Abstract
Existing predictive signs as available in current literature may miss potential proximal thoracic (PT) curve deterioration and shoulder imbalance, following selective main thoracic (MT) curve correction in adolescent idiopathic scoliosis (AIS). The present study is an attempt to evaluate and complement these signs, through a retrospective study of 56 AIS patients who underwent correction and fusion from 1986 till 2003 with follow-up 4–16 years. Forty-nine had fusion of MT curve, 7 of MT and PT. Cotrel–Dubousset instrumentation in 45, Luque in 12. Preoperative data: MT 50° (40°–80°), PT 25° (0°–50°), shoulder elevation from −4 cm (right) to 2 cm (left), clavicle angle from −14° to 5°, PT bending correction from 0 to 100% and T1 tilt from −15° to 14°. We introduced the first rib index (FRI), i.e., the difference between the diameter of right and left first rib arch as a percentage of the sum of both diameters, averaging from −22.7 to 14.3%. (Minus signs refer to or predict right, while positive left shoulder elevation.) Evaluation included all predictive parameters as related principally to postoperative left shoulder elevation ≥1 cm, patient satisfaction and surgeon fulfillment. Postoperative correction MT curve 53% (23–83%) and PT 35% (0–100%). One progressive paraplegic started 40 min following normal wake-up test. Immediate decompression, full recovery. Three cases with wound infection recovered after late removal of instrumentation. Loss of correction ≥10° in five. Fifteen had postoperative persisting left shoulder elevation ≥1 cm. Seven of these expressed dissatisfaction. Statistically FRI proved valuable predictive factor always in combination with previously described signs. We concluded that a postoperative left shoulder elevation ≥2 cm is a potential cause of dissatisfaction and may be prevented with thorough validation of all predictive signs, principally the FRI.
Keywords: Idiopathic scoliosis, Proximal thoracic curve, Shoulder imbalance
Introduction
The upper thoracic spine (T1–T5) in adolescent idiopathic scoliosis (AIS) may present an added curve, the proximal thoracic (PT), at times almost equal to and symmetrically opposite to the underlying main thoracic (MT). This is the typical “double primary thoracic curve pattern”, first described by Moe [14], who recommended extension of fusion to T1 for such cases, in order to avoid a postoperative upper body asymmetry, basically shoulder imbalance. For a mainly corrective operation this would be an embarrassing [16] result for the surgeon, with legitimate complaints from patients and their parents [17, 20].
In the great majority of cases, the PT spine in AIS shows a wide variety of greater or lesser, complete or incomplete (fractional) [20] curves that may potentially lead to postoperative shoulder imbalance either transient or permanent. The literature refers to the first ones as “nonstructural (false minor)” in contrast to “the structural (true minor)” [2]. Thus, the surgeon is often faced with a dilemma in preoperative planning, between an unnecessary extension of fusion to T1, or the risk of postoperative shoulder imbalance [9]. Routine fusion to T1 is not recommended due to possible adverse effects such as extended surgical time, increased blood loss, upper extensor muscle dissection-denervation [9], skin scar and prominence of instrumentation in the lower neck. Furthermore, this choice may be decisive for the surgical approach (anterior or posterior) [10] and the degree of MT curve correction, since this may affect the behavior of the PT curve. The potential for spontaneous correction of a free PT curve may be overcome by excessive correction of the MT curve below [6–9, 16, 20]. This risk has worsened with progressive use of more powerful and efficient instrumentation systems and widened the range of PT curves that need fusion [16, 20].
A side-to-side shoulder height (SH) difference <1 cm is considered the upper limit of balance, a difference of 1–2 cm of minimal, 2–3 cm moderate and >3 cm of significant imbalance [9, 10]. Others [16] lower the difference to 0.5 cm. Positive values refer to left and negative to right shoulder elevation. This “directionality” [10] is also used for predictive factors, a plus sign predicting left, and a minus a right postoperative shoulder elevation.
The literature offers several prognostic criteria as safeguards [3]: (1) evaluation of clinical picture [20], (2) PT Cobb angle ≥30° [13] or ≥40° [16], (3) a wedged vertebra [20], (4) a right T1 tilt ≥5° [2, 8, 11], (5) a PT bending Cobb angle ≥25° [9, 13], (6) PT extension lower than T5 [14, 16], (7) a preoperative left shoulder elevation >0.5 cm [11, 16], or even-level shoulders are considered ominous signs, and also (8) a clavicle angle ≥2°, as described recently [10] that correlates with shoulder inequality.
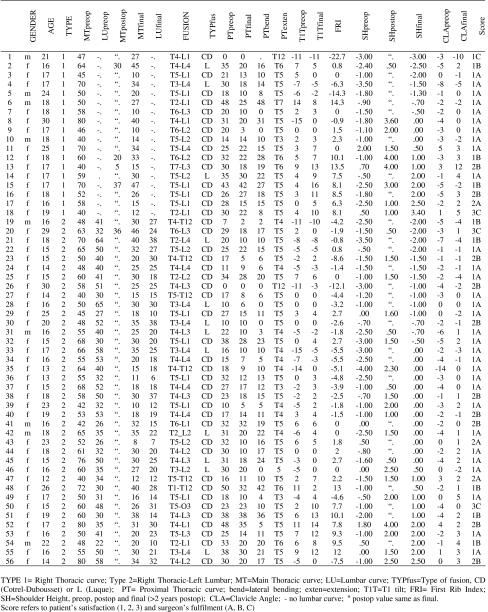
In everyday practice we may encounter cases that defy the above prognostic rules and “when a PT curve becomes structural” (with the potential risk of postoperative shoulder imbalance) “is still controversial” [10]. As an example we had a slender 18-year-old girl (Fig. 1) with a 52° right thoracic and 26° left PT curve T1–T5. The term “slender” in this study refers to adolescents with a body mass index (BMI) 20–23 kg/m2. She had a 3° right T1 tilt, a −1.8 cm (right) shoulder elevation and a −5° clavicle angle (right clavicle up). She underwent Cotrel–Dubousset (CD) fusion T5–L1 with 26° in both curves, an increased T1 tilt from 3° to 11° and an unpleasant 2 cm left shoulder elevation, last reconfirmed at age 28. A closer study of her radiographs revealed that her right first rib arch diameter was 1.1 cm longer than the left. This difference expressed as percentage of the sum of both diameters, not previously described, was defined as “first rib index” (FRI) and further investigated for its possible predictive value.
Fig. 1.
Case no. 16 (type 1): right thoracic curve. a, b Preoperative right shoulder elevation. c, d Postoperative left shoulder elevation
The present study is a retrospective assessment of the PT curve in AIS and validation of all prognostic factors including FRI, as related mainly to postoperative shoulder asymmetry, patient satisfaction and surgeon fulfillment.
Materials and methods
From June 1986 to January 2003, we operated on 110 patients with scoliosis of the spine. Of these, 30 were of known etiology, 1 was juvenile and 19 had thoracolumbar or lumbar curves without PT curve problem. Of 60 operated patients with adolescent idiopathic scoliosis, 3 were excluded because of incomplete follow-up data and 1 because of traffic accident complications early postoperatively. The remaining 56 consecutive patients in Table 1, 9 males and 47 females with idiopathic scoliosis, operated from June 1986 to January 2003, were retrospectively assessed with emphasis on PT curves and shoulder imbalance. The mean age was 18 years (12–30 years). Of those 56 patients, 18 had single right thoracic (MT) curves (apex T11–T12 disc and up, no true lumbar curve with opposite tilted end vertebrae) and 38 double right thoracic–left lumbar (LU) curves.
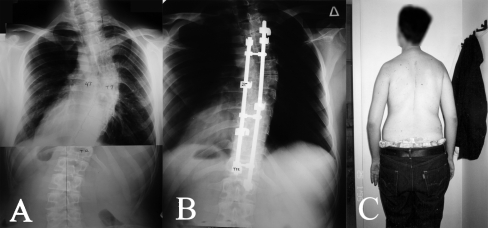
Table 1.
Case summaries
Measurements were marked on standard posteroanterior and lateral standing analog radiographs 35 × 43 cm of the spine, exposed with the tube at 2 m standard distance. Supine side bending films were also available. (1) Cobb angle of MT 56°, range 40°–80°, (2) PT Cobb 25°, range 0°–50°, (3) preoperative SH measured at upper bony surface of lateral end of clavicle [16] or the lowest point of the scapulohumeral joint, or coracoid process [4], if necessary, ranged from −4 cm (right shoulder up) to 2 cm (left shoulder up) mean −1.2 cm, (4) clavicle angle (CLA) from −14° (right clavicle up from horizontal) to 5° (left clavicle up) mean −2°, (5) T1 tilt (T1T) varied between −15° (left tilt) and 14° (right) mean 0°, (6) PT bending correction (PTbend) from 0 to 100%, and (7) PT curve extension (PTexten) to T6 or T7 in five cases. Two of these last patients, #6 and 48, were the typical double thoracic type of Moe with almost equal PT and MT curves, a right shoulder elevation and T1T 14° and 11°. In patients #1, 19 and 26 the PT spine was part of a nearly single curve, unified with the MT (T1–T12), with a left T1 tilt and prominent −3 cm right shoulder elevation (Fig. 2).
Fig. 2.
Case no. 1: a preoperative unified single thoracic curve T1–T12. b Postoperative fusion T4–T12. c Persistent right upper body prominence
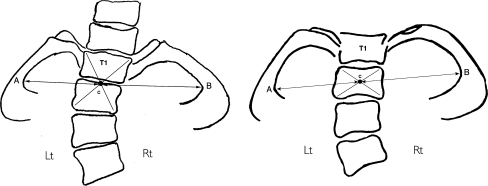
The diameter of the first rib arch (Fig. 3), measured from the geometric center C (intersection of two diagonals) of the respective level vertebral body/bodies (T2 or T1 and T2), whichever was nearest to a line AB connecting the most distal internal points of the first rib arches, measured 4.8–8 cm, mean 6.1 cm. The difference in length between right and left first rib arch diameter (CB − CA) expressed as a ratio  and defined as FRI, was from −22.7% (left arch longer) to 14.3% (right arch longer predicting left shoulder elevation). The measurement of this index is simple, giving reliable values as tested by repeated measurements.
and defined as FRI, was from −22.7% (left arch longer) to 14.3% (right arch longer predicting left shoulder elevation). The measurement of this index is simple, giving reliable values as tested by repeated measurements.
Fig. 3.
First rib index (FRI) = CB − CA in cm
Forty-four patients had CD hook fusion, 5 of them to T1 or T2. Luque (L) in 12 patients, 2 of them to T2. Extension to T1 or T2 was at the time not always based on consistent criteria. Proximal kyphosis of 37°–42° in three patients (only one fused). Transitional (TL) kyphosis around 12° in three patients (one not included in fusion).
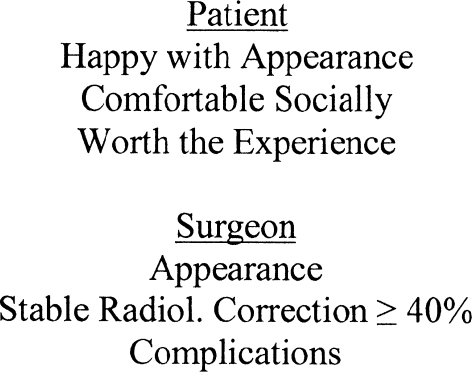
The issue of patient satisfaction scores presents inconsistencies [6, 7, 10, 15, 17, 19]. In view of such difficulties, our final assessment for patient satisfaction and surgeon fulfillment relied on the following question (asked by the surgeon-first author): “Are you satisfied with the operative result?” The patients had three optional answers: “Yes”, “Reserved” or “No” (denoted by 1, 2, 3, respectively). In order to have a clear perception of the term “satisfaction” and the patient’s answer to be more precise, the basic question was further specified by three parameters: “Happy with Appearance”, “Comfortable Socially” and “Worth the Experience” (see Fig. 4). These three parameters (guidelines) summarize the modified SRS Outcomes Instrument [21]. The “Yes” answer denotes positive opinion for all three parameters. The “Reserved” answer denotes positive opinion for at least one parameter and at most for 2. Finally, the “No” answer denotes negative opinion for all three parameters.
Fig. 4.
Further analysis of question: “Are you satisfied with operative result?”
Surgeon’s fulfillment was based on: “Clinical Appearance”, “Stable Radiological Correction ≥ 40%” and “Complications” (see Fig. 4). A combination of these three parameters, corresponded successively to “Yes”, “Reserved” or “No” answers by the surgeon and marked by A, B, C, respectively. As in the case of patient satisfaction, surgeons’ answer “Yes” denotes positive opinion for all three parameters, “Reserved” denotes positive opinion for at least one parameter and at most for two and “No” answer negative opinion for all three parameters.
Our final scoring was as follows: 1A referred to “excellent”, 1B or 2A to “good”, 1C or 2B to “reserved” and 3C to “bad”.
All patients were operated by the same surgeon (the first author of the present study). Follow-up 4–16, mean 6 years.
Statistical analysis
The statistical analysis of the data aimed to assess whether and how the variability of the SH final (SHfinal) is explained by the variability of FRI, PTpreop, SHpreop, T1T, CLA and PTbend. The corresponding correlation coefficients were estimated and multiple linear regression analysis was performed in order to find a prediction model for SHfinal (response variable).
For the statistical analysis the package STATGRAPHICS Plus v.4 (Statistical Graphics Corp.) was used.
Results
Correction of MT curve 53% ranges from 23 to 83%. Correction of PT curve 35% ranges from 0 to 100%.
Complications
We had one insidious paraplegic starting progressively during recovery in operating room approximately 40 min after normal wake-up test (no monitoring available). Immediate MRI and reopening at upper end of exposure (T5). Removal of local epidural hematoma under pressure, cauterization and clipping of venal varicose plexus, with instrumentation in place. Full recovery after 6 weeks. One primary and two delayed deep wound infections treated with local washing and antibiotics, cleared only after late removal of CD instrumentation, with maintenance of correction. Five patients had loss of correction in main curve ≥10°. One, #50, with deep wound infection had also an unbalanced body correction [16].
Shoulder balance outcomes, patient satisfaction and surgeon fulfillment
From Table 2, we can see that 25 patients had radiologically level shoulders postoperatively (>−1 and <+1 cm) from originally 15. Out of 38 with preoperative right shoulder elevation 16 remained with this imbalance postoperatively. Finally the number of patients with left shoulder elevation increased from 3 to 15 postoperatively.
Table 2.
Preoperative and final shoulder height
| Shoulder balance | Number of cases | |
|---|---|---|
| SHpreop | SHfinal | |
| Balance | 15 | 25 |
| Right imbalance | 38 | 16 |
| Left imbalance | 3 | 15 |
| Total | 56 | 56 |
SHpreop preoperative shoulder height, SHfinal final shoulder height, balance −1 < shoulder height < +1, right imbalance shoulder height ≤ −1, left imbalance shoulder height ≥ +1
Table 3 shows patient satisfaction within the above three categories: 6 of 25 in the balance group had a “reserved” answer, 3 due to less than optimal general correction and 1 with a primary wound infection of long duration. One girl had a 1.5 cm left shoulder elevation that subsided to 0.5 cm. Finally, one slender girl (#43) with level shoulders postoperatively and an excellent near perfect curve correction remained “Reserved”. Her problem was a preoperative noticeable left trapezial area soft tissue prominence that persisted postoperatively. Of 16 patients with right shoulder imbalance (−3 to −1 cm) 2 remained “reserved” mainly because of lower body imbalance. A third female patient was categorized as “bad”. She had loss of correction after partial instrumentation failure and a mild late superficial infection. Patient #1, a boy with a −3 cm (right) shoulder elevation seemed quite pleased with the operative result (answered “Yes”), but the surgeon had a different opinion (answer “No”). Generally, patients with right shoulder elevation had no complaints. Fifteen patients had persisting left shoulder elevation 1–3.6 cm. Within this group eight patients, (including one boy) with 1–2 cm left shoulder elevation, were either the short plump (body mass index 18–20 kg/m2) or the muscular athletic type and seemed quite pleased with their appearance (answered “Yes”). The remaining seven were tall, slender girls (like the one in Fig. 1). Five of them presented a shoulder imbalance ≥2 cm including one with a 4 cm difference that subsided to 1 cm 10 years postoperatively. This discrepancy was an embarrassing outcome. They were categorized as “Reserved” but were definitely not inclined to undergo a second operation, gradually over the years coming to terms with this faulty detail. Two of the seven girls category was “No”. One with the worst shoulder difference (3.4 cm), the other with body-shoulder imbalance and a deep wound infection. Both were subjected to a second operation.
Table 3.
Postoperative patient satisfaction vs. final shoulder height
| SHfinal | Number of cases | Patient satisfaction | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Balance | 25 | 19 | 6 | 0 |
| Right imbalance | 16 | 13 | 2 | 1 |
| Left imbalance | 15 | 8 | 5 | 2 |
| Total | 56 | 40 | 13 | 3 |
SHfinal final shoulder height, balance −1 < shoulder height < +1, right imbalance shoulder height ≤ −1, left imbalance shoulder height ≥ +1
Patient’s satisfaction and surgeons’ fulfillment, as summarized in Table 4, was excellent to good (1A, 1B, 2A) in 42 patients (75%), acceptable with reservations (1C, 2B) in 11 (20%) and bad (3C) in 3 (5%). Opinions of patients and surgeon were more or less in agreement.
Table 4.
Patient satisfaction vs. surgeon fulfillment
| Surgeon fulfilmenta | Patient satisfactiona | |||
|---|---|---|---|---|
| 1 (Yes) | 2 (Resrd) | 3 (No) | Total | |
| A (Yes) | 31 | 3 | 0 | 34 |
| B (Resrd) | 8 | 10 | 0 | 18 |
| C (No) | 1 | 0 | 3 | 4 |
| Total | 40 | 13 | 3 | 56 |
aPatients and surgeon answers to the question: ‘Are you satisfied with the operative results?’
Statistical correlations
Table 5 shows Pearson’s correlation coefficients between SHfinal as compared to FRI, PTpreop, SHpreop, T1T, CLA and PTbend variables.
Table 5.
Pearson’s correlations between SHfinal and each one of the preoperative measurements of FRI, PTpreop, SHpreop, T1T, CLA and PTbend
| FRI | PTpreop | SHpreop | T1T | CLA | PTbend | |
|---|---|---|---|---|---|---|
| SHfinal | 0.59 (0.0000) | 0.42 (0.0012) | 0.39 (0.0031) | 0.35 (0.0086) | 0.30 (0.0270) | 0.24 (0.0695) |
P values in parentheses
SHfinal final shoulder height, FRI first rib index, PT proximal thoracic curve, T1T T1 tilt, CLA clavicle angle, PTbend proximal thoracic lateral bending
The coefficients measure strength of linear relationships among corresponding variables. P values below 0.05 indicate statistical significance at 95% confidence level. In this series all correlations are positive and seem statistically significant (except PTbend) at the 95% confidence level, though weak. Highest correlation is between SHfinal and FRI.
The multiple linear regression analysis, with forward and backward selection, leads to two models explaining a small percentage of the variability of the SHfinal ( and
and  correspondingly). However, this analysis indicates that the FRI variable has, in both cases, the greatest contribution to the explicable percentage of the variability of the SHfinal. In other words, FRI includes “interesting” information for the variability of SHfinal, particularly as compared to the remaining predictors.
correspondingly). However, this analysis indicates that the FRI variable has, in both cases, the greatest contribution to the explicable percentage of the variability of the SHfinal. In other words, FRI includes “interesting” information for the variability of SHfinal, particularly as compared to the remaining predictors.
Based on the above analysis and previously mentioned predictive factors’ values [2, 8, 11, 13, 16], we studied cases satisfying at least one of the following conditions:
 |
1 |
and SHpreop of any value.
Under the above circumstances, the multiple linear regression analysis (with forward and backward selection) leads to the equation:
 |
2 |
with n = 26 (cases), R2 = 84.46%,  and standard errors of the estimates as shown in Table 6.
and standard errors of the estimates as shown in Table 6.
Table 6.
Multiple linear regression analysis of preoperative: FRI, PTpreop, SHpreop, T1T, CLA and PTbend on SHfinal
| Preoperative parameter | Estimate | Standard error | P value |
|---|---|---|---|
| FRI | 0.24 | 0.03 | 0.0000 |
| SHpreop | 0.85 | 0.15 | 0.0000 |
| T1T | −0.45 | 0.06 | 0.0000 |
| PTpreop | 0.07 | 0.01 | 0.0000 |
SH shoulder height, FRI first rib index, PT proximal thoracic curve, T1T T1 tilt, CLA clavicle angle, PTbend proximal thoracic lateral bending
The above equation contains only four factors out of the original six. One of them (SHpreop) comes without conditions. This equation is proposed as a good  prediction model for SHfinal outcome as derived from the preoperative FRI, SH, T1T and PT values provided that at least one of the conditions (1) is satisfied. For example, if FRI = 7.5%, SHpreop = 0.5 cm, T1T = 4°, and PTpreop = 30° then the mean prediction for the SHfinal is 2.57 cm with 95% confidence interval (2.00 cm, 3.14 cm).
prediction model for SHfinal outcome as derived from the preoperative FRI, SH, T1T and PT values provided that at least one of the conditions (1) is satisfied. For example, if FRI = 7.5%, SHpreop = 0.5 cm, T1T = 4°, and PTpreop = 30° then the mean prediction for the SHfinal is 2.57 cm with 95% confidence interval (2.00 cm, 3.14 cm).
The preoperative factors (FRI, SH, T1T and PT) explain, through model (2), 82.25% of the variability of SHfinal. The remaining 17.75% may be explained by other factors (known, suspected or unknown) including intersurgical parameters (level of fusion, amount of MT curve correction, etc.). The value of model (2) is its’ possibility to predict shoulder imbalance risk through preoperative factors. Nevertheless, in “Conclusions”, we present some preliminary and practical guidelines referring to intersurgical parameters and based mainly on our retrospective observations.
The relation of patients age to SHfinal was tested statistically and no significant relationship was found (P ≥ 0.3870).
Discussion
In published studies on PT curves of AIS [10, 11, 16], the lower limit for their inclusion is 20°. The present study comprises all PT curves, because even smaller ones may result in postoperative shoulder imbalance either temporary or long lasting. Nineteen Thoracolumbar (TL) curves in our series and 71 from the literature had no PT curve problem. In other studies [11] TL curves were excluded. A review of 104 scolioses with single right thoracic curves, published during the same period, showed a wide variety in morphology of PT curves similar to our series, defying any attempt towards a meaningful practical classification in almost 90% of them. The typical double thoracic curve pattern requiring fusion to T1 or T2 according to Moe [14], occurred in approximately 8% of cases. At the other end are almost 2% of patients (Fig. 2) with a nearly unified right thoracic curve up to T1 (PT + MT), not previously mentioned in the literature to our knowledge, although seen in published cases, with considerable left T1 tilt and right shoulder elevation, that may also need fusion to T1 or T2 as seen in patient #1. In the majority of PT curves though, the surgeon has to make a critical choice in fusion levels between so called “structural” [13] (liable to postoperative shoulder imbalance) and “nonstructural” curves, that may spontaneously adapt to the fused MT curve below with balanced shoulders, as did the majority of PT curves in the present and published series.
A transient immediately postoperative left shoulder elevation in spite of good prognostic signs as in 14 of our patients, may be due to pain or change of posture and mechanism of spontaneous correction may involve the righting reflex of head control by neck muscle power [11].
As mentioned in “Materials and methods”, patient satisfaction scores are notoriously unreliable. In our cases, based on long personal follow-up we found that a side-to-side difference ≥2 cm (moderate imbalance) with left shoulder high may incite resentment and grievances, especially among girls as in seven of our patients, particularly during teenage years, because that is when it matters most. After 8–10 years this imbalance although still present is usually completely forgotten. They are often married now with children and different priorities. Boys and rather short, plump girls or athletic types are much less prone to express discontent as seen here and in the recent literature [17]. Shoulder inequalities up to 1.5 cm may exist even in normal people [1].
A trapezial area fullness or bulging, (preexisting or as a result of main curve correction [20]) may appear with left shoulder elevation, or occasionally be a problem by itself, that merits special attention and careful discussion with patients and parents.
Right shoulder elevation is not mentioned as a problem in published case reports. In the present series 16 patients had differences up to −4 cm, some improving postoperatively [10], not causing any complaints. In the boy #1 (Fig. 2), with a unified PT + MT curve from T1 to T12 (fused T4–L1) a preoperative −3 cm (right) shoulder prominence persisted postoperatively. He expressed no complaints, but the surgeon remained skeptical about the result.
A fairly accurate prediction of postoperative shoulder imbalance ≥2 cm should be followed by inclusion of the PT curve in the instrumented fusion especially when attempting to balance the shoulders [10]. Interestingly this procedure will not always guarantee balanced shoulders postoperatively [10, 16]. Two of our cases, #18 and 54, fused to T1 and T2 (corrected from 30° to 22° and from 33° to 20°) had considerable postoperative shoulder imbalance, along with increased or unimproved T1 tilt. Similar results were seen in published cases [11]. This correlation between postop T1 tilt and SHfinal was statistically strong in our cases (P = 0.0000). Reduction of T1 tilt appears to be a possible prerequisite for postoperative shoulder balance and may be ascertained radiographically during the operation as we realized retrospectively in two of our cases with X-rays in OR taken for unrelated purposes. This problem is discussed in a recent article [5].
A tempered correction of the main curve is a useful option in preventing deterioration of secondary curves [8, 12, 14, 20]. In the present series the ratio of PT to MT curve correction had a strong correlation with SHfinal (P = 0.0006).
As seen in our statistical analysis, the correlation of each separate predictive factor to SHfinal is weak in covering postoperative shoulder balance disturbances. A combination of four predictive factors satisfying at least one of the conditions (1) will help the surgeon adequately estimate SHfinal.
Within this combined predictive model, FRI seems to be significantly contributing to predict postoperative upper body asymmetry. More specifically, a prediction value of SHfinal ≥2 cm is considered to be critical in surgical decision making. Of course, the final decision depends heavily on the personality and idiosyncrasy of each patient.
Conclusions
A postoperative elevation of the left shoulder area may be a sequel of selective surgical correction (medialization) of a right MT curve in AIS. An elevation ≥2 cm may incite resentment and grievances, mainly among teenage girls. This untoward effect has been associated with the presence of a superimposed “structural” PT curve. Deterioration of this curve postoperatively is believed to be coupled with left upper body imbalance and increased T1 tilt according to our preliminary observations. The FRI is a valuable predictive sign for such development in combination with other preoperative known predictive factors. Furthermore, it is easily detected and remains stable through repeat examinations or recumbency.
To avoid this complication a “tempered” correction of MT curve is a sensible measure, that relies on the potential for spontaneous correction of the PT curve. Extension of fusion with full correction of PT curve is the other alternative solution, especially with contemporary trends aiming at 100% correction of the MT curve.
More specifically in approximately 7–8% of cases with typical double thoracic curves of Moe, fusion of both MT and Pt curves with reduction of T1 tilt remains the elective procedure.
In the unusual case (2%) of a unified MT and PT into a single thoracic curve, fusion to T1 is also necessary to avoid an excessive unsightly right body-shoulder imbalance.
Finally, in cases with ominous predictive signs especially in slender, teenage girls (approximately 16% in this series) the surgeon may rely on an X-ray after having inserted the corrective rod on the concave side. If T1 then shows a persisting or increased right T1 tilt he may decide either to lessen correction of MT curve or extend fusion and reduce T1 tilt.
A reasonable criticism of this study is its retrospective nature. A second criticism concerns the number of patients that may seem insufficient to cover the wide variations in morphology of PT curves.
The favorable aspects are treatment by one surgeon, a long personal follow-up, and the fact that the patients are of the same cultural community thus excluding possible cultural issues that might have interfered with outcomes [18].
Acknowledgments
The authors would like to express their sincere thanks to Prof. Alexander Sideridis of the Informatics Laboratory at AUA, Athens, Greece, for his generous support. No financial or other support received connected with this paper.
Footnotes
Part of this paper was presented at the 62nd annual meeting of the Hellenique Orthop. Society (October 2006) and received the 1st award for best clinical paper.
References
- 1.Akel I, Pekmezci M, Yazici M et al (2006) The evaluation of shoulder balance in healthy adolescent population and its correlation with radiological measures. In: SRS annual meeting, abstract 9 [DOI] [PMC free article] [PubMed]
- 2.Asher MA, Lenke LG, Labelle HHL et al (2003) Interobserver and intraobserver reliability of the srs classification of adolescent idiopathic scoliosis. In: SRS annual meeting, abstract 1B
- 3.Betz RR, Harms J, Clements DH, et al. Comparison of anterior and posterior instrumentation for correction of adolescent thoracic idiopathic scoliosis. Spine. 1999;24:225–239. doi: 10.1097/00007632-199902010-00007. [DOI] [PubMed] [Google Scholar]
- 4.Bridwell KH, Shufflebarger HL, Lenke LG, et al. Parent’s and patient’s preferences and concerns in idiopathic adolescent scoliosis. Spine. 2000;25:2392–2399. doi: 10.1097/00007632-200009150-00020. [DOI] [PubMed] [Google Scholar]
- 5.Cambell RM, Jr, Adcox MB, et al. The effect of mid-thoracic VEPTR opening wedge thoracostomy on cervical tilt associated with congenital thoracic scoliosis in patients with thoracic insufficiency syndrome. Spine. 2007;32:2171–2177. doi: 10.1097/BRS.0b013e31814b2d6c. [DOI] [PubMed] [Google Scholar]
- 6.Cole AA, Al-Hussainy H, Chiverton N et al (2007) Is it possible to objectively assess cosmesis in adolescent idiopathic scoliosis? In: SRS annual meeting, abstract
- 7.Donaldson S, Hedden D, Stephens D, et al. Surgeon reliability in rating physical deformity in adolescent idiopathic scoliosis. Spine. 2007;32(3):363–367. doi: 10.1097/01.brs.0000253605.71168.2e. [DOI] [PubMed] [Google Scholar]
- 8.King HA, Moe JH, Bradford DS, et al. The selection of fusion levels in thoracic idiopathic scoliosis. JBJS. 1983;65A:1302–1313. [PubMed] [Google Scholar]
- 9.Kuklo TR, Lenke LG, Won DS, et al. Spontaneous proximal thoracic curve correction after isolated fusion of the main thoracic curve in adolescent idiopathic scoliosis. Spine. 2001;26:1966–1975. doi: 10.1097/00007632-200109150-00006. [DOI] [PubMed] [Google Scholar]
- 10.Kuklo TR, Lenke LG, Graham EJ, et al. Correlation of radiographic, clinical and patient assessment of shoulder balance following fusion versus nonfusion of the proximal thoracic curve in adolescent idiopathic scoliosis. Spine. 2002;27:2013–2020. doi: 10.1097/00007632-200209150-00009. [DOI] [PubMed] [Google Scholar]
- 11.Lee CK, Denis F, Winter RB, Lonstein JE. Analysis of the upper thoracic curve in surgically treated idiopathic scoliosis. A new concept of the double thoracic curve pattern. Spine. 1993;18:1599–1608. doi: 10.1097/00007632-199309000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Lenke LG, Bridwell KH, O’Brien MF, et al. Recognition and treatment of the PT curve in AIS treated with Cotrel–Dubousset instrumentation. Spine. 1994;19:1589–1597. doi: 10.1097/00007632-199407001-00007. [DOI] [PubMed] [Google Scholar]
- 13.Lenke LG, Betz RR, Harms J, Bridwell KH, et al. Adolescent idiopathic scoliosis. a new classification to determine extent of spinal arthrodesis. JBJS. 2001;83A:1169–1181. [PubMed] [Google Scholar]
- 14.Moe JH (1972) Methods of correction and surgical technics in scoliosis. Orthop Clin North Am:22–25 [PubMed]
- 15.Resnik DK. Evidence-based spine surgery. Spine. 2007;11S:S15–S19. doi: 10.1097/BRS.0b013e318053d4b4. [DOI] [PubMed] [Google Scholar]
- 16.Suk SI, Kim WJ, Kim JH, et al. Indications of proximal thoracic curve fusion in thoracic adolescent idiopathic scoliosis. Spine. 2000;25:2342–2349. doi: 10.1097/00007632-200009150-00012. [DOI] [PubMed] [Google Scholar]
- 17.Tones M, Moss N, Polly DW. A review of quality of life and psychosocial issues in scoliosis. Spine. 2006;26:3027–3038. doi: 10.1097/01.brs.0000249555.87601.fc. [DOI] [PubMed] [Google Scholar]
- 18.Watanabe K, Lenke LG, Bridwell KH, et al. Cross-cultural comparison of the scoliosis research society outcomes instrument between American and Japanese idiopathic scoliosis patients: are there differences? Spine. 2007;32(24):2711–2714. doi: 10.1097/BRS.0b013e31815a7ef0. [DOI] [PubMed] [Google Scholar]
- 19.Wilson PL, Newton PO, Wenger DR, et al. A multicenter study analyzing the relationship of a standardized radiographic scoring system of adolescent idiopathic scoliosis and the scoliosis research society outcomes instrument. Spine. 2002;27:2036–2040. doi: 10.1097/00007632-200209150-00013. [DOI] [PubMed] [Google Scholar]
- 20.Winter RB. The idiopathic double thoracic curve pattern: its recognition and surgical management. Spine. 1989;14:1287–1292. doi: 10.1097/00007632-198912000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Winter RB. Modified SRS outcomes instrument. Appendix A. Spine. 2000;25:2384–2386. [Google Scholar]