32–42]. For details on study selection please see Fig. 1.
Fig. 1.
Identification and selection of studies
Description of studies
Publication years ranged from 1988 to 2008. The mean age of subacute patients ranged from 30 to 48 years, and for the chronic patients from 39 to 49 years. The proportion of male patients ranged from 33 to 88% in the subacute populations (except one study, where only men were included) and from 32 to 76% in the chronic populations. The proportion of men over all studies was 67% for the subacute group and 60% for chronic group. The studies were conducted in eight different countries including Canada, Denmark, Germany, Israel, Netherlands, Norway, Sweden, and USA. For details see Table 1.
Parameters of return to work
Table 2 shows the distribution of risk factors for return to work for the subacute and chronic group, which were stratified for the two biomedical (modifiable and not modifiable) and psychosocial domains (modifiable and not modifiable).
Table 2.
Number of risk factors (modifiable/non modifiable)
| Subacute | Chronic | Total | |
|---|---|---|---|
| Biomedical | 56 (35/21) 63% | 44 (27/17) 62% | 100 (62/38) |
| Psychosocial | 61 (51/10) 84% | 61 (40/21) 66% | 122 (91/31) |
Predictors for return to work
Studies on subacute patients reported 117 significant (P < 0.05) predictors in the model, out of which 56 were biomedical (35 modifiable, 21 non-modifiable) and 61 psychosocial (51 modifiable, 10 non-modifiable). Studies on chronic patients reported 105 significant (P < 0.05) predictors in the model, out of which 44 were biomedical (27 modifiable, 17 non-modifiable) and 61 psychosocial (40 modifiable, 21 non-modifiable).
Discussion
Main findings
To our knowledge this is the first meta-epidemiologic study comparing risk factors for return to work in two populations of patients with a different duration of NSLBP. We found that the pattern of risk factor does not change markedly with increasing duration of symptoms. We observed a higher rate of modifiable psychosocial factors at earlier stages compared to later stages. Our findings are in accordance with findings by Waddell et al. [43]. They showed that at the subacute stage psychosocial factors play a eminent role in development of chronic NSLBP. Our data suggest that psychosocial interventions might be more effective at an early disease stage since we found a higher proportion of modifiable factors in the subacute group compared to the chronic group. Finally our data support current LBP guidelines recommending a multidisciplinary approach of physicians, physiotherapists and psychologists irrespective of the duration of symptoms.
Strengths and limitations
One strength of this study is the application of a robust systematic review methodology. We made strenuous efforts to minimize the risk of selection bias. Another strength is that relevant reports were searched systematically without language restriction. The definition and clinical implementation of non-specific LBP remains a problem. Some of the studies reviewed included patients with nerve root irritation. We decided to include these studies, as the suggested management of this diagnosis is the same as for NSLBP unless there are severe and progressive neurological deficits. There is a lack of consistency concerning the predictors included in the selection process for the models and the predictors retained in the final models.
Implications for research
The predictive values and their generalizability are moderate in the studies included. This is not surprising, bearing in mind that many factors influence these values in LBP patients: unstable course of LBP, large differences of risk profile in different settings, interventions, changing risk profile over time, large amount of factors influencing return to work, some are rare, but if present they are strong predictors. We assume that the inconsistencies between predictors of the included studies are due to the inclusion of patients with different risk profiles, different interventions, and different instruments that were used to identify a predictor. However, we were unable to perform statistical analyses confirming this suspicion.
In a recent publication by Hayden and co-workers about the quality of systematic reviews in the field of prognostic low back pain research the authors identified various methodological flaws on both, the study and review level [44]. While we think that we ruled out most of the shortcomings observed in the Hayden review in our study, we agree with their observation that prognostic studies, particularly in the field of low-back pain research need further methodological improvement. We propose the inclusion of existing standardized instruments completed with additional risk factors related to the biopsychosocial model (e.g. patients attitudes and beliefs, e.g. about recovery and future work capability, and work situation (measured work load and self-perceived work situation), family context, social relationships at work place, local economy, etc.), assessed at a common and clinically relevant time point (e.g. between 4 and 12 weeks pain duration) in a sufficiently large population. The process of validation should follow expert recommendations [45–49]. Another important issue relates to the reporting of primary studies. We propose that future authors of observational studies in the field of low back pain consult the recently published STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) [8] reporting guidelines. The experience of earlier initiatives to improve reporting such as the Consort, STARD and QUOROM statements [7] showed promising improvements.
Conclusions
Our data suggest that the interdisciplinary approach in patients at risk to develop chronic NSLBP is justified in both, the subacute and chronic stage. Psychosocial interventions might be more effective in subacute stages since a higher proportion of modifiable risk factors were identified in that group.
Appendix
Quality assessment form
Were the hypothesis/aim/objective of the study clearly described (prognostic)?
