Abstract
In a prospective study, 23 consecutive girls with Rett syndrome and neuromuscular scoliosis were evaluated for functioning at a long-term follow-up. The patients had mostly improved, which was confirmed by their parents. Rett syndrome is associated with neuromuscular scoliosis and has a typically long C-shaped thoracolumbar kyphoscoliosis. Prospective long-term follow-up studies related to these patients’ total situation are sparse. Most studies focus on the Cobb angle of the scoliosis, whereas parents are mainly concerned about the girls’ continued functioning. Twenty-three patients with Rett syndrome and neuromuscular scoliosis were evaluated preoperatively from 1993 to 2002. At follow-up, 19 patients remained in the study. Three patients died (not due to surgery), and one patient could not participate because it was too far to travel. Mean follow-up time was 74 months (range 49–99 months). The assessments comprised the sitting balance, seating supports in wheelchair, weight distribution, time used for rest, care given, and angle of scoliosis. Follow-up questionnaires and two-open-ended questions about the positive and negative effects of surgery were sent to parents. Sitting balance, number of seating supports in wheelchair, weight distribution, time used for rest, and the Cobb angle had all improved after surgery. The parents assessed improvement in seating position, daily activities, time used for rest, and cosmetic appearance. We can conclude that the stabilized spine resulted in sufficient strength to keep the body upright with the possibility of looking around at the surroundings more easily. The girls got better seating position with less need for seating adaptations in the wheelchair and with reduced time needed for resting during the day. Finally we can conclude that the indication for surgery is to get a better posture which lead to less risk of pressure sores, and that un upright position lead to better possibility to easily breath with fewer episodes of pneumonia and a better general health as result. The evidence of positive surgical effects for girls with Rett syndrome is of great importance in indication for surgery in the decision-making process.
Keywords: Rett syndrome, Neuromuscular scoliosis, Long-term follow-up, Functioning
Introduction
Rett syndrome is associated with a neurological form of scoliosis, and occurs almost exclusively in girls. It typically has a long C-shaped thoracolumbar kyphoscoliosis. The occurrence of scoliosis increases with age. The onset of scoliosis is usually before 8 years of age and progresses rapidly. Surgery is indicated when curves exceed 40° [3].
Scoliosis is rarely present at birth, but tends to increase with growth according to a British survey [4]. Seventy-four percent in a Swedish survey developed scoliosis and 83% reported other deformities. The majority of the girls had problems with postural control with leaning in different directions in the sitting position [8].
The progression of the scoliosis in Rett syndrome is more rapid than in idiopathic scoliosis, with a curve progression of >15°/year [9].
Prospective long-term follow-up studies for patients with neuromuscular scoliosis and Rett syndrome in relation to the patient’s total situation are few, and the results often focus on the angle of the scoliosis. However, the interests of the parents are different. They ask about the girls’ continued ability to walk, which sitting positions will be allowed, and whether surgery will affect the girls’ daily activities postoperatively.
In a previous study by Larsson et al. [6] for children who do not understand verbal instructions, the parents’ motives for surgery most often wanted to obtain improvements in seating posture and respiration.
Aim
The aim of this study was to evaluate the long-term follow-up of functioning with a focus on the self-reported quality of care, measurements of seating position, and angle of scoliosis, in patients with neuromuscular scoliosis and Rett syndrome, pre- and postoperatively in order to elucidate the preoperative decision-making process between the surgeon and the parents.
Methods
In this prospective study, the patients were evaluated before and after surgery concerning their activities and function. They were also evaluated radiographically. In addition, two follow-up questionnaires were used after surgery. The mean follow-up time was 74 months (range 49–99 months).
Patients
From September 1992 to April 2002, 23 consecutive patients with Rett syndrome and neuromuscular scoliosis were evaluated before surgery. Eighty-three percent (19 of 23 patients) were available for long-term evaluation. The reasons for discontinuation are as follows. One patient’s relative did not participate in the postoperative assessment due to distance. One patient died 3 months after surgery, which had no relation neither to surgery nor to the deformity. Two patients died 5 years after surgery from underlying diseases. The mean age preoperatively was 13 years (range 9–18), and the mean age at follow-up was 19 years (range 16–24 years).
Six patients had used a brace, and seven had persistent skin discoloration at the tuber ischi, preoperatively. Seven were able to walk preoperatively (three independently and four with support from one person).
The surgical technique for all the patients was posterior segmental instrumentation with sublaminar wires, hooks, and screws. For 19 patients, the instrumentation and fusion were extended to the pelvis or sacrum; to L5 in 1 patient, L4 in 2, and to L3 in 1 patient. The fixation to the sacrum was done by screws in the S1 pedicle. In 3 of the 23 patients, an anterior instrumentation with the Zielke apparatus was used, and after 1995, the Aaro anterior instrumentation,1 was used in combination with the posterior segmental instrumentation in 4 of the 23 patients.
Set of instruments
A combination of new and existing instruments was used [10–12] consisting of general information, activities and function, and a follow-up questionnaire. The parents were asked about the motive for surgery and were given the following yes/no response alternatives: respiration, pain, seating position, and cosmetic concerns. An open-ended question was also included to allow other answers to be given (Table 1). The follow-up questionnaire consisted of a subjective assessment in which the parents evaluated the long-term follow-up results of surgery in 12 areas [12]. The five response alternatives were: very positive, positive, unchanged, negative, and very negative. The results were trichotomized to positive (very positive and positive), unchanged, or negative (very negative and negative). The part of the instrument with activities and function consists of sitting balance on a seven-point scale, and was rated from no ability (1 point) to full ability to sit with ability to attain the position (7 points) [11], weight distribution on seating surface in force (N), pressure (N/cm2) [12], angle of scoliosis (Cobb), reaching [12], pain estimation [12]. We could not use the ADL, pain estimation, and reaching variables, or the lung function test because the patients with Rett syndrome could not understand or follow verbal instructions [5–7]. Along with the invitation to take part in the long-term follow-up, two-open-ended questions were mailed to the parents: “What do you think has improved since the surgery?” and “What do you think is worse since the surgery?” [7] (Table 2). The responses to these two questions were analyzed, grouped together, classified into different dimensions, and illustrated by quotations.
Table 1.
Parents’ motives for surgery
| Motive for surgery | Number of answers |
|---|---|
| Predictive areas | |
| Respiration | 5 |
| Pain | 2 |
| Sitting posture | 9 |
| Cosmetic appearance | 0 |
| Open-ended questions | |
| Prevent progression | 8 |
| Better strength in spine | 6 |
| Continue to walk | 3 |
| Get rid of brace | 2 |
| Better balance | 1 |
| Better communication | 1 |
Table 2.
The timing of assessments with the instruments used during the study concerning general information, activity and function, the follow-up questionnaire, and the two-open-ended questions
| Variable | Preop | Postop 1 year | Long-term |
|---|---|---|---|
| General information | × | ||
| Personal data | × | ||
| Diagnoses | × | ||
| Motive for surgery | × | ||
| Persistent skin discoloration | × | × | × |
| Ambulating/wheelchair use | × | × | × |
| Occupation | × | ||
| Understands/does not understand verbal instructions | × | ||
| Brace | × | × | × |
| Activity and function | |||
| Angle of scoliosis (Cobb) | × | × | × |
| Weight distribution on seating surface force (N), pressure (N/cm2) | × | × | × |
| Sitting balance (1–7 points) | × | × | × |
| Seating supports in wheelchair (0–7 supports) | × | × | × |
| Time used for resting (h/week) | × | × | × |
| Care given (physical effort 0–30 points) | × | × | × |
| Care given (time consumption in min) | × | × | × |
| Lung function (VC) | − | – | − |
| Reaching (0–60 points) | − | – | – |
| Pain estimation (1–15 points) | − | – | – |
| Klein and Bell ADL scale (0–303 points) | − | – | – |
| Follow-up questionnaire | |||
| Pain | × | × | |
| Breathing | × | × | |
| Gastrointestinal function | × | × | |
| Seating | × | × | |
| Reaching | × | × | |
| Daily activities | × | × | |
| Care given | × | × | |
| Ambulation | × | × | |
| Cosmetic appearance | × | × | |
| Need for rest | × | × | |
| School | × | × | |
| Work | × | × | |
| Two-open-ended questions | |||
| What do you think has improved since the surgery? | × | ||
| What do you think has worsened since the surgery? | × | ||
Statistics
To detect any significant differences between the preoperative and postoperative results, the median values and Wilcoxon signed rank test were used.
To examine whether the patients who discontinued (the two patients who died after 5 years) could affect the results, we performed an intention-to-treat analysis, with an analysis of the last observation carried forward from the 1-year follow-up results [1].
Results
Early complications of surgery
Short-term problems were found in 10 of 23 patients (44%). Of these ten patients, six had respiratory problems and two required respiratory treatment for several days (one of the 7 who were fused with anterior and posterior instrumentation had atelektas). Superficial postoperative wound infections were found in four patients.
Late events
In four patients, progression of the deformity was found probably due to crankshaft phenomenon related to remaining growth. One patient had a complementary stabilization below the fixation from L5 to S1 after 1 year, and one above the fixation from T2 to C5 after 6 months.
Comparisons were made between the preoperative and long-term follow-up results, and between the 1-year follow-up and long-term follow-up results. Improvements were found in Cobb angle between the preoperative results and the long-term follow-up with a median value from 66° to 18° (with a mean value from 67° to 25°, P < 0.0001), weight distribution on the seating surface was more even, with a median value from 89 to 78% on one seating surface (with a mean value from 87 to 74%, P < 0.0003). Sitting balance was better (P < 0.01), there were less seating supports in a wheelchair (P < 0.05), and less time for resting time (P < 0.05). The care given in physical effort and in time consumption was unchanged. There were no significant differences between the 1-year follow-up results and the long-term follow-up results (Table 3). At the long-term follow-up, none of the patients had persistent skin discoloration, and none used a brace. Patients who were able to walk preoperatively continued to walk at both the 1-year and long-term follow-ups.
Table 3.
Comparison of median values between the preoperative and long-term results, and the 1-year and long-term results
| Variable | Preop median (range q1–q3) | Postop 1 year median (range q1–q3) | Postop long-term median (range q1–q3) | Preop/long-term (P) | 1 year/long-term (P) |
|---|---|---|---|---|---|
| Angle of scoliosis (Cobb) | 66 (51–83) | 18 (10–35) | 17 (8–33) | 0.0001 | 0.3246 |
| Weight distribution on one seating surface (%) | 89 (80–97) | 78 (52–90) | 60 (57–66) | 0.0045 | 0.1727 |
| Sitting balance (1–7 points) | 4 (1–6) | 6 (1–7) | 6 (2–7) | 0.0051 | 0.1573 |
| Seating supports in wheelchair (0–7 supports) | 3 (1–3) | 1 (1–3) | 2 (1–3) | 0.0267 | 0.5898 |
| Time used for resting (h/week) | 8 (7–14) | 7 (5–13) | 4 (2–7) | 0.0184 | 0.4487 |
| Care given (physical effort 0–30 points) | 20 (19–22) | 21 (19–23) | 19 (18–21) | 0.8061 | 0.8335 |
| Care given (time consumption in mins) | 355 (233–400) | 275 (203–381) | 345 (293–419) | 0.2604 | 0.5002 |
Intention-to-treat analysis
An intention-to-treat analysis of the discontinued patients (n = 2) was conducted. The analysis was done by replacing the missing values by the last observation carried forward. This analysis showed that the discontinued patients did not affect the results.
Parents’ motives for surgery
Although some parents had two or three motives for surgery, most had only one. The results showed that the parents most often wanted to obtain improvements in seating posture, respiration, and better strength in the spine (Table 1).
Follow-up questionnaire
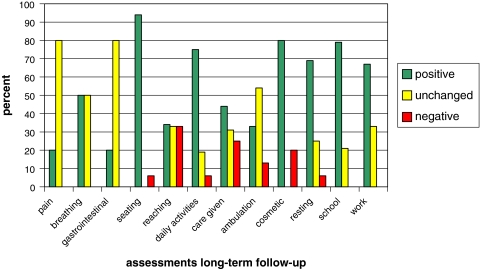
The results of the follow-up questionnaire, there the response alternative were trichotomized to positive, unchanged, negative, showed that seating posture, daily activities, school, work, and cosmetic appearance had improved (Fig. 1). There were no significant differences between the 1-year and the long-term follow-up results.
Fig. 1.
The results of the follow-up questionnaire. Parents’ assessment of how surgery affected 12 different areas at the long-term follow-up (n = 19)
Open-ended questions
Responses to the open-ended questions that were sent to relatives concerning what had improved or worsened since the surgery were classified in the following dimensions: daily activities, posture, mobility, general health, and quality of life.
Most of the answers were positive in relation to daily activities. Examples given were:
“Can look around at the surroundings better now”; “Can participate better in activities than before surgery”; “The communication/contact has increased, even with strangers because she can sit straight and look straight ahead”; “Easier for her to eat, and she doesn’t drop food any longer”; “Before surgery, she mostly slept”; “She has become more social and lively”; “She takes part in all activities now”; “Rides at a trot with only one person running beside her”. There were no negative responses in relation to daily activities.
Many parents had positive views about the girls’ change in posture:
“Stable and safe”; “Feeding and caring for her are easier”; “Has strength to keep herself in an upright position”; “Better head position”; “Straighter back of the head”; “Better head balance and doesn’t need to use a neck brace”; “Stable when sitting”; “Better sitting position in a car”; “Can sit in a wheelchair without seating supports”; “Better seating position because of better posture”; “Better seating and standing positions”; “Straight sitting position in the wheelchair”.
There were some negative responses in relation to posture.
“Can’t sit on the floor”; “The hip is fixed in an oblique position”; “The back of the head has become oblique”; “Pelvis is oblique”; “The rotation of the spine has continued”; “Difficult for her to stand”; “She walks with a stoop”.
The positive experiences reported concerning mobility were:
“Easier to change position”; “More stable when walking”; “Better balance”.
Negative experiences concerning mobility were:
“Stiffness in changing napkin”; “Can’t get up from the floor”; “More stiffness in the spine”; “Needed to use a lift”; “Stiffer in her ability to move”; “Can’t turn around in bed”; “More difficult to handle her in lifting situations”.
The answers concerning general health and quality of life were mostly positive:
“Better breathing”; “Fewer episodes of pneumonia”; “Better absorption of oxygen”; “Fewer cold episodes”. “More lively”; “Better general health”; “She no longer throws up”; “Happier”; “Better health”; “Undoubtedly, her quality of life is much better”; “The whole family feels better after the scoliosis surgery”.
Some negative responses concerning regained general health and quality of life were:
“Increased heat in one foot”; “Urine leakage when we are lifting her up”; “The left leg has become more swollen with a red-blue color”; “Her weight has increased”; “She has a bump on her back”.
Discussion
Huang et al. [3] suggested that surgical intervention is the only method available to reduce the degree of deformity and improve trunk balance for sitting and walking compared with brace treatment in girls with Rett syndrome over 8 years of age.
All the girls in the present long-term follow-up study who were able to walk preoperatively continued to be able to walk at the long-term follow-up. These results are in line with Harrison and Webb [2], whose retrospective, short-term follow-up after surgical correction of scoliosis (n = 8) found that all the girls who were able to walk preoperatively (n = 5) were still able to walk 1 year postoperatively. Kerr et al. [4] found that of 13 girls who walked independently preoperatively, 12 still did so 1 year postoperatively.
Scoliosis surgery to stabilize the trunk in patients with Rett syndrome has been described in a retrospective study by Kerr et al. [4]. In this study, the parents completed a health questionnaire after surgery an average of 7 years postoperatively. The results of the questionnaire and the open-ended questions demonstrated an overall well-being and reported better sitting posture and better breathing, which reflected the parents’ motive for surgery preoperatively.
The present prospective, long-term follow-up study (>4 years) showed an overall positive result except for care giving, which was unchanged. However, an unchanged result after surgery does not necessarily indicate poor results. An explanation could be that girls with Rett syndrome need a lot of care day and night because of the syndrome that is not related to the surgery.
The results from the present study correspond with the long-term follow-up of functioning after spinal surgery in patients with neuromuscular scoliosis [7]. The parents’ views confirmed the other measurements, except for general health and quality of life, which could be of interest in a future study. There were no differences between the 1-year follow-up results and the long-term follow-up results, which are the same as in the patients who did not understand verbal instructions in the long-term follow-up of patients with neuromuscular scoliosis [7].
We could not use the whole set of instruments because of the girls’ difficulties in understanding verbal instructions during the assessments [5–7]. Accordingly, we could not measure activities of daily living from an objective perspective. Nevertheless, the parents reported solely positive effects on daily activities in the open-ended questions.
Conclusions
We can conclude that the stabilized spine resulted in sufficient strength to keep the body upright with the possibility of looking around at the surroundings more easily. The girls got better seating position with less need for seating adaptations in the wheelchair and with reduced time needed for resting during the day.
Finally we can conclude that the indication for surgery is to get a better posture which lead to less risk of pressure sores, and that un upright position lead to better possibility to easily breath with fewer episodes of pneumonia and a better general health as result.
The evidence of positive surgical effects for girls with Rett syndrome is of great importance in indication for surgery in the decision-making process.
Footnotes
In the Aaro anterior system the rod is replaced by two cm thick six cm wideband. It passes vertebral plates fixated to the vertebrae by two screws. The correction is by compression.
References
- 1.Gillings D, Koch G. The application of the principle of intention-to-treat to the analysis of clinical trials. Drug Inf J. 1991;25:411–424. [Google Scholar]
- 2.Harrison DJ, Webb PJ. Scoliosis in the Rett syndrome: natural history and treatment. Brain Dev. 1990;12(1):154–156. doi: 10.1016/s0387-7604(12)80200-2. [DOI] [PubMed] [Google Scholar]
- 3.Huang T-J, Lubicky JP, Hammerberg KW (1994) Scoliosis in Rett Syndrome. Orthopaedic review. December 1994, pp 931–937 [PubMed]
- 4.Kerr AM, Webb P, Prescott RJ, Milne Y. Results of surgery for scoliosis in Rett syndrome. J Child Neurol. 2003;18(10):703–708. doi: 10.1177/08830738030180101201. [DOI] [PubMed] [Google Scholar]
- 5.Larsson E-L, Aaro S, Ahlinder P, Öberg B. Preoperative evaluation of activity and function in patients with paralytic scoliosis. Eur Spine J. 1998;7:294–301. doi: 10.1007/s005860050078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Larsson E-L, Aaro S, Öberg B. Activities and functional assessment 1 year after spinal fusion for paralytic scoliosis. Eur Spine J. 1999;8:100–109. doi: 10.1007/s005860050137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Larsson E-LC, Aaro SI, Normelli HC, Öberg BE. Long-term follow-up of functioning after spinal surgery in patients with paralytic scoliosis. Spine. 2005;30(19):2145–2152. doi: 10.1097/01.brs.0000180403.11757.6a. [DOI] [PubMed] [Google Scholar]
- 8.Larsson G, Lindström B, Engerström IW. Rett syndrome from a family perspective: the Swedish Rett Center survey. Brain Dev. 2005;27(Suppl 1):14–19. doi: 10.1016/j.braindev.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 9.Lidström J, Stokland E, Hagberg B. Scoliosis in Rett syndrome. Clinical and biological aspects. Spine. 1994;19(14):1632–1635. doi: 10.1097/00007632-199407001-00013. [DOI] [PubMed] [Google Scholar]
- 10.Meguro K, Ueda M, Yamaguchi T, et al. Disturbance in daily sleep/wake pattern in patients with cognitive impairment and decreased daily activity. J Am Geriatr Soc. 1990;38:1176–1182. doi: 10.1111/j.1532-5415.1990.tb01495.x. [DOI] [PubMed] [Google Scholar]
- 11.Mulcahy CM, Poutney TE, Nelham RL, Green EM, Billington GD. Adaptive seating for motor handicap: problems, a solution, assessment, and prescription. Br J Occup Ther. 1988;51:347–352. [Google Scholar]
- 12.Samuelsson K, Larsson E-L, Normelli H, Öberg B, Aaro S, Tropp H. Development of an instrument for clinical evaluation after surgery for neuromuscular scoliosis. Eur Spine J. 1996;5:400–406. doi: 10.1007/BF00301968. [DOI] [PubMed] [Google Scholar]