Were the patients enrolled consecutive?
Were the main characteristics of the included patients in the study clearly described?
Was the response rate at baseline at least 80% of the possibly eligible patients?
Were the psychosocial data collected with validated instruments?
Were data on physical workload collected?
Was a clear definition of non-specific low back pain used?
Was the treatment standardized?
Were prognostic factors that were assessed addressed by treatment?
Statistical adjustment for important prognostic factors?
Were the statistical methods adequately described?
Was the outcome clearly defined?
Were the outcome measures available for at least 80% of the included patients?
Was the model cross validated in a group of patients different from the group in which it was derived, preferably with different clinicians?
Was there a serious methodological flaw not covered by the check-list?
Footnotes
C. A. M. Heitz and R. Hilfiker equally contributed to this work.
References
- 1.Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 1992;268:760–765. doi: 10.1001/jama.268.6.760. [DOI] [PubMed] [Google Scholar]
- 2.Waddell G. The back pain revolution. Edinburgh: Churchill Livingstone; 2004. [Google Scholar]
- 3.Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, Mannion AF, Reis S, Staal JB, Ursin H, Zanoli G. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15(Suppl 2):S192–S300. doi: 10.1007/s00586-006-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koes BW, van Tulder MW, Ostelo R, Kim Burton A, Waddell G. Clinical guidelines for the management of low back pain in primary care: an international comparison. Spine. 2001;26:2504–2513. doi: 10.1097/00007632-200111150-00022. [DOI] [PubMed] [Google Scholar]
- 5.Abenhaim L, Rossignol M, Valat JP, Nordin M, Avouac B, Blotman F, Charlot J, Dreiser RL, Legrand E, Rozenberg S, Vautravers P. The role of activity in the therapeutic management of back pain. Report of the International Paris Task Force on Back Pain. Spine. 2000;25:1S–33S. doi: 10.1097/00007632-200002151-00001. [DOI] [PubMed] [Google Scholar]
- 6.Karjalainen K, Malmivaara A, van Tulder M, Roine R, Jauhiainen M, Hurri H, Koes B (2003) Multidisciplinary biopsychosocial rehabilitation for subacute low back pain among working age adults. Cochrane Database Syst Rev CD002193 [DOI] [PubMed]
- 7.Undertaking systematic reviews of research on effectiveness: CRD’s guidance for those carrying out or commissioning reviews In: CRD (ed). Center for Reviews and Dissemination, York, UK
- 8.Altman D, Egger M, Gotzsche P, Pocock S, Vandenbroucke J, von Elm E (2007) In: STrengthening the Reporting of OBservational studies in Epidemiology (STROBE). http://www.strobe-statement.org. Assessed 14 April 2009
- 9.Dionne CE, Bourbonnais R, Fremont P, Rossignol M, Stock SR, Larocque I. A clinical return-to-work rule for patients with back pain. CMAJ. 2005;172:1559–1567. doi: 10.1503/cmaj.1041159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dionne CE, Bourbonnais R, Fremont P, Rossignol M, Stock SR, Nouwen A, Larocque I, Demers E. Determinants of “return to work in good health” among workers with back pain who consult in primary care settings: a 2-year prospective study. Eur Spine J. 2007;16:641–655. doi: 10.1007/s00586-006-0180-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Faber E, Burdorf A, Bierma-Zeinstra SM, Miedema HS, Koes BW. Determinants for improvement in different back pain measures and their influence on the duration of sickness absence. Spine. 2006;31:1477–1483. doi: 10.1097/01.brs.0000219873.84232.26. [DOI] [PubMed] [Google Scholar]
- 12.Hagen EM, Svensen E, Ericksen HR. Predictors and modifiers of treatment effect influencing sick leave in subacute low back pain patients. Spine. 2005;30:2717–2723. doi: 10.1097/01.brs.0000190394.05359.c7. [DOI] [PubMed] [Google Scholar]
- 13.Heymans MW, De Vet HCW, Knol DL, Bongers PM, Koes BW, Van Mechelen W. Workers’ beliefs and expectations affect return to work 0ver 12 months. J Occup Rehabil. 2006;16:685–695. doi: 10.1007/s10926-006-9058-8. [DOI] [PubMed] [Google Scholar]
- 14.Heymans MW, Anema JR, van Buuren S, Knol DL, van Mechelen W, de Vet HCW. Return to work in a cohort of low back pain patients: development and validation of a clinical prediction rule. Ned Tijdschr Voor Fysiotherapie. 2007;117:199–206. doi: 10.1007/s10926-009-9166-3. [DOI] [PubMed] [Google Scholar]
- 15.Hunt DG, Zuberbier OA, Kozlowski AJ, Berkowitz J, Schultz IZ, Milner RA, Crook JM, Turk DC. Are components of a comprehensive medical assessment predictive of work disability after an episode of occupational low back trouble? Spine. 2002;27:2715–2719. doi: 10.1097/00007632-200212010-00011. [DOI] [PubMed] [Google Scholar]
- 16.Loisel P, Vachon B, Lemaire J, Durand MJ, Poitras S, Stock S, Tremblay C. Discriminative and predictive validity assessment of the Quebec task force classification. Spine. 2002;27:851–857. doi: 10.1097/00007632-200204150-00013. [DOI] [PubMed] [Google Scholar]
- 17.Lotters F, Burdorf A. Prognostic factors for duration of sickness absence due to musculoskeletal disorders. Clin J Pain. 2006;22:212–221. doi: 10.1097/01.ajp.0000154047.30155.72. [DOI] [PubMed] [Google Scholar]
- 18.Öhlund C, Lindstroem I, Eek C, Areskoug B, Nachemson A. The causality field (extrinsic and intrinsic factors) in industrial subacute low back pain patients. Scand J Med Sci Sports. 1996;6:98–111. doi: 10.1111/j.1600-0838.1996.tb00077.x. [DOI] [PubMed] [Google Scholar]
- 19.Okurowski L, Pransky G, Webster B, Shaw WS, Verma S. Prediction of prolonged work disability in occupational low-back pain based on nurse case management data. J Occup Environ Med. 2003;45:763–770. doi: 10.1097/01.jom.0000079086.95532.e9. [DOI] [PubMed] [Google Scholar]
- 20.Pransky GS, Verma SK, Okurowski L, Webster B. Length of disability prognosis in acute occupational low back pain: development and testing of a practical approach. Spine. 2006;31:690–697. doi: 10.1097/01.brs.0000202761.20896.02. [DOI] [PubMed] [Google Scholar]
- 21.Prkachin KM, Schultz IZ, Hughes E. Pain behavior and the development of pain-related disability: the importance of guarding. Clin J Pain. 2007;23:270–277. doi: 10.1097/AJP.0b013e3180308d28. [DOI] [PubMed] [Google Scholar]
- 22.Shaw WS, Means-Christensen A, Slater MA, Patterson TL, Webster JS, Atkinson J. Shared and independent associations of psychosocial factors on work status among men with subacute low back pain. Clin J Pain. 2007;23:409–416. doi: 10.1097/AJP.0b013e31804eff30. [DOI] [PubMed] [Google Scholar]
- 23.Schultz IZ, Crook J, Meloche GR, Berkowitz J, Milner R, Zuberbier OA, Meloche W. Psychosocial factors predictive of occupational low back disability: towards development of a return-to-work model. Pain. 2004;107:77–85. doi: 10.1016/j.pain.2003.09.019. [DOI] [PubMed] [Google Scholar]
- 24.Schultz IZ, Crook J, Berkowitz J, Milner R, Meloche GR. Predicting return to work after low back injury using the Psychosocial Risk for Occupational Disability instrument: a validation study. J Occup Rehabil. 2005;15:365–376. doi: 10.1007/s10926-005-5943-9. [DOI] [PubMed] [Google Scholar]
- 25.Soucy I, Truchon M, Cote D. Work-related factors contributing to chronic disability in low back pain. Work. 2006;26:313–326. [PubMed] [Google Scholar]
- 26.Truchon M, Cote D. Predictive validity of the chronic pain coping inventory in subacute low back pain. Pain. 2005;116:205–212. doi: 10.1016/j.pain.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 27.Turner JA, Franklin G, Fulton-Kehoe D, Sheppard L, Wickizer TM, Wu R, Gluck JV, Egan K. Worker recovery expectations and fear-avoidance predict work disability in a population-based workers’ compensation back pain sample. Spine. 2006;31:682–689. doi: 10.1097/01.brs.0000202762.88787.af. [DOI] [PubMed] [Google Scholar]
- 28.Turner JA, Franklin G, Fulton-Kehoe D, Sheppard L, Stover BD, Wu R, Gluck JV, Wickizer TM. ISSLS prize winner: early predictor of chronic work disability. A prospective, population-based study of workers with back injuries. Spine. 2008;33:2809–2818. doi: 10.1097/BRS.0b013e31817df7a7. [DOI] [PubMed] [Google Scholar]
- 29.van der Weide WE, Verbeek JH, Salle HJ, van Dijk FJ. Prognostic factors for chronic disability from acute low-back pain in occupational health care. Scand J Work Environ Health. 1999;25:50–56. doi: 10.5271/sjweh.383. [DOI] [PubMed] [Google Scholar]
- 30.van der Weide WE, Verbeek JH, van Dijk FJ. Relation between indicators for quality of occupational rehabilitation of employees with low back pain. Occup Environ Med. 1999;56:488–493. doi: 10.1136/oem.56.7.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weber A, Wilhelm M, Weber U, Raspe H. Is the subjective health status a good predictor of work resumption? Soz Praventivmed. 1998;43:177–184. doi: 10.1007/BF01349247. [DOI] [PubMed] [Google Scholar]
- 32.Bloch FSPR (2001) Who returns to work & why? A six-country study on work incapacity & reintegration. Transaction Publishers, New Brunswick, London
- 33.Bradish CF, Lloyd GJ, Aldam CH, Albert J, Dyson P, Doxey NC, Mitson GL. Do nonorganic signs help to predict the return to activity of patients with low-back pain? Spine. 1988;13:557–560. doi: 10.1097/00007632-198805000-00021. [DOI] [PubMed] [Google Scholar]
- 34.Haldorsen EMH, Indahl A, Ursin H. Patients with low back pain not returning to work: a 12-month follow-up study… including commentary by Waddell G. Spine. 1998;23:1202–1208. doi: 10.1097/00007632-199806010-00004. [DOI] [PubMed] [Google Scholar]
- 35.Haldorsen EMH, Kronholm K, Skouen JS, Ursin H. Predictors for outcome of a multi-modal cognitive behavioural treatment program for low back pain patients—a 12-month follow-up study. Eur J Pain. 1998;2:293–307. doi: 10.1016/S1090-3801(98)90028-3. [DOI] [PubMed] [Google Scholar]
- 36.Hansson TH, Hansson EK. The effects of common medical interventions on pain, back function, and work resumption in patients with chronic low back pain: a prospective 2-year cohort study in six countries. Spine. 2000;25:3055–3064. doi: 10.1097/00007632-200012010-00013. [DOI] [PubMed] [Google Scholar]
- 37.Indahl A, Haldorsen EH, Holm S, Reikeras O, Ursin H. Five-year follow-up study of a controlled clinical trial using light mobilization and an informative approach to low back pain. Spine. 1998;23:2625–2630. doi: 10.1097/00007632-199812010-00018. [DOI] [PubMed] [Google Scholar]
- 38.Indahl A, Velund L, Reikeraas O. Good prognosis for low back pain when left untampered. A randomized clinical trial. Spine. 1995;20:473–477. doi: 10.1097/00007632-199502001-00011. [DOI] [PubMed] [Google Scholar]
- 39.Lancourt J, Kettelhut M. Predicting return to work for lower back pain patients receiving worker’s compensation. Spine. 1992;17:629–640. doi: 10.1097/00007632-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Storheim K, Brox JI, Holm I, Bo K. Predictors of return to work in patients sick listed for sub-acute low back pain: a 12-month follow-up study. J Rehabil Med. 2005;37:365–371. doi: 10.1080/16501970510040344. [DOI] [PubMed] [Google Scholar]
- 41.van der Giezen AM, Bouter LM, Nijhuis FJ. Prediction of return-to-work of low back pain patients sicklisted for 3–4 months. Pain. 2000;87:285–294. doi: 10.1016/S0304-3959(00)00292-X. [DOI] [PubMed] [Google Scholar]
- 42.Weber ARH (1998) Abschlussbericht zum deutschen Teil der internationalen ISSA-Studie “Work Incapacity and Reintegration”
- 43.Waddell G, Burton AK, Main CJ. Screening to identify people at risk of long-term incapacity for work. London: The Royal Society of Medicine Press Limited; 2003. [Google Scholar]
- 44.Hayden JA, Chou R, Hogg-Johnson S, Bombardier C (2009) Systematic reviews of low back pain prognosis had variable methods and results-guidance for future prognosis reviews. J Clin Epidemiol [Epub ahead of print] [DOI] [PubMed]
- 45.Wyatt JC, Altman DG (1995) Commentary: prognostic models: clinically usefull or quickly forgotten? Br Med J 311:1539–1541
- 46.Vergouwe Y, Steyerberg EW, Eijkemans MJ, Habbema JD. Substantial effective sample sizes were required for external validation studies of predictive logistic regression models. J Clin Epidemiol. 2005;58:475–483. doi: 10.1016/j.jclinepi.2004.06.017. [DOI] [PubMed] [Google Scholar]
- 47.Altman DG, Royston P. What do we mean by validating a prognostic model? Stat Med. 2000;19:453–473. doi: 10.1002/(SICI)1097-0258(20000229)19:4<453::AID-SIM350>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 48.Laupacis A, Sekar N, Stiell IG. Clinical prediction rules. A review and suggested modifications of methodological standards. JAMA. 1997;277:488–494. doi: 10.1001/jama.277.6.488. [DOI] [PubMed] [Google Scholar]
- 49.Justice AC, Covinsky KE, Berlin JA. Assessing the generalizability of prognostic information. Ann Intern Med. 1999;130:515–524. doi: 10.7326/0003-4819-130-6-199903160-00016. [DOI] [PubMed] [Google Scholar